Abstract
The sudden, stabbing, paroxysmal pain of neuralgia is the fiercest agony that a patient may experience in his life. Many varied medical treatments and surgical procedures have been suggested in the literature for neuralgic pain. Most of the patients fail to respond to medical treatments or succumb to complications of total anesthesia owing to surgical procedures. Herein, we tried a new treatment modality in patients suffering from postherpetic neuralgia with appreciable success in all the three cases that are presented in this paper. Streptomycin sulfate dissolved in 2% lidocaine solution was deposited at the peripheral branches on the involved nerves targeting the trigger zones, given weekly once for a maximum of 6 week period and continued once in 2 weeks if symptoms persisted. All patients were followed-up for 1 year and there was a marked improvement on follow-up.
Keywords: Neuralgic pain, peripheral injections, postherpetic neuralgia, streptomycin
INTRODUCTION
The etiology and pathogenesis of neuralgic pain is unclear and as a result of this no consistent treatment parameters are followed. The first line of treatment is usually pharmacological. In case of postherpetic neuralgia (PHN) topical agents are used as the first line as they are free of systemic side-effects. Anti-convulsant drugs and antidepressants have been tried in various studies. When patients fail to respond to medical treatment, various surgical interventions have to be employed to relieve the patient from his intractable pain. Peripheral injections and minor surgical procedures have been preferred over major surgical procedures as peripheral injections require no sophisticated and expensive instrumentations and can be employed on an out-patient basis. Peripheral injections of different substances such as alcohol,[1] glycerol,[2] botulinum[3] and streptomycin[4,5,6] have been tried earlier in patients with idiopathic trigeminal neuralgia (ITN). A thorough search of literature failed to reveal the use of streptomycin as peripheral injections for PHN.
CASE REPORTS
Case 1
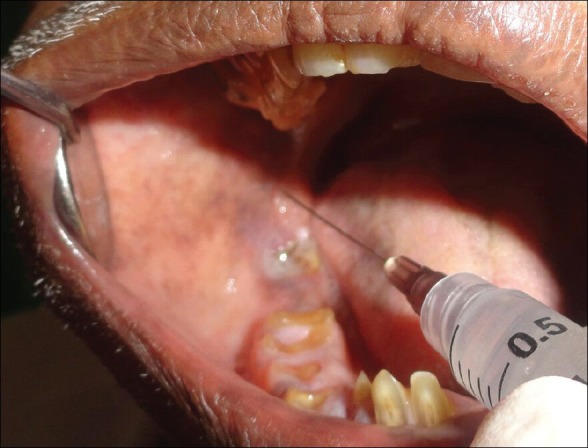
A 60-year-old male patient reported to the clinics with a chief complaint of vesicular eruptions on the left side of the face since 5 days. Past medical history was not contributing and the patient reported burning sensation in the affected area. The localization and distribution of the skin findings were distinctive and presented as ulcers ranging from 4 mm to 0.5 cm interspersed with crustaceans, extending on the left half of the face, characteristically not crossing the midline [Figure 1]. Intraoral examination revealed similar vesicular eruptions on the left side of the mid-palatine suture involving the hard and soft palate, not crossing the midline. Based on the clinical findings, the patient was diagnosed as herpes zoster involving the ophthalmic and maxillary division of the trigeminal nerve. After a thorough medical evaluation and required investigations, the patient was put on antiviral therapy, Acyclovir 800 mg orally 5 times daily for 7 days. To combat pain, tramadol 50 mg twice daily was given. At 4 weeks follow-up revealed good improvement in lesions, the lesions of the face and palate showed remission [Figure 2]. Patient reported of reduction in burning sensation, but persistent pain. Patient gave a history of continuous stabbing and burning type of pain with periods of exacerbations and remissions. Patient reported of exacerbation of pain with even a light touch of clothing in the left middle half of the face, a stimulus that does not usually evoke pain (allodynia). The region from the ala of the nose to the lower canthus of the eye and laterally up to the malar region evoked pain on touch indicative of trigger zones. A new treatment approach was tried in this patient. All the other medications were stopped and the patient was given Streptomycin sulfate injections 1 g mixed with 2% lidocaine deposited in the peripheral region of posterior superior alveolar nerve and the infra orbital area [Figure 3]. The injections were given bi-weekly for the first 6 weeks and followed once every alternate week for the next 4 weeks. Patient showed marked improvement in symptoms after 6 weeks and complete remission of pain in the following 4 weeks. Patient was followed-up for the next 1 year and remained pain free.
