Abstract
Objective
To test the impact of two levels of intervention on communication frequency, quality, success, and ease between nurses and intubated intensive care unit (ICU) patients.
Design
Quasi-experimental, 3-phase sequential cohort study: (1) usual care, (2) basic communication skills training (BCST) for nurses, (3) additional training in augmentative and alternative communication devices and speech language pathologist consultation (AAC + SLP). Trained observers rated four 3-min video-recordings for each nurseepatient dyad for communication frequency, quality and success. Patients self-rated communication ease.
Setting
Two ICUs in a university-affiliated medical center.
Participants
89 intubated patients awake, responsive and unable to speak and 30 ICU nurses.
Main results
Communication frequency (mean number of communication acts within a communication exchange) and positive nurse communication behaviors increased significantly in one ICU only. Percentage of successful communication exchanges about pain were greater for the two intervention groups than the usual care/control group across both ICUs (p = .03) with more successful sessions about pain and other symptoms in the AAC + SLP group (p = .07). Patients in the AAC SLP intervention group used significantly more AAC methods (p = .002) and rated communication at high difficulty less often (p < .01).
Conclusions
This study provides support for the feasibility, utility and efficacy of a multi-level communication skills training, materials and SLP consultation intervention in the ICU.
Keywords: Communication, Mechanical ventilation, Critical care, Patient–provider communication, Augmentative and alternative, communication, Nurse–patient communication
Introduction
Communication difficulties are a common problem for mechanically ventilated patients in the intensive care unit (ICU) that causes distress, fear, and anger1–9 for patients and is a source of frustration and stress for ICU staff.10,11 Critical care nurses receive little or no training in communication assessment or the use of augmentative and alternative communication (AAC) techniques with intubated patients.11,12 Moreover, nurses report inconsistent availability of AAC communication materials and speech therapy consultation in the ICU.11–14 Few solutions have been offered or systematically tested with intubated ICU patients.15–17
The only published randomized controlled trial of an AAC intervention in a critical care setting examined the use of communication boards in 50 post-operative cardiac surgical patients.17 Patients in the experimental group (n = 20) reported significantly higher satisfaction during the early postoperative period than did those who received usual care.17 Specific electronic communication devices were tested for use with ICU patients in several pilot feasibility studies.18–22 Patients initiated communication more often when using electronic devices and ease of communication ratings improved; however, observed patient use of the devices was sparse and inconsistent.19,21 These studies employed small samples and lacked comparison groups.18–22 Physical and cognitive fluctuation or deterioration during critical illness, physical restraint use, inconsistency in nurse–patient assignments, and staff lack of knowledge or access to AAC tools are barriers to the widespread use of AAC techniques and devices in the ICU.14,19,21,23,24 There have been no large scale controlled trial studies of AAC tools in the ICU and no studies have tested the effectiveness of providing nurses with education on communication strategies to use with intubated ICU patients.
We developed a two-tiered, multi-faceted, interdisciplinary intervention. This paper reports results from a 3-phase clinical trial to measure the impact of these interventions on the frequency, quality, success, and ease of communication interactions between nurses and intubated ICU patients. Phase 1 was a usual care, control group. Phase 2 intervention consisted of nurse communication training and the provision of AAC materials. Phase 3 added electronic AAC devices and speech language pathologist (SLP) consultation to the intervention. We hypothesized that observations of communication frequency, success, quality and ease would improve between phases, as the level of intervention strategies increased.
Methods
Design
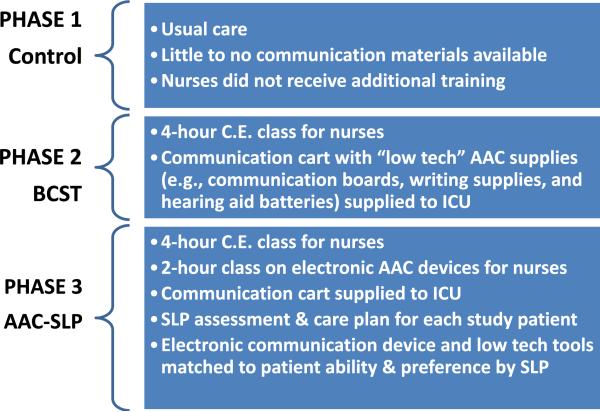
The Study of Patient-Nurse Effectiveness with Assisted Communication Strategies (SPEACS) was a quasi-experimental clinical trial, employing a 3-phase sequential cohort design. Study design and methods have been previously published in detail.25–28 Fig. 1 shows a summary of each phase. All procedures were approved by the University Institutional Review Board. Nurses and patients or their decisional surrogates provided written informed consent for participation.
Fig. 1.
Intervention Description by Phase. BCST = Basic Communication Skills Training; AAC = Augmentative and Alternative Communication; SLP = Speech Language Pathologist, C.E. = continuing education, SLP – speech language pathologist. Reprinted with permission from Broyles LM, Tate JA, Happ MB. Am J Crit Care, 2012; 21(2):e21-32.
Setting
The study was conducted in the 32-bed medical intensive care unit (MICU) and 22-bed cardiovascular-thoracic intensive care unit (CT-ICU) of a large tertiary care medical center in the Mid-Atlantic region. Recruitment began in July, 2004 and ended in June, 2008. We report results with unit names removed to preserve anonymity of participants.
Sample
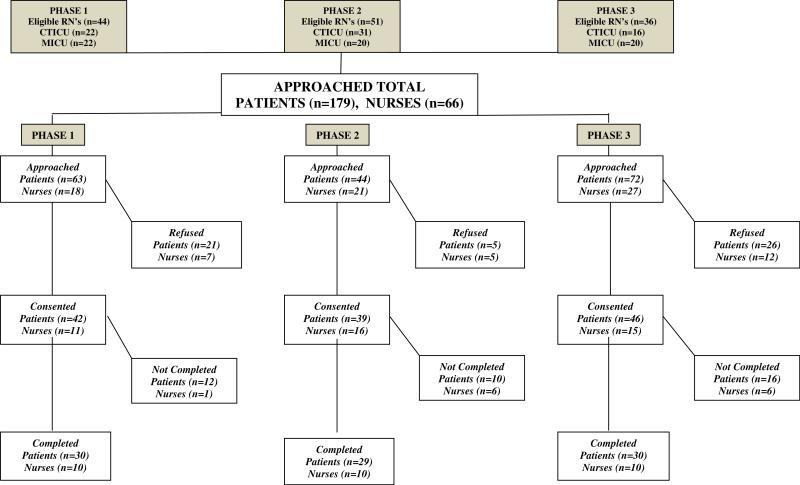
Inclusion criteria for nurses were a minimum of one year critical care practice experience and regularly working two consecutive day shifts in the study unit. Nurses were excluded if they had a hearing or speech impairment. Eligible nurses who met criteria were identified from the staffing schedule and selected using stratified random sampling procedure to achieve 10 nurses (5 per ICU) in each phase of the study (See Fig. 2).25 The target enrollment (10 nurses per phase) was specified by the study design and a priori sample size calculation.25 For each phase, 10 new nursing staff were recruited and past participants were excluded to maintain independence of the sample for each phase. Nurses received $150 in grocery store gift cards at the conclusion of study participation.
Fig. 2.
Enrollment diagram. RN = registered nurse.
