Abstract
Introduction:
The aim of this in vitro study was to evaluate the bond strength of Photo-Activated Disinfection (PAD) system to dentin with different root canal sealers by using a push-out test design.
Materials and Methods:
A total of 30 extracted mandibular premolar teeth with single and straight roots were used. The crowns were removed and the root canals were prepared by using ProTaper rotary files. The smear layer was removed and the roots were randomly divided into two groups (n = 15) according to the use of PAD system as the final disinfecting agent. Each group was then divided into 6 (n = 5) subgroups and obturated with gutta-percha and 3 different root canal sealers. The groups were Group 1: Sodium hypochlorite (NaOCl) + ethylenediaminetetraacetic acid (EDTA)-AH Plus sealer; Group 2: NaOCl + EDTA + PAD-AH Plus; Group 3: NaOCl + EDTA-Sealapex; Group 4: NaOCl + EDTA + PAD-Sealapex; Group 5: NaOCl + EDTA-mineral trioxide aggregate (MTA)-Fiallapex; and Group 6: NaOCl + EDTA + PAD-MTA-Fillapex. 1-mm thickness horizontal sections (n: 5 × 4 = 20) were sliced for the push-out bond strength measurement.
Results:
Group 3 and 4 showed significantly lower bond strengths compared with all the other groups (P < 0.05). No statistically significant difference was found among Groups 1, 2 and 5, but there was statistically significant difference between Group 5 and 6 (P < 0.05).
Conclusion:
This in vitro study indicated that the PAD system adversely affected the bond strength of the MTA Fillapex root canal sealer.
Keywords: AH Plus, bond strength, mineral trioxide aggregate Fillapex, photo-activated disinfection, Sealapex
INTRODUCTION
Successful obturation of the root canal system depends upon preparing, shaping, disinfecting and hermetically sealing the root canal system. During and after preparation, disinfection of the root canal is an important factor in the success of the treatment. Sodium hypochlorite (NaOCl) is the most commonly used root canal irrigation solution to date due to its antimicrobial and tissue-dissolving properties. However, it does not completely disinfect the root canal system.[1] Thus, an additional disinfection agent is essential. Photo-activated disinfection (PAD) is a recently available disinfectant option that helps to reduce the number of microorganisms in artificial root canals.[2] PAD uses light of a specific wavelength to activate a photo-sensitizing dye in the presence of oxygen.[3] This technique has been shown to be successful in eliminating all cultivable bacteria in the root canal.[4]
Various materials have been used for hermetic obturation of the root canal in the past. Gutta-percha and a traditional root canal sealer are the most commonly used and accepted materials for hermetic root canal obturation.[5] Gutta-percha is an impermeable core material, but leakage between the sealer and the dentin and the sealer and the Gutta-percha, in addition to voids within the sealer, may lead to treatment failure.[6] Many factors affect the sealing ability of the sealer such as irrigation or the disinfection agent and the type and the quality of the sealer.
AH Plus is an epoxy resin–based root canal sealer, which has been widely used for root canal obturation. It has acceptable physical properties,[7] good sealing ability, good adhesion to root canal walls and satisfactory biocompatibility.[8] Sealapex is a calcium hydroxide–based root canal sealer, which has been used since 1980. It has good sealing ability,[9] exhibits volumetric expansion during setting[10] and is resistant to long-term microleakage.[9] Mineral trioxide aggregate (MTA) Fillapex is a calcium silicate–based root canal sealer. According to the manufacturer, it contains MTA, salicylate resin, natural resin, diluting resins, nanoparticulated resin, bismuth and silica.
Several studies evaluated the effect of different irrigation solutions on the bond strength of root canal sealers. However, no study could be found evaluating the effect of the PAD system on the bond strength of different root canal sealers. The aim of this in vitro study was to evaluate and compare the effect of the PAD system on the bond strength of AH Plus, Sealapex and MTA Fillapex root canal sealers using the push-out test design.
MATERIALS AND METHODS
Preparation of specimens
A total of 30 extracted human mandibular premolar teeth with single and straight roots were used in this study. The external surfaces of the teeth were cleaned with periodontal curettes and maintained in 0.1% thymol solution. The crowns were removed with a water-cooled diamond saw and the roots were standardized to a length of 15 mm.
