Abstract
Imaging is one of the most important tools for orthodontists to evaluate and record size and form of craniofacial structures. Orthodontists routinely use 2-dimensional (2D) static imaging techniques, but deepness of structures cannot be obtained and localized with 2D imaging. Three-dimensional (3D) imaging has been developed in the early of 1990's and has gained a precious place in dentistry, especially in orthodontics. The aims of this literature review are to summarize the current state of the 3D imaging techniques and to evaluate the applications in orthodontics.
Keywords: 3D imaging, 3D scanning, orthodontic diagnosis, treatment planning
INTRODUCTION
Over the years, orthodontic and dentofacial orthopedic diagnosis and treatment planning have relied essentially upon technological and mechanical supports such as imaging, jaw monitoring, and functional analyses. The goals of these techniques are to replicate or describe the anatomic and physiological facts exactly and to display the three-dimensional (3D) anatomy precisely.[1]
Imaging is one of the most important tools for orthodontists to evaluate and record size and form of craniofacial structures.[2] Orthodontists routinely use 2-dimensional (2D) static imaging techniques to record the craniofacial anatomy, but deepness of structures cannot be obtained and localized with 2D imaging. 3D imaging has been developed in the early of 1990's and has gained a precious place in dentistry, especially in orthodontics, and also in orofacial surgical applications. In 3D diagnostic imaging, a series of anatomical data is gathered using certain technological equipment, processed by a computer and later showed on a 2D monitor to present the illusion of deepness.[3]
Facial soft and hard tissues and dentition are 3 main sections, also named as triad, in orthodontics and orthognatic surgery.[4] The triad has a significant function in planning of orthodontic treatment. Therefore, imaging of these structures is one of useful diagnostic tools for clinicians to make decision treatment modality.[5] 3D imaging for orthodontic purposes contain pre- and post-treatment evaluation of dentoskeletal and craniofacial relationships and facial appearance and beauty, inspecting treatment results in terms of soft and underlying hard tissues, and 3D treatment predictions. 3D dental, facial, and skeletal records for making diagnostic decisions and planning treatment are the other benefits of using 3D imaging in orthodontics.[6]
A large number of diagnostic methods have been developed to display facial structures and the dentition,[7,8,9] most of which were abandoned due to their various drawbacks. The most popular method of current medicine is possibly 3D imaging techniques giving detailed and problem-oriented information about soft and hard tissues, such as Computerized Tomography (CT), Cone Beam Computerized Tomography (CBCT), Micro Computerized Tomography (MCT), 3D laser scanning, structured light technique, sterophotogrametry or 3D surface imaging systems (3dMD), 3D facial morphometry (3DFM), Tuned-Aperture Computed Tomography (TACT), and Magnetic Resonance Imaging (MRI).[10,11,12,13,14,15,16,17]
The aims of this literature review are to present current state of the 3D imaging techniques and to evaluate the applications in orthodontics.
HISTORICAL BACKGROUND
In 1895, discovery of X-rays by W. C. Roentgen opened a new era in medicine and dentistry. Thirty-six years later, standardized methods for the production of cephalometric radiographs were introduced to the dental specialists by Broadbent and Hofrath simultaneously and independently,[18] and it remained comparatively unaltered until recently. Broadbent emphasized the importance of the position and distance arrangements to achieve distortion-free radiographs when taking the lateral and posteroanterior cephalometric radiographs.[18] Cephalograms have been widely used in clinical implementations and as an investigation technique to evaluate growth and treatment responses. However, there are several disadvantages of 2-dimensional cephalometry as a scientific method. The fact that a conventional head films reduce 3D objects to 2-dimensional view is first and the most important reason. When 3D objects are displayed in a 2-dimension, structures displace as vertically and horizontally in proportion to their distance from the film.[19,20] Secondly, cephalometric analyses are based on an excellent superimposition of the left and right sides at mid-sagittal plane, but such superimposition is rarely observed because facial symmetry is infrequent. Third reason is that manual data collection and processing in cephalometric analysis have been shown to have low correctness and precision.[21] Finally, major errors in cephalometric measurements are associated with uncertainties in locating anatomical landmarks due to the deficiency of well-defined outlines, hard edges, and shadows as well as patient position.[19]
Beside these limitations, lots of cephalometric analyses have been developed to help diagnose skeletal and dental malocclusions and dentofacial deformities.[22,23] The quantitative errors associated with traditional 2D cephalometry have been substantial enough to make orthodontic diagnosis and treatment planning.[19,22,23,24,25,26,27,28]
Following the introduction of 3D imaging, clinicians have had great opportunity to evaluate anatomic structures 3-dimensionally in orthodontic practice. Several investigators conducted 3D imaging researches, and Singh and Savara[29] reported the first 3D analysis about growth changes in maxilla. Computer softwares helped to collect and analyze 3D coordinates directly from digital cephalometric images, so that tracing manually and digitizing with mouse on screen were abandoned.[30,31]
3D imaging technique has been improved to use in different areas of health sciences. Being improved old photogrammetric techniques, stereophotogrammetry has been introduced to provide a more extensive and accurate assessments of the captured things. Using one or more converging pairs of views, a 3D model can be constructed and monitored from any perspectives and measured from any directions. In 1944, Thalmann-Degan recorded facial differences after orthodontic treatment. This was the earliest clinical report about stereophotogrammetry.[21] Computerized stereophotogrammetry has come into market as parallel to computer developments and has provided faster, more comprehensive and correct taking and constructing sequences.[32]
The first CT scanning device was developed around 40 years ago. After a short time, a stack of CT sectional images was used to obtain 3D information. At the beginning of 1980s, clinicians used 3D imaging in craniofacial deformities. For craniofacial surgical needs, first simulation software was introduced in 1986. Then, the principles and applications of 3D CT- and MRI-based imaging in medicine were published. A specific discipline was established on 3D imaging, dealing with different types of imaging, manipulation, and analysis of multi-dimensional medical structures.[32]
3D IMAGING METHODS
Computed tomography (CT)
CT imaging, also called computerized axial tomography (CAT) imaging, uses special X-ray equipment to generate cross-sectional images of the body.