Eligible patients were identified when enrolled study nurses’ were scheduled to work two consecutive day shifts. Patient inclusion criteria included: endotracheal or tracheal intubation without ability to vocalize; predicted by clinicians to remain intubated for 2–3 days after study enrollment; awake and responding to commands; and understands English. Exclusion criteria included: GCS < 13; previous hearing or speech impairment seriously interfering with communication function as measured by National Outcome Measurement System subscale score <329; or previous diagnosis of dementia. We included patients who were delirious or who had received sedation in order to maximize generalizability.
Intervention
During Phase 1, assistive communication materials available were primarily pen and paper and, less commonly, alphabet letter boards or materials (e.g., dry erase boards) supplied by patients’ families (Fig. 1).27 SLPs were consulted only for dysphasia and swallowing evaluations.
In Phase 2, nurses were provided a 4 h basic communication skill training aimed at improving their knowledge and skill in assessing the communication abilities of intubated ICU patients and in applying AAC strategies. Content was consistent with the principles of augmentative and assistive communication30 and relationship-centered care.31 Each nurse participant received an instructional binder and pocket-reference algorithm to guide communication assessment and strategies. “Low tech” communication materials (e.g., spiral notebooks, felt-tip pens, clipboards, hand grip writing aids, a variety of communication boards featuring alphabet, pictures, or phrases, and hearing aid batteries) were supplied to the units in “communication carts” when training commenced.32 Carts were inventoried and re-stocked weekly.
In Phase 3, nurses received the basic communication skills training and additional 2 h training in electronic communication devices. The dedicated SLP, specially trained in AAC for the acute care setting, provided a 45–60 min individual evaluation and AAC intervention for each patient in this study group with daily follow-up during the two-day observation period. A communication care plan was devised that included both a low tech and electronic communication device option which was matched to individual patient ability and preference. The communication care plan also highlighted appropriate nurse communication strategies and potential communication topics.33
Data collection
Outcome evaluation
For each nurse–patient dyad (i.e., pair), four observations were video recorded twice daily (morning and afternoon) during two consecutive days, for each nurse–patient dyad. A minimum of 3 min was recorded to ensure adequate and equal opportunities for communication interaction. Three minutes has been established as a functional time frame for sending, receiving, confirmation, and follow-up of messages in the ICU.25,26,34–36 To minimize the “Haw thorne effect,” one de-sensitizing session, not included in the analysis, was videotaped for each dyad in the morning of the first observation day. Data collector field notes supplemented video recordings.
Measures
Patient and nurse demographic and clinical information relevant to communication and hospitalization were collected to describe the sample. Patient data included severity of illness (APACHE III),37,38 delirium (CAM-ICU),39 sedation–agitation (RASS),40,41 intubation type, and length of time intubated prior to observation. The ten-point RASS observational scale (−5 to +4) is validated for use in MV patients. Psychometric properties are well established. The RASS values were collapsed to three categories: sedated (−5 to −1), calm (0) and agitated (+1 to + 4) for the analysis.
There were no previously established measures of communication performance between nurses and patients in the critical care setting other than counts of positive and negative behaviors34,36,42 and “interaction”35 with little methodological description. We used a microanalytic measurement approach and adapted communication outcome measures (i.e., frequency,35,43–45 quality,34,36,42 success,43–45 and ease3) from the communication disorders literature and prior observational studies of nurse–patient communication in the ICU. Although there are no established benchmarks for communication performance outcomes between intubated patients and clinicians in the ICU, the usual care group measures provided a baseline for comparison.26 Video recordings were transcribed for verbal and nonverbal behaviors and then segmented into communication acts and exchanges by trained coders. A communication act is a unit of communicative behavior, non-vocal or verbal, that is directed from one conversational participant to another in an attempt to convey a message. An exchange is a cluster of continuous communication acts related to the communication of a single idea.46
Coders rated each video recording for communication outcomes. Ratings of communication acts were aggregated within each nurse–patient exchange and ultimately each observation session. Table 1 provides communication measurement definitions. In particular, the number of acts per exchange were computed and subsequently averaged across the exchanges occurring within each session to measure the frequency of communication. The number of patient initiated exchanges and number of patient communication acts per exchange were similarly computed as indicators of patient communication frequency and independence.43
Table 1.
Communication outcomes – measurement glossary.
| Variable | Operational definition |
|---|---|
| Frequencya | (a) Mean number of communication acts/exchange, (b) Mean number of communication exchanges/3-min session; (c) Patient initiated exchanges; (d) Patient acts/exchange |
| Successa | 1 = no communication response when one is obligated |
| 2 = message attempted but not conveyed or abandoned | |
| 3 = message partially conveyed (partner has to interpret to obtain partial meaning, partner has to clarify) | |
| 4 = message conveyed with adequate partner response indicating comprehension of basic meaning | |
| 5 = message conveyed with elaborated partner response (action or verbal) indicating complete comprehension of entire message (basic idea plus details) | |
| NA = message did not obligate a response | |
| Qualitya | Sum of positive, facilitative communication behaviors by nurse during communication acts versus sum of negative, communication-inhibiting nurse behaviors for 3-min session |
| Positive nurse behaviors | (1) Asks tagged yes–no questions, (2) Provides response choices, (3) Physically assists patients, (4) Suggests mode of communication, (5) Repeats patient response, (6) Augments comprehension, (7) Repeats for clarification, (8) Greets patient by name/touch, (9) Asks open ended questions when patient has method to respond, (10) Makes eye contact |
| Negative nurse behaviors | (1) Removes AAC system inappropriately (i.e., out-of-reach or before patient finished), (2) Does not gain patient's attention before interaction, (3) Does not provide assistance when needed, (4) Asks questions that patient can't answer, (4) Ignores patient communication attempt, (5) Does not provide opportunity for patient response (pause time), (6) Interrupts patient's message, (7) Does not gain patient's attention, (8) Self talk, mumbling (9) Speaks too rapidly, (10) Does not look at patient during interaction |
| AAC use | Sum of acts (events) using augmentative and alternative communication tools to convey a message per communication exchange |
| Easea | Patient's self-report on a scale of 1 (not difficult at all) to 5 (extremely difficult) at the end of each video-recorded observation session. The categories were collapsed for analysis into three levels: low (=1, 2), medium (=3), and high (=4, 5) difficulty. |
AAC = augmentative and alternative communication.
Indicates main outcome variable.
Each nurse communication act was rated for quality in terms of the total number of positive and negative behaviors which were then averaged for each exchange and further aggregated across exchanges for each session. We also computed the rate of AAC use events per exchange as a component of communication quality. Each communication exchange was rated for success on a 5 point scale, ultimately yielding the percentage of successful exchanges per session when ratings were collapsed to unsuccessful (scores between1 and 3) or successful (score 4 or 5) (Table 1). We further examined the subset of communication exchanges about pain for percentage of successful exchanges. We derived a measure of pain and symptom communication success by scoring each video session as ‘successful’ if all exchanges about pain and other symptoms in the session were rated as successful. Ease of communication was measured at the end of each session by patients’ self-report on a scale of 1 (not difficult at all) to 5 (extremely difficult) and collapsed for analysis into three levels: low (=1, 2), medium (=3), and high (=4, 5) difficulty.
