Abstract
Aim:
The purpose of the present randomized clinical trial was to evaluate the color change, rebound effect and sensitivity of at-home bleaching with 15% carbamide peroxide and power bleaching using 38% hydrogen peroxide.
Materials and Methods:
For bleaching techniques, 20 subjects were randomized in a split mouth design (at-home and power bleaching): In maxillary and mandibular anterior teeth (n = 20). Color was recorded before bleaching, immediately after bleaching, at 2 weeks, 1, 3 and 6 month intervals. Tooth sensitivity was recorded using the visual analog scale. The Mann-Whitney test was used to compare both groups regarding bleaching effectiveness (ΔE1), rebound effect (ΔE2) and color difference between the rebounded tooth color and unbleached teeth (ΔE3) while the Wilcoxon compared ΔE within each group. Distribution of sensitivity was evaluated using the Chi-square test (α =0.05).
Results:
There was no significant difference between groups regarding ΔE1 and ΔE3 (P > 0.05). Even though, ΔE2 showed no significant difference between groups after bleaching as well as at 2 week, 1 month and 3 month follow-up periods (P > 0.05). Although, significant difference was found in ΔE2 (P < 0.05 Mann-Whitney) between two methods after 6 months and a high degree of rebound effect was obtained with power bleaching. Within each group, there was no significant difference between ΔE1 and ΔE3 (P < 0.05 Wilcoxon). The distribution of sensitivity was identical with both techniques (P > 0.05).
Conclusion:
Bleaching techniques resulted in identical tooth whitening and post-operative sensitivity using both techniques, but faster color regression was found with power bleaching even though color regression to the baseline of the teeth in both groups was the same after 6 months.
Keywords: At-home bleaching, post-treatment sensitivity, power bleaching, tooth bleaching, tooth color regression
INTRODUCTION
The most conservative way to modify the color of teeth is the use of a bleaching procedure. The most frequently used bleaching techniques are “power bleaching” (in-office) and “at-home bleaching”. Power bleaching utilizes a high concentration of bleaching agent (30-35% hydrogen peroxide) administered in a dental office setting. On the other hand, at-home bleaching employs the use of low concentrations of whitening agent (10-20% carbamide peroxide) placed in a custom-made mouth guard and administered daily over a 2-6 week period.[1,2]
The office-administered power bleaching procedure is an appropriate alternative to at-home bleaching, especially in the case of severe discolorations of individual teeth, lack of patient compliance or if rapid treatment is desired. The bleaching process could be initiated using power bleaching method in the dental office then continued at-home using a home bleaching technique.[3]
Regression of tooth whitening resulting from dental bleaching is a phenomenon that occurs following bleaching procedures.[4] It was thought that the initial whitening of the tooth color may be due to enamel dehydration.[5] In a, randomized clinical trial, Matis et al.[6] showed a rebound effect associated with 10% and 15% concentrations of carbamide peroxide gels.
Giachetti et al.[7] showed no clinically significant regression of bleaching efficacy with at-home and in-office bleaching techniques producing satisfactory and long-lasting bleaching results.
Post-treatment sensitivity is usually related to small microscopic enamel defects and subsurface pores, which allow the whitening agent to penetrate into the dental tubules and ultimately the pulp, causing reversible pulpitis and consequent teeth thermal sensitivity, but not causing permanent damage to the pulp. These responses are correlated with the peroxide concentration, time, frequency of gel application and pulp temperature rise after light activation.[8,9] Schulte et al.[10] found that sensitivity was severe enough to cause 14% of patients to discontinue bleaching treatments.
However, dentin exposure may be a factor in tooth sensitivity as it is often misdiagnosed as not being present.[11] However, other researchers[12] have correlated the incidence and severity of thermal sensitivity with gingival recession and the frequency of treatments, but not the actual duration, of the treatment.[13]
The purpose of the present randomized clinical trial was to evaluate the color change, rebound effect and sensitivity of at-home bleaching with 15% carbamide peroxide and power bleaching with 38% hydrogen peroxide.
