Abstract
Objective:
The purpose of this study was to investigate the morphology and number of roots of Korean mandibular third molars, and to evaluate the prevalence of C-shaped, two-rooted, and three-rooted mandibular third molars using cone-beam computed tomography (CBCT).
Materials and Methods:
Serial axial CBCT images of the mandibles were gathered from 137 Korean patients. The total number of roots in the mandibular third molars of these patients was measured, and both the incidence and the correlations between left- and right-side occurrences, as well as between males and females, were analyzed.
Results:
Most of the mandibular third molars either had two roots (56.5%) or one root (37.9%). There was no significant difference regarding the incidence of the different types of roots according to gender (female versus male) or topology (right versus left side). A higher percentage (80.5%) of the patients had similar root morphology on both sides.
Conclusion:
The morphology and number of 214 mandibular third molars were examined using CBCT. There was a high prevalence of two-rooted mandibular and one-rooted mandibular third molars from this Korean population. Even though the anatomical variations in the mandibular third molars may not be high, these data regarding the occurrence and morphology of the roots will provide useful information to dentists performing these procedures.
Keywords: Cone-beam computed tomography, C-shaped root, mandibular third molar, morphology, radix entomolaris
INTRODUCTION
Mandibular third molars are removed for various reasons.[1] More recently, they have been used in autotransplantation procedures to replace non-restorable teeth.[2] The transplantation of third molars may help to maintain alveolar bone and enable endosseous implantation without requiring bone regeneration, fulfilling functional and aesthetic demands.[3,4] Information regarding morphology and number of roots may be especially beneficial for careful extraction and subsequent endodontic procedures in autotransplantation.[5] Root morphology may vary among different population groups.[6] Relatively few studies have been conducted on the root and canal morphology of mandibular third molars,[7,8] and there is no available report that specifically examines the use of cone-beam computed tomography (CBCT).
CBCT was introduced for head and neck applications and consists of a conical radiographic source and a high-performance digital panel detector.[9] CBCT has been used in various applications, including measurements for gingival and dentogingival units,[10,11] as a preoperative tool in decision making for furcation involvement,[12] evaluation of the facial bony wall,[13] estimation of cancellous bone density,[14] clinical assessment of bone grafting,[15] assessment of root length,[16] and resorption of the root.[17] It has been suggested that CBCT data may provide a better basis for treatment plans.[18]
The main purpose of this study was to investigate the root morphology of Korean mandibular third molars, and to evaluate the prevalence of C-shaped (gutter-shaped), two-rooted, and three-rooted mandibular third molars with distolingual roots.
MATERIALS AND METHODS
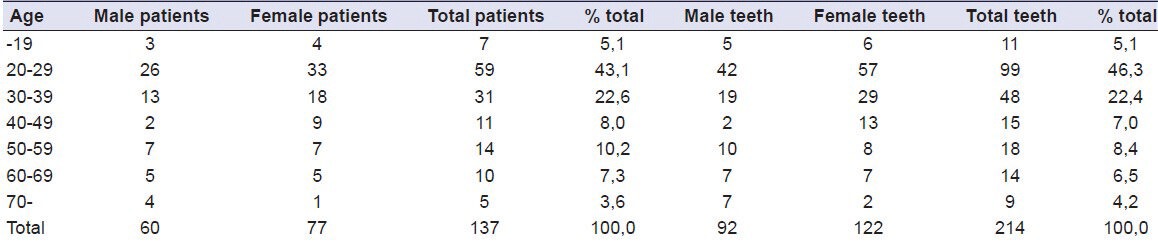
We studied 137 patients who visited the dental hospital at Seoul St. Mary's Hospital in Seoul, Korea, between March 2009 and May 2011. Evaluations were performed on 60 male and 77 female patients whose mean age was 35.3 ± 15.3 [Table 1]. This study was approved by the Institutional Review Board.
Table 1.