CT devices are divided into 2 groups: Cone beam and fan beam.[33] Using conventional fan beam CT devices, the X-ray source and detectors with the circular metal frame rotate around the patient. Patients are placed in a horizontal position on a table when CT scanner works. The table slowly passes through the center of a large X-ray machine. The procedure causes no pain, but some tests require a contrast material to make some parts of body appear better in the image.
CT scanner works as follows:
The patient is moved into circular opening of the CT imaging by a motorized table. When the patient is ready, the operator starts the CT imaging system, and a complete rotation of X-ray source and detector lasts about 1 second. The CT device generates a narrow, fan-shaped beam of X-rays scanning a section of the patient's body. A “snapshot” image was recorded and collected by a detector opposite from the X-ray source. The obtained data are transmitted to a computer for each turn of the scanner and detector. One or multiple cross-sectional images of the body parts were reconstructed.
The patient is usually scanned in the axial plane sections taken in succession; the desired image appears when these sections combined. CT can achieve 64 and/or 128 sections in advanced fan beam CT at a one time. The system is most expensive because the image is obtained by increasing number of sensors. However, this system can perform in less time and at a low dose shooting.[33] In this technique, due to the sectioning of tissues, organs are not superposed on each other.
Although CT scans are very high-priced and have high radiation dose to be suitable for a lot of orthodontic applications, the benefits outweigh the risks in certain situations. For example, treatment of craniofacial deformities may be insufficient with 2-dimensional diagnostic records. CT scans generate a very intensive data set that contains 3D information about soft and hard tissues. These data may be extremely precious for diagnostic point of view.
In addition, the usage area of CT is quite wide in dentistry, such as in the diagnosis of some pathologies, and even the contents of the boundaries (solid, liquid, Agar-Agar) in determining the salivary gland pathologies,[34] examination of the structure of the temporomandibular joint (TMJ),[35] TMJ ankylosis or fractures,[35] examination of the maxillary sinus,[36] orofacial trauma and fractures,[37] differences in airway volumes after rapid palatal expansion,[38] and implant applications.[39]
Some disadvantages of CT are:
Expensive,
Not available in every hospital,
Skips lesions far away from the sections,
Foreign objects like restoration and prosthetics create artifacts,
In addition, CT data is insufficient compared with other soft-tissue imaging techniques.[40]
Cone beam computerized tomography (CBCT)
Craniofacial CBCT devices [Figure 1] are designed to overcome some of the limitations of conventional CT scanning devices.[41] There are a lot of differences among the CBCT devices including patient positioning, scan time, resolution, radiation dose, and clinical ease of use of cross-sectional area.[42] In addition, while some CBCT devices scan all head area, others scan only the chin area.
Figure 1.
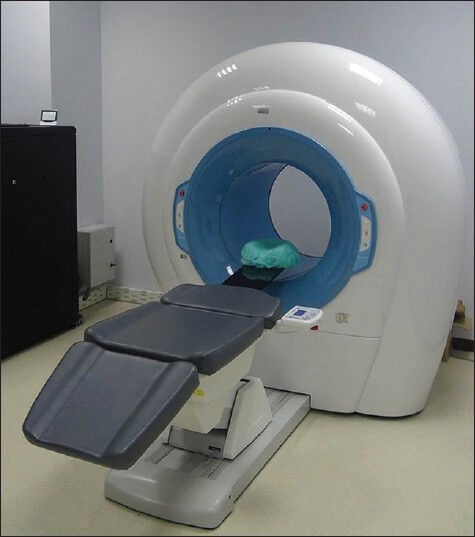
Cone beam computerized tomography for craniofacial imaging
With the cone-beam systems, dental therapists can achieve 3D (volumetric) data with very low radiation dose at one time.[43] At the same time, CBCT allows re-alignment of 2-dimensional images in coronal, sagittal, oblique, and various incline planes [Figure 2]. When we compare CBCT with CT, patients’ visualization with less radiation dose is possible.[42,44] CBCT devices provide 15 times less radiation dose than conventional CT scanners do. The radiation dose of CBCT equals to a dose of average 12 panoramic radiographs.[11]
Figure 2.
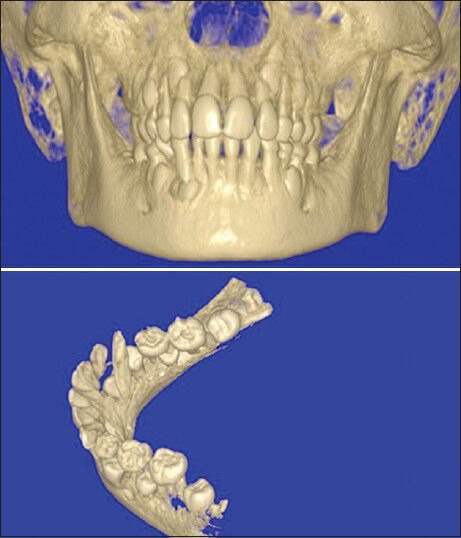
CBCT images of craniofacial structure obtained from various incline planes
In orthodontics, craniofacial images obtained with CBCT devices provide important information in different categories. Complex relation between treatment, development, and craniofacial data can be explained or data can be used as an independent solution for one and more of the following categories:[40]
Determination of normal and abnormal anatomy
Making decision on root length and alignment
Jaw size and distance of examined teeth
Determination of relationship between jaw size and examined teeth size
Determination of 3D maxillo-mandibular relationship
Determination of the status of the TMJ
Determination of the effects of orthodontic treatment in craniofacial anatomy
Detection and localization of impacted or supernumerary teeth.
