Abstract
Objective:
The aim of this study was to determine how physical and morphological properties affect the fracture resistance of roots, and which criteria are important for root specimen standardization in fracture resistance studies.
Materials and Methods:
Seventy-five freshly extracted human canine teeth were selected. Crowns were sectioned from the cement–enamel junction and the root lengths were set at 16 mm. Then they were prepared up to ProTaper F3 file. Each root was numbered and data were obtained by measuring mesiodistal and buccolingual dimensions, volume, weight, and density. Tests for fracture strength were performed using an Instron Testing Machine (Instron Corp. MA, USA). The force was applied axially, angled at 45 degrees with a constant speed of 1 mm/min. For each sample, the force at the time of fracture was recorded in Newtons. Results were evaluated statistically using linear regression analysis.
Results:
Volume and weight of the roots had more effect than mesiodistal or buccolingual dimensions on root fracture resistance.
Conclusions:
In root fracture resistance studies, volume or weight of the roots must be standardized when distributing roots to groups.
Keywords: Fracture resistance, physical, root, root volume, root weight, standardization, volume measurement
INTRODUCTION
Endodontically treated teeth are susceptible to fracture in comparison with vital teeth.[1] The most often reported reasons have been dehydration of dentin, removal of tooth structure during root canal treatment, prolonged use of high concentrations of irrigation solutions, and excessive pressure during obturation.[2,3] In the literature there are several studies in which the fracture resistance of endodontically treated teeth were evaluated or the techniques for reinforcing of these teeth were described.[4,5,6]
It is important to examine systems in an in vitro model prior to in vivo use in order to identify treatment or materials that might improve clinical performances. Extracted human teeth are also widely used for in vitro studies in fracture resistance tests.[3,7] However standardization among the extracted teeth should be performed in order not to affect the study's results.
Standardization of the roots is one of the important steps in the study in which fracture resistance is evaluated. If roots were not distributed among the groups equally, these variables could have affected the results of the studies. In many studies, the mesiodistal (MD) and buccolingual (BL) dimensions and the lengths of the roots were standardized in order to prevent these effects. Researchers also attempt to choose the same type of teeth in order to standardize the specimens. In spite of these standardization attempts, it has been discussed that the standard deviations within the groups were rather high,[7,8,9] rendering the results meaningless, and prompting studies using a larger number of specimens. Therefore, different variables should be evaluated in terms of standardization among the groups. The aim of this study was to determine how physical (weight, volume, and density) and morphological (MD and BL dimensions) properties affect the fracture resistance of roots, and which criteria are important for standardization in fracture resistance evaluated studies. The null hypothesis was that different physical properties of roots would not affect the fracture resistance of endodontically treated roots.
MATERIALS AND METHODS
Seventy-five human canine teeth extracted for periodontal reasons with completed apices and similar lengths were used in this study. The teeth were stored in 0.1% timol at room temperature until they were used. Mesiodistal (MD) and buccolingual (BL) radiographs were taken of the specimens to evaluate the anatomical structures of the teeth. The teeth with internal or external resorption, those which had two or more root canals, and those with calcification were discarded. The teeth were examined under a stereomicroscope to discard specimens with cracks and craze lines. Soft tissues and calculus were removed mechanically from the root surfaces using a periodontal scaler. Specimens were decoronated with a diamond disc under a water coolant to obtain a standardized root length of 16 mm. Each specimen was enumerated using a fixed pen. Before the fracture resistance test was carried out, weight, volume [Figure 1], and density [Figure 1] were calculated with ‘Precisa XB 220A’ precision balance (Precisa, Gravimetrics AG, Dietikon, Switzerland) which had a capacity of 220 g, and a readability of 0.0001 g. Weight change in distilled water is equal to root volume, because density of distilled water is 1 g/cm3. Density was calculated by weight dividing to volume. MD and BL dimensions at 16 mm (the coronal end of the root) from the apex of the each root were recorded with root number. A size 10 K-file (Dentsply, Maillefer, Ballaigues, Switzerland) was inserted into the canal until it was visible at the apical foramen, and the working length was determined to be 1 mm short of this position. Root canal shaping procedures were performed with ProTaper Universal rotary files (Dentsply Maillefer, Ballaigues, Switzerland), and apical region was prepared to size #30 (F3) in all specimens. The canal was irrigated with 2 ml freshly prepared 5% NaOCl solution with a 27-gauge needle after each file. A final rinse with 5 ml 17% EDTA for 1 min, followed by rinsing with 5 ml 5% NaOCl for 1 min was applied for smear layer removal. Then the canals were irrigated with distilled water. The specimens were dried with paper points and filled with gutta-percha and AH Plus sealer® (Dentsply DeTrey, Kontanz, Germany) using cold lateral compaction.