Descriptive statistics of study population according to the age and gender
An i-CAT scanner (Imaging Sciences International, Hatfield, PA, USA) with a spatial resolution of 10 line pairs per centimeter and an isotropic 0.4-mm voxel size was used for this study. Serial axial CBCT images were evaluated continuously by moving the toolbar from the floor of pulp chamber to the apex to determine the number of roots and their morphology, using commercially available software (M-view™, Seoul, Korea).
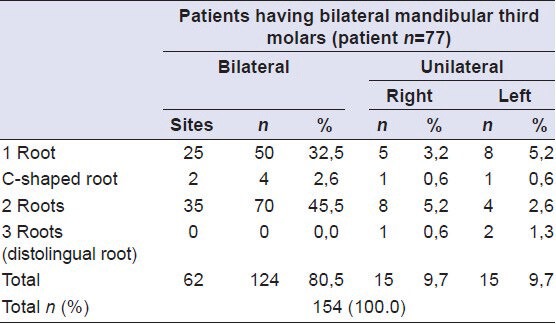
The incidences of mandibular third molars with one-root, C-shaped roots, two roots, or three roots were evaluated by age group, gender, and topology [Figures 1–4]. To evaluate the bilateral occurrence of one-rooted, C-shaped, and three-rooted mandibular third molars, evaluations were performed only on the patients who had bilateral mandibular third molars (patient n = 77).
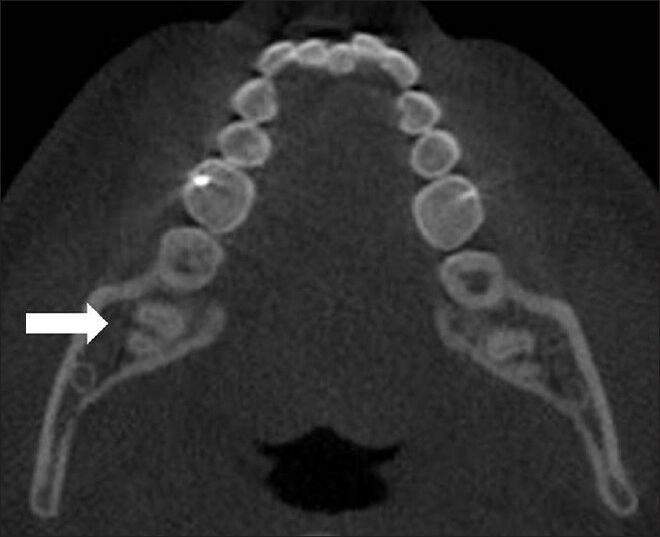
Figure 1.
Cone-beam computed tomography images showing mandibular third molars with one root (arrow)
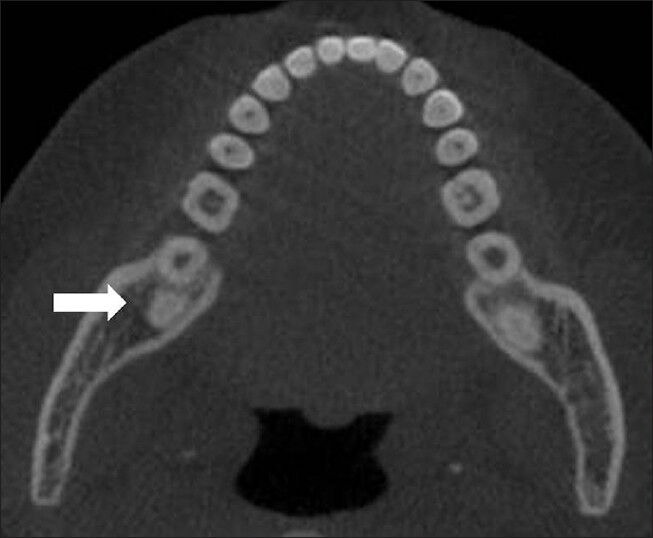
Figure 4.