The ability of providing 3D images of craniofacial structures with minimum amount of distortion has increased the availability of this technology.[11,40]
Advantages of CBCT in orthodontics
Cost: CBCT devices have gained smaller size, thanks to technological developments. The cost of CBCT imaging is very low compared to computerized tomography. Image processing is easier because it is limited to the head and face. Maintenance cost of CBCT devices is much less
Reduction of radiation dose: Referring to the results of the different studies, CBCT devices emit up to 98% less radiation. CBCT devices emit on average 36.9-50.3 microsievert (μSv) of radiation dose: On average, 1.320 to 3.324-μSv for the mandible and 1.031 to 1.420 μSv for maxilla
Quick scan: With CBCT devices, all raw data are obtained in a single turn. In this way, the patient's length of stay is reduced and the device increases patient satisfaction
Dimensional reconstruction feature: The most important advantage of CBCT is possible to display and arrange 3D data in personal computers
Image processing: Various comprehensive softwares for implant placement and orthodontic measurements are available.
Disadvantages of CBCT in orthodontics
Cone beam geometry, sensor sensitivity, and contrast resolutions as well as some other limitations lead to some disadvantages in the CBCT technique:
The main factor of weakness in image quality is image artifacts, such as metal brackets and restorations.
The actual color of the skin and soft tissue images cannot be determined.[11]
Unwanted patient movement may cause image disorder.
Price of these devices is more expensive than conventional X-ray equipment, and these devices require more space.
Radiation scattering may occur preventing of image monitoring.
CBCT has not only relatively limited capacity in displaying soft tissues, but also has an arguably place for investigation of hard tissue of the head and face.
CBCT in orthodontic application
Impacted teeth and intraoral anomalies
In determining position of the ectopic cuspids accurately, CBCT can be used for the establishment of therapeutic strategies to employ minimal invasive surgery.[45] Although the pathologies created by ectopic teeth and surrounding structures can be identified with conventional radiograph, the studies being conducted with CBCT scans give more accurate data regarding the actual relationships between impacted teeth and adjacent teeth, and possible root resorptions [Figure 2].[46]
Another application area of CBCT is to determine the position of oral abnormalities in patients. Previous studies showed that after using the CBCT, incidence of oral abnormalities has increased compared to the earlier studies.[45,47]
The nasopharyngeal airway analysis
CBCT technology has caused great progress in the nasopharyngeal airway analysis. While enlarging the airway is not a direct goal of orthodontic treatment, CBCT and lateral cephalographs are widely used for airway measurements. As a result, either surgical removal of the adenoids/tonsils or obstructive sleep apnea therapy due to narrow airways can be applied if necessary.
The potency of CBCT to measure airway volumes has helped orthodontists for studying in airway volume differences as a result of rapid palatal expansion[48] and premolar extraction.[49] In both studies, airways were found to be unchanged after orthodontic treatment.
In another study using lateral cephalograms and CBCT, there was a moderate difference in upper airway area and volume measurements of 11 patients.[33]
Cleft lip/palate patients
Among different patient groups, CBCT is more important for individuals with congenital malformations.[50] Since the prevalence of cleft lip/palate (CL/P) is very high in population,[51,52] it is not unexpected that researches on CBCT imaging in orofacial deformities have concentrated on these patients. Since CBCT use in CL/P patients was found efficient in early clinical cases,[53] a great number of researchers estimated the alveolar cleft volume to assist pre-alveolar graft surgery.[54,55] The proper amount of graft material can be prepared via CBCT volumetric analyses to assure enough alveolar bone in CL/P patients. In addition, CBCT is also used for soft tissue evaluation of CL/P patients pre- and post-operatively.
Both conventional radiographs and CBCT imaging are principally used to assess mineralized tissues. Differences of nasal and labial tissues between the age-matched non-CL/P patients and CL/P patients without synchronous rhinoplasty and the CL/P patients with synchronous rhinoplasty were examined using CBCT. Nasal reconstruction conducted during primary lip repair is named as synchronous rhinoplasty. Based upon differences in soft tissue measurements from CBCT images among 3 groups, synchronous rhinoplasty is suggested to optimize nasal and labial appearance in CL/P patients.[56]
Temporomandibular joint (TMJ) morphology
Condylar head size, shape and position, the joint space can be evaluated in CBCT. The condyle is viewed from only lateral side in lateral cephalometric films, but with CBCT, frontal and axial cross-sections can be displayed. However, since CBCT is not sufficient to view the soft tissues, examination of disk structures in TMJ is difficult.[57]
CBCT image analyses
The front or profile photos can be converted to DICOM (Digital Imaging and Communications in Medicine) database with a new software programs. 3-dimensional view of the face can be created in any desired direction. Changing the image transparency, anatomic relationships between the hard and soft tissues can be defined. Changes in the appearance of the face after tooth movement, orthognathic surgery or other craniofacial treatment can be detected with CBCT image. In addition, models of images obtained from CBCT can be prepared with 3D Fotoscan devices.[58]
Three-dimensional superposition
Images of cranial structures taken at different times can be superimposed on pre-defined points using the 3-dimensional software. Measurements performed on these images are imported to a computer, and then growth changes and treatment progress are evaluated. Thus, stability and post-treatment assessment can be made with the help of 3D superposition.[58]
In addition, CBCT provides information about root inclination and torque, bone thickness and morphology at the points where mini-screws are decided to be implanted and osteotomy sites during surgical planning.[59]
The positions of the mandibular and maxillary incisor roots, the amount of bone in the posterior maxilla for distalization, the amount of bone available for the maxillary buccal segments for dental expansions, neighborhood between maxillary sinus and maxillary teeth roots can be examined before and after selected treatment procedure.[60]
Micro-computed tomography (MCT)
MCT is substantially the same as CT except that the reconstructed cross-sections are bounded to a much minor area [Figure 3]. 0.012 mm thin cross-sections can be taken with conventional CT, but MCT can be obtained with the nano-sized sections. MCT, a non-invasive and a non-destructive technique, is used for the analysis of mineralized tissues. The future of MCT lies in its capacity to sample input over a much minor volume than full body, considerably reducing the radiation exposure.
Figure 3.