The null hypothesis of this study was that there was no difference between two dental bleaching methods regarding the (1) degree and (2) durability of the resultant whitening of the treated teeth and (3) both bleaching methods are identical in terms of post-treatment sensitivity at different time intervals after bleaching.
MATERIALS AND METHODS
Using a patient selection method from a study by Ontiveros and Paravina,[14] 20 individuals (eight men and 12 women) in good general and dental health and ages between 18 and 55 years with an anterior teeth shade mean of 2M2 or darker (Vita 3D Master, Vitapan Classical, VITA Zahnfabrik, Bad Säckingen, Germany) were included in the study.
Prospective candidates with active caries, periodontal disease, orthodontic treatment or teeth with previous hypersensitivity, tetracycline staining and fluorosis related-discoloration were excluded from the study. All participants were given a brief explanation about the investigation and all consented to participate and signed a consent form approved by the Committee on Ethics in Research, University of Mashhad Medical Sciences. This single blind randomized clinical trial was registered at: http://www.IRCT.ir with an identification number IRCT201104236267N1.
Prior to the start of the study, the degree of tooth sensitivity of each participant was evaluated using the visual analog scale (VAS). Each person described the degree of discomfort in response to the application of air sprayed from a dental syringe at a pressure about 45-60 psi and held 2 mm away from middle-third of facial surface of the anterior teeth in each arch for 3 s. The teeth on the opposite arch were isolated from the air flow during testing using the operator's finger and cotton rolls.
At the same time shades of the teeth were determined within the standardized lightness, chroma and hue (LCH) color space by an operator experienced in color evaluation using a visual shade matching system. (Vita 3D Master). First, the lightness (L) of the teeth was assessed by selecting the closest match from one of five value groups. Next, chroma (C) was assessed. Finally, hue (H) was selected by determining if the tooth was more reddish or more yellowish than the shade sample selected. Shade assessments were made under constant light conditions. In addition, tooth shades of the upper and lower front teeth were determined in the LCH color space using a Vita Easyshade spectrophotometer. This allowed images that were not affected by visual perception, office lighting or time of day. The device is capable of instantly measuring a broad range of 45 shades, including three bleached, 26 Vitapan 3D Master and 16 Vita classical shades.
Participants were enrolled in a split mouth study design. For this purpose, a block randomization schedule was used for the arch assignments according to the type of bleaching treatment to be employed. The schedule was prepared in advance and recorded on 20 reference cards. Each card had a chart that consisted of two versions. One version assigned at-home bleaching for maxillary anterior teeth and power bleaching for mandibular anterior teeth. In the other version, the treatment assignment was reversed (at-home bleaching assigned to mandibular anterior teeth and power bleaching for maxillary anterior teeth).
Each of the 20 subjects selected a card at the treatment appointment. The color examiner was blinded to treatment group assignment throughout the study. It was not possible for the participants to be blinded.
Study casts were fabricated for each patient then the facial surfaces of the teeth were blocked out at a distance of approximately 0.5 mm coronal to the gingival margins. Customized at-home bleaching trays were then fabricated using a vacuum-formed process. Participants were instructed in the use of dispensed gel (Opalescence 15%, Ultradent, South Jordan, UT, USA). At night, for a period of 4 h/day, during a contiguous 2 week period according to the manufacturers’ recommendations.
Upon completion of the at-home bleaching phase of the study, participants were recalled to perform the in-office power bleaching procedure of the opposing dental arch. The gingival tissue adjacent to the teeth to be bleached was isolated using a light-cured resin (Bleach mask Light Cure, Bydental, Maltinti, Italy). A 38% hydrogen peroxide gel (BY WHITE XTRA 38%, Bydental, Maltinti, Italy) was used in three 15-min applications and activated by light emitting diode (LED) curing system (Sky Light Easy, Bydental, Maltinti, Italy).[15] This light source consists of a matrix of LEDs with a wave length of 465 nm and power of 8 W with 12 high intensity diodes. The power bleaching gel was refreshed every 15 min during a 45 min application period. The post-bleaching sensitivity of both arches was evaluated using the VAS. Post-bleaching shade determination of both jaws was done 2 h following the power bleaching as mentioned previously. Participants were asked to restrict smoking or drinking beverages such as wine, tea or coffee during the study.