Figure 1.

Extraoral picture showing lesions on the left half of the face, not crossing the midline
Figure 2.

Four weeks follow-up picture showing remission of lesions
Figure 3.

Streptomycin lidocaine solution deposited in the posterior superior alveolar nerve peripherally
Case 2
A 56-year-old female patient reported to the clinics with the chief complaint of ulcers on the right side of his face since 5 days. The past medical and dental history was not contributing. Clinical examination revealed multiple ulcerative lesions on the right side of the face extending from the malar region to about 1 cm below the ala-tragus line, interspersed with multiple crustaceans, of varying sizes ranging from 2 mm to 5 mm, characteristically not crossing the midline. The clinical appearance was distinctive and was suggestive of herpes zoster involving the maxillary division of the trigeminal nerve. Patient had no intraoral findings or any other associated symptoms. Patient was put on antiviral therapy (acyclovir 800 mg five times daily for 2 weeks) and tramadol 50 mg daily. A 2 week follow-up showed complete remission of lesions, but patient still complained of severe pain evoked on touch. Patient was given streptomycin sulfate injections (1 g mixed with 2% lidocaine deposited in the region of posterior superior alveolar nerve following the technique of local anesthesia). The injections were given bi-weekly for the first 6 weeks and followed once every alternate week for the next 5 weeks. Patient showed marked improvement in symptoms after 8 weeks. The following 5 weeks also showed improvement, although complete remission of pain was not achieved. The peripheral injections were continued bi-weekly for the next 4 weeks. Patient reported to be pain free for the next 3 months after which he failed to report for follow-up appointments.
Case 3
A 62-year-old male patient reported to the clinics with a complaint of a continuous burning type of pain on the right side of the lower half of his face since 2 months [Figure 4]. Pain was severe, episodic and stabbing type, which evoked on application of physical stimuli like light touch and cold weather. Patient gave a history of boils and ulcers on the same side of the face 3 months ago for which he had visited his physician who prescribed acyclovir (400 mg TID [in three divided doses]) and aceclofenac (100 mg BID [in two divided doses]). Patient reports remission of the lesions within 15 days. Patient was a known case of herpes zoster involving the mandibular division of the trigeminal nerve. Clinical examination showed scars indicating healed ulcers on the right side of lower third of face extending onto the lower border of the mandible. No relevant intraoral findings were evident. Hard tissue examination revealed generalized attrition of teeth with root stumps in relation to 14, 15, 16, 17, 26, 27, 36, 37, 43, 44, 45, 46 and 48. Patient was diagnosed as a case of PHN. Streptomycin-lidocaine injections (1 g streptomycin sulfate mixed with 2% lidocaine deposited in the inferior alveolar nerve intraorally) were given bi-weekly for the first 6 weeks followed by once every alternate week for the next 6 weeks until the patient was pain free. Patient remained pain free for the next 1 year [Figure 5].
Figure 4.

Extraoral profile picture of the patient
Figure 5.
Streptomycin-lidocaine solution deposited in the inferior alveolar nerve peripherally
DISCUSSION
Pain initiated by a primary lesion or dysfunction of the nervous system is defined as neuropathic pain.[7] Based on the symptoms, neuropathic orofacial pain may be divided into two broad categories: Paroxysmal and continuous.[8] Paroxysmal neuropathies such as trigeminal neuralgias are characterized by short electrical or sharp pain. Continuous pain, sometimes of a burning quality, is more commonly seen in post-traumatic neuropathy and is a common feature of PHN.