Mandibular third molars with three roots having distolingual root (arrow)
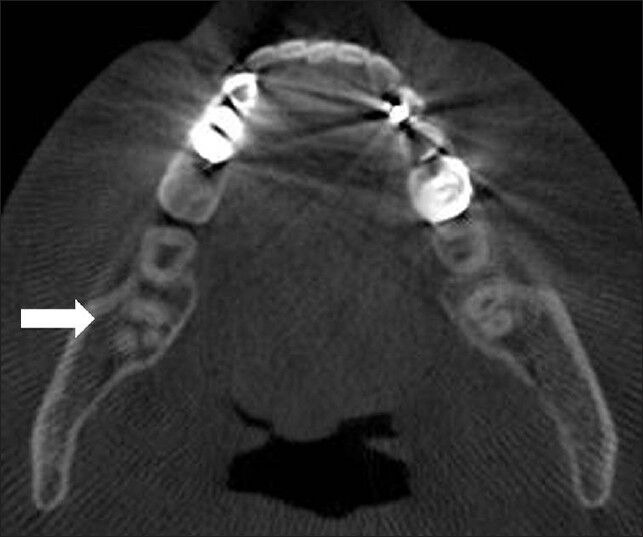
Figure 2.
Mandibular third molars with one root with C-shaped canal (arrow)
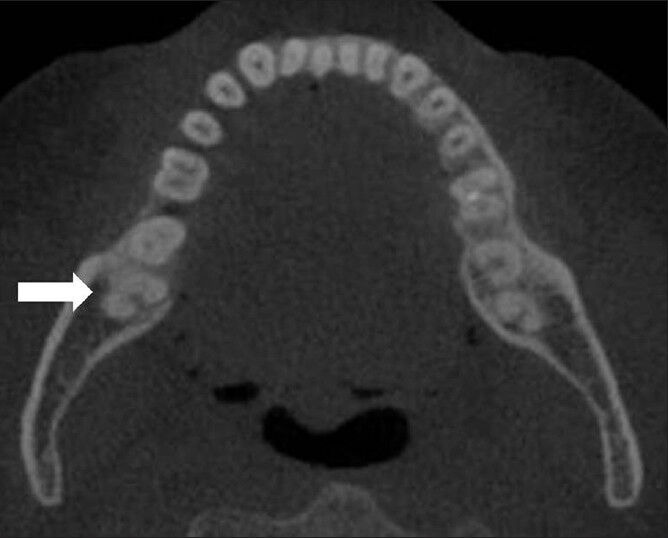
Figure 3.
Mandibular third molars with two roots (arrow)
Statistical analyses of the occurrences, according the contributing factors, were performed using the Chi-square test. Data analysis was done with commercially available software (PASW Statistics 18, SPSS Inc., Chicago, IL, USA) and the level of significance was 0.05.
RESULTS
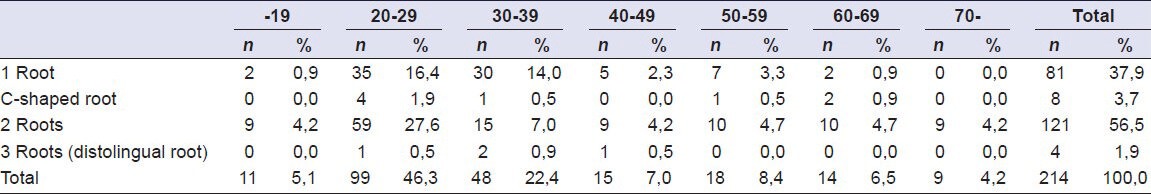
The number and percentage of mandibular third molars evaluated in the study group are listed in Table 1. Analysis of these root numbers by age group is seen in Table 2. One hundred and twenty-one teeth (56.5%) were detected to have two roots. Eighty-one third molars (37.9%) were one-rooted. Only 3.7% of mandibular third molars had C-shaped roots, and 1.9% had three roots with distolingual roots. Calculating the incidence of each type by using the total number of teeth in each age group as the denominator, the occurrence of three-rooted teeth in each affected age group (20-29, 30-39, 40-49) increased to a respective 1.0% (1/99), 4.2% (2/48), and 6.7% (1/15). The percentage of C-shaped roots for the age groups 20-29, 30-39, 50-59, 60-69 was a respective 4.0% (4/99), 2.1% (1/48), 5.6% (1/18), and 14.3% (2/14). The overall occurrence of the number of roots in each age group was reported to show significant difference [P < 0.05, Table 2], and the incidence of multi-rooted third molars tended to increase with patient age.