Reliability of measurement
Consistency of communication ratings was achieved using a three-pronged approach. First, raters were trained and routinely tested for consistency by independently rating novel video sessions; they achieved and maintained >80% independent inter-rater agreement on ratings of success and >95% on other outcome variables. The 80% threshold is commonly acceptable inter-rater agreement in observational coding from videos.42,47–49 Secondly, all videos were reviewed by 2 raters, a primary and secondary rater, before finalizing. Finally, a stratified random sample of 10% of video recordings representing all phases was independently assessed by an external, PhD prepared reviewer who was experienced in coding nonverbal communication and blinded to phase assignment. Inter-rater reliability, estimated using simple or weighted kappa statistics, showed excellent to near perfect agreement on outcome variables of interest50: initiator of communication (k = 1.00), pain–symptom topic determination (k = .816), scaled success ratings (k .868), dichotomous success ratings (k = .749), quality (positive and negative nurse communication behaviors) (k = .814–.997), topic categories (k .816), and patient communication method (AAC use) (k = .951–.999).
Statistical analysis
Exploratory data analyses were first performed to identify any data anomalies (e.g., missing data, outliers, severe violations of underlying statistical assumptions) that might invalidate study findings. Descriptive statistics were computed to evaluate data distributions and summarize the sample and group characteristics. Using appropriate group comparative statistics (e.g., ANOVA, Kruskal–Wallis test, Fisher's exact test), the three groups were compared to identify any imbalances which may lead to possible confounding.
Linear mixed models were fit to analyze the communication outcomes for frequency, success, and quality. In those instances where the distribution of residuals was non-normal (e.g., percentage of successful exchanges), a data transformation was applied. In terms of design effects, these models included fixed between-subjects effects for phase (usual care, BCST, ACC + SLP) and type of intensive care unit (labeled unit A or B), fixed+within-subjects effect for session (1–4), and their interactions. Random effects were included for nurse and dyad. The best-fitting covariance structure for the repeated session assessments was chosen based on standard information criteria (AIC, AICC, and BIC). When analyzing longitudinal categorical outcomes of success (all exchanges successful vs. not) and the ordinal outcome of communication ease (difficulty), generalized linear mixed models were fit, considering the same design effects, but now assuming a binomial and multi-nomial error structure using cumulative logits, respectively. Models initially included all main effects and interactions; however, parsimonious models, which dropped non-significant interaction effects, were also estimated. In addition to non-directional omnibus tests, linear contrasts were employed to test the expected differential of the two levels of communication intervention. Covariates (e.g., delirium, intubation type, physical restraint use, years of nursing experience, days of intubation prior to observation) were also included in the model based on the literature and the exploratory data analyses results. Finally, we conducted a sub-analysis of acts per exchange by computing the percentage of acts with the linguistic function of clarification in each exchange (averaged across exchanges within a session). Parsimonious models, which dropped nonsignificant covariate and interaction effects, are reported. Analyses were conducted using SAS for Windows Version 9.2 (SAS Institute, Inc., Cary, NC) with the level of significance set at .05.
Results
Sample
Among 131 eligible nurses (RNs) identified for the study, 42 (31.1%) were enrolled; twelve (28.6%) nurses withdrew/dropped out (due to personal reasons, relocation, change in employment status, or to attend graduate school) before study completion for a final nurse sample of 30 RNs. Each study nurse was observed with a total of three intubated ICU patients. A total of 179 patients met study eligibility criteria and were approached for enrollment, 127 (70.9%) were enrolled and 93 patients completed all procedures. Four were removed from the sample when their assigned study nurse dropped out (Fig. 2). A nurse who was only able to complete required study observation days with two patients was retained in the sample. The final sample for analysis consisted of 89 nurse–patient dyads and 356 video recorded observations. Tables 2 and 3 present participant (patient and nurse) clinical and demographic characteristics by phase. There were no statistically significant differences between units on main demographic variables for patients or nurses.
Table 2.
Patient characteristics.
| Usual care |
BCST |
AAC + SLP |
Total |
p-value |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Unit A (n = 15) |
Unit B (n = 15) |
Unit A (n = 14) |
Unit B (n = 15) |
Unit A (n = 15) |
Unit B (n = 15) |
Unit A (n = 44) |
Unit B (n = 45) |
Group | Unit | Group by unit | |
| Total (n = 30) | Total (n = 29) | Total (n = 30) | Total (N = 89) | ||||||||
| Demographic characteristic | |||||||||||
| Age (years) | 54.1 ± 15.6 | 58.5 ± 16.1 | 58.4 ± 16.9 | 57.8 ± 14.7 | 58.4 ± 10.1 | 53.7 ± 20.8 | 57.0 ± 14.2 | 56.7 ± 17.1 | .87 | .93 | .55 |
| 56.3 ± 15.7 | 58.1 ± 15.5 | 56.1 ± 16.2 | 56.8 ± 15.7 | ||||||||
| Femalea | 5 (33) | 11 (73) | 8 (57) | 8 (53) | 6 (40) | 7 (47) | 19 (43) | 26 (58) | .64 | .25 | .23 |
| 16 (53) | 16 (55) | 13 (43) | 45 (51) | ||||||||
| Whitea | 12 (80) | 11 (73) | 13 (93) | 13 (87) | 15 (100) | 15 (100) | 40 (91) | 39 (87) | .03 | NA | 1.00 |
| 23 (77) | 26 (90) | 30 (100) | 79 (89) | ||||||||
| Education (years) | 13.1 ± 2.2 | 12.9 ± 1.9 | 13.6. ± 2.8 | 12.4 ± 2.1 | 14.1 ± 3.7 | 12.8 ± 2.7 | 13.6 ± 2.9 | 12.7 ± 2.2 | .74 | .11 | .61 |
| 13.0 ± 2.0 | 13.0 ± 2.5 | 13.5 ± 3.2 | 13.2 ± 2.6 | ||||||||
| Clinical characteristic | |||||||||||
| APACHE III score | 48.6 ± 9.9 | 50.3 ± 16.2 | 55.9. ± 11.7 | 56.3 ± 25.6 | 59.0 ± 13.3 | 50.5 ± 17.7 | 54.5 ± 12.3 | 52.4 ± 20.0 | .27 | .56 | .44 |
| 49.5 ± 13.2 | 56.1 ± 19.8 | 54.8 ± 16.0 | 53.4 ± 16.6 | ||||||||
| Days intubated prior to enrollment | 62.8 ± 63.5 | 24.8 ± 13.5 | 64.3 ± 49.7 | 66.1 ± 78.3 | 80.4 ± 46.7 | 97.1 ± 119.9 | 69.3 ± 53.2 | 62.7 ± 86.5 | .02 | .73 | .72 |
| 12.6 ± 11.7 | 27.9 ± 24.0 | 28.7 ± 31.0 | 23.0 ± 24.5 | ||||||||
| Intubation type: tracheostomy | 13 (87) | 5 (33) | 13 (93) | 10 (67) | 14 (93) | 13 (87) | 40 (91) | 28 (62) | .09 | .01 | .53 |
| 18 (60) | 23 (79) | 27 (90) | 68 (76) | ||||||||
| Physical restraint | 0 (0) | 6 (40) | 2 (14) | 4 (27) | 1 (7) | 3 (20) | 3 (7) | 13 (29) | .73 | .99 | .96 |
| 6 (20) | 6 (21) | 4 (13) | 16 (18) | ||||||||
| CAM-ICUa- delirium present | 2 (13) | 5 (33) | 3 (21) | 6 (40) | 3 (20) | 2 (13) | 8 (18) | 13 (29) | .68 | .48 | .53 |
| 7 (23) | 9 (45) | 5 (23) | 21 (32) | ||||||||
| RASSa- sedated/agitated | 12 (80) | 11 (73) | 12 (86) | 7 (47) | 13 (87) | 11 (73) | 37 (84) | 14 (64) | .80 | .12 | .55 |
| 7 (23) | 19 (66) | 24 (80) | 66 (74) | ||||||||
| Pulmonary disease/infection | 10 (67) | 13 (87) | 2 (14) | 11 (73) | 7 (47) | 11 (73) | 19 (43) | 35 (78) | .03 | .00 | .44 |
| 23 (76) | 13 (45) | 18 (60) | 54 (60) | ||||||||
| Cardio, thoracic, or vascular surgery | 4 (27) | 0 (0) | 13 (93) | 2 (13) | 10 (67) | 3 (20) | 27 (61) | 5 (11) | .00 | .00 | .37 |
| 4 (13) | 15 (52) | 13 (43) | 32 (36) | ||||||||
| Postoperative complications | 6 (40) | 1 (7) | 13 (93) | 2 (13) | 4 (27) | 4 (27) | 23 (52) | 7 (16) | .04 | .00 | .00 |
| 7 (23) | 15 (52) | 8 (27) | 30 (34) | ||||||||
Note: Mean and standard deviation reported for continuous data (Mean + SD) and count and percentages (n, (%)) reported for categorical data. Abbreviations: BCST = basic communication skills training, AAC + SLP = basic communication skills training and electronic augmentative and alternative communication device education with an individualized speech language pathologist consultation, APACHE III = acute physiology and chronic health evaluation, version 3, CAM-ICU = confusion assessment method for the ICU, RASS = Richmond agitation and sedation scale.