PHN
PHN is a debilitating complication of herpes zoster, the risk of which increases with age. It is the most common long-term complication of herpes zoster caused by the reactivation of varicella zoster virus (VZV). VZV establishes latency in the dorsal root ganglia following a primary infection and may be reactivated with an acute phase causing pain and skin rash. Secondary attacks of herpes zoster occur in 6-14% of individuals.[9] Although immune senescence through ageing is the most common cause of reduced cell mediated immunity, other causes such as viral reactivation,[10] immune compromise and immunosuppressant drugs also contribute to the spectrum of patients developing herpes zoster.
There is no universally accepted definition of PHN, but that suggested by Dworkin and Portenoy,[11] “presence of significant pain or abnormal sensation 3 months after rash healing,” is now commonly used both clinically and in the research study design [Figure 6].
Figure 6.
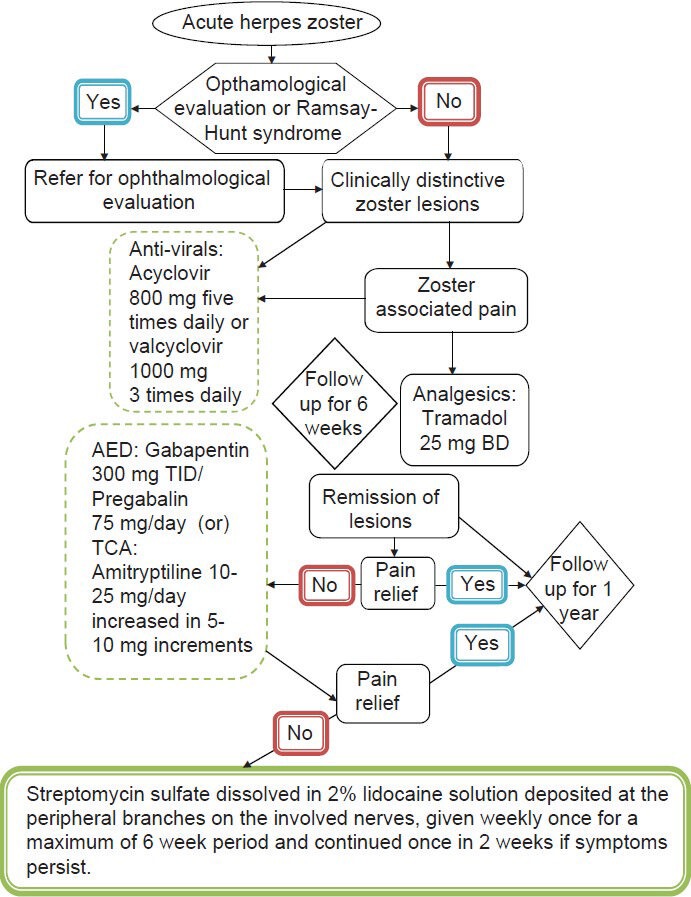
Schematic representation of current trends in the treatment of herpes zoster and postherpetic neuralgia
The pathophysiology of PHN may be best described in terms of irritable nociception and central sensitization. It has been shown that after injury due to infection, as in PHN, the more peripherally located C fiber terminals undergo atrophy and the larger diameter, deeper A-fiber terminals sprout up into the superficial laminae of the dorsal horn. When this happens, normally non-noxious stimulation of mechanoceptors within the skin will activate the dorsal horn producing pain impulses (allodynia).[12] PHN may manifest as one or more of either spontaneous aching or burning, paroxysmal shooting pain, allodynia or hyperalgesia.