Table 2.
Analysis of incidence of mandibular third molars with one-root, C-shaped root, two roots, or three roots according to age groups
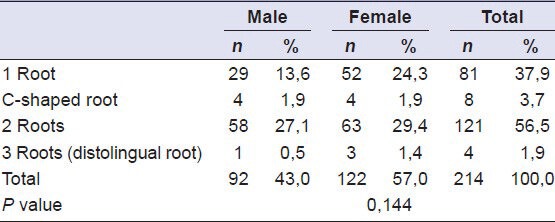
The classification of mandibular third molars by root number and gender is seen in Table 3. Using the total number of mandibular molars in male and female patients as the denominator, the incidences of one root (31.5% (29/92) for male versus 42.6% (52/122) for female), C-shaped root (4.3% (4/92) for male versus 3.3% (4/122) for female), two roots (63.0% (58/92) for male versus 51.6% (63/122) for female), three roots (1.1% (1/192) for male versus 2.5% (2/112 for female) were similar between males and females (P = 0.144).
Table 3.
Classification of mandibular third molars by root number and gender
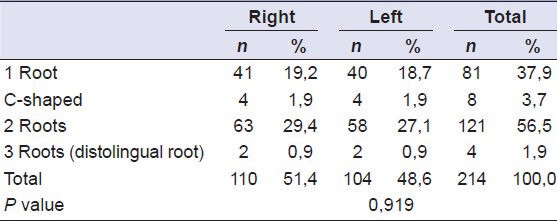
Classification of mandibular third molars by number of roots and topology is done in Table 4. The incidences of one root (37.3% (42/110) for right side versus 38.5% (40/104) for left side), C-shaped root (3.6% (4/110) for right side versus 3.8% (4/104) for left side), two roots (57.3% (63/110) for right side versus 55.8% (58/104) for left side), three roots (1.8% (2/110) for right side versus 1.9% (2/104) for left side) appeared to be very similar between the right and left sides (P = 0.919).
Table 4.
Classification of permanent mandibular third molars by root number and topology (right and left side)
An analysis of bilateral and unilateral distribution of mandibular third molars with C-shaped roots, two roots, or three roots having distolingual roots is listed in Table 5. To evaluate the bilateral occurrence of one-rooted, C-shaped, two-rooted, and three-rooted mandibular third molars, only patients who had bilateral mandibular third molars were included in the study. The incidence rate of each of these types was calculated using the total number of mandibular molars in each group (the one-rooted, C-shaped, two-rooted, and three-rooted groups) as the denominator. Bilateral occurrence was more evident for all groups except for the three-rooted group. Calculated bilateral and unilateral distributions for each group are as follows: one-rooted group (79.4% (50/63) for bilateral distribution versus 20.6% (13/63) for unilateral distribution), C-shaped group (66.7% (4/6) for bilateral distribution versus 33.3% (2/6) for unilateral distribution), two-rooted group (85.4% (70/82) for bilateral distribution versus 14.6% (12/82) for unilateral distribution), and three-rooted group (0.0% (0/3) for bilateral distribution versus 100.0% (3/3) for unilateral distribution).
Table 5.
Analysis of bilateral and unilateral distribution of mandibular third molars with C-shaped root, two roots or three roots having distolingual root
DISCUSSION
This study used CBCT images to evaluate the number of roots and the morphology of 214 mandibular third molars in 137 Korean individuals. The mandibular third molar, the last tooth in the molar series, is reported to be associated with greater variation in root pattern and canal systems.[8] It is widely accepted that mandibular molars usually have two roots: one located mesially and one distally.[19] This study showed that highest percentage of mandibular third molars (56.5%) had two roots, which is consistent with previous reports that showed respective results of 53.0% and 53.4%.[8,20]
The incidence of three roots found for this report was rare (1.9%), and the additional roots were found in the distolingual area. An additional root that is located distolingually is called radix entomolaris,[21] and this is a morphological variant identified as an Mongolian trait.[22] An additional root located in the lingual area is reported to be very rare (0.9%) in mandibular third molars.[8,23] We found that the overall occurrence of the number of roots according to age groups was significantly different; specifically, the younger the group, the lower the incidence rate of multi-rooted teeth. Further study with a larger number of patients may be needed to draw conclusions about this apparent trend.