p-value from an F-test from two-way analysis of variance.
p-value using exact estimation in binary logistic regression.
Table 3.
Baseline nurse characteristics.
| Characteristic | Usual care (n = 10) |
BCST (n = 10) |
AAC + SLP (n = 10) |
Total (N = 30) |
Test statistic, p-value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Unit A (n = 5) | Unit B (n = 5) | Unit A (n = 5) | Unit B (n = 5) | Unit A (n = 5) | Unit B (n = 5) | Unit A (n = 15) | Unit B (n = 15) | ||
| Age (years) | 43.2 ± 11.7 | 40.4 ± 5.3 | 30.0 ± 12.4 | 30.4 ± 12.3 | 29.6 ± 4.6 | 38.8 ± 1.9 | 34.3 ± 11.5 | 36.5 ± 8.5 | Fphase = 4.2, p = .03 |
| 41.8 ± 8.7 | 30.2 ± 11.6 | 34.2 + 5.9 | 35.4 + 10.0 | Funit = .5, p = .50 | |||||
| Fpxu = 1.2, p = .33 | |||||||||
| Female | 3 (60) | 5(100) | 4 (80) | 4 (80) | 5 (100) | 3 (60) | 12 (80) | 12 (80) | Scorephase = .4, p = 1.00 |
| 8 (80) | 8 (80) | 8 (80) | 24 (80) | Scoreunit = NA, p = NA+ | |||||
| Scorepxu = 4.1, p = .49 | |||||||||
| Bachelors or greater | 4 (80) | 4 (80) | 5 (100) | 5 (100) | 3 (60) | 2 (40) | 12 (80) | 11 (73) | Scorephase = 5.7, p = .08 |
| 8 (80) | 10 (100) | 5 (50) | 23 (77) | Scoreunit = NA, p = NA+ | |||||
| Scorepxu = .1, p = 1.00 | |||||||||
| Nursing experience (years) | 13.4 ± 12.1 | 17.8 ± 6.1 | 8.8 ± 13.6 | 7.8 ± 14.1 | 5.0 ± 3.7 | 7.8 ± 7.9 | 9.1 ± 10.5 | 11.1 ± 10.5 | Fphase = 2.2, p = .13 |
| 15.6 ± 9.3 | 8.3 ± 13.1 | 6.4 ± 6.0 | 10.1 ± 10.4 | Funit = .3, p = .59 | |||||
| Fpxu = .2, p = .84 | |||||||||
| Critical care experience (years) | 12.0 ± 12.4 | 10.6 ± 5.6 | 8.0 ± 12.4 | 5.6 ± 9.2 | 2.4 ± .6 | 4.6 ± 5.3 | 7.5 ± 10.2 | 6.9 ± 6.9 | Fphase = 2.1, p = .15 |
| 11.3 ± 9.1 | 6.8 ± 10.3 | 3.5 ± 3.7 | 7.2 ± 8.6 | Funit < .1, P = .87 | |||||
| Fpxu = .2, p = .82 | |||||||||
Note: F-tests obtained from two-way analysis of variance.
Scores obtained using exact testing in logistic regression.
BCST = basic communication skills training.
AAC = augmentative and alternative communication.
SLP = speech language pathology.
NA = not available; no variability in the BCST group.
The mean number of days that patients were intubated prior to participating in the study varied among the three groups with the final, Phase 3, intervention group having significantly longer pre-study intubation periods than the Phase 1 usual care group (F 4.3, p = .015). Accordingly, tracheostomy was slightly more prevalent in the intervention groups than in the usual care group. Despite the use of random selection, nurses in the Phase 1 were significantly older than nurses in the Phase 2 group (Tukey HSD Mean difference = 11.6 years, p = .025). Although age differences were found, there were no statistically significant differences in years of nursing or critical care experience between three groups of nurses. All of these factors were considered in the multivariate analyses.
Outcomes
We delivered all components of each intervention level at both ICU sites (Table 4) and nurse ratings of the training programs were high.51 Training materials and communication supplies were acceptable to most (92%) nurse participants on course evaluations.
Table 4.
Cohort comparison of communication outcomes.
| Communication outcome | Usual care (n = 30) | BCST (n = 29) | AAC + SLP (n = 30) | Total (N = 89) | Test statistic, p-value |
|---|---|---|---|---|---|
| Frequency MNAEA | 5.52 ± .41 | 7.37 ± .42 | 7.50 ± .41 | 6.76 ± .20 | Fphase = 7.10, p < .01 |
| Funit = 1.32, p = .25 | |||||
| Fpxu = 8.89, p < .01 | |||||
| Positive behaviorB | .72 ± .06 | .81 ± .07 | .63 ± .07 | .73 ± .02 | Fphase = 2.33, p = .10 |
| Funit = 11.30, p < .01 | |||||
| Fpxu = 3.57, p = .03 | |||||
| SuccessA | .72 ± .04 | .72 ± .04 | .79 ± .04 | .74 ± .02 | Fphase = .80, p = .46 |
| Funit = .02, p = .90 | |||||
| Success about pain and other symptomsA | Wald Chi Sqphase = 5.38, p = .07 | ||||
| Wald Chi Squnit = .08, p = .78 | |||||
| Not successful | 18 (64.3) | 10 (26.3) | 10 (38.5) | 38 (45.8) | |
| Successful | 10 (35.7) | 19 (65.5) | 16 (61.5) | 45 (54.2) | |
| Missing | 2 | 0 | 4 | 6 | |
| Success about painA | Wald Chi Sqphase = 7.11, p = .03 | ||||
| Wald Chi Squnit = .47, p = .50 | |||||
| Not successful | 16 (61.5) | 7 (29.2) | 6 (27.3) | 29 (40.3) | |
| Successful | 10 (38.5) | 17 (70.8) | 16 (72.7) | 43 (59.7) | |
| Missing | 4 | 5 | 8 | 17 | |
| Level of difficulty in communicationC: | Fphase = 7.67, p < .01 | ||||
| Funit = 8.02, p < .01 | |||||
| Easy | 18 (60.0) | 16 (55.2) | 21 (75.0) | 55 (61.8) | |
| Difficult | 8 (26.7) | 9 (31.0) | 3 (10.7) | 20 (22.5) | |
| Missing | 4 | 4 | 6 | 14 |
Note: F-tests obtained from mixed modeling analyses. Statistics obtained when adjusting for the following set of variables.