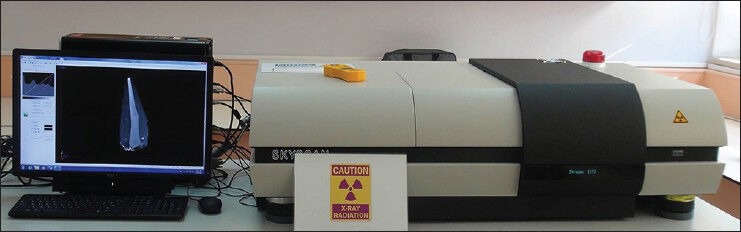
Micro-computed tomography for analysis of mineralized tissues with micro-sized sections
With the use of modern technology at X-ray sources and detectors, MCT devices have 10,000 times more resolution than medical CT scanners do.[61] The system has a micro focus X-ray source, a CCD camera, and a personal computer for control of the system. The X-ray radiation source with focal spot size of 10 mm is used to scan the objects. CCD camera provides high-resolution images. MCT gives important information about wound healing and micro vascular researches in orthopedics. The MCT devices are also used in researches related to endodontics, prosthetics, TMJ, and dental caries.[62,63] Current MCT scanning of bone has revealed accurate and precise information about bone stereology and micro architecture. This method has been used clinically to evaluate osteoblastic/osteoclastic alveolar remodeling as well as bone dehiscence and root resorption in orthodontics.[64,65] Osseo-integrated implants used for orthodontic anchorage can be evaluated with MCT.
3D laser scanning
As a less invasive method of capturing the face, laser scanning supplies 3D images for treatment planning or evaluating effects of orthodontic and especially orthognathic treatment. In addition, the 3D laser scanners can produce digital models.
However, this technique has several disadvantages for 3D scanning. For example:
Procedure is so slow that distortion occurs on the scanned image
While the scanner revolves around the patient's head, the patients should stay motionless for one minute or longer. Due to the potential patient movement and security issues related to laser, intraoral laser scanning is very difficult to obtain digital models[41]
Safety issues are important, such as exposing eyes to the laser beam, particularly in growing children
There is an inability to capture soft tissue surface texture, which results in difficulties in identification of landmarks due to surface color.[22]
Structured light technique
Because much of what is diagnosed in facial aesthetics need to be related to the deeper structures of bone and muscle, it can be feasible to investigate the face at its surface level only. Structured light scanning enables the 3-dimensional shape of the face in a simple way and without ionizing radiation. The result is a 3D shape of the patient's face, viewable on a computer screen.[66] 3D facial analyses are accessible now, and 3D superimposition disclosing treatment effects would come into use. The image is illuminated by the light, and taking a single image is sufficient in structured light technique.
The position of illuminated points in obtained image is necessary for 3D reconstruction of the object.[67] The main aim of this technique is to combine the facial shape and underlying radiographic data from other sources to conclude 3D structures for diagnosis, treatment goal, and evaluation of treatment results. Also, 3-dimensional images of the teeth can be obtained using the structured light technique in the mouth. However, to obtain high-concentration samples, the face needs to be illuminated a few times with random patterns of light.[68] This rises the capture time with increased probability of head action. In addition, the use of one imager does not assure an 180o (ear to ear) facial model, which is not convenient and has resulted in decreased applicability of this technique.[69] Structured light technique can be used to determine the position of the brackets correctly. Ora-Scanner (the first 3D hand-held intra-oral scanner) is based on structured light techniques. In this system, white light is used. Techalertpaisan and Kuroda[70] used 2 LCD projectors, a camera and a computer, to produce 3D image of face shape that may be altered, moved, or revolved lightly in all directions. This system requires at least 2 seconds to capture an image, which may be too long in avoiding the movements of babies and children. Another kind of structured light technique was presented by Curry et al.[71] This system has got 2 cameras and 1 projector. Hue coded light figure is projected on the face before obtaining every image. The displacement of the pattern enables the software to evaluate an accurate 3D model. Structured light figure, when united with stereophotogrammetry to measure the light figure precisely, ends up with the generation of an accurate 3D plan.
Sterophotogrametry
Stereophotogrammetry includes photographing a 3D object from 2 different coplanar planes in order to acquire a 3D reconstruction of the images [Figure 4]. This technique has proven to be very effective in the face display. It mentions to the private case with 2 cameras, arranged as a steropair, are used to recover 3D distances of features on the surface of the face.[72] The technique has been implemented clinically by using a mobile stereometric camera.[21] Contemporary stereophotogrammetry may be used to clear up accurate 3D skull mapping. In 1944, the first clinical use of stereo photogrammetry applied by Thalmann-Degan and recorded the changes that occur on the face of the patients as a result of orthodontic treatments.[21] Ras et al.[15] have developed a stereophotorammetric system that presents the 3D coordinates of any chosen facial landmarks. This system includes 2 synchronized semi-metric cameras installed on an outline with distance of 50 cm between them and located convergent with an angle of 15.[73]
Figure 4.

Stereophotogrammetry with 2 different coplanar planes for 3D images
Due to tissue reflections, hair and eyebrows intervention, change of posture between the different views and movements during imaging decrease the probability of obtaining the most accurate facial images. In addition, since laser or light cannot penetrate to excessively curved and reflective surfaces, certain structures, such as the eyes and ears, cannot give a good image.
3D facial morphometry (3DFM)
3D Facial Morphometry may be used in clinics after capturing the subject as a supplement to the cephalometric analyses. The system consists of 2 infrared cameras, a hardware for the recognition of markers and a software for the 3D rebuilding of landmarks’ coordinates.[16] Landmarks are positioned on the face and later covered with 2 mm semi-spherical reflective markers. An ultraviolet stroboscope is used to light up the projective markers. Two- sides’ determination is generally needed to acquire the whole face. Placement of landmarks on the face is labor-consuming and takes very long time. Repeatability of the landmarks determination is very difficult and questionable. Changes of facial statement between two achievement periods enhance size of error. This system cannot produce models to display the natural soft-tissue appearance of the face expression. In conclusion, it is not wise to use this system as equipment for making decisions on orthodontic treatment, and for communication between patients and orthodontists or surgeons.