Treatment update and current trends
In the acute phase of herpes zoster the goal of the treatment is to control the symptoms and prevent complications. Antiviral medications such as acyclovir, famcyclovir and valcyclovir are nucleoside analogues that inhibit the replication of human herpes virus including VZV. When given in patients with herpes zoster, these agents reduce the duration of viral shedding, hasten rash healing, reduce the severity and duration of acute pain and reduce the risk of progression to PHN.[13]
Pain management in PHN
In case of PHN, it is the best to begin with a medication that either has the fewest adverse effects or that is perhaps associated with least side-effects. For example, topical medications are almost always free of systemic side-effects. However, topical therapy alone is not promising and patients often benefit from the simultaneous use of several medications working together synergistically.
Topical lidocaine patches are particularly effective in patients with allodynia. Lidocaine works by decreasing small fiber nociceptive activity and the patch itself will act as a protective barrier from the brush of clothing. Lidocaine 5% patch can be applied (up to three patches at one time) to the affected area for a maximum of 12 h in a 24 h period.[14] However, the effect is only transient with this patch. Capsiacin 0.075% cream applied three times a day, which works by inhibiting the substance P is also shown to be effective as a topical agent. Capsiacin is associated with a burning sensation, which limits its clinical use.[15]
Tricyclic antidepressants (TCA) are the criterion standard for the management of pain in PHN. Multiple clinical studies have shown the efficacy of nortriptyline and amitriptyline, which is given 10-20 mg/day as a starting dose, increased in 10 mg increments every 3-5 days until satisfactory pain relief is obtained.[16] The mechanism of action of TCA in producing analgesia is independent of its antidepressant effect. They enhance the central endogenous pain inhibiting mechanisms by inhibiting the noradrenalin and serotonin receptors at the synapses.[17] However, TCAs are often associated with adverse side-effects such as antichlolinergic effects, sedation and potential cardiac dysarrythemias. Selective serotonin and norepinephrine reuptake inhibitors such as duloxetine and velafaxine can be used in patients intolerable to TCAs, but these drugs do not specifically relieve neuropathic pain.[17]
The newer generation anti-convulsants, such as pregabalin and gabapentin have fewer side-effects and require less hematological monitoring than older anti-convulsants such as carbamazepine and valproic acid. Pregabalin and gabapentin have both shown to relieve pain, however, pregabalin has the advantage of a more predictable and linear pharmacological profile. Gabapentin is given in a dosage of 300 mg on day 1, 300 mg BID on day 2 and 300 mg TID from day 3 for a period of 2-3 weeks.[18] Pregabalin is given as 75 mg/day at bed time and can be increased by 75 mg every 5 days up to a maximum of 300 mg twice a day. However, these agents are known to cause adverse effects of somnolence, dizziness and withdrawal symptoms and should be used with caution in elderly patients.[19]
The role of opiods in patients with PHN is controversial. Their long-term risks of sedation, mental clouding and abuse limits their use although they are particularly safe in the context of systemic, cardiac, renal and hepatic adverse effects. Suggested starting doses include, oxycodone 5 mg 4-6 h and increased in 5-10 mg increments as needed up to 40 mg/day; tramadol 25 mg twice a day, increased every 3 days to a maximum of 200 mg/day.[20] Other reasonable options include oxycodone with acetaminophen or morphine. When prescribing opiods, clinicians should recommend prophylactic constipation therapy in the form of a laxative or stool softener.
Streptomycin as a new treatment modality
Streptomycin sulfate was accidently discovered to be efficient in the treatment of painful conditions after it was used topically for the treatment of tuberculous laryngitis with necrosis of the skin. It was noted that patients obtained pain relief in the neck and so this character of streptomycin was later employed in dentistry for the treatment of facial pains. The earliest report of use of streptomycin in dentistry for facial pains was in the year 1963.[21] After 18 years, Sokolovic et al.[4] started using streptomycin in cases of ITN. He concluded that, among 20 patients of the study, 10 patients were completely pain free after 30 month follow-up, six patients missed their follow-up after 2-18 months, but were pain free when last seen and in four patients the pain had recurred 18-30 months after treatment. Further, a double-blind controlled trial conducted by Stajcic et al.[5] in the year 1990 revealed that streptomycin lidocaine injections provided longer pain free durations for patients with ITN. Kriener in 1996 reported a case of ITN treated with streptomycin lidocaine injections in which the patient remained pain free during the 8 month follow-up period.[6] The above studies were done on ITN patients while this paper highlights similar effects on PHN.