The #15 K-files (DiaDent, Chongju, Korea) were placed into the root canals and working lengths were determined 1 mm beyond the apex. The root canals were then prepared with ProTaper (Dentsply Maillefer, Ballaigues, Switzerland) rotary files to the size of F3 file. The root canals were irrigated with 2 ml of sterile saline solution after each instrumentation. The canals were irrigated with 3 ml of 5.25% NaOCl (Wizard, Ankara, Turkey) for 1 min, followed by 3 ml 17% ethylenediaminetetraacetic acid and then 5 ml of distilled water for 1 min to effectively remove the smear layer. The specimens were then randomly divided into 2 groups (n = 15) according to the use of the PAD system as the final disinfection agent. In the first 15 teeth, the PAD solution was injected into the root canal using a sterile endodontic micro-needle (gauge 27). The liquid was then agitated in each canal for 60 s using #30 K-files. The emitter was inserted 3 mm above the apex and light cured for 20 s. All the samples were then dried with absorbent paper points and each group was divided into 3 (n = 5) subgroups. All the samples were obturated with the lateral condensation technique using gutta-percha and 3 different root canal sealers: AH Plus sealer (Dentsply Maillefer), Sealapex (Kerr, Italia) and MTA Fillapex (Angelus Industria de Produtos Odontologicos S/A, Londrina, Brazil). Excess Gutta-percha was removed with a hot instrument and condensed vertically. All the specimens were stored at 37°C and 95% humidity for 1 week to allow sufficient setting time each root was then cut perpendicular to the long axis by using an Isomet slow-speed saw under water cooling. 1 mm thick horizontal sections from the coronal and mid-thirds of each root (n: 5 × 4 = 20) were sliced for the push-out bond strength measurement [Figure 1].
Figure 1.

1 mm thickness of horizontal sections that taken from the coronal and mid-thirds of each root for the push-out bond strength measurement
Push-out test
Push-out test was accomplished by using a 1-mm diameter cylindrical stainless steel plunger and applying a constant compressive load at a speed of 0.5 mm/min until bond failure occurred. Bond failure load was noted when a sharp decline was observed on the complete dislodgement of the root filling material. Results were calculated by dividing the load in Newton's by the area of the bonded interface.
Statistical analysis
The data were converted to MPa and statistically analyzed using one-way ANOVA and the post-hoc Tukey test with significance set at P < 0.05.
RESULTS
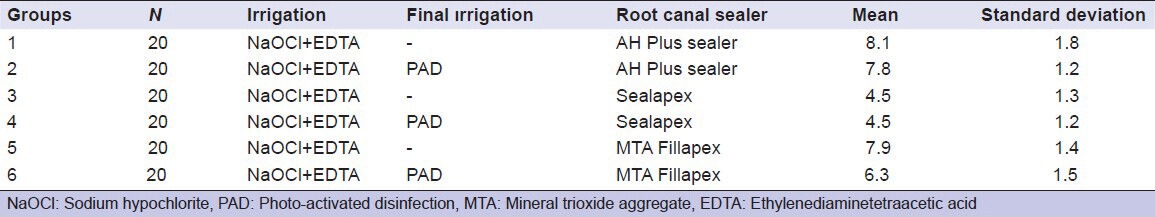
The means and standard deviations of the push-out bond strength (in MPa) of the root canal sealers were shown in Table 1. Comparing the results, there was a significant difference among the groups. The Sealapex groups (Group 3 and Group 4) showed statistically lower bond strength compared with the other groups (P < 0.05). There was no significant difference between Groups 1, 2 and 5. However, there was a statistically significant difference between Groups 5 and 6 (P < 0.05). And also there was a statistically significant difference between Groups 1, 2 and 6. According to the results of this study, the PAD system affected the bond strength of the MTA Fillapex root canal sealer.
Table 1.