Tuned-aperture computer tomography (TACT)
There are many shortcomings of current radiologic techniques. In 1990, the National Institute of Dental Research decided to support the improvement of a system for manufacturing 3D images tomosynthetically from a device including a multi-tube X-ray and X-ray charge-coupled device screen. The most comprehensive result of this effort is TACT system that may alter multiple 3D pictures.[74] Tuned-Aperture Computed Tomography or TACT (Wake Forest University, School of Medicine, Winston-Salem, North Caroline, USA) is developed by Richard Webber.[1] TACT is a low-dose 3-dimensional imaging system. A calibration or reference marker in the area of view to permit for synthetic reconstruction of the desired image plane is placed by the TACT technique. However, it does not meet the need for accurate control and information of the imaging geometry. The object and image sensor must be remain fixed in this technique, and the position of the X-ray source can be elective. The calibration marker permits to decide on the imaging geometry used to exhibit the absolute imaging from the final result image. This technique allows the processing of all resultant images into 3D volume. In fact, this method is used in medicine, but it can be used in the dentistry as well. The uses of TACT for dental purposes have been shown in several studies. TACT seems to have a greater diagnostic value in its ability to detect dental caries, impacted teeth, and to evaluate pre-implant images.[75] The future of TACT for orthodontics lies in its ability in evaluation of dento-alveolar bone volume, detection of root resorption, and evaluation of the TMJ disorders.[76]
Magnetic resonance imaging (MRI)
MRI operates by achieving a resonance signal from the hydrogen nucleus. Therefore, it is basically imaging of water in the tissue. MRI method is the highest contrast resolution medical imaging technique. Radio waves are sent to desired location for examination in a magnetic field. The energy produced from hydrogen atoms in the cells stimulated by radio waves are converted to numbers; they are processed on a computer and then converted to image. MRI is very convenient for the study of skeletal physiology, tumors, and the healing of grafts. Although MRI technique has a shorter history in the TMJ investigation, it is considered to be the gold standard for imaging of the TMJ.[77] If one needs detailed information about the intracapsular joint effusion, joint pain, and adhesion and perforation of articular disc, MRI is a preferred choice. The information provided by MRI, condylar erosion, osteopathy, and the determination of the position of the disk is successful in about 90%.[78]
Advantages of MRI in orthodontics:
It gives very valuable information about the position and morphology of disk and excellent soft-tissue resolution with radiation-free imaging technique
Based on the changes in the signal intensities, it can also display detailed osseous tissues
It can be safely used in patients who are allergic to the contrast agent
The images can be obtained without repositioning the patient
It also provides opportunity to examine inflammatory processes and scar tissues.
Disadvantages of MRI:
It requires expensive and advanced equipment
Unavailability in every medical center and dental office
It takes a long time to use in TMJ
It is contraindicated in the patients with claustrophobia.[27]
Stainless steel and other metals used in orthodontic brackets were shown to produce artifacts.[79] Therefore, patients undergoing orthodontic treatment should be carefully evaluated for MRI needs.
CONCLUSIONS
Need for high speed, high density, small size, and multifunctional device has driven the development of 3D imaging. New imaging techniques require expensive software and a lot of time to operate them. The future of 3D imaging seems to be faster and more flexible robotic devices.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Webber RL, Horton RA, Tyndall DA, Ludlow JB. Tuned-aperture computed tomography (TACT). Theory and application for three-dimensional dento-alveolar imaging. Dentomaxillofac Radiol. 1997;26:53–62. doi: 10.1038/sj.dmfr.4600201. [DOI] [PubMed] [Google Scholar]
- 2.Ucar FI, Sekerci AE, Uysal T, Bengi AO. Standardization of records in orthodontics. Part 2: Craniofacial imaging techniques. Turkish Journal of Orthodontics. 2012;25:167–87. [Google Scholar]
- 3.Hajeer MY, Millett DT, Ayoub AF, Siebert JP. Applications of 3D imaging in orthodontics: Part 1. J Orthod. 2004;31:62–70. doi: 10.1179/146531204225011346. [DOI] [PubMed] [Google Scholar]
- 4.Plooij JM, Maal TJ, Haers P, Borstlap WA, Kuijpers-Jagtman AM, Bergé SJ. Digital three-dimensional image fusion processes for planning and evaluating orthodontics and orthognathic surgery. A systematic review. Int J Oral Maxillofac Surg. 2011;40:341–52. doi: 10.1016/j.ijom.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 5.Mavili ME, Canter HI, Saglam-Aydinatay B, Kamaci S, Kocadereli I. Use of three-dimensional medical modeling methods for precise planning of orthognathic surgery. J Craniofac Surg. 2007;18:740–7. doi: 10.1097/scs.0b013e318069014f. [DOI] [PubMed] [Google Scholar]
- 6.Karadeniz EI, Gonzales C, Elekdag-Turk S, Isci D, Sahin-Saglam AM, Alkis H, et al. The effect of fluoride on orthodontic tooth movement in humans. A two-and three-dimensional evaluation. Aust Orthod J. 2011;27:94–101. [PubMed] [Google Scholar]