Participants were followed at 2 weeks, then at 1, 3 and 6 month intervals. At each interval, tooth shade determinations and tooth hypersensitivity were made following the same protocol that was conducted at the baseline. Figure 1 is a schematic view of color change in tested teeth.
Figure 1.
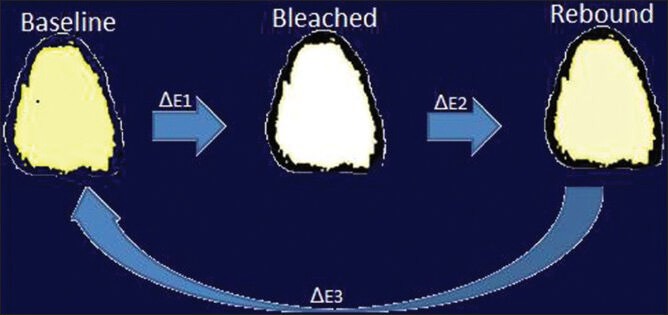
Schematic view of bleaching effectiveness (ΔE1), rebound effect (ΔE2) and color difference between post-treatment and unbleached teeth (ΔE3)
Bleaching effectiveness (ΔE1 = the difference between baseline and immediate color assessment) and the rebound effect (ΔE2 = the difference between immediate and when the color rebound happened) and color difference between rebounded tooth color and unbleached teeth (ΔE3) were estimated.
Statistical analyses
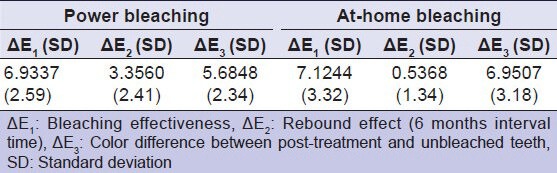
It should be mentioned that even though the data was quantitative the Kolmogorov-Smirnov test failed to show the normality of the data. As a result, dealing with data in this study was in two respects; inferential and descriptive in nature. This means that the inferential aspect derived from hypotheses of study resulted in the nonparametric statistical analyses [Figure 2] being used for data comparisons and while, mean and standard deviations of data just described the ΔE [Table 1].
Figure 2.
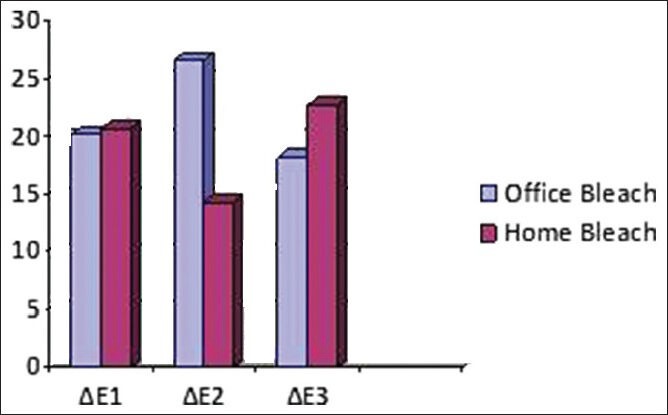
Mean rank values of ΔE associated with the two bleaching methods. (Note: ΔE1 = Bleaching effectiveness; ΔE2 = Rebound effect; ΔE3 = Color difference between post-treatment and unbleached teeth)
Table 1.