Figure 1.
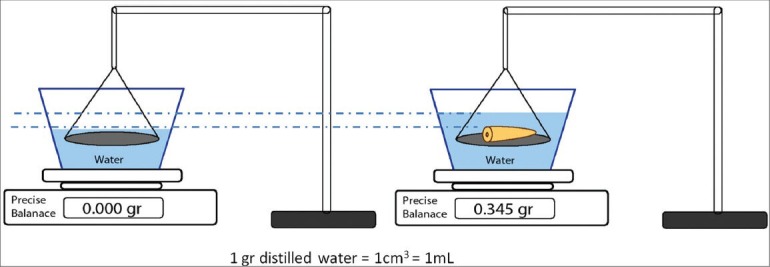
Calculation of root volume and density using a precise balance
Proper wax stencils were molded and the roots were mounted into acyclic resin at an angle of 45 degrees to its long axis, leaving 6 mm of each root exposed [Figure 2].
Figure 2.
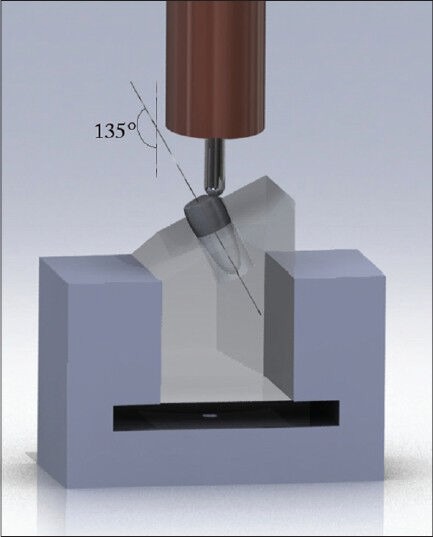
Fracture test design
A universal testing machine (Instron Corp., Norwood, MA, USA) was used for the strength test. The upper plate included a spherical steel tip with a diameter of 4 mm. Vertical force was loaded with a speed of 1 mm/min until fracture occurred. The force when the fracture occurred was recorded in Newtons for each root. The statistical analysis was performed with Pearson's correlation IBM® SPSS® Statistics 20 software.
RESULTS
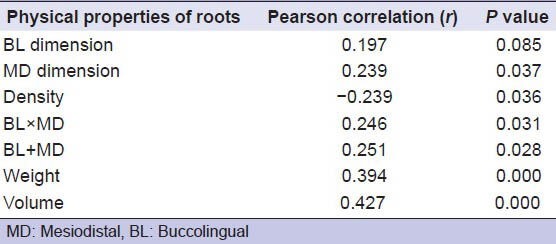
The results indicated that volume (r = 0.427, P < 0.001) and weight (r = 0.394, P < 0.001) of the roots had a more significant effect than BL (r = 0.197, P = 0.085), MD (r = 0.239, P = 0.037) dimension which implying that volume or weight had greater importance regarding the prediction of fracture strength [Table 1]. Properties with higher correlation coefficient means higher effect on root strength.
Table 1.