Gender predilection for the presence of distolingual roots and C-shaped roots in mandibular third molars was also evaluated in this study. This report showed no significant difference based on gender. Previous reports have already found no significant differences in third molar development between males and females,[24] and no significant relationship between the gender of the patient and the presence or absence of third molars has been found either.[25]
Topological predilection for the presence of either the distolingual root or C-shaped root in mandibular third molars is rarely reported in the literature. This study observed very similar occurrences between the right and left sides of the same patient's jaw. No significant side differences of mandibular third molar mineralization have been reported previously,[26] and prior study found that left-right symmetry in the root development of the mandibular third molar was very high, with a correlation coefficient of 0.93 for males and 0.95 for females.[27]
Analysis was performed to evaluate the unilateral or bilateral occurrence of one-rooted, C-shaped, two-rooted, and three-rooted teeth in the mandibular third molars. Most patients (80.5%) exhibited similar morphology on both their right and left mandibular sides. A previous report indicated that 78.2% of the individuals studied possessed both mandibular third molars, while 11.3% had one and 10.5% had none.[26]
Extraction of mandibular third molars is a common operation in oral and maxillofacial surgery, and many reports have been published related to this issue.[28,29] Various aspects such as the prevalence of caries experience, carious lesions, or restorations on the occlusal surface have been determined in asymptomatic third molars that have erupted to the occlusal plane.[30] The prevalence of caries in third molars is considered to be high as well as associated with patients’ caries experiences in first and second molars.[30]
The morphology of mandibular third molars may be of interest to the operator for many procedures including surgical removal, autotransplantation for atraumatic procedures, and endodontic treatment.[4,21,31] Tooth autotransplantation using mandibular third molars is reported be a useful surgical method to replace non-restorable teeth, with a high long-term survival rate.[2] Recently, phase-contrast radiography was used to assess the root morphology of mandibular third molars, and it was suggested that phase-contrast radiography may be more useful than conventional radiography for this purpose.[32]
CONCLUSIONS
The morphology and root counts of 214 mandibular third molars were examined using CBCT. There was a high prevalence of two-rooted and one-rooted mandibular third molars from a Korean population, and it was found that the incidence of multi-rooted third molars tended to increase with patient age. These data regarding the occurrence and morphology of teeth roots will provide useful information to dentists for various dental procedures.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Libersa P, Savignat M, Tonnel A. Neurosensory disturbances of the inferior alveolar nerve: a retrospective study of complaints in a 10-year period. J Oral Maxillofac Surg. 2007;65:1486–9. doi: 10.1016/j.joms.2007.03.023. [DOI] [PubMed] [Google Scholar]
- 2.Yan Q, Li B, Long X. Immediate autotransplantation of mandibular third molar in China. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:436–40. doi: 10.1016/j.tripleo.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 3.Reich PP. Autogenous transplantation of maxillary and mandibular molars. J Oral Maxillofac Surg. 2008;66:2314–7. doi: 10.1016/j.joms.2008.06.039. [DOI] [PubMed] [Google Scholar]