Mean (SD) values of ΔE associated with the two bleaching methods
The difference between the bleaching methods immediately after bleaching, then at 2 weeks, 1 month, 3 month and 6 month follow-up periods was compared using the Mann-Whitney test. Between groups, the bleaching effectiveness (ΔE1) and rebound effect (ΔE2) and ΔE3 were compared using the Mann-Whitney test because of non-matching data comparison between the two groups. The Friedman test was used to identify differences among ΔE1, ΔE2 and ΔE3 for each bleaching technique that was indicated for matching comparisons among three or more groups. The Wilcoxon test was done as the Friedman test showed some difference between ΔE1, ΔE2 and ΔE3 for each bleaching technique. The Wilcoxon is indicated for matching comparisons between only two groups.
The distribution of tooth sensitivity for comparing both methods and jaws was evaluated using the Chi-square test (α =0.05), that was indicated for qualitative data, for a non-matching comparison between two groups.
RESULTS
Eight participants from the power bleaching phase and six from the at-home bleaching phase complained about tooth sensitivity after treatment. Two of them experienced sensitivity after both treatment methods. Three participants were dissatisfied with the taste of the at-home bleaching agent. Nonetheless, all were able to complete the bleaching intervals successfully.
It should be noted that there was no significant difference between both bleaching methods immediately after bleaching, or at the 2 week, 1 month and 3 month follow-up periods. (P > 0.05 Mann-Whitney).
The only statistic significant difference between the two bleaching methods was found in ΔE2 (P = 0.001 < 0.05, Mann-Whitney) and at the 6 months follow-up period suggesting that the rebound effect in power bleaching method was significantly faster than that of at-home bleaching after 6 months.
In both groups, there was no significant difference between ΔE1 and ΔE3 (home bleach = 0.59 > 0.05 and office bleach = 0.069 > 0.05 Wilcoxon).
The Chi-square test showed that post-treatment sensitivity was identical (P > 0.05) for both methods [Figure 3].
Figure 3.
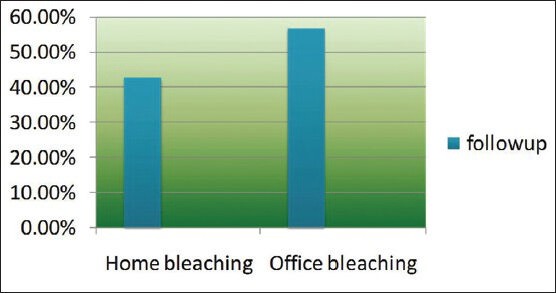
Prevalence of sensitivity with each bleaching method
DISCUSSION
The aim of this clinical trial was to address practitioner concerns regarding the efficacy, longevity and degree of hypersensitivity of bleached teeth after in-office vital bleaching compared with at-home bleaching techniques. This clinical trial was designed to evaluate the color change and rebound effect of at-home bleaching and power bleaching and to compare the two techniques within a maximum of 6 months after bleaching. The degree of tooth hypersensitivity after bleaching was also evaluated. It was hypothesized that both techniques would be the same regarding these clinical issues.
In this single blind study, only one examiner who measured the color after bleaching protocol was blinded to the experimental conditions.
The CIELAB[16] system was used to measurement of color difference in bleached teeth. This system is a 3D uniform color space with equal distances corresponding to equally perceived color differences. This system has three axes: The L* axis represents lightness and extends from 0 (black) to 100 (white); and a* and b* represent the redness-greenness and yellowness-blueness axis, respectively. When a* and b* coordinates approach zero, the colors become neutral. The spectrophotometer was considered more reliable by Matis et al.[17] because this method is more objective and sensible than a visual scale and photos. ΔE is the color difference between two objects and can be calculated within the CIELAB color system.[16] The naked eye is able to distinguish color differences if the ΔE value is more than 3.3.[18] Based on the CIE* L a* b* system the results of this study showed that both treatment groups significantly lightened the teeth because ΔE1 (Bleaching effectiveness) showed values more than 3.3 with power bleach (6.9337 ± 2.59) as well as with at-home bleach (7.1244 ± 3.32).