BCST = basic communication skills training.
AAC + SLP = communication training, electronic augmentative and alternative communication devices + speech language pathology consultation.
MNAE = mean number of communication acts in an exchange.
: no covariate adjustment required.
: sedation (RASS) (F = 6.63, p < .01) added to the model.
: delirium (cAM-ICU) (F = 11.46, p < .001) added to the model.
Note: Mean and standard error reported for continuous data (mean + SD) and count and percentages (n, (%)) reported for categorical data.
Frequency
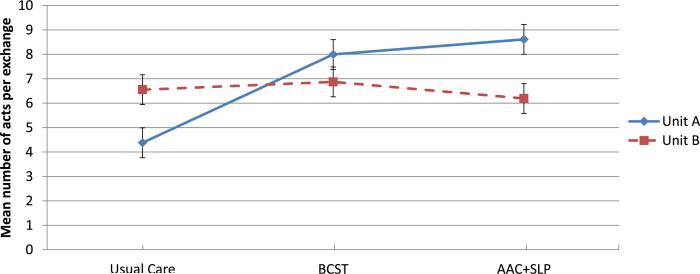
Mean number of communication acts within a communication exchange showed a significant intervention effect, and an interaction between unit and group (F = 8.89, p < .01). Only Unit A had an increase in the mean number of communication acts per exchange between the usual care group and each of the intervention group [Phase 1 vs. Phase 3 (t = 5.27, p < .0001); Phase 1 vs. Phase 2 (t = 4.17, p < .0001)] (See Fig. 3). This group by unit interaction remained significant when adjusting for covariates. None of the covariates were associated with frequency. There were no differences between groups in mean number of exchanges, mean percentage of patient-initiated exchanges, or mean percentage of patient acts in exchanges.
Fig. 3.
Communication frequency* by unit and phase. Legend: *Mean number of communication acts per exchange.
Further examination of the increase in communication act frequency revealed an increase in the rate of acts with the linguistic function of clarification (e.g., interpretation of nonverbal messages, reading aloud of written message, validation of message, and any attempt to resolve a breakdown). The percentage of acts per exchange used for clarification was significantly higher in the intervention groups (15.3% for Phase 2 and 12.5% for Phase 3) compared to the Phase 1 control group (9.3%) (F = 7.20, p < .001). There were no significant differences in percentage of clarification acts between Phase 2 and Phase 3 intervention groups.
Success
The percentage of successful exchanges (ratings of 4 or 5) was generally high across groups (approximately 75%). There were no differences between groups in mean percentages of successful communication exchanges even when controlling for delirium.
When success was analyzed by topic of exchanges, the intervention groups exhibited a significantly greater percentage of successful communication exchanges about pain than did the control group (Wald Chi-Square 7.11, p = .03) [Phase 1 vs. Phase 2 (Odds Ratio = 3.87); Phase 1 vs. Phase 3 (Odds Ratio = 4.18)]. There were no significant differences between the two= intervention groups. The significant difference in successful exchanges about pain in the intervention groups (compared with control) remained when controlling for delirium. The intervention effect was also maintained when considering such covariates as sedation, method of intubation, and APACHE score. No covariates were associated with success about pain.
We further analyzed successful topic communication about pain and other symptoms together by examining the proportion of observation sessions in which all pain and symptom exchanges were successful. This analysis included 82 dyads in which pain or symptom topics were discussed and showed a borderline signifi-cant intervention effect (Wald Chi-Square =5.38, p = .07) The borderline intervention effect was maintained when considering such covariates as sedation, method of intubation, and APACHE score. No covariates were associated with success about pain and other symptoms.
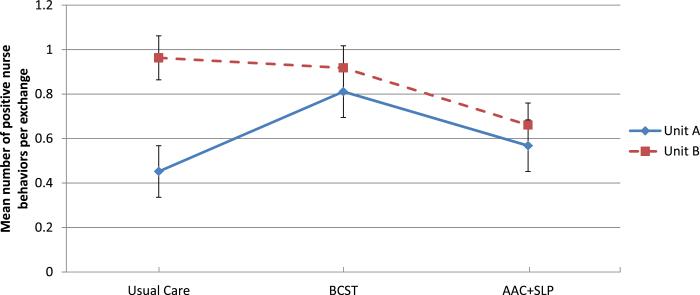
Quality
Negative nurse behaviors were infrequent and remained relatively constant across groups. Positive nurse behaviors increased significantly from Phase 1 to the Phase 2 intervention group only, and only in Unit A (t = 2.35, p = .020) (See Fig. 4). There was an increase in positive nurse behaviors overall when the patient tested positive for delirium (t = 3.21, p = .001). Sedation level exerted a significant positive effect on positive nurse behaviors regardless of unit, session, or group (F = 6.59, p = .002). Specifically, when nurses worked with patients sedated (i.e., negative RASS scores), they used more positive behaviors than when patients were calm and cooperative (t = 3.13, p = .002). When selecting among covariates using backward elimination, only sedation was retained in the final model.
Fig. 4.
Positive nurse communication behaviors (quality) by unit and phase.
The use of AAC modalities, an indicator of communication quality, was significantly different among groups (F = 6.14, p = .002). Use of AAC was extremely low, averaging only .84% in the Phase 1 group, and .51% in the Phase 2 intervention group, but 6.31% in the Phase 3 group, with a statistically significant difference between the Phase 2 and Phase 3 intervention groups (t 3.10, p = .002).
Communication ease
The percentage of sessions rated by patients as “difficult” accounted for approximately 27% of the Phase 1 group sessions, 31% of the Phase 2 group sessions, and 11% of the Phase 3 group sessions (F = 7.67, p < .01). Units also differed on this measure (F = 8.02, p < .01). Patients in unit B were more likely to report dif=ficulty when communicating (26.8%), relative to patients in unit A (19.3%). There was no interaction between the intervention and the unit effects. Delirium, as measured by the CAM-ICU, was the only covariate associated with communication ease. The phase and unit effects were maintained when considering all of the possible covariates.
Discussion
This is the first published study to test the efficacy of a comprehensive communication intervention with intubated ICU patients. We used micro-analysis of nurse–patient communication in the ICU beyond simple observer checklists of positive and negative behaviors used previously.34,36,42 Our hypotheses were partially supported. Both interventions showed positive effects on the process of nurse–patient communication in the ICU. Importantly, the intervention groups showed improvement in length of communication, and successfulness of communication about pain and other symptoms. This finding is most important to quality of care and patient safety in the ICU because misinterpretation of communication about pain and other symptoms can lead to over or under-treatment. Given that nurses in the usual care group (Phase 1) were generally older and more experienced than nurses in the intervention groups (Phases 2 and 3), our findings demonstrate that improvements can be made in communication skills beyond what comes with experience. Communication quality as measured by positive nurse behaviors improved differentially by intervention (Phase 2) and unit. The Phase 3 intervention added value across units in the use of AAC and multiple modalities of communication and in improvements to patient's perceptions about the ease of communication. Communication partner training can increase the likelihood and frequency of successful interactions with communication-impaired individuals.43,46,49,52,53 A randomized controlled trial evaluated the effect of a nurse training program that emphasized psychosocial caring behaviors such as attention, eye contact, touch, and treating the ICU patient as a person.42 In general, positive behaviors increased and negative behaviors decreased for both nurses and patients following nurse training (p ≤ .04). That training program, however, did not include content on AAC techniques or tools, and the measurement was not targeted specifically to intubated ICU patients.