Mean push-out bond strengths and standard deviations of groups in Mpa
DISCUSSION
Disinfection of the root canals with an irrigation solution is very important for the success of root canal treatment. The PAD system is an additional disinfection agent, which aids deep disinfection of the root canal system, thereby reducing numbers of microorganisms in artificial root canals. However, both irrigation solutions and disinfection agents change the chemical and structural composition of root canal dentin, as well as its permeability[11] and this may affect the sealing ability of the root canal sealers.[12] The importance of the adhesive properties of root canal sealers has been highlighted in many studies.[13,14,15]
Several studies have used various techniques such as leakage, micro-tensile, shear bond and push-out bond strength methods to analyze the sealing ability of root canal sealers. In this study, a push-out bond strength test was used. Leakage studies have drawbacks, as does the micro-tensile method, which can result in premature bond failure when cutting the specimens.[16] The ability of the push-out test to evaluate the bonding strength surpasses that of other tests because it generates parallel fractures in the interfacial area of dentin-bonding.[17] Thus, this test has become popular recently.[16] However, a limitation of the push-out test is that it creates non-uniform stress distribution.[18] We prevented this limitation in this study by using 1 mm thick slices.
Removal of the smear layer provides better adhesion of the sealers to the dentin and this plays an important role in the success of root canal treatment.[19] For this reason, the smear layer was removed to evaluate the sealing ability of the root canal sealers to the dentin in the present study. In addition, the length of the samples was adjusted to 15 mm to avoid anatomical variations and to standardize the slices.
There are a wide variety of commercially available root canal sealers and their physical properties are different. We investigated sealers based on calcium hydroxide (Sealapex), epoxy resin (AH Plus) and calcium silicate (MTA Fillapex) to determine their sealing ability when the root canals were finally disinfected with the PAD system. To the best of our knowledge, this is the first study to evaluate the sealing ability of 3 different root canal sealers using the PAD system.
All groups in this study showed measurable adhesive properties and the results showed that there was a significant difference between the groups. The resin-based AH Plus root canal sealer can be considered as a gold standard material for testing the sealing ability of root canal sealers.[20] In this study, we used the AH Plus root canal sealer as a control group and found that the PAD system did not adversely affect the sealing ability of the AH Plus root canal sealer.
Cobankara et al.[21] studied the sealing ability of 4 root canal sealers using the fluid filtration method and found that Sealapex performed better than AH Plus sealer. Yücel et al.[22] studied the sealing ability of AH Plus, AH 26, Sealapex and Ketac-Endo canal sealers in a bacterial leakage study. They found no statistically significant differences between AH Plus and the Sealapex root canal sealer. Vasconcelos et al.[23] studied the sealing ability of 5 different root canal sealers using the fluid filtration method and found that AH Plus root canal sealer performed better sealing ability than Sealapex. In the present study, Sealapex showed reduced bond strength compared with AH Plus and MTA Fillapex root canal sealers. This may be due to Sealapex containing calcium oxide, which causes water absorption and volumetric expansion during setting.[10] As a result, the solubility of Sealapex may be increased and its adhesion may be decreased.[23]
According to the results of this study, there was no statistically significant difference in the sealing ability of the sealer in the Sealapex group, irrespective of whether the PAD system was used as a final disinfectant agent. This indicates that the PAD system did not negatively affect the sealing ability of the Sealapex root canal sealer to dentin.
The calcium silicate–based MTA Fillapex root canal sealer contains resins, silica, bismuth trioxide and MTA. Sagsen et al.[24] evaluated the bond strength of 2 new calcium silicate–based and AH Plus endodontic sealers and found that MTA Fillapex had lower push-out bond values than the AH Plus sealer. Assmann et al.[20] studied the bond strength of MTA Fillapex, Endo-CPM and AH Plus root canal sealers and found no statistically significant difference between the AH Plus and the MTA Fillapex sealers. Similarly, in this study, there was no statistically significant difference between the MTA Fillapex sealer and the AH Plus root canal sealer. The present study supports the findings of Assmann et al.[20] This may be explained by similarities between the composition of MTA Fillapex and resin-based root canal sealers.[25]
The results of this study also revealed a statistically significant difference in the MTA Fillapex group when the PAD system used was used as a final irrigant. Thus, the PAD system appeared to negatively affect the bonding of the MTA Fillapex root canal sealer.
MTA Fillapex contains MTA. When set sealer comes into contact with phosphate-containing fluids, calcium and hydroxyl ions are released.[26] This has an adverse effect on the adhesion of MTA Fillapex. In addition, in manufacturing MTA Fillapex, the original formulation of MTA is altered to improve its viscosity, setting time and adhesion,[27] all of which affect the composition of the sealer. Physical and chemical properties of the root canals are important for deep penetration of the sealer into the dentin tubules.[28] If the contact surface between the root canal sealer and the dentin increases, the adhesion capacity of the root canal sealer increases.[29] The PAD system uses photo-sensitizing dye, which might adversely affect the contact angle of the MTA Fillapex root canal sealer. Alternatively, there might be an interaction between the photo-sensitizing dye and MTA Fillapex. Further investigations are needed to shed light on these issues.