Results showed that there was no significant difference between groups regarding the degree of whitening (ΔE1). Therefore, the first null hypothesis of this study stating that the “degree of bleached teeth in both groups are statistically the same,” was accepted. Indeed, both protocols were effective in promoting tooth bleaching. This finding is in agreement with one previous study carried out by Almeida et al.[19] who compared the effectiveness of at-home and in-office bleaching techniques. They found no statistical difference between both methods regarding the degree of teeth whitening.
As stated in the statistical analysis of this study, there was no significant difference between both methods regarding regression of the whitening immediately after bleaching and at the 2 week, 1 month and 3 month follow-up periods. For this reason, the values of ΔE2 represented in Table 1 relates only to the 6 month time interval. A comparison between groups in terms of color regression showed a value significantly less than 3.3 for at-home bleaching (ΔE2 = 0.5368) compared with the power bleach technique (ΔE2 = 3.3560). Hence, the second null hypothesis of the study stating “having an identical durability of the whitening in treated teeth” for power bleaching was not accepted, while it was accepted for at-home bleaching because this technique showed a ΔE2 = 0.5368 ± 1.34 < 3.3. This means that the color regression was as negligible as it could be detected by the naked eye. Furthermore, this finding could support a hypothesis that has been accepted by a previous study stating “light could produce an initial effect that is not sustained for a long time.[20]
Regarding efficacy and longevity, there is a positive correlation between the rebounding of mineral density of the tooth and the degree of lightening. Using the at-home bleaching technique, the teeth receive a continual application of hydrogen peroxide during which the demineralization and remineralization processes interact.[4] While in power bleaching, the color regression is primarily a result of the reversal of whitening which is due to just the remineralization process.[21] Furthermore, power bleaching can have a dehydration effect on bleached teeth, which interferes with the evaluation of the color differences. In the present study, in order to decrease the consequences of whitening such as dehydration of teeth, the color evaluation of bleached teeth was done 2 h after the completion of the bleaching procedure rather than immediately thereafter. Even though, this time is insufficient for complete rehydration of the bleached teeth there is a limitation on delaying the color evaluation any longer because the regression of whitening might occur and interfere with the true results in terms of the degree of whitening and color regression. This procedure also has already been described by Li et al.[4]
Bizhang, et al.,[22] Marson, et al.[23] concluded that the at-home bleaching and in-office bleaching techniques were equally effective at the 3 months interval time after bleaching. The result of these studies could support the findings at the 3 months post-treatment time interval of the present study. However, the post-treatment evaluation period of these two studies were very short, which made it difficult to detect any loss of whitening.
Bernardon, et al.[24] found no difference in the bleaching result with regard to sensitivity and durability at the 6 month post-treatment interval. They used at-home bleaching with 10% carbamide peroxide versus in-office bleaching using 35% hydrogen peroxide activated with a LED/diode laser for two sessions each week for 2 weeks. The result of Brandon's study is in contrast with the present findings regarding rebound effect. This difference could be probably due to either the mode of light activation or the frequency of power bleaching that was performed in that study.
As for color difference between rebounded tooth color and unbleached teeth; (ΔE3), the values (5.6848 ± 2.34) and (6.9507 ± 3.18) resulted from power bleaching and at-home bleaching respectively, with no significant difference between them. This means that the whitened teeth showed an identical color relapse after 6 months. While, evaluating within groups showed no significant difference between ΔE1 and ΔE3 in this respect. This indicates that the amount of teeth whitening and the relapse to the initial color (baseline color) were also statistically equal for both groups.
According to the findings of the longevity of vital bleaching, we found that the longevity of both types is a maximum of 6 months; while in contrast to the results of the present study, Swift et al.[25] showed that satisfactory results persist for 1-2 years and patient should be advised regarding the need for re-bleaching procedures for 1 week every year. In that study, color evaluation was using only a Vita 3D Master shade guide that was not quantitative.