The mechanism of action of streptomycin involves stabilization of nerve cell membrane and inhibition of acetylcholine release at the nerve endings.[6] Hence when streptomycin is deposited at the peripheral nerve endings, it reduces the irritable nociception at the nerve endings, which evokes the pain.
Side-effects of streptomycin are minimal and the pain associated in deposition of the solution is reduced by the effect of lidocaine. Similar effects are observed in patients treated with peripheral injections of botulinium toxin[3] and other sclerosing agents like alcohol,[1] but most cases succumb to the complication of loss of sensations in the treated area. Such an effect was not seen with streptomycin lidocaine injections.
Among the three reported cases, one case failed to report for follow-up, but was relieved of pain when last seen, while the other two patients remained pain free after a period of 1 year and are still under follow-up.
CONCLUSION
Although options for improved pain management of PHN are increasing, many patients fail to achieve near complete to complete pain relief. Presently, the most effective treatment options, apart from good psychological management, are careful use of certain TCA, anti-convulsant drugs and well-managed use of opiod drugs such as oxycodone and morphine, all which have their own share of contraindications and side-effects. Further, treatment costs along with patient distress and suffering has a major impact on such patients. This paper highlights a new cost- effective treatment modality with minimal side-effects. Streptomycin, an antibiotic, which has been attempted in the past to relieve orofacial pain, has tremendous scope for further research in the future.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Fardy MJ, Patton DW. Complications associated with peripheral alcohol injections in the management of trigeminal neuralgia. Br J Oral Maxillofac Surg. 1994;32:387–91. doi: 10.1016/0266-4356(94)90031-0. [DOI] [PubMed] [Google Scholar]
- 2.Stajcić Z. Peripheral glycerol injections in the treatment of idiopathic trigeminal neuralgia. A preliminary study. Int J Oral Maxillofac Surg. 1989;18:255–7. doi: 10.1016/s0901-5027(89)80087-6. [DOI] [PubMed] [Google Scholar]
- 3.Türk U, Ilhan S, Alp R, Sur H. Botulinum toxin and intractable trigeminal neuralgia. Clin Neuropharmacol. 2005;28:161–2. doi: 10.1097/01.wnf.0000172497.24770.b0. [DOI] [PubMed] [Google Scholar]
- 4.Sokolović M, Todorović L, Stajcić Z, Petrović V. Peripheral streptomycin/lidocaine injections in the treatment of idiopathic trigeminal neuralgia. A preliminary report. J Maxillofac Surg. 1986;14:8–9. doi: 10.1016/s0301-0503(86)80249-1. [DOI] [PubMed] [Google Scholar]
- 5.Stajcić Z, Juniper RP, Todorović L. Peripheral streptomycin/lidocaine injections versus lidocaine alone in the treatment of idiopathic trigeminal neuralgia. A double blind controlled trial. J Craniomaxillofac Surg. 1990;18:243–6. doi: 10.1016/s1010-5182(05)80423-8. [DOI] [PubMed] [Google Scholar]
- 6.Kreiner M. Use of streptomycin-lidocaine injections in the treatment of the cluster-tic syndrome. Clinical perspectives and a case report. J Craniomaxillofac Surg. 1996;24:289–92. doi: 10.1016/s1010-5182(96)80061-8. [DOI] [PubMed] [Google Scholar]
