Abstract
Objectives:
This study evaluated the in vitro shear bond strength (SBS) of a resin-based pit-and-fissure sealant (Fluroshield [F], Dentsply/Caulk) associated with either an etch-and-rinse (Adper Single Bond 2 [SB], 3M/ESPE) or a two-step self-etch adhesive system (Adper SE Plus [SE], 3M/ESPE) on Er: YAG laser-irradiated enamel.
Materials and Methods:
Seventeen sound third molar crowns were embedded in acrylic resin, and the mesial–distal enamel surfaces were flattened. The enamel sites were irradiated with a 2.94-μm wavelength Er: YAG laser (120 mJ, 4 Hz, noncontact mode/17 mm, 20 s). The specimens were randomly assigned to three groups according to the bonding technique: I - 37% phosphoric acid etching + SB + F; II - SE + F and III - F applied to acid-etched enamel, without an intermediate layer of bonding agent. In all of the groups, a 3-mm diameter enamel-bonding site was demarcated and the sealant cylinders were bonded. After 24 hours in distilled water, the shear bond strength was tested at a crosshead speed of 0.5 mm/minute. The data were analyzed by one-way ANOVA and Tukey's test. The debonded specimens were examined with a stereomicroscope to assess the failure modes.
Results:
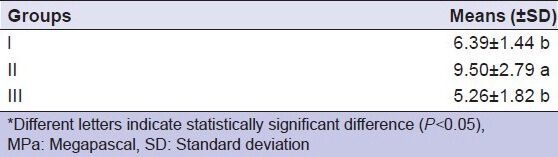
The mean SBS values in MPa were I = 6.39 (±1.44); II = 9.50 (±2.79); and III = 5.26 (±1.82). No statistically significant differences were observed between groups I and III; SE/F presented a significantly higher SBS than that of the other groups (P = 0.001). With regard to the failure mode, groups I (65%) and II (75%) presented adhesive failures, while group III showed 50% adhesive failure. Cohesive failure did not occur.
Conclusion:
The application of the two-step self-etch bonding agent (Adper SE Plus) beneath the resin pit-and-fissure sealant placement resulted in a significantly higher bond strength for the Er:YAG laser-irradiated enamel.
Keywords: Adhesive system, Er:YAG laser, pit and fissure sealant, shear bond strength
INTRODUCTION
On account of the morphological complexity of the occlusal pits and fissures, these surfaces are highly susceptible to caries. Therefore, more effective measures are necessary, such as, the application of occlusal sealants.[1] Sealant retention is essentially a micromechanical process established by the infiltration of the sealant into the microporous network on the enamel surface, and good marginal adaptation enables sealing and minimizes microleakage.[2]
The most caries-susceptible period is soon after tooth eruption, because newly erupted teeth are far less mineralized and hence, are more susceptible to acid attacks. Paradoxically, the possibility of failure increases for sealants placed shortly after tooth eruption, when the distal marginal ridge has just cleared the soft tissue, leaving the occlusal surface at risk for moisture and salivary contamination during the sealing procedure.[3,4] Based on this risk, the low utilization of sealants has been attributed to lack of confidence in their bonding to the enamel and to the difficulty in their achieving adequate dry field isolation.[5]
Total etching in the range of 30-40% phosphoric acid is the standard method for treating enamel surfaces with sealant. Complete penetration of the etchant into the fissures should occur for good retention of the sealant to the enamel. However, in a previous study,[6] none of the tested materials were able to penetrate into a fissure model.