Post-treatment sensitivity of teeth, results from the penetration of peroxide through the enamel and dentin tubules to the pulp. Cooper et al.[26] claimed that this takes approximately five 15-min to occur. This explains why the color of dentin adjacent to the pulp can be whitened as rapidly as the dentin along the dentinoenamel junction.[27] There was no significant difference between both methods regarding tooth sensitivity. This finding leads to the acceptance of the third null hypothesis of the study.
One previous study demonstrated that sensitivity persisted for up to 4 days after treatment.[28] However, a longer duration of sensitivity up to 39 days has been reported as well.[29,30] In the present study, the overall percentages of subjects who experienced mild tooth sensitivity after bleaching were 42.9% for the at-home bleaching and 57.1% for power bleaching. This finding is same as the results of previous study carried out by Tavares et al.[31] who found no significant difference between at-home and power bleaching procedures. Kossatz et al.[32] found a range of 50 to 80% of patients experienced post-treatment tooth sensitivity after power bleaching.
Matis et al.[33] showed that the subjects who received three 15-min treatments with light activation expressed less gingival and tooth sensitivity than that was observed with one application of H2O2 within 40 min. In the present study, 38% H2O2 was applied in three 15-min treatments as a preventive strategy.
One of the limitations of this study was to not to test the re-bleaching procedure as well as the efficacy of doing so. A second limitation is related to the interval time between the 3 and 6 month evaluation intervals. This was very long in comparison with the other time intervals of this study and probably led to the inability to determine the exact time of color regression. As a result, it is not known if color regression occurred between the 3rd and 4th month interval or the 4th and 5th month interval or the 5th and 6th month post-treatment time interval. However, it is statistically clear that in-office bleached teeth reverted back to the original color sooner than at-home bleached teeth. The specific time when this occurred in this study could not be determined beyond that it was between the 3rd and 6th month time interval. However, it is important to note that after 6 months there was no trace of the whitening effect produced by either the at-home or in-office bleaching methods. On the other hand, in-office bleaching seems to achieve satisfactory results when more than one bleaching session is performed according to the findings of Gottardi et al.[34] who found no statistical difference in color rebound between 6 months and 2 years. Further study is required to address the limitations of the present study.
CONCLUSION
Within the limits of this study, it was determined that the degree of whitening was the same for both power bleaching in a dental office setting and the at-home bleaching technique. There was no difference in color regression between at-home and power bleaching at the 2 week, 1 month and 3 month follow-up periods. Regression of the whitening effect occurred after 6 months. Regression was more rapid with power bleaching than with home bleaching. As for the matter of post-treatment sensitivity, both bleaching methods are clinically identical at different time intervals.
Footnotes
Source of Support: This study was supported by grant from the Research Council of Mashad University of Medical Sciences, Iran.
Conflict of Interest: None declared
REFERENCES