Physical and morphological properties of the samples along with Pearson correlation coefficients and P values. Negative value means inverse correlation
DISCUSSION
When extracted human teeth are used for evaluating the fracture resistance of roots, there is a potential for large uncontrollable variations to affect strength. For that reason, all controllable factors should be standardized as much as possible.[7] Many researchers who have carried out this type of study-performed standardization, according to root length, MD and BL dimensions. However, many of these studies admitted very high standard deviations as normal.[7,8,9,10] Thus, this study aimed to control factors such as weight, volume, and density, which can affect the fracture resistance of teeth in order to contribute to the standardization process.
In the current study, the volumes or weights of root specimens have more statistically significant value than density, MD, and BL dimension. In previous studies, however, these variations did not take into account when the standardization of groups was performed. Future studies should be standardized to inhibit high standard deviations.
During the study design, standardization is generally achieved based on the lengths, and MD and BL dimensions of roots with referrals to other studies in the literature. However, this study has shown that the physical properties of teeth can affect the resistance of roots. Thus, it is important to determine the alternative properties of roots which could be useful for the standardization process in future investigations.
CONCLUSIONS
This is the first study in the literature to conclude that ‘the volume or weight of root as the most important determining factors in root fracture’. Within the limitations of this study, it can be concluded that when forming groups to evaluate fracture resistance, after the root length is standardized, the roots should be equally distributed according to their volumes or weights, rather than their MD and BL dimensions, as these dimensions cannot closely simulate the entire strength of the root as much as the volume or weight.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Sornkul E, Stannard JG. Strength of roots before and after endodontic treatment and restoration. J Endod. 1992;18:440–3. doi: 10.1016/S0099-2399(06)80845-9. [DOI] [PubMed] [Google Scholar]
- 2.Uzunoglu E, Aktemur S, Uyanik MO, Durmaz V, Nagas E. Effect of ethylenediaminetetraacetic acid on root fracture with respect to concentration at different time exposures. J Endod. 2012;38:1110–3. doi: 10.1016/j.joen.2012.04.026. [DOI] [PubMed] [Google Scholar]
- 3.Topçuoğlu HS, Arslan H, Keleş A, Köseoğlu M. Fracture resistance of roots filled with three different obturation techniques. Med Oral Patol Oral Cir Bucal. 2012;17:e528–32. doi: 10.4317/medoral.17518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zicari F, Van Meerbeek B, Scotti R, Naert I. Effect of ferrule and post placement on fracture resistance of endodontically treated teeth after fatigue loading. J Dent. 2013;41:207–15. doi: 10.1016/j.jdent.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 5.Borelli B, Sorrentino R, Zarone F, Ferrari M. Effect of the length of glass fiber posts on the fracture resistance of restored maxillary central incisors. Am J Dent. 2012;25:79–83. [PubMed] [Google Scholar]
- 6.Er K, Tasdemir T, Siso SH, Celik D, Cora S. Fracture resistance of retreated roots using different retreatment systems. Eur J Dent. 2011;5:387–92. [PMC free article] [PubMed] [Google Scholar]
- 7.Teixeira FB, Teixeira EC, Thompson JY, Trope M. Fracture resistance of roots endodontically treated with a new resin filling material. J Am Dent Assoc. 2004;135:646–52. doi: 10.14219/jada.archive.2004.0255. [DOI] [PubMed] [Google Scholar]
- 8.Ersev H, Yilmaz B, Pehlivanoğlu E, Ozcan-Çalişkan E, Erişen FR. Resistance to vertical root fracture of endodontically treated teeth with MetaSEAL. J Endod. 2012;38:653–6. doi: 10.1016/j.joen.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 9.Sagsen B, Er O, Kahraman Y, Akdogan G. Resistance to fracture of roots filled with three different techniques. Int Endod J. 2007;40:31–5. doi: 10.1111/j.1365-2591.2006.01177.x. [DOI] [PubMed] [Google Scholar]
- 10.Dikbas I, Tanalp J, Ozel E, Koksal T, Ersoy M. Evaluation of the effect of different ferrule designs on the fracture resistance of endodontically treated maxillary central incisors incorporating fiber posts, composite cores and crown restorations. J Contemp Dent Pract. 2007;8:62–9. [PubMed] [Google Scholar]