In an effort to improve sealant success, many preparations and cleaning techniques have been described that are used on the tooth surface before sealant application.[7] The advantages of adding a bonding agent layer between the etched enamel and the sealant to increase retention have been demonstrated in cases of moisture and salivary contamination.[8,9,10] Some authors have found that the use of bonding agents beneath sealants placed on saliva-contaminated enamel can reduce microleakage,[11] enhance resin flow into the fissures, and improve short-term clinical success.[8,9]
Additionally, several invasive and noninvasive techniques, such as enameloplasty, air polishing, and laser treatment, can be used for effective placement, and to increase the long-term retention capacity of resin-based fissure sealants.[12,13]
The use of Er:YAG laser irradiation for dental applications has become increasingly widespread, and its employment as an alternative technique for pretreatment and surface conditioning in pit-and-fissure sealing has been under discussion.[14,15,16] The Er:YAG laser removes enamel via a thermomechanical ablation process. This process successfully occurs due to the Er:YAG laser's wavelength of 2.94 μm, which is close to the absorption spectrum of water and the OH- groups in hydroxyapatite.[17,18] As the lased substrate is not completely vaporized, but is only disintegrated into fragments, most of the incident radiation is consumed in the ablation process. This process leaves very little residual energy for adverse thermal interactions with the pulp and surrounding tissues.[17,19]
With regard to the lack of published research analyzing the interactions among pit-and-fissure sealants, bonding agents, and dental substrates treated by the erbium-yttrium-aluminum-garnet laser and the effects of Er:YAG laser irradiation on adhesion, the aim of the present study was to evaluate in vitro, the shear bond strength (SBS) of a resin-based pit-and-fissure sealant associated with different dental bonding systems and Er:YAG laser-irradiated enamel. The null hypothesis tested was that the application of an adhesive system beneath the sealant would not result in a higher bond strength for the Er:YAG laser-irradiated enamel.
MATERIALS AND METHODS
This study was approved by the Research Ethics Committee of Ribeirão Preto Dental School, University of São Paulo. Freshly extracted, sound, human third molars were hand-scaled and cleaned with water/pumice slurry and rotating bristle brushes to remove calculus and surface-adhered debris. The teeth were examined under a ×20 magnifier to discard those teeth with structural defects. Seventeen teeth were selected for the study and were stored in 0.9% saline, with 0.4% sodium azide at 4°C. Prior to use, the teeth were washed thoroughly in running water to eliminate the remaining traces of the storage solution, the roots were removed 3 mm below the cementoenamel junction, and the crowns were embedded in polyester resin, using polyvinyl chloride rings (2.1 cm in diameter and 1.1 cm in height). After resin polymerization, the rings were discarded, and the mesial and distal enamel surfaces (n = 33) were ground and polished while wet with #600-grit silicon carbide (SiC) papers (Buehler Ltd., Lake Bluff, IL, USA) in a low-speed polishing machine (Politriz DP-9U2; Struers, A/S, Copenhagen, Denmark), to obtain flat, smooth test surfaces that were cleaned by rubber cup/pumice prophylaxis for 10 seconds. For standardization, the bonding sites were demarcated by attaching a piece of insulating tape with a 3-mm diameter central hole on each surface.
Er:YAG laser irradiation was performed with a 2.94-μm wavelength Er:YAG laser, using 120 mJ of pulse energy and a 4-Hz repetition rate. The Er:YAG laser device used was the Kavo Key Laser 2 model (Kavo Dental GmbH and Co, Biberach, Germany). The laser beam (spot size = 0.63 mm) was delivered in a non-contact and defocused mode, with a fine water mist at 1.5 mL/minute for 20 seconds.[19] A 2051 hand piece was attached to the flexible fiber delivery system. The irradiation distance was standardized using a custom-made apparatus consisting of a holder, which positioned the hand piece in such a way that the laser beam was delivered perpendicular to the specimen surface at a constant working distance of 17 mm from the target site and a semi-adjustable base, to which the specimen was fixed with wax. One previously trained operator handled the micrometer screws of the apparatus in such a way that the semi-adjustable base of the specimen was alternately moved in right-to-left and forward-to-backward directions, thereby allowing the laser beam to provide accurate irradiation of the entire enamel site.
After laser irradiation, the specimens were randomly assigned to three groups (n = 11) according to the bonding/curing protocol adopted. The following materials were tested under different experimental conditions: A filled resin-based pit-and-fissure sealant (Fluroshield [F], Dentsply/Caulk, Milford, DE, USA), a single-bottle etch-and-rinse adhesive system (AdperSingle Bond 2 [SB], 3M/ESPE, St. Paul, MN, USA), and a self-etching adhesive system (Adper SE Plus [SE], 3M/ESPE, St. Paul, MN, USA). All the materials were used according to manufacturer's instructions.