- 4.Mendes RA, Rocha G. Mandibular third molar autotransplantation: literature review with clinical cases. J Can Dent Assoc. 2004;70:761–6. [PubMed] [Google Scholar]
- 5.Kitahara T, Nakasima A, Shiratsuchi Y. Orthognathic treatment with autotransplantation of impacted maxillary third molar. Angle Orthod. 2009;79:401–6. doi: 10.2319/022008-103.1. [DOI] [PubMed] [Google Scholar]
- 6.Peiris R, Takahashi M, Sasaki K, Kanazawa E. Root and canal morphology of permanent mandibular molars in a Sri Lankan population. Odontology. 2007;95:16–23. doi: 10.1007/s10266-007-0074-8. [DOI] [PubMed] [Google Scholar]
- 7.Gulabivala K, Opasanon A, Ng YL, Alavi A. Root and canal morphology of Thai mandibular molars. Int Endod J. 2002;35:56–62. doi: 10.1046/j.1365-2591.2002.00452.x. [DOI] [PubMed] [Google Scholar]
- 8.Gulabivala K, Aung TH, Alavi A, Ng YL. Root and canal morphology of Burmese mandibular molars. Int Endod J. 2001;34:359–70. doi: 10.1046/j.1365-2591.2001.00399.x. [DOI] [PubMed] [Google Scholar]
- 9.Misch KA, Yi ES, Sarment DP. Accuracy of cone beam computed tomography for periodontal defect measurements. J Periodontol. 2006;77:1261–6. doi: 10.1902/jop.2006.050367. [DOI] [PubMed] [Google Scholar]
- 10.Januario AL, Barriviera M, Duarte WR. Soft tissue cone-beam computed tomography: a novel method for the measurement of gingival tissue and the dimensions of the dentogingival unit. J Esthet Restor Dent. 2008;20:366–73. doi: 10.1111/j.1708-8240.2008.00210.x. discussion 374. [DOI] [PubMed] [Google Scholar]
- 11.Fu JH, Yeh CY, Chan HL, Tatarakis N, Leong DJ, Wang HL. Tissue biotype and its relation to the underlying bone morphology. J Periodontol. 2010;81:569–74. doi: 10.1902/jop.2009.090591. [DOI] [PubMed] [Google Scholar]
- 12.Kaner D, Friedmann A. Soft tissue expansion with self-filling osmotic tissue expanders before vertical ridge augmentation: a proof of principle study. J Clin Periodontol. 2011;38:95–101. doi: 10.1111/j.1600-051X.2010.01630.x. [DOI] [PubMed] [Google Scholar]
- 13.Januario AL, Duarte WR, Barriviera M, Mesti JC, Araujo MG, Lindhe J. Dimension of the facial bone wall in the anterior maxilla: A cone-beam computed tomography study. Clin Oral Implants Res. 2011;22:1168–71. doi: 10.1111/j.1600-0501.2010.02086.x. [DOI] [PubMed] [Google Scholar]
- 14.Naitoh M, Hirukawa A, Katsumata A, Ariji E. Prospective study to estimate mandibular cancellous bone density using large-volume cone-beam computed tomography. Clin Oral Implants Res. 2010;21:1309–13. doi: 10.1111/j.1600-0501.2010.01950.x. [DOI] [PubMed] [Google Scholar]
- 15.Hamada Y, Kondoh T, Noguchi K, Iino M, Isono H, Ishii H, et al. Application of limited cone beam computed tomography to clinical assessment of alveolar bone grafting: a preliminary report. Cleft Palate Craniofac J. 2005;42:128–37. doi: 10.1597/03-035.1. [DOI] [PubMed] [Google Scholar]
- 16.Lund H, Grondahl K, Grondahl HG. Cone beam computed tomography for assessment of root length and marginal bone level during orthodontic treatment. Angle Orthod. 2010;80:466–73. doi: 10.2319/072909-427.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Topkara A, Karaman AI, Kau CH. Apical root resorption caused by orthodontic forces: A brief review and a long-term observation. Eur J Dent. 2012;6:445–53. [PMC free article] [PubMed] [Google Scholar]
- 18.Walter C, Weiger R, Zitzmann NU. Accuracy of three-dimensional imaging in assessing maxillary molar furcation involvement. J Clin Periodontol. 2010;37:436–41. doi: 10.1111/j.1600-051X.2010.01556.x. [DOI] [PubMed] [Google Scholar]