- 7.Merskey H, Bogduk N. 2nd ed. Seattle: IASP Press; 1994. Classification of Chronic Pain: Description of Chronic Pain Syndromes and Definition of Pain Terms. [Google Scholar]
- 8.Okeson JP. The American Academy of Oraofacial Pain. Chicago, IL: Quintesence Publishing; 1996. Orofacial Pain: Guidelines for Assessment, Classification and Management. [Google Scholar]
- 9.Bowsher D. The lifetime occurrence of Herpes zoster and prevalence of post-herpetic neuralgia: A retrospective survey in an elderly population. Eur J Pain. 1999;3:335–42. doi: 10.1053/eujp.1999.0139. [DOI] [PubMed] [Google Scholar]
- 10.Weksler ME. Immune senescence. Ann Neurol. 1994;35(Suppl):S35–7. doi: 10.1002/ana.410350711. [DOI] [PubMed] [Google Scholar]
- 11.Dworkin RH, Portenoy RK. Proposed classification of herpes zoster pain. Lancet. 1994;343:1648. doi: 10.1016/s0140-6736(94)93106-2. [DOI] [PubMed] [Google Scholar]
- 12.Woolf CJ, Shortland P, Coggeshall RE. Peripheral nerve injury triggers central sprouting of myelinated afferents. Nature. 1992;355:75–8. doi: 10.1038/355075a0. [DOI] [PubMed] [Google Scholar]
- 13.Shafran SD, Tyring SK, Ashton R, Decroix J, Forszpaniak C, Wade A, et al. Once, twice, or three times daily famciclovir compared with aciclovir for the oral treatment of herpes zoster in immunocompetent adults: A randomized, multicenter, double-blind clinical trial. J Clin Virol. 2004;29:248–53. doi: 10.1016/S1386-6532(03)00164-1. [DOI] [PubMed] [Google Scholar]
- 14.Rowbotham MC, Davies PS, Verkempinck C, Galer BS. Lidocaine patch: Double-blind controlled study of a new treatment method for post-herpetic neuralgia. Pain. 1996;65:39–44. doi: 10.1016/0304-3959(95)00146-8. [DOI] [PubMed] [Google Scholar]
- 15.Watson CP, Tyler KL, Bickers DR, Millikan LE, Smith S, Coleman E. A randomized vehicle-controlled trial of topical capsaicin in the treatment of postherpetic neuralgia. Clin Ther. 1993;15:510–26. [PubMed] [Google Scholar]
- 16.Wu CL, Raja SN. An update on the treatment of postherpetic neuralgia. J Pain. 2008;9:S19–30. doi: 10.1016/j.jpain.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 17.Johnson R. Herpes zoster – Predicting and minimizing the impact of post-herpetic neuralgia. J Antimicrob Chemother. 2001;47(Suppl T1):1–8. doi: 10.1093/jac/47.suppl_1.1. [DOI] [PubMed] [Google Scholar]
- 18.Rowbotham M, Harden N, Stacey B, Bernstein P, Magnus-Miller L. Gabapentin for the treatment of postherpetic neuralgia: A randomized controlled trial. JAMA. 1998;280:1837–42. doi: 10.1001/jama.280.21.1837. [DOI] [PubMed] [Google Scholar]
- 19.Sabatowski R, Gálvez R, Cherry DA, Jacquot F, Vincent E, Maisonobe P, et al. Pregabalin reduces pain and improves sleep and mood disturbances in patients with post-herpetic neuralgia: Results of a randomised, placebo-controlled clinical trial. Pain. 2004;109:26–35. doi: 10.1016/j.pain.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 20.Sampathkumar P, Drage LA, Martin DP. Herpes zoster (shingles) and postherpetic neuralgia. Mayo Clin Proc. 2009;84:274–80. doi: 10.4065/84.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Halasz I, Zappe L. Local use of streptmycin in the treatment of pain syndromes. Ideggyogy Sz. 1963;16:145–51. [PubMed] [Google Scholar]