In Group I, the enamel surface was etched with a 35% phosphoric acid gel (Scotchbond etchant, 3M/ESPE) for 15 seconds, rinsed thoroughly for 15 seconds, and dried with a mild, oil-free air stream to obtain a uniformly white, dull, chalk-like appearance. Then Adper Single Bond 2 was applied to the enamel bonding site in a uniform layer, slightly thinned with a mild, oil-free air stream, and light-cured for 10 seconds with a visible light curing unit (XL 3000; 3M/ESPE) with a 450 mW/cm2 output of power. Next, Fluroshield sealant was applied and light-cured for 20 seconds. In Group II, Adper SE Plus was applied to the bonding site by first treating the enamel with Liquid A so that a continuous, red-colored layer appeared on the surface. Liquid B was then applied and scrubbed into the surface of the bonding area for 20 seconds. The red-colored components had been activated. After the treated enamel surface was air-dried thoroughly for 10 seconds, to evaporate the water, a second coat of Liquid B was applied, lightly air-thinned, and light-cured for 10 seconds. Next, the Fluroshield sealant was applied and light-cured for 20 seconds. In Group III (the control group), the enamel surface was etched with a 35% phosphoric acid gel (Scotchbond etchant, 3M/ESPE) for 15 seconds, rinsed thoroughly for 15 seconds, and dried with a mild, oil-free air stream, to obtain a uniformly white, dull, chalk-like appearance, and then Fluroshield was applied.
In all of the groups, the adhesive systems and the sealant were carefully applied onto the delimited enamel surface with disposable microbrush tips (Microbrush Corporation, Orlando, FL, USA) to avoid excess and pooling of material along the edges of the insulating tape, which could compromise tension distribution during the test, and hence, the validity of the results. Once the bonding protocols were completed, the specimens were individually fixed in a metallic clamping device that secured the test enamel surface parallel to a flat base. A split bisected polytetrafluoroethylene jig was positioned on the tooth/sealant block, providing a cylindrical cavity 4 mm in height and 3 mm in diameter that was coincident with the demarcated enamel bonding site. The sealant was inserted into the jig in two increments, with each one polymerized for 20 seconds. As the cavity was completely filled, the specimen was removed from the clamping device, and the jig was opened and separated, leaving a sealant cylinder (4 mm × 3 mm) adhering to the enamel surface [Figure 1].
Figure 1a-f.
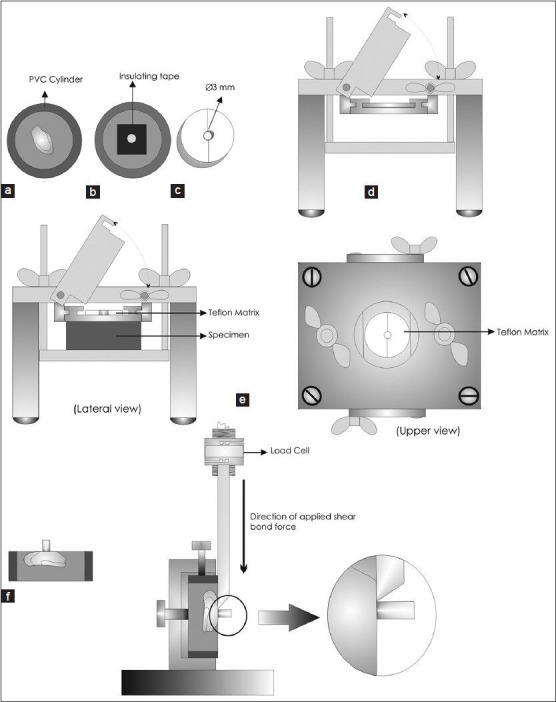
Diagram of the study mechanism
After 24 hours of storage in distilled water at 37°C, SBS was tested to failure using a knife blade in a universal testing machine (Model MEM 2000, EMIC Ltda, São José dos Pinhais, PR, Brazil) running at a crosshead speed of 0.5 mm/minute, with a 50-kgf load cell. The mean SBS in MPa and the standard deviation were calculated, and the data were analyzed statistically by one-way ANOVA. Tukey's exact test was used for multiple comparisons at a 5% significance level. The debonded specimens were observed with a 40 × stereomicroscope, to assess the failure modes, which were classified as adhesive, cohesive, or mixed. All the examinations (two per specimen) were performed by a single examiner blinded to the groups to which the specimens belonged. The Kappa value was 0.90.