- 7.Andresen V. Three contributions to orthodontological diagnosis. International Journal of Orthodontia, Oral Surgery and Radiography. 1926;12:235–51. [Google Scholar]
- 8.Van Loon J. A new method for indicating normal and abnormal relations of the teeth to the facial lines. Dental Cosmos. 1915;57:1093–101. [Google Scholar]
- 9.Schwarz R. New cephalometric method and apparatus and its application to orthodontia. Int J Orthod Oral Surg Radiol. 1925;11:989–1017. [Google Scholar]
- 10.Herman GT. 2nd ed. New York: Springer; 2009. Fundamentals of computerized tomography: Image reconstruction from projection; pp. 1–17. [Google Scholar]
- 11.Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006;72:75–80. [PubMed] [Google Scholar]
- 12.Ritman EL. Micro-computed tomography-current status and developments. Annu Rev Biomed Eng. 2004;6:185–208. doi: 10.1146/annurev.bioeng.6.040803.140130. [DOI] [PubMed] [Google Scholar]
- 13.Paddock SW, Eliceiri KW. Laser scanning confocal microscopy: History, applications, and related optical sectioning techniques. Methods Mol Biol. 2014;1075:9–47. doi: 10.1007/978-1-60761-847-8_2. [DOI] [PubMed] [Google Scholar]
- 14.Fechteler P, Eisert P, Rurainsky J. Fast and high resolution 3D face scanning. (III-4).ICIP. 2007;3:III–81. [Google Scholar]
- 15.Ras F, Habets LL, van Ginkel FC, Prahl-Andersen B. Quantification of facial morphology using stereophotogrammetry-demonstration of a new concept. J Dent. 1996;24:369–74. doi: 10.1016/0300-5712(95)00081-x. [DOI] [PubMed] [Google Scholar]
- 16.Ferrario VF, Sforza C, Poggio CE, Serrao G. Facial three-dimensional morphometry. Am J Orthod Dentofacial Orthop. 1996;109:86–93. doi: 10.1016/s0889-5406(96)70167-1. [DOI] [PubMed] [Google Scholar]
- 17.Edelman RR, Hesselink J, Zlatkin M. Saunders; 2005. Clinical magnetic resonance imaging: 3-volume set. [Google Scholar]
- 18.Broadbent BH. A new x-ray technique and its application to orthodontia. Angle Orthod. 1931;1:45–66. [Google Scholar]
- 19.Athanasiou AE. London: Mosby-Wolfe; 1997. Orthodontic cephalometry; pp. 241–92. [Google Scholar]
- 20.Nalçaci R, Oztürk F, Sökücü O. A comparison of two-dimensional radiography and three-dimensional computed tomography in angular cephalometric measurements. Dentomaxillofac Radiol. 2010;39:100–6. doi: 10.1259/dmfr/82724776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burke PH, Beard FH. Stereophotogrammetry of the face: A preliminary investigation into the accuracy of a simplified system evolved for contour mapping by photography. Am J Orthod. 1967;53:769–82. doi: 10.1016/0002-9416(67)90121-2. [DOI] [PubMed] [Google Scholar]
- 22.Baumrind S. Towards a general model for clinical craniofacial research. In: Hunter WS, Carlson DS, editors. Essay in Honor of Robert Moyers. Ann Arbor: The University of Michigan; 1991. [Google Scholar]
- 23.Han UK, Vig KW, Weintraub JA, Vig PS, Kowalski CJ. Consistency of orthodontic treatment decisions relative to diagnostic records. Am J Orthod Dentofacial Orthop. 1991;100:212–9. doi: 10.1016/0889-5406(91)70058-5. [DOI] [PubMed] [Google Scholar]
- 24.Hixon EH. The norm concept and cephalometrics. Am J Orthod. 1956;42:898–906. [Google Scholar]
- 25.Moyers RE, Bookstein FL. The inappropriateness of conventional cephalometrics. Am J Orthod. 1979;75:599–617. doi: 10.1016/0002-9416(79)90093-9. [DOI] [PubMed] [Google Scholar]
- 26.Baumrind S, Frantz RC. The reliability of head film measurements: 1. Landmark identification. Am J Orthod. 1971;60:111–27. doi: 10.1016/0002-9416(71)90028-5. [DOI] [PubMed] [Google Scholar]
- 27.Vig PS. Current Controversies in Orthodontics. Chicago: Quintessence Publishing; 1991. Orthodontic controversies: Their origins, consequences and resolution; pp. 269–310. [Google Scholar]
- 28.Gron P. A geometrical evaluation of image size in dental radiography. J Dent Res. 1960;39:289–301. doi: 10.1177/00220345600390021101. [DOI] [PubMed] [Google Scholar]
- 29.Singh IJ, Savara BS. Norms of size and annual increments of seven anatomical measures of maxillae in girls from three to sixteen years of age. Angle Orthod. 1966;36:312–24. doi: 10.1043/0003-3219(1966)036<0312:NOSAAI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Dean D, Hans MG, Bookstein FL, Subramanyan K. Three-dimensional Bolton-brush growth study landmark data: Ontogeny and sexual dimorphism of the Bolton standards cohort. Cleft Palate Craniofac J. 2000;37:145–56. doi: 10.1597/1545-1569_2000_037_0145_tdbbgs_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 31.Subramanyan K, Dean D. Scanned bi-orthogonal radiographs as a source for 3D cephalometric data. SPIE. 1996;34:717–24. [Google Scholar]
- 32.Udupa JK, Herman GT. Boca Raton: CRC Press; 1991. 3D Imaging in medicine. [Google Scholar]
- 33.Aboudara CA, Hatcher D, Nielsen IL, Miller A. A three dimensional evaluation of the upper airway in adolescents. Orthod Craniofac Res. 2003;6(Suppl 1):173–5. doi: 10.1034/j.1600-0544.2003.253.x. [DOI] [PubMed] [Google Scholar]
- 34.Rabinov K, Kell T, Jr, Gordon PH. CT of the salivary glands. Radiol Clin North Am. 1984;22:145–59. [PubMed] [Google Scholar]
- 35.Westesson PL, Katzberg RW, Tallents RH, Sanchez-Woodworth RE, Svensson SA. CT and MR of the temporomandibular joint: Comparison with autopsy specimens. AJR Am J Roentgenol. 1987;148:1165–71. doi: 10.2214/ajr.148.6.1165. [DOI] [PubMed] [Google Scholar]
- 36.Bolger WE, Butzin CA, Parsons DS. Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope. 1991;101:56–64. doi: 10.1288/00005537-199101000-00010. [DOI] [PubMed] [Google Scholar]