CONCLUSION
Taking into consideration the limitations of this in vitro study, we concluded that AH Plus and MTA Fillapex sealers had greater bond strength compared with Sealapex root canal sealers. The superior adhesion capacity of the AH Plus sealer might make it more advantageous when additional disinfection is required for root canal disinfection. We also concluded that the PAD system adversely affected the bond strength of the MTA Fillapex root canal sealer to dentin.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Siqueira JF, Jr, Machado AG, Silveira RM, Lopes HP, de Uzeda M. Evaluation of the effectiveness of sodium hypochlorite used with three irrigation methods in the elimination of Enterococcus faecalis from the root canal, in vitro. Int Endod J. 1997;30:279–82. doi: 10.1046/j.1365-2591.1997.00096.x. [DOI] [PubMed] [Google Scholar]
- 2.Williams JA, Pearson GJ, Colles MJ. Antibacterial action of photoactivated disinfection 1 used on endodontic bacteria in planktonic suspension and in artificial and human root canals. J Dent. 2006;34:363–71. doi: 10.1016/j.jdent.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 3.Souza LC, Brito PR, de Oliveira JC, Alves FR, Moreira EJ, Sampaio-Filho HR, et al. Photodynamic therapy with two different photosensitizers as a supplement to instrumentation/irrigation procedures in promoting intracanal reduction of Enterococcus faecalis. J Endod. 2010;36:292–6. doi: 10.1016/j.joen.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 4.Bonsor SJ, Nichol R, Reid TM, Pearson GJ. Microbiological evaluation of photo-activated disinfection in endodontics (an in vivo study) Br Dent J. 2006;200:337–41. doi: 10.1038/sj.bdj.4813371. 329. [DOI] [PubMed] [Google Scholar]
- 5.Economides N, Kokorikos I, Kolokouris I, Panagiotis B, Gogos C. Comparative study of apical sealing ability of a new resin-based root canal sealer. J Endod. 2004;30:403–5. doi: 10.1097/00004770-200406000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Hovland EJ, Dumsha TC. Leakage evaluation in vitro of the root canal sealer cement Sealapex. Int Endod J. 1985;18:179–82. doi: 10.1111/j.1365-2591.1985.tb00437.x. [DOI] [PubMed] [Google Scholar]
- 7.Zmener O, Spielberg C, Lamberghini F, Rucci M. Sealing properties of a new epoxy resin-based root-canal sealer. Int Endod J. 1997;30:332–4. doi: 10.1046/j.1365-2591.1997.00086.x. [DOI] [PubMed] [Google Scholar]
- 8.Bin CV, Valera MC, Camargo SE, Rabelo SB, Silva GO, Balducci I, et al. Cytotoxicity and genotoxicity of root canal sealers based on mineral trioxide aggregate. J Endod. 2012;38:495–500. doi: 10.1016/j.joen.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 9.Sleder FS, Ludlow MO, Bohacek JR. Long-term sealing ability of a calcium hydroxide sealer. J Endod. 1991;17:541–3. doi: 10.1016/S0099-2399(06)81719-X. [DOI] [PubMed] [Google Scholar]
- 10.Caicedo R, von Fraunhofer JA. The properties of endodontic sealer cements. J Endod. 1988;14:527–34. doi: 10.1016/S0099-2399(88)80084-0. [DOI] [PubMed] [Google Scholar]
- 11.Doğan H, Qalt S. Effects of chelating agents and sodium hypochlorite on mineral content of root dentin. J Endod. 2001;27:578–80. doi: 10.1097/00004770-200109000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Erickson RL. Surface interactions of dentin adhesive materials. Oper Dent. 1992;(Suppl 5):81–94. [PubMed] [Google Scholar]
- 13.Kataoka H, Yoshioka T, Suda H, Imai Y. Dentin bonding and sealing ability of a new root canal resin sealer. J Endod. 2000;26:230–5. doi: 10.1097/00004770-200004000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Gogos C, Stavrianos C, Kolokouris I, Papadoyannis I, Economides N. Shear bond strength of AH-26 root canal sealer to dentine using three dentine bonding agents. J Dent. 2003;31:321–6. doi: 10.1016/s0300-5712(03)00064-2. [DOI] [PubMed] [Google Scholar]