RESULTS
The mean SBS and standard deviations are presented in Table 1. The sealant technique with the two-step self-etch adhesive system showed a statistically higher mean shear bond strength of the lased enamel than the techniques used in the other groups. No statistically significant differences were found between groups I and III (P = 0.001).
Table 1.
Shear bond strength (MPa), means, and standard deviations in each of the experimental groups
The failure patterns on the debonded surfaces showed that most specimens in groups I (65%) and II (75%) presented adhesive failures between the dental substrate and the adhesive layer. Group III showed 50% adhesive failure. Cohesive failure did not occur.
DISCUSSION
Over the last few decades, the application of a bonding agent beneath the sealant has been widely suggested to improve adhesion to acid-etched enamel, because the hydrophilic monomers present in the contemporary bonding agents increase surface wetting and resin penetration.[3,5,8] Accordingly, the results of the present study have revealed that the application of an intermediate bonding agent layer prior to sealant placement in lased enamel surfaces increases the SBS, which is significantly higher in the group that received a layer of the self-etching adhesive system.
Baygin et al.[15] reported that Er, Cr: YSGG laser-treated groups (both at 20 and 40 Hz) were found to be similar to an acid-etched group prior to placement of a resin-based fissure sealant, and no smear layers, melting, or carbonization was seen. Additionally, Shahabi et al.[16] demonstrated that samples conditioned only by phosphoric acid showed the highest tensile bond strength values, statistically similar to samples conditioned by the Er:YAG laser followed by acid etching before sealant application. In contrast, Lepri et al.[14] observed that the Er:YAG laser was not able to increase the effectiveness of the conventional acid etching of enamel in the bonding of sealants under both dry and wet conditions. Despite the well-known cutting efficacy of the Er:YAG laser, it has been demonstrated that laser irradiation does not eliminate the need for acid-etching to achieve clinically adequate sealant retention.[16,20,21] Therefore, in the present study, laser irradiation was followed by phosphoric acid etching, except for Group II, in which a self-etching system was used (Adper SE Plus).
Self-etching adhesives were recently introduced to simplify bonding procedures and reduce technique sensitivity.[22] The risks of over-etching, over-wetting, and over-drying of tooth substrates are thus avoided. However, there is no consensus in the literature regarding the use of self-etching adhesives on enamel.[23,24]
Studies have shown that the adhesion of self-etching adhesive systems to pit-and-fissure sealants is less effective than the use of etch-and-rinse adhesive systems,[25,26] while other studies have reported good results for this association.[9,23,27] Gomes-Silva et al.[28] demonstrated that the association of the Clearfil S3 Bond self-etching adhesive system with Fluoroshield sealant resulted in a significantly increased bond strength compared to the use of the Single Bond etch-and-rinse adhesive system, with saliva-contaminated acid-etched enamel. In a previous study evaluating a two-year clinical success, Feigal and Quelhas[9] concluded that a self-etching adhesive is effective in bonding the sealant to the enamel, and that the simplified protocol reduced the treatment time and complexity, which is a great advantage in pediatric dentistry. Thus, in light of the existence of several articles in the literature concerning sealant techniques and their associations with adhesive systems, in the current study, there were no groups that did not undergo the laser procedure.
Esteves-Oliveira et al.[29] have observed enamel surfaces treated with Er:YAG and Er, Cr:YSGG lasers, showing the absence of a smear layer, and they found more roughness, a microretentive pattern, and prism exposure. Some studies have suggested that even some of the more aggressive versions of self-etching primers fail to etch through clinically significantly thick smear layers or unground aprismatic enamel, resulting in decreased bond strength.[30] Thus, self-etching adhesive systems may present clinically acceptable retention rates associated with a surface preparation method that creates a thin, or even no smear layer. Therefore, micromechanical retention resulting from this association may contribute to the deep penetration of the sealant into the microporous network and may explain the results of the current investigation.
In this context, some authors[31] who analyzed the bond strength of self-etching systems after Er:YAG irradiation or diamond burr cutting have found a similar bonding to enamel, while other authors[29] have reported that Er:YAG laser irradiation produces a lower mean bond strength than that of burr-prepared enamel surfaces when they are used with Clearfill SE Bond. Nevertheless, to our knowledge, no studies have yet evaluated the interaction of lased substrates with adhesive systems and a sealant technique.