- 37.Zilkha A. Computed tomography in facial trauma. Radiology. 1982;144:545–8. doi: 10.1148/radiology.144.3.7100469. [DOI] [PubMed] [Google Scholar]
- 38.Görgülü S, Gokce SM, Olmez H, Sagdic D, Ors F. Nasal cavity volume changes after rapid maxillary expansion in adolescents evaluated with 3-dimensional simulation and modeling programs. Am J Orthod Dentofacial Orthop. 2011;140:633–40. doi: 10.1016/j.ajodo.2010.12.020. [DOI] [PubMed] [Google Scholar]
- 39.Ito K, Gomi Y, Sato S, Arai Y, Shinoda K. Clinical application of a new compact CT system to assess 3-D images for the preoperative treatment planning of implants in the posterior mandible a case report. Clin Oral Implants Res. 2001;12:539–42. doi: 10.1034/j.1600-0501.2001.120516.x. [DOI] [PubMed] [Google Scholar]
- 40.Harorli A, Akgul M, Dagistan S. Ataturk University Press; 2006. Radiology in Dentistry. [Google Scholar]
- 41.Halazonetis DJ. From 2-dimensional cephalograms to 3-dimensional computed tomography scans. Am J Orthod Dentofacial Orthop. 2005;127:627–37. doi: 10.1016/j.ajodo.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 42.Kau CH, Richmond S, Palomo JM, Hans MG. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. 2005;32:282–93. doi: 10.1179/146531205225021285. [DOI] [PubMed] [Google Scholar]
- 43.White SC. Cone-beam imaging in dentistry. Health Phys. 2008;95:628–37. doi: 10.1097/01.HP.0000326340.81581.1a. [DOI] [PubMed] [Google Scholar]
- 44.Tsiklakis K, Donta C, Gavala S, Karayianni K, Kamenopoulou V, Hourdakis CJ. Dose reduction in maxillofacial imaging using low dose cone beam CT. Eur J Radiol. 2005;56:413–7. doi: 10.1016/j.ejrad.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 45.Mah JK, Danforth RA, Bumann A, Hatcher D. Radiation absorbed in maxillofacial imaging with a new dental computed tomography device. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:508–13. doi: 10.1016/s1079-2104(03)00350-0. [DOI] [PubMed] [Google Scholar]
- 46.Baysal A, Karadede I, Hekimoglu S, Ucar F, Ozer T, Veli I, et al. Evaluation of root resorption following rapid maxillary expansion using cone-beam computed tomography. Angle Orthod. 2012;82:488–94. doi: 10.2319/060411-367.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ericson S, Kurol PJ. Resorption of incisors after ectopic eruption of maxillary canines: A CT study. Angle Orthod. 2000;70:415–23. doi: 10.1043/0003-3219(2000)070<0415:ROIAEE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 48.Zhao Y, Nguyen M, Gohl E, Mah JK, Sameshima G, Enciso R. Oropharyngeal airway changes after rapid palatal expansion evaluated with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;137(Suppl 4):S71–8. doi: 10.1016/j.ajodo.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 49.Valiathan M, El H, Hans MG, Palomo MJ. Effects of extraction versus non-extraction treatment on oropharyngeal airway volume. Angle Orthod. 2010;80:1068–74. doi: 10.2319/010810-19.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Korbmacher H, Kahl-Nieke B, Schöllchen M, Heiland M. Value of two cone-beam computed tomography systems from an orthodontic point of view. J Orofac Orthop. 2007;68:278–89. doi: 10.1007/s00056-007-0653-x. [DOI] [PubMed] [Google Scholar]
- 51.Chien PC, Parks ET, Eraso F, Hartsfield JK, Roberts WE, Ofner S. Comparison of reliability in anatomical landmark identification using two-dimensional digital cephalometrics and three-dimensional cone beam computed tomography in vivo. Dentomaxillofac Radiol. 2009;38:262–73. doi: 10.1259/dmfr/81889955. [DOI] [PubMed] [Google Scholar]
- 52.Ludlow JB, Gubler M, Cevidanes L, Mol A. Precision of cephalometric landmark identification: Cone-beam computed tomography vs conventional cephalometric views. Am J Orthod Dentofacial Orthop. 2009;136:312.e1–10. doi: 10.1016/j.ajodo.2008.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wörtche R, Hassfeld S, Lux CJ, Müssig E, Hensley FW, Krempien R, et al. Clinical application of cone beam digital volume tomography in children with cleft lip and palate. Dentomaxillofac Radiol. 2006;35:88–94. doi: 10.1259/dmfr/27536604. [DOI] [PubMed] [Google Scholar]
- 54.Shirota T, Kurabayashi H, Ogura H, Seki K, Maki K, Shintani S. Analysis of bone volume using computer simulation system for secondary bone graft in alveolar cleft. Int J Oral Maxillofac Surg. 2010;39:904–8. doi: 10.1016/j.ijom.2010.04.050. [DOI] [PubMed] [Google Scholar]
- 55.Quereshy FA, Barnum G, Demko C, Horan M, Palomo JM, Baur DA, et al. Use of cone beam computed tomography to volumetrically assess alveolar cleft defects-preliminary results. J Oral Maxillofac Surg. 2012;70:188–91. doi: 10.1016/j.joms.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 56.Miyamoto J, Nakajima T. Anthropometric evaluation of complete unilateral cleft lip nose with cone beam CT in early childhood. J Plast Reconstr Aesthet Surg. 2010;63:9–14. doi: 10.1016/j.bjps.2008.08.071. [DOI] [PubMed] [Google Scholar]