Frequency
Our findings demonstrate an increase in number of acts per exchange, a measure of the density of communication between nurses and intubated ICU patients, in the intervention groups when compared with usual care controls. Sub-analysis showed increase in clarification acts. This may represent communication breakdowns with successful repairs or an increased conscientiousness on the part of nurses to achieve true understanding of patient messages. Clarification behaviors, such as repeating back and validation, were part of the nurse training program, thus an increase in clarification frequency may indicate skill acquisition as a result of training. The relationships between clarification behaviors and other communication outcomes, such as success and perceived ease of communication, are worthy of further exploration.
The proportion of patient initiated communication exchanges did not increase. Although initiation and independence in communication are hallmarks of successful AAC interventions,43 the nature of the provider–patient relationship in critical illness may preclude much shift. Clinician dominance is consistent with prior studies of communication in the ICU as well as studies of patient–provider communication in other settings.34–36,42 The first 3 min of the nurse–patient interaction, used here for consistency of measurement, may be more task-oriented, and therefore nurse controlled, than subsequent interactions or this may be typical of nurseepatient interaction in the ICU. It is important to note that there are no benchmarks or standards for communication frequency or the other communication outcome measures in the critical care setting. These study results may be helpful in building the evidence toward best communication practice.
Success
Successfulness of communication exchanges about pain and symptoms was significantly greater in the intervention groups compared to the usual care group. This finding has important implications for quality of care improvements. Anecdotes from the SLP, such as the case in which a patient received pain medicine for 2 weeks as a misinterpretation of his requests for pants, confirm the problems and potential for undiscovered errors when pain symptom communication is misunderstood. Our study brings to light the likelihood of misinterpretation of pain and symptom communication under usual care conditions. The use of visual pain tools and/or behavioral pain scales are recommended for intubated patients,54 but, were not part of standard practice in these ICUs at the time the study was conducted. Improved communication skills might, however, improve the utilization of these instruments. Future research will evaluate the impact of communication interventions on pain symptom management and other quality of care indicators.51,55
Quality
Positive communication behaviors showed some change but only in one ICU (Unit A) and only in the Phase 2 intervention group. Unit B nurses in the usual care group demonstrated a relatively high use of positive communication behaviors perhaps due to level of experience or intrinsic characteristics. The most interesting finding with respect to positive communication behaviors is that nurses used more positive behaviors when patients were delirious, or sedated. This finding indicates that nurses tried harder when patients had greater barriers to communication, specifically cognitive impairments. Finally, although the communication methods used by patients in this study are similar to those documented in previous research,19,34,35,56,57 AAC use improved in the Phase 3 intervention group with the guidance of a speech language pathologist (SLP). The use of multiple modalities with electronic AAC devices has been demonstrated in previous research and settings.19,21,24,58
Ease
Patients in Phase 3 who received the individualized SLP assessment and intervention perceived less difficulty with communication than patients in the usual care (Phase 1) or nurse communication skills training (Phase 2) intervention groups. This finding suggests that attention to communication care planning by a communication specialist can add value and ease the communication process for patients. SLPs are expert in communication disorders, AAC tools and devices. AAC consultation services provided by SLPs to acute and critical care units have been previously described,21,25,30,33,59–61 but are not yet standard care in ICUs nationwide. Importantly, these experts can conduct a thorough assessment of a patient's communication ability and match communication strategies and materials to the individual patient's abilities, needs and preferences. Consultation services can be recommended or required for patients at highest risk for communication difficulty, such as those with prolonged MV, upper extremity weakness or paralysis, and/or cognitive injury. Further analysis of the SLP intervention components in relation to communication outcomes and nurse–patient usage of AAC modalities beyond the first 3 min of interaction is warranted.
The intervention effects on communication frequency and quality were evident only in Unit A. The nurse participants in Unit A may have had a greater receptivity to the program content or a more facilitative work environment than Unit B nurses, however, the graphic displays (Figs. 3 and 4) show that the Phase 1 group of nurse–patient dyads in Unit B tested higher than Unit A dyads on both of these measures. The nurse and patient groups in each unit did not differ significantly by phase on any co-variate characteristics that might explain this different “start point” or skill level. Unit culture and work environments were not assessed in this study but should be part of future intervention implementation research.
This study is timely, particularly in the United States, given that new standards for hospital accreditation require identification of the patient's oral and written communication needs including “the need for personal devices such as hearing aids or glasses, language interpreters, communication boards, and translated or plain language materials”.62 Moreover, the application of new clinical practice guidelines for treating pain, agitation and delirium among adult patients in the ICU will likely result in mechanically ventilated patients in more awake and communicative states.63
Limitations
Our study was limited to two ICUs in a single hospital and may not reflect nurse–patient communication outcomes in other settings. Moreover, unit culture, attitudes, and environmental differences may have influenced communication interactions between nurses and nonvocal ICU patients. Random selection of nurses for study participation does, however, increase the potential generalizability of study results. Nurse sampling in each phase was complicated by a relatively high dropout rate (28.6%). Importantly, all but one of these dropouts was due to nurse movement out of the unit for relocation, job change, or to attend advanced practice education. This was costly in terms of study operations and limited the sampling pool. It is a real life factor worthy of careful consideration in future pragmatic clinical trials that involve nurses as participants engaged over a prolonged time period. Design features requiring two consecutive day shifts for nurse–patient dyad observation prolonged the length of time for participant accrual. Operational challenges included changes in nurse assignments, work absences, and changes in patient status, such as extubation, transfer, or deterioration.
Although a de-sensitizing, unrated video recording session was conducted with all patient–nurse dyads, the unavoidable visibility of the camera and recording team increased the likelihood that “best” behavior was observed. The study design assumes equal participant reactivity, and “best” performance, among the three groups. The collection of observation data from both morning and afternoon time periods during a shift of care is a strength in terms of generalizability, however, limiting to the first 3 min of the nurse–patient interaction may systematically exclude patient-driven communication from the data sample. Future studies should consider communication sampling using momentary event sampling or other techniques to improve representation of patient-driven communication in the dataset. The external rater was reviewed against a gold standard of dual raters, discussion, and arbitration. We did not separate the agreements/disagreements into calculations of false positives and false negatives, therefore specificity (true negative rate) and sensitivity (true positive rate) are unknown.
Additionally, these results must be considered within the context of the nurses’ level of experience. Although randomly selected, the nurses in the control group were experienced critical care nurses with 30% holding CCRN certification. Patients were representative of mixed cardiothoracic surgical and medical ICU populations; however, patients in the intervention groups had higher rates of delirium and longer periods of being nonvocal before study enrollment. These potential confounders were controlled in the analysis.
Conclusion
The SPEACS intervention showed positive effects, specifically, significant increases in length of communication exchanges, AAC use, and in success of communication about pain and other symptoms. Communication difficulty was reduced by the addition of SLP individualized assessment and AAC intervention. This study provides support for the feasibility and utility of a multi-level communication intervention consisting of communication skills training, materials and SLP consultation in the ICU. The findings provide preliminary evidence for efficacy of a training intervention.