- 19.Wang Y, Zheng QH, Zhou XD, Tang L, Wang Q, Zheng GN, et al. Evaluation of the root and canal morphology of mandibular first permanent molars in a western Chinese population by cone-beam computed tomography. J Endod. 2010;36:1786–9. doi: 10.1016/j.joen.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 20.Furri M. Differences in the confluence of mesial canals in mandibular molar teeth with three or four root canals. Int Endod J. 2008;41:777–80. doi: 10.1111/j.1365-2591.2008.01431.x. [DOI] [PubMed] [Google Scholar]
- 21.Schafer E, Breuer D, Janzen S. The prevalence of three-rooted mandibular permanent first molars in a German population. J Endod. 2009;35:202–5. doi: 10.1016/j.joen.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 22.Tu MG, Huang HL, Hsue SS, Hsu JT, Chen SY, Jou MJ, et al. Detection of permanent three-rooted mandibular first molars by cone-beam computed tomography imaging in Taiwanese individuals. J Endod. 2009;35:503–7. doi: 10.1016/j.joen.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 23.Guerisoli DM, de Souza RA, de Sousa Neto MD, Silva RG, Pecora JD. External and internal anatomy of third molars. Braz Dent J. 1998;9:91–4. [PubMed] [Google Scholar]
- 24.Orhan K, Ozer L, Orhan AI, Dogan S, Paksoy CS. Radiographic evaluation of third molar development in relation to chronological age among Turkish children and youth. Forensic Sci Int. 2007;165:46–51. doi: 10.1016/j.forsciint.2006.02.046. [DOI] [PubMed] [Google Scholar]
- 25.Bolanos MV, Moussa H, Manrique MC, Bolanos MJ. Radiographic evaluation of third molar development in Spanish children and young people. Forensic Sci Int. 2003;133:212–9. doi: 10.1016/s0379-0738(03)00037-9. [DOI] [PubMed] [Google Scholar]
- 26.Meinl A, Tangl S, Huber C, Maurer B, Watzek G. The chronology of third molar mineralization in the Austrian populationL: A contribution to forensic age estimation. Forensic Sci Int. 2007;169:161–7. doi: 10.1016/j.forsciint.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 27.Gunst K, Mesotten K, Carbonez A, Willems G. Third molar root development in relation to chronological age: a large sample sized retrospective study. Forensic Sci Int. 2003;136:52–7. doi: 10.1016/s0379-0738(03)00263-9. [DOI] [PubMed] [Google Scholar]
- 28.Hashemi HM, Beshkar M, Aghajani R. The effect of sutureless wound closure on postoperative pain and swelling after impacted mandibular third molar surgery. Br J Oral Maxillofac Surg. 2012;50:256–8. doi: 10.1016/j.bjoms.2011.04.075. [DOI] [PubMed] [Google Scholar]
- 29.Metin M, Sener I, Tek M. Impacted teeth and mandibular fracture. Eur J Dent. 2007;1:18–20. [PMC free article] [PubMed] [Google Scholar]
- 30.Shugars DA, Jacks MT, White RP, Jr, Phillips C, Haug RH, Blakey GH. Occlusal caries experience in patients with asymptomatic third molars. J Oral Maxillofac Surg. 2004;62:973–9. doi: 10.1016/j.joms.2003.08.040. [DOI] [PubMed] [Google Scholar]
- 31.Pattanshetti N, Gaidhane M, Al Kandari AM. Root and canal morphology of the mesiobuccal and distal roots of permanent first molars in a Kuwait population: A clinical study. Int Endod J. 2008;41:755–62. doi: 10.1111/j.1365-2591.2008.01427.x. [DOI] [PubMed] [Google Scholar]
- 32.Sato T, Nakamoto N, Abe T, Fukushima Y, Tomaru Y, Sakata Y, et al. Preliminary results of a study comparing conventional radiography with phase-contrast radiography for assessing root morphology of mandibular third molars. Dentomaxillofac Radiol. 2011;40:91–5. doi: 10.1259/dmfr/13833682. [DOI] [PMC free article] [PubMed] [Google Scholar]