- 57.Gribel BF, Gribel MN, Manzi FR, Brooks SL, McNamara JA., Jr From 2D to 3D: An algorithm to derive normal values for 3-dimensional computerized assessment. Angle Orthod. 2011;81:3–10. doi: 10.2319/032910-173.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.White AJ, Fallis DW, Vandewalle KS. Analysis of intra-arch and interarch measurements from digital models with 2 impression materials and a modeling process based on cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;137:456.e1–9. doi: 10.1016/j.ajodo.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 59.Cevidanes LH, Styner MA, Proffit WR. Image analysis and superimposition of 3-dimensional cone-beam computed tomography models. Am J Orthod Dentofacial Orthop. 2006;129:611–8. doi: 10.1016/j.ajodo.2005.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Leuzinger M, Dudic A, Giannopoulou C, Kiliaridis S. Root-contact evaluation by panoramic radiography and cone-beam computed tomography of super-high resolution. Am J Orthod Dentofacial Orthop. 2010;137:389–92. doi: 10.1016/j.ajodo.2009.10.027. [DOI] [PubMed] [Google Scholar]
- 61.Stampanoni M, Wyss P, Abela R, Borchert GL, Vermeulen D, Ruegsegger P. International symposium on optical science and technology: International society for optics and photonics; 2002. X-ray tomographic microscopy at the Swiss light source; pp. 42–53. [Google Scholar]
- 62.Keleº A, Alcin H, Kamalak A, Versiani MA. Oval-shaped canal retreatment with self-adjusting file: A micro-computed tomography study. Clin Oral Investig. 2013 doi: 10.1007/s00784-013-1086-0. DOI: 10.1007/s00784-013-1086-0. [DOI] [PubMed] [Google Scholar]
- 63.Borba M, Miranda WG, Jr, Cesar PF, Griggs JA, Bona AD. Evaluation of the adaptation of zirconia-based fixed partial dentures using micro-CT technology. Braz Oral Res. 2013;27:396–402. doi: 10.1590/S1806-83242013000500003. [DOI] [PubMed] [Google Scholar]
- 64.King AD, Turk T, Colak C, Elekdag-Turk S, Jones AS, Petocz P, et al. Physical properties of root cementum: Part 21. Extent of root resorption after the application of 2.5° and 1.5° tips for 4 weeks. A microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2011;140:e299–305. doi: 10.1016/j.ajodo.2011.06.023. [DOI] [PubMed] [Google Scholar]
- 65.Karadeniz EI, Gonzales C, Nebioglu-Dalci O, Dwarte D, Turk T, Isci D, et al. Physical properties of root cementum: Part 20. Effect of fluoride on orthodontically induced root resorption with light and heavy orthodontic forces for 4 weeks: A microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2011;140:e199–210. doi: 10.1016/j.ajodo.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 66.Underhill TE, Chilvarquer I, Kimura K, Langlais RP, McDavid WD, Preece JW, et al. Radiobiologic risk estimation from dental radiology: Part 1. Absorbed doses to critical organs. Oral Surg Oral Med Oral Pathol. 1988;66:111–20. doi: 10.1016/0030-4220(88)90077-1. [DOI] [PubMed] [Google Scholar]
- 67.Yamamoto K, Hayakawa Y, Kousuge Y, Wakoh M, Sekiguchi H, Yakushiji M, et al. Diagnostic value of tuned-aperture computed tomography versus conventional dentoalveolar imaging in assessment of impacted teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:109–18. doi: 10.1067/moe.2003.17. [DOI] [PubMed] [Google Scholar]
- 68.Nguyen CX, Nissanov J, Öztürk C, Nuveen MJ, Tuncay OC. Three-dimensional imaging of the craniofacial complex. Clin Orthod Res. 2000;3:46–50. doi: 10.1034/j.1600-0544.2000.030108.x. [DOI] [PubMed] [Google Scholar]
- 69.Tuncay OC. Three-dimensional imaging and motion animation. Semin Orthod. 2001;7:244–50. [Google Scholar]
- 70.Techalertpaisarn P, Kuroda T. Three-dimensional computer-graphic demonstration of facial soft tissue changes in mandibular prognathic patients after mandibular sagittal ramus osteotomy. Int J Adult Orthodon Orthognath Surg. 1998;13:217–25. [PubMed] [Google Scholar]
- 71.Curry S, Baumrind S, Carlson S, Beers A, Boyd R. Integrated three-dimensional ciraniofacial mapping at the Craniofacial Research Instrumentation Laboratory/University of the Pacific. Seminars in Orthodontics. 2001;7:258–65. [Google Scholar]
- 72.Hajeer MY, Ayoub AF, Millett DT, Bock M, Siebert JP. Three-dimensional imaging in orthognathic surgery: The clinical application of a new method. Int J Adult Orthodon Orthognath Surg. 2002;17:318–30. [PubMed] [Google Scholar]
- 73.Larheim TA. Current trends in temporomandibular joint imaging. Oral surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:555–76. doi: 10.1016/s1079-2104(05)80154-4. [DOI] [PubMed] [Google Scholar]
- 74.Webber RL, Horton RA. Tuned-aperture computed tomography (TACT). Theory and application in dental radiology. In: Farman AG, editor. Avances in maxillofacial imaging. BV: Elsevier Science; 1997. pp. 359–62. [Google Scholar]
- 75.Mah J, Enciso R, Jorgensen M. Management of impacted cuspids using 3-D volumetric imaging. J Calif Dent Assoc. 2003;31:835–41. [PubMed] [Google Scholar]
- 76.Bookstein FL. The geometry of craniofacial growth invariants. Am J Orthod. 1983;83:221–34. doi: 10.1016/0002-9416(83)90086-6. [DOI] [PubMed] [Google Scholar]
- 77.van Dijke CF, Kirk BA, Peterfy CG, Genant HK, Brasch RC, Kapila S. Arthritic temporomandibular joint: Correlation of macromolecular contrast-enhanced MR imaging parameters and histopathologic findings. Radiology. 1997;204:825–32. doi: 10.1148/radiology.204.3.9280267. [DOI] [PubMed] [Google Scholar]
- 78.Robb RA. The dynamic spatial reconstructor: An x-ray video-fluoroscopic CT scanner for dynamic volume imaging of moving organs. IEEE Trans Med Imaging. 1982;1:22–33. doi: 10.1109/TMI.1982.4307545. [DOI] [PubMed] [Google Scholar]
- 79.Mckee IW, Williamson PC, Lam EW, Heo G, Glover KE, Major PW. The accuracy of 4 panoramic units in the projection of mesiodistal tooth angulations. Am J Orthod Dentofacial Orthop. 2002;121:166–75. doi: 10.1067/mod.2002.119435. [DOI] [PubMed] [Google Scholar]