Acknowledgments
The authors recognize with gratitude the following contributions: Brooke Paull Baumann, MS, SLP-CCC for clinical expertise as interventionist on the study; Michael Donahoe, MD for clinical support and critical care expertise; Leah Loyd, Kyle Castrovinci, PJ Tate, Carl Frey, Bryan Ghingold for videography and data collection; Lauren Fee, MS, SLP-CCC, and Karen Schmidt, PhD for data coding and reliability assessments; Vidatak for donation of a portion of the E-Z Talk™ Boards used in this study.
Disclosures: The SPEACS Basic Communication Skills Training intervention program is copyrighted to the University of Pittsburgh and Duquesne University, authors MB Happ, KL Garrett and JA Tate. Components of the program are available on http://www.pitt.edu/~speacs.
Funding: Funded by the National Institute of Child Health and Human Development (5R01-HD 043988). Additional support from the National Institute for Nursing Research (K24- NR010244).
References
- 1.Bergbom-Engberg I, Haljamae H. Assessment of patients’ experience of discomforts during respirator therapy. Crit Care Med. 1989;17(10):1068–1072. doi: 10.1097/00003246-198910000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Carroll SM. Nonvocal ventilated patients’ perceptions of being misunderstood. West J Nurs Res. 2004;26(85–103) doi: 10.1177/0193945903259462. [DOI] [PubMed] [Google Scholar]
- 3.Menzel LK. Factors related to the emotional responses of intubated patients to being unable to speak. Heart Lung. 1998;27(4):245–252. doi: 10.1016/s0147-9563(98)90036-x. [DOI] [PubMed] [Google Scholar]
- 4.Patak L, Gawlinski A, Fung NI, Doering L, Berg J. Patients’ reports of health care practitioner interventions that are related to communication during mechanical ventilation. Heart Lung. 2004;33:323–327. doi: 10.1016/j.hrtlng.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Rotondi AJ, Chelluri L, Sirio C, et al. Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Crit Care Med. 2002;30(4):746–752. doi: 10.1097/00003246-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Nelson J, Meier DE, Litke A, Natale DA, Siegel RE, Morrison SR. The symptom burden of critical illness. Crit Care Med. 2004;32:1527–1534. doi: 10.1097/01.ccm.0000129485.08835.5a. [DOI] [PubMed] [Google Scholar]
- 7.Nelson JE, Meier DE, Oei EJ, et al. Self-reported symptom experience of critically ill cancer patients receiving intensive care. Crit Care Med. 2001;29(2):277–282. doi: 10.1097/00003246-200102000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Pennock BE, Crawshaw L, Maher T, Price T, Kaplan PD. Distressful events in the ICU as perceived by patients recovering from coronary artery bypass surgery. Heart Lung. 1994;23:323–327. [PubMed] [Google Scholar]
- 9.Khalaila R, Zbidat W, Anwar K, Bayya A, Linton DM, Sviri S. Communication difficulties and psychoemotional distress in patients receiving mechanical ventilation. Am J Crit Care. 2011;20(6):470–479. doi: 10.4037/ajcc2011989. [DOI] [PubMed] [Google Scholar]
- 10.Alasad J, Ahmad M. Communication with critically ill patients. J Adv Nurs. 2005;50(4):356–362. doi: 10.1111/j.1365-2648.2005.03400.x. [DOI] [PubMed] [Google Scholar]
- 11.Leathart AJ. Communication and socialisation (2): perceptions of neophyte ITU nurses. Intensive Crit Care Nurs. 1994;10(2):142–154. doi: 10.1016/0964-3397(94)90011-6. [DOI] [PubMed] [Google Scholar]
- 12.Magnus VS, Turkington L. Communication interaction in ICUePatient and staff experiences and perceptions. Intensive Crit Care Nurs. 2006;22:167–180. doi: 10.1016/j.iccn.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 13.Bergbom-Engberg I, Haljamae H. The communication process with ventilator patients in the ICU as perceived by the nursing staff. Intensive Crit Care Nurs. 1993;9(1):40–47. doi: 10.1016/0964-3397(93)90008-l. [DOI] [PubMed] [Google Scholar]
- 14.Hemsley B, Sigafoos J, Balandin S, et al. Nursing the patient with severe communication impairment. J Adv Nurs. 2001;35:827–835. doi: 10.1046/j.1365-2648.2001.01920.x. [DOI] [PubMed] [Google Scholar]
- 15.Patak L, Wilson-Stronks A, Costello J, et al. Improving patient-provider communication: a call to action. J Nurs Adm. 2009;39(9):372–376. doi: 10.1097/NNA.0b013e3181b414ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Happ MB. Communicating with mechanically ventilated patients: state of the science. AACN Clin Issues. 2001;12(2):247–258. doi: 10.1097/00044067-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Stovsky B, Rudy E, Dragonette P. Comparison of two types of communication methods used after cardiac surgery with patients with endotracheal tubes. Heart Lung. 1988;17(3):281–289. [PubMed] [Google Scholar]
- 18.Etchels MC, MacAulay F, Judson A, et al. ICU-talk: the development of a computerized communication aid for patients in ICU. Care Crit Ill. 2003;19(1):4–9. [Google Scholar]
- 19.Happ MB, Roesch TK, Garrett K. Electronic voice-output communication aids for temporarily nonspeaking patients in a medical intensive care unit: a feasibility study. Heart Lung. 2004;33(2):92–101. doi: 10.1016/j.hrtlng.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 20.Miglietta MA, Bochicchio G, Scalea TM. Computer-assisted communication for critically ill patients: a pilot study. J Trauma. 2004;57(3):488–493. doi: 10.1097/01.ta.0000141025.67192.d9. [DOI] [PubMed] [Google Scholar]
- 21.Dowden P, Beukelman D, Lossing C. Serving nonspeaking patients in acute care settings: intervention outcomes. AAC. 1986;2:38–44. [Google Scholar]
- 22.MacAulay F, Judson A, Etchels M, et al. ICU-talk, a communication aid for intubated intensive care patients. Assets ’02: Proceedings of the Fifth International ACM Conference on Assistive Technologies. 2002:226–230. [Google Scholar]
- 23.Fowler SB. Impaired verbal communication during short-term oral intubation. Nurs Diagn. 1997;8(3):93–98. doi: 10.1111/j.1744-618x.1997.tb00317.x. [DOI] [PubMed] [Google Scholar]
- 24.Happ MB, Roesch TK, Kagan SH. Patient communication following head and neck cancer surgery: a pilot study using electronic speech-generating devices. Oncol Nurs Forum. 2005;32(6):1179–1187. doi: 10.1188/05.ONF.1179-1187. [DOI] [PubMed] [Google Scholar]
- 25.Happ MB, Sereika SM, Garrett KL, Tate JA. Use of quasi-experimental sequential cohort design in the Study of Patient-Nurse Effectiveness with Assisted Communication Strategies (SPEACS). Contemp Clin Trials. 2008;29:801–808. doi: 10.1016/j.cct.2008.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Happ MB, Sereika S, Garrett K, et al. Nurse-patient communication interactions in the ICU. Am J Crit Care. 2011;20(2):e28–40. doi: 10.4037/ajcc2011433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Broyles LM, Tate JA, Happ MB. Use of augmentative and alternative communication by family members in the ICU. Am J Crit Care. 2012;21(2):e21–32. doi: 10.4037/ajcc2012752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nilsen M, Serika S, Happ MB. Nurse and patient characteristics associated with duration of nurse talk during patient encounters in ICU. Heart and Lung. 2012;42(1):5–12. doi: 10.1016/j.hrtlng.2012.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American Speech-Language-Hearing Association . National Outcomes Measurement System (NOMS): Functional Communication Measure for Adults. American Speech-Language-Hearing Association; Rockville: 1998. [Google Scholar]