- 1.Haywood VB, Heymann HO. Nightguard vital bleaching. Quintessence Int. 1989;20:173–6. [PubMed] [Google Scholar]
- 2.Lima DA, De Alexandre RS, Martins AC, Aguiar FH, Ambrosano GM, Lovadino JR. Effect of curing lights and bleaching agents on physical properties of a hybrid composite resin. J Esthet Restor Dent. 2008;20:266–73. doi: 10.1111/j.1708-8240.2008.00190.x. [DOI] [PubMed] [Google Scholar]
- 3.Barghi N. Making a clinical decision for vital tooth bleaching: At-home or in-office? Compend Contin Educ Dent. 1998;19:831–8. [PubMed] [Google Scholar]
- 4.Li Q, Xu BT, Li R, Yu H, Wang YN. Quantitative evaluation of colour regression and mineral content change of bleached teeth. J Dent. 2010;38:253–60. doi: 10.1016/j.jdent.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Matis BA, Cochran MA, Franco M, Al-Ammar W, Eckert GJ, Stropes M. Eight in-office tooth whitening systems evaluated in vivo: A pilot study. Oper Dent. 2007;32:322–7. doi: 10.2341/06-135. [DOI] [PubMed] [Google Scholar]
- 6.Matis BA, Mousa HN, Cochran MA, Eckert GJ. Clinical evaluation of bleaching agents of different concentrations. Quintessence Int. 2000;31:303–10. [PubMed] [Google Scholar]
- 7.Giachetti L, Bertini F, Bambi C, Nieri M, Scaminaci Russo D. A randomized clinical trial comparing at-home and in-office tooth whitening techniques: A nine-month follow-up. J Am Dent Assoc. 2010;141:1357–64. doi: 10.14219/jada.archive.2010.0081. [DOI] [PubMed] [Google Scholar]
- 8.Berga-Caballero A, Forner-Navarro L, Amengual-Lorenzo J. At-home vital bleaching: A comparison of hydrogen peroxide and carbamide peroxide treatments. Med Oral Patol Oral Cir Bucal. 2006;11:E94–9. [PubMed] [Google Scholar]
- 9.Haywood VB. History, safety, and effectiveness of current bleaching techniques and applications of the nightguard vital bleaching technique. Quintessence Int. 1992;23:471–88. [PubMed] [Google Scholar]
- 10.Schulte JR, Morrissette DB, Gasior EJ, Czajewski MV. The effects of bleaching application time on the dental pulp. J Am Dent Assoc. 1994;125:1330–5. doi: 10.14219/jada.archive.1994.0177. [DOI] [PubMed] [Google Scholar]
- 11.Bevenius J, Lindskog S, Hultenby K. The micromorphology in vivo of the buccocervical region of premolar teeth in young adults. A replica study by scanning electron microscopy. Acta Odontol Scand. 1994;52:323–34. doi: 10.3109/00016359409029030. [DOI] [PubMed] [Google Scholar]
- 12.Jorgensen MG, Carroll WB. Incidence of tooth sensitivity after home whitening treatment. J Am Dent Assoc. 2002;133:1076–82. doi: 10.14219/jada.archive.2002.0332. [DOI] [PubMed] [Google Scholar]
- 13.Leonard RH, Jr, Smith LR, Garland GE, Caplan DJ. Desensitizing agent efficacy during whitening in an at-risk population. J Esthet Restor Dent. 2004;16:49–55. doi: 10.1111/j.1708-8240.2004.tb00452.x. [DOI] [PubMed] [Google Scholar]
- 14.Ontiveros JC, Paravina RD. Color change of vital teeth exposed to bleaching performed with and without supplementary light. J Dent. 2009;37:840–7. doi: 10.1016/j.jdent.2009.06.015. [DOI] [PubMed] [Google Scholar]
- 15.Pobbe Pde O, Viapiana R, Souza-Gabriel AE, Marchesan MA, Sousa-Neto MD, Silva-Sousa YT, et al. Coronal resistance to fracture of endodontically treated teeth submitted to light-activated bleaching. J Dent. 2008;36:935–9. doi: 10.1016/j.jdent.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 16.Paris: Bureau Central de la CIE; 1978. Commission Internationale de L’Eclairage. Recommendations on Uniform Colour Spaces, Colour Terms. [Publication 15, Supplement 2] [Google Scholar]
- 17.Matis BA, Hamdan YS, Cochran MA, Eckert GJ. A clinical evaluation of a bleaching agent used with and without reservoirs. Oper Dent. 2002;27:5–11. [PubMed] [Google Scholar]