Over-etching of tooth tissues can occur as a negative outcome of etch-and-rinse adhesive system techniques, which leave the surfaces more permeable and prone to acid attacks, especially if the demineralized substrates are not completely filled with adhesive resins.[32] In contrast, the Er:YAG laser irradiation of hard dental tissue modifies the calcium-to-phosphorus ratio, reduces the carbonate-to-phosphate ratio, and leads to the formation of more stable and less acid-soluble compounds, thus reducing susceptibility to acid attacks and caries.[33,34,35] Moreover, the microablative process causes vaporization of water and dental organic components, promoting the microexplosive destruction of inorganic substances. It is also thought to have an antibacterial effect by trapping free ions and forming remineralization microspaces.[33,36,37]
In light of the above considerations, a suitable explanation for the better performance of the self-etching adhesive system in the current study relies on the over-etching surface caused by the etch-and-rinse technique and on the absence of a smear layer on the laser irradiated enamel surface.
With regard to the types of failures observed in the fractured specimens, adhesive or mixed failure patterns were predominantly observed in these groups. A predominance of adhesive and mixed failures for lased specimens was also reported by Shahabi et al.[16]
Further research is required to determine the best sealant technique protocol for laser-prepared enamel and to support the development of materials that are able to interact properly with this substrate. The long-term implications of this interaction on the longevity of adhesion should also be investigated. From the standpoint of time-saving, lowered complexity of treatment, and patient management, the association of sealants with new self-etching adhesive systems and laser techniques has a significant advantage over the traditional method and over the association with etch-and-rinse adhesives, and these advantages should not be overlooked by modern restorative dentistry. The present in vitro study assessed the shear bond strength of self-etching and total-etch adhesive systems to Er:YAG laser-irradiated enamel. The lack of studies testing the same methodology, technology, and materials was a hindrance to an effective comparison between the results this study and other studies.
CONCLUSIONS
Based on the results reported here and within the limitations of an in vitro investigation, it can be concluded that the application of the two-step self-etch bonding agent (Adper SE Plus), beneath the resin pit-and-fissure sealant placement, resulted in a significantly higher bond strength for Er:YAG laser-irradiated enamel compared to the etch-and-rinse system.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Shaw L. Modern thoughts on fissure sealants. Dent Update. 2000;27:370–4. doi: 10.12968/denu.2000.27.8.370. [DOI] [PubMed] [Google Scholar]
- 2.Jensen OE, Handelman SL. Effect of an autopolymerizing sealant on viability of microflora in occlusal dental caries. Scand J Dent Res. 1980;88:382–8. doi: 10.1111/j.1600-0722.1980.tb01243.x. [DOI] [PubMed] [Google Scholar]
- 3.Simonsen RJ. Pit and fissure sealant: Review of the literature. Pediatr Dent. 2002;24:393–414. [PubMed] [Google Scholar]
- 4.Feigal RJ. The use of pit and fissure sealants. Pediatr Dent. 2002;24:415–22. [PubMed] [Google Scholar]
- 5.Feigal RJ, Hitt J, Splieth C. Retaining sealant on salivary contaminated enamel. J Am Dent Assoc. 1993;124:88–97. doi: 10.14219/jada.archive.1993.0069. [DOI] [PubMed] [Google Scholar]