- 30.Beukelman DR, Garrett KL, Yorkston KM. Augmentative Communication Strategies for Adults With Acute or Chronic Medical Conditions. Paul H. Brookes Publishing Co; Baltimore: 2007. [Google Scholar]
- 31.Koloroutis M. Relationship Based Care. Minneapolis: Creative Health Care Management. 2004 [Google Scholar]
- 32.Garrett K, Happ MB, Costello J, Fried-Oken M. AAC in intensive care units. In: Buekelman DR, Garrett K, Yorkston KM, editors. Augmentative Communication Strategies for Adults With Acute or Chronic Medical Conditions. Brookes Publishing Company; Baltimore, MD: 2007. [Google Scholar]
- 33.Radtke JV, Baumann BM, Garrett KL, Happ MB. Listening to the voiceless patient: Case reports in assisted communication in the ICU. J Palliat Care Med. 2011;14(6):791–795. doi: 10.1089/jpm.2010.0313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Salyer J, Stuart BJ. Nurse-patient interaction in the intensive care unit. Heart Lung. 1985;14(1):20–24. [PubMed] [Google Scholar]
- 35.Ashworth P. Care to Communicate: An Investigation Into Problems of Communication Between Patients and Nurses in Intensive Therapy Units. White-friars Press; London: 1980. [Google Scholar]
- 36.Hall DS. Interactions between nurses and patients on ventilators. Am J Crit Care. 1996;5(4):293–297. [PubMed] [Google Scholar]
- 37.Knaus WA, Wagner DP, Draper EA, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–1636. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- 38.Wagner DP, Knaus WA, Harrell FE, Zimmerman JE, Watts C. Daily prognostic estimates for critically ill adults in intensive care units: results from a prospective, multicenter, inception cohort analysis. Crit Care Med. 1994;22(9):1359–1372. doi: 10.1097/00003246-199409000-00004. [DOI] [PubMed] [Google Scholar]
- 39.Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286(21):2703–2710. doi: 10.1001/jama.286.21.2703. [DOI] [PubMed] [Google Scholar]
- 40.Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond agitation-sedation scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166(10):1338–1344. doi: 10.1164/rccm.2107138. [DOI] [PubMed] [Google Scholar]
- 41.Ely EW, Truman B, Shintani A, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond agitation-sedation scale (RASS). JAMA. 2003;289(22):2983–2991. doi: 10.1001/jama.289.22.2983. [DOI] [PubMed] [Google Scholar]
- 42.de los Rios Castillo JL, Sanchez Sosa JJ. Well-being and medical recovery in the critical care unit: the role of the nurse-patient interaction. Salud Mental. 2002;25(2):21–31. [Google Scholar]
- 43.Light J, Dattilo J, English J, Gutierrez L, Hartz J. Instructing facilitators to support the communication of people who use augmentative communication systems. J Speech Hear Res. 1992;35(4):865–875. doi: 10.1044/jshr.3504.865. [DOI] [PubMed] [Google Scholar]
- 44.Garrett K, Beukelman D. Changes in the interaction patterns of an individual with severe aphasia given three types of partner support. Clin Aphasiol. 1995;23:203–234. [Google Scholar]
- 45.Garrett KL, Huth C. The impact of graphic contextual information and instruction on the conversational behaviours of a person with severe aphasia. Aphasiology. 2002;16(4–6):523–536. [Google Scholar]
- 46.Calculator S, Luchko CD. Evaluating the effectiveness of a communication board training program. J Speech Hear Disord. 1983;48(2):185–191. doi: 10.1044/jshd.4802.185. [DOI] [PubMed] [Google Scholar]
- 47.Morse J, Beres MA, Spiers JA, Mayan M, Olson K. Identifying signals of suffering by linking verbal and facial cues. Qual Health Res. 2003;13(8):1063–1077. doi: 10.1177/1049732303256401. [DOI] [PubMed] [Google Scholar]
- 48.Topf M. Three estimates of inter-rater reliability for nominal data. Nurse Res. 1986;35:253–255. doi: 10.1097/00006199-198607000-00020. [DOI] [PubMed] [Google Scholar]
- 49.Burgio LD, Allen-Burge R, Roth DL, et al. Come talk with me: improving communication between nursing assistants and nursing home residents during care routines. Gerontologist. 2001;41(4):449–460. doi: 10.1093/geront/41.4.449. [DOI] [PubMed] [Google Scholar]
- 50.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 51.Happ MB, Sereika S, Garrett KL, et al. Study of Patient-Nurse Effectiveness with Assisted Communication Strategies (SPEACS) in the ICU. Am J Resp Crit Care Med. 2010;181:A4018. doi: 10.1016/j.cct.2008.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McCallion P, Toseland RW, Lacey D, Banks S. Educating nursing assistants to communicate more effectively with nursing home residents with dementia. Gerontologist. 1999;39(5):546–558. doi: 10.1093/geront/39.5.546. [DOI] [PubMed] [Google Scholar]
- 53.Buckwalter KC, Cusack D, Beaver M, Sidles E, Wadle K. The behavioral consequences of a communication intervention on institutionalized residents with aphasia and dysarthria. Arch Psychiatr Nurs. 1988;2(5):289–295. [PubMed] [Google Scholar]
- 54.Tate JA, Seaman JB, Happ MB. Overcoming barriers to pain assessment: communicating pain information with intubated older adults. Geriatr Nurs. 2012;33(4):310–313. doi: 10.1016/j.gerinurse.2012.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Arslanian-Engoren C, Scott LD. The lived experience of survivors of prolonged mechanical ventilation: a phenomenological study. Heart Lung. 2003;32(5):328–334. doi: 10.1016/s0147-9563(03)00043-8. [DOI] [PubMed] [Google Scholar]
- 56.Wojnicki-Johansson G. Communication between nurse and patient during ventilator treatment: patient reports and RN evaluations. Intensive Crit Care Nurs. 2001;17(1):29–39. doi: 10.1054/iccn.2000.1547. [DOI] [PubMed] [Google Scholar]
- 57.Leathart AJ. Communication and socialisation (1): an exploratory study and explanation for nurse-patient communication in an ITU. Intensive Crit Care Nurs. 1994;10(2):93–104. doi: 10.1016/0964-3397(94)90004-3. [DOI] [PubMed] [Google Scholar]
- 58.Fried-Oken M, Howard JM, Stewart SR. Feedback on AAC intervention from adults who are temporarily unable to speak. AAC. 1991;7:43–50. [Google Scholar]
- 59.Costello JM. AAC intervention in the intensive care unit: the Children’s Hospital Boston Model. AAC. 2000;16:137–153. [Google Scholar]
- 60.Fox L, Rau M. Augmentative and alternative communication for adults following glossectomy and laryngectomy surgery. AAC. 2001;17:161–166. [Google Scholar]
- 61.Hurtig R, Downey D. Augmentative and Alternative Communication in Acute and Critical Care Settings. Plural Publishing; 2008. [Google Scholar]
- 62.The Joint Commission. Advancing Effective Communication, Cultural Competence, and Patient- and Family-Centered Care: A Roadmap for Hospitals. 2010 Available from: http://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf.
- 63.Barr J, Fraser GL, Puntillo GL, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the ICU. CCM. 2013;41:263–306. doi: 10.1097/CCM.0b013e3182783b72. [DOI] [PubMed] [Google Scholar]