- 18.American Dental Association; 2006. ADA Acceptance Program. Guidelines Dentist-dispensed Home-use Tooth Bleaching Products. [Google Scholar]
- 19.Almeida LC, Riehl H, Santos PH, Sundfeld ML, Briso AL. Clinical evaluation of the effectiveness of different bleaching therapies in vital teeth. Int J Periodontics Restorative Dent. 2012;32:303–9. [PubMed] [Google Scholar]
- 20.Kugel G, Ferreira S, Sharma S, Barker ML, Gerlach RW. Clinical trial assessing light enhancement of in-office tooth whitening. J Esthet Restor Dent. 2009;21:336–47. doi: 10.1111/j.1708-8240.2009.00287.x. [DOI] [PubMed] [Google Scholar]
- 21.Xu B, Li Q, Wang Y. Effects of pH values of hydrogen peroxide bleaching agents on enamel surface properties. Oper Dent. 2011;36:554–62. doi: 10.2341/11-045-1. [DOI] [PubMed] [Google Scholar]
- 22.Bizhang M, Chun YH, Damerau K, Singh P, Raab WH, Zimmer S. Comparative clinical study of the effectiveness of three different bleaching methods. Oper Dent. 2009;34:635–41. doi: 10.2341/08-069-C. [DOI] [PubMed] [Google Scholar]
- 23.Marson FC, Sensi LG, Vieira LC, Araújo E. Clinical evaluation of in-office dental bleaching treatments with and without the use of light-activation sources. Oper Dent. 2008;33:15–22. doi: 10.2341/07-57. [DOI] [PubMed] [Google Scholar]
- 24.Bernardon JK, Sartori N, Ballarin A, Perdigão J, Lopes GC, Baratieri LN. Clinical performance of vital bleaching techniques. Oper Dent. 2010;35:3–10. doi: 10.2341/09-008CR. [DOI] [PubMed] [Google Scholar]
- 25.Swift EJ, Jr, May KN, Jr, Wilder AD, Jr, Heymann HO, Bayne SC. Two-year clinical evaluation of tooth whitening using an at-home bleaching system. J Esthet Dent. 1999;11:36–42. doi: 10.1111/j.1708-8240.1999.tb00374.x. [DOI] [PubMed] [Google Scholar]
- 26.Cooper JS, Bokmeyer TJ, Bowles WH. Penetration of the pulp chamber by carbamide peroxide bleaching agents. J Endod. 1992;18:315–7. doi: 10.1016/S0099-2399(06)80479-6. [DOI] [PubMed] [Google Scholar]
- 27.McCaslin AJ, Haywood VB, Potter BJ, Dickinson GL, Russell CM. Assessing dentin color changes from nightguard vital bleaching. J Am Dent Assoc. 1999;130:1485–90. doi: 10.14219/jada.archive.1999.0061. [DOI] [PubMed] [Google Scholar]
- 28.Dahl JE, Pallesen U. Tooth bleaching: A critical review of the biological aspects. Crit Rev Oral Biol Med. 2003;14:292–304. doi: 10.1177/154411130301400406. [DOI] [PubMed] [Google Scholar]
- 29.Leonard RH, Jr, Haywood VB, Phillips C. Risk factors for developing tooth sensitivity and gingival irritation associated with nightguard vital bleaching. Quintessence Int. 1997;28:527–34. [PubMed] [Google Scholar]
- 30.Tam L. Clinical trial of three 10% carbamide peroxide bleaching products. J Can Dent Assoc. 1999;65:201–5. [PubMed] [Google Scholar]
- 31.Tavares M, Stultz J, Newman M, Smith V, Kent R, Carpino E, et al. Light augments tooth whitening with peroxide. J Am Dent Assoc. 2003;134:167–75. doi: 10.14219/jada.archive.2003.0130. [DOI] [PubMed] [Google Scholar]
- 32.Kossatz S, Dalanhol AP, Cunha T, Loguercio A, Reis A. Effect of light activation on tooth sensitivity after in-office bleaching. Oper Dent. 2011;36:251–7. doi: 10.2341/10-289-C. [DOI] [PubMed] [Google Scholar]
- 33.Matis BA, Cochran MA, Wang G, Eckert GJ. A clinical evaluation of two in-office bleaching regimens with and without tray bleaching. Oper Dent. 2009;34:142–9. doi: 10.2341/08-64. [DOI] [PubMed] [Google Scholar]
- 34.de Silva Gottardi M, Brackett MG, Haywood VB. Number of in-office light-activated bleaching treatments needed to achieve patient satisfaction. Quintessence Int. 2006;37:115–20. [PubMed] [Google Scholar]