- 6.Bottenberg P, Graber HG, Lampert F. Penetration of etching agents and its influence on sealer penetration into fissures in vitro. Dent Mater. 1996;12:96–102. doi: 10.1016/S0109-5641(96)80075-3. [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Godoy F, Gwinnett AJ. An SEM study of fissure surfaces conditioned with a scraping technique. Clin Prev Dent. 1987;9:9–13. [PubMed] [Google Scholar]
- 8.Feigal RJ, Musherure P, Gillespie B, Levy-Polack M, Quelhas I, Hebling J. Improved sealant retention with bonding agents: A clinical study of two-bottle and single-bottle systems. J Dent Res. 2000;79:1850–6. doi: 10.1177/00220345000790110601. [DOI] [PubMed] [Google Scholar]
- 9.Feigal RJ, Quelhas I. Clinical trial of a self-etching adhesive for sealant application: Success at 24 months with Prompt L Pop. Am J Dent. 2003;16:249–51. [PubMed] [Google Scholar]
- 10.Torres CP, Balbo P, Gomes-Silva JM, Ramos RP, Palma-Dibb RG, Borsatto MC. Effect of individual or simultaneous curing on sealant bond strength. J Dent Child. 2005;72:31–5. [PubMed] [Google Scholar]
- 11.Borsatto MC, Corona SA, Alves AG, Chimello DT, Catirse AB, Palma-Dibb RG. Influence of salivary contamination on marginal microleakage of pit and fissure sealants. Am J Dent. 2004;17:365–7. [PubMed] [Google Scholar]
- 12.Beauchamp J, Caufield PW, Crall JJ, Donly KJ, Feigal R, Gooch B, et al. Evidence-based clinical recommendations for the use of pit-andfissure sealants: A report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2008;139:257–68. doi: 10.14219/jada.archive.2008.0155. [DOI] [PubMed] [Google Scholar]
- 13.Kramer N, García-Godoy F, Lohbauer U, Schneider K, Assmann I, Frankenberger R. Preparation for invasive pit and fissure sealing: Air-abrasion or bur? Am J Dent. 2008;21:383–7. [PubMed] [Google Scholar]
- 14.Lepri TP, Souza-Gabriel AE, Atoui JA, Palma-Dibb RG, Pecora JD, Corona SA. Shear bond strength of a sealant to contaminated-enamel surface: Influence of erbium: Yttrium-aluminum-garnet laser pretreatment. J Esthet Restor Dent. 2008;20:386–94. doi: 10.1111/j.1708-8240.2008.00214.x. [DOI] [PubMed] [Google Scholar]
- 15.Baygin O, Korkmaz FM, Tuzuner T, Tanriver M. The effect of different enamel surface treatments on the microleakage of fissure sealants. Laser Med Sci. 2012;27:153–60. doi: 10.1007/s10103-011-0918-x. [DOI] [PubMed] [Google Scholar]
- 16.Shahabi S, Bagheri HG, Ramazani K. Tensile bond strength of sealants following Er:YAG laser etching compared to acid etching in permanent teeth. Laser Med Sci. 2012;27:371–5. doi: 10.1007/s10103-010-0869-7. [DOI] [PubMed] [Google Scholar]
- 17.Hibst R, Keller U. Experimental studies of the application of the Er:YAG laser on dental hard substances: I. Measurement of the ablation rate. Lasers Surg Med. 1989;9:338–44. doi: 10.1002/lsm.1900090405. [DOI] [PubMed] [Google Scholar]
- 18.Hibst R, Keller U. The mechanism of Er: YAG laser induced ablation of dental hard substances. Proc Soc Photo Opt Instrum Eng. 1993;1880:156–62. [Google Scholar]
- 19.Li ZZ, Code JE, Van de Merwe WP. Er: YAG laser ablation of enamel and dentin of human teeth: Determination of ablation rates at various fluences and pulse repetition rates. Lasers Surg Med. 1992;12:625–30. doi: 10.1002/lsm.1900120610. [DOI] [PubMed] [Google Scholar]
- 20.Lupi_Pegurier L, Marie-France B, Genovese O, Rocca JP, Muller-Bolla M. Microleakage of resin-based sealants after Er:YAG laser conditioning. Lasers Med Sci. 2007;22:183–8. doi: 10.1007/s10103-006-0437-3. [DOI] [PubMed] [Google Scholar]
- 21.Borsatto MC, Corona SA, Araújo FP, Souza-Gabriel AE, Pecora JD, Palma-Dibb RG. Effect of Er:YAG laser on tensile bond strength of sealants in primary teeth. J Dent Child. 2007;74:104–8. [PubMed] [Google Scholar]
- 22.Perdigão J, Lopes M. Effect of conditioner and restorative resin on enamel bond strengths. Am J Dent. 2000;13:88–92. [PubMed] [Google Scholar]