- 15.Lee KW, Williams MC, Camps JJ, Pashley DH. Adhesion of endodontic sealers to dentin and gutta-percha. J Endod. 2002;28:684–8. doi: 10.1097/00004770-200210000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Skidmore LJ, Berzins DW, Bahcall JK. An in vitro comparison of the intraradicular dentin bond strength of Resilon and gutta-percha. J Endod. 2006;32:963–6. doi: 10.1016/j.joen.2006.03.020. [DOI] [PubMed] [Google Scholar]
- 17.Drummond JL, Sakaguchi RL, Racean DC, Wozny J, Steinberg AD. Testing mode and surface treatment effects on dentin bonding. J Biomed Mater Res. 1996;32:533–41. doi: 10.1002/(SICI)1097-4636(199612)32:4<533::AID-JBM6>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 18.Sudsangiam S, van Noort R. Do dentin bond strength tests serve a useful purpose? J Adhes Dent. 1999;1:57–67. [PubMed] [Google Scholar]
- 19.Guerisoli DM, Marchesan MA, Walmsley AD, Lumley PJ, Pecora JD. Evaluation of smear layer removal by EDTAC and sodium hypochlorite with ultrasonic agitation. Int Endod J. 2002;35:418–21. doi: 10.1046/j.1365-2591.2002.00488.x. [DOI] [PubMed] [Google Scholar]
- 20.Assmann E, Scarparo RK, Böttcher DE, Grecca FS. Dentin bond strength of two mineral trioxide aggregate-based and one epoxy resin-based sealers. J Endod. 2012;38:219–21. doi: 10.1016/j.joen.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 21.Cobankara FK, Orucoglu H, Sengun A, Belli S. The quantitative evaluation of apical sealing of four endodontic sealers. J Endod. 2006;32:66–8. doi: 10.1016/j.joen.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 22.Yücel AC, Güler E, Güler AU, Ertaº E. Bacterial penetration after obturation with four different root canal sealers. J Endod. 2006;32:890–3. doi: 10.1016/j.joen.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 23.Vasconcelos BC, Bernardes RA, Duarte MA, Bramante CM, Moraes IG. Apical sealing of root canal fillings performed with five different endodontic sealers: Analysis by fluid filtration. J Appl Oral Sci. 2011;19:324–8. doi: 10.1590/S1678-77572011005000005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sagsen B, Ustün Y, Demirbuga S, Pala K. Push-out bond strength of two new calcium silicate-based endodontic sealers to root canal dentine. Int Endod J. 2011;44:1088–91. doi: 10.1111/j.1365-2591.2011.01925.x. [DOI] [PubMed] [Google Scholar]
- 25.Vivan RR, Zapata RO, Zeferino MA, Bramante CM, Bernardineli N, Garcia RB, et al. Evaluation of the physical and chemical properties of two commercial and three experimental root-end filling materials. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:250–6. doi: 10.1016/j.tripleo.2010.04.021. [DOI] [PubMed] [Google Scholar]
- 26.Sarkar NK, Caicedo R, Ritwik P, Moiseyeva R, Kawashima I. Physicochemical basis of the biologic properties of mineral trioxide aggregate. J Endod. 2005;31:97–100. doi: 10.1097/01.don.0000133155.04468.41. [DOI] [PubMed] [Google Scholar]
- 27.Camilleri J. Modification of mineral trioxide aggregate. Physical and mechanical properties. Int Endod J. 2008;41:843–9. doi: 10.1111/j.1365-2591.2008.01435.x. [DOI] [PubMed] [Google Scholar]
- 28.ØRstavik DA. Materials used for root canal obturation: Technical, biological and clinical testing. Endod Topics. 2005;12:25–38. [Google Scholar]
- 29.Wu MK, de Gee AJ, Wesselink PR. Effect of tubule orientation in the cavity wall on the seal of dental filling materials: An in vitro study. Int Endod J. 1998;31:326–32. [PubMed] [Google Scholar]