- 23.Perdigão J, Carmo AR, Anauate-Neto C, Amore R, Lewgoy HR, Cordeiro HJ, et al. Clinical performance of a selfetching adhesive at 18 months. Am J Dent. 2005;18:135–40. [PubMed] [Google Scholar]
- 24.Marquezan M, da Silveira BL, Burnett LH, Jr, Rodrigues CR, Kramer PF. Microtensile bond strength of contemporary adhesives to primary enamel and dentin. Clin Pediatr Dent. 2008;32:127–32. doi: 10.17796/jcpd.32.2.l512r1p807w54582. [DOI] [PubMed] [Google Scholar]
- 25.Venker DJ, Kuthy RA, Qian F, Kanellis MJJ. Twelve-month sealant retention in a school-based program using self-etching primer/adhesive. Public Health Dent. 2004;64:191–7. doi: 10.1111/j.1752-7325.2004.tb02752.x. [DOI] [PubMed] [Google Scholar]
- 26.Hannig M, Grafe A, Atalay S, Bott B. Microleakage and SEM evaluation of fissure sealants by use of self-etching priming agents. J Dent. 2004;32:75–81. doi: 10.1016/j.jdent.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 27.Al-Sarheed MA. Evaluation of shear bond strength and SEM observation of all-in one self-etching primer used for bonding of fissure sealants. J Contemp Dent Pract. 2006;7:9–16. [PubMed] [Google Scholar]
- 28.Gomes-Silva JM, Torres CP, Contente MM, Oliveira MA, Palma-Dibb RG, Borsatto MC. Bond strength of a pit-and-fissure sealant associated to etch-and-rinse and self-etching adhesive systems to saliva-contaminated enamel: Individual vs. simultaneous light curing. Braz Dent J. 2008;19:341–7. doi: 10.1590/s0103-64402008000400010. [DOI] [PubMed] [Google Scholar]
- 29.Esteves-Oliveira M, Zezell DM, Apel C, Turbino ML, Aranha AC, Eduardo CP, et al. Bond strength of self-etching primer to bur cut, Er, Cr:YSGG, and Er:YAG lased dental surfaces. Photomed Laser Surg. 2007;25:373–80. doi: 10.1089/pho.2007.2044. [DOI] [PubMed] [Google Scholar]
- 30.Van Landuyt KL, Kanumilli P, De Munck J, Peumans M, Lambrechts P, Van Meerbeek B. Bond strength of a mild self-etch adhesive with and without prior acid-etching. J Dent. 2006;34:77–85. doi: 10.1016/j.jdent.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 31.De Munck J, Van Meerbeek B, Yudhira R, Lambrechts P, Vanherle G. Micro-tensile bond strength of two adhesives to Erbium: YAG-lased vs. bur-cut enamel and dentin. Eur J Oral Sci. 2002;110:322–9. doi: 10.1034/j.1600-0722.2002.21281.x. [DOI] [PubMed] [Google Scholar]
- 32.Chimello-Sousa DT, de Souza AE, Chinelatti MA, Pecora JD, Palma-Dibb RG, Milori Corona SA. Influence of Er:YAG laser irradiation distance on the bond strength of a restorative system to enamel. J Dent. 2006;34:245–51. doi: 10.1016/j.jdent.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 33.Castellan CS, Luiz AC, Bezinelli LM, Lopes RM, Mendes FM, Eduardo CP, et al. In vitro evaluation of enamel demineralization after Er:YAG and Nd:YAG laser irradiation on primary teeth. Photomed Laser Surg. 2007;25:85–90. doi: 10.1089/pho.2006.2043. [DOI] [PubMed] [Google Scholar]
- 34.Hossain M, Nakamura Y, Yamada Y, Ito M, Matsumoto K. Caries -preventive effect of Er:YAG laser irradiation with or without water mist. J Clin Laser Med Surg. 2000;18:61–5. doi: 10.1089/clm.2000.18.61. [DOI] [PubMed] [Google Scholar]
- 35.Corrêa-Afonso AM, Ciccone-Nogueira JC, Pecora JD, Palma-Dibb RG. In vitro assessment of laser efficiency for caries prevention in pits and fissures. Microsc Res Tech. 2012;75:245–52. doi: 10.1002/jemt.21050. [DOI] [PubMed] [Google Scholar]
- 36.Maung NL, Wohland T, Hsu CY. Enamel diffusion modulated by Er:YAG laser (Part 2) Organic matrix. J Dent. 2007;35:794–9. doi: 10.1016/j.jdent.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 37.Rodrigues LK, Nobre Dos Santos M, Pereira D, Assaf AV, Pardi V. Carbon dioxide laser in dental caries prevention. J Dent. 2007;32:531–40. doi: 10.1016/j.jdent.2004.04.004. [DOI] [PubMed] [Google Scholar]


