Abstract
Objective:
The purpose of this study was to investigate compliance, awareness and practices of infection control procedures among senior dental students at the College of Dentistry, University of Sharjah, United Arab Emirates.
Materials and Methods:
The study comprised of 119 subjects of 4th and 5th year dental students. A questionnaire was developed with 25 open and closed-ended questions related to barrier techniques, vaccination status, infection control practices and awareness. This was distributed among the senior dental students and completed upon signing the consent form. Each questionnaire was coded to ensure the confidentiality of responses.
Results:
The questionnaire was distributed among 223 senior dental students at the University of Sharjah of which only 119 students (53%) responded. Compliance with the use of protective barriers was high with the exception of protective eye wear, utilized by a mere 27% of students. There was a significant difference between 4th and 5th year dental students’ attitudes (P < 0.05) regarding the treatment of patients with infectious diseases. Compared with 44.4% of the 5th year students, 68.5% of the 4th year students did not mind treating patients with infectious diseases. Owing to this, 61.9% of the 5th year students suffered from non-sterile percutaneous and mucous membrane exposures compared with 44.6% of the 4th year students (P < 0.05).
Conclusions:
Efforts are needed to improve attitudes, implement information and motivate students in the correct and routine use of infection control measures. With all infection control protocols already implemented in dental schools, the challenge remains on improving compliance with infection control recommendations.
Keywords: Dental students, infection control, oral health, survey
INTRODUCTION
Dental health-care workers are at high risk of exposure to cross infection with bloodborne pathogens such as hepatitis B virus (HBV) and hepatitis C virus (HCV), human immunodeficiency virus (HIV) and Mycobacterium tuberculosis, streptococci and other viruses and bacteria that colonize the oral cavity and the respiratory tract.[1,2]
During dental procedures, transmission of infections could occur through direct contact with blood, saliva or contaminated treatment water from dental units, injury with an anesthetic needle or splash exposure of the mucous membranes, droplets and aerosols as well as indirect contact with contaminated instruments and surfaces.[1,3,4,5] Accidental exposure to infections in dental settings can be avoided by using safety precautions at work and implementing infection control guidelines. However, since some exposures cannot be prevented, vaccination and proper post-exposure management are the main forms of protection.[6]
Direct involvement in patient treatment as part of their clinical training puts dental students at risk of exposure to pathogens. Since the majority of carriers of infectious diseases cannot be identified, implementation of standard universal precautions in dental schools is the most effective way to control cross infection.[7,8]
Dental schools should provide their students with current guidelines and training in infection control and facilitate appropriate immunization.[6] Implementation can be achieved at all levels and is the first step toward changing the attitudes and habits of oral health-care professionals.[9]
In the College of Dentistry at University of Sharjah, infection control lectures start as early as the 1st year. Infection control procedures are applied in dental laboratories in the 2nd and 3rd year. In the 4th and 5th years of study, students apply the concepts of infection control in the clinical training sessions. The personal protective equipment (PPE) at dental clinics at University of Sharjah includes disposable caps, gowns, gloves and protective eyewear. These are to be used at all times when treating a patient. Students are to refrain from wearing jewelry in the dental clinics and must have short fingernails. Students are required to have taken the HB vaccination before entering the clinical years. In year 4 clinics, students are introduced to the clinical environment. They deal mainly with simple periodontal procedures and operative dentistry as well as pedodontics and single rooted endodontic procedures. As they progress into year 5, they further develop and consolidate their skills pertaining to patient management in complex conservative dentistry, pediatric dentistry, periodontics and endodontics. They also start practicing in fixed prosthodontics and oral surgery.
The purpose of this study was to investigate awareness, knowledge and compliance with recommended infection control procedures among year 4 and year 5 senior clinical dental students at the College of Dentistry, University of Sharjah, United Arab Emirates.
MATERIALS AND METHODS
In the United Arab Emirates, there are five undergraduate private dental schools, graduating approximately 250 students yearly. There are no public dental schools in the United Arab Emirates. This study was conducted in one of these schools, at the College of Dentistry, University of Sharjah in Sharjah city during the spring semester of 2011. The study group comprised of 4th and 5th year dental students (n = 119). Our sample of students in University of Sharjah would be representative of the other private dental schools in the country. The questionnaire used was adapted and modified from the article published by De Souza et al.[10] on his study conducted in Rio de Janeiro, Brazil. The questionnaire consisted of 25 open and closed-ended questions related to barrier techniques, vaccination status, percutaneous and mucous membrane exposures in addition to the dental treatment of infected patients, infection control practices and awareness. It was distributed to all senior dental students. After obtaining permission from the deanship of the college, three of the co-authors approached to the students at the beginning of the students’ clinical sessions and invited them to participate in the study. The authors used the class lists obtained from the dean's office to verify that the questionnaires were distributed to all of the senior students. There were no absentees since attendance to clinical sessions is mandatory. Students, who agreed to participate in the study, signed the consent form prior to answering the questionnaire. The self-administered questionnaires were collected immediately after completion on the same day. It took 2 days to access all clinical students because of different clinical groups. To ensure confidentiality of responses the questionnaires were coded.
The data were tabulated and analyzed by the Chi-square test. All analyses were conducted using the Statistical Package for Social Sciences (SPSS11.5) by IBM.
RESULTS
The questionnaire was distributed to 223 dental students from year 4 to year 5, of which only 119 of them responded (response rate = 53%). The distributions of male and female students are shown in Table 1.
Table 1.
Distribution of the students according to gender and the year of study in dental college
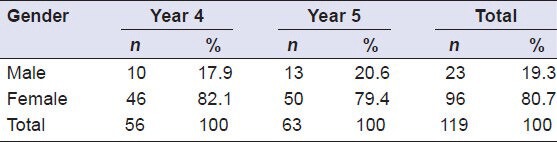
The average age was 24 years, ranging from 21 to 27 years. Gender division was 19.3% males and 80.7% females.
Vaccination status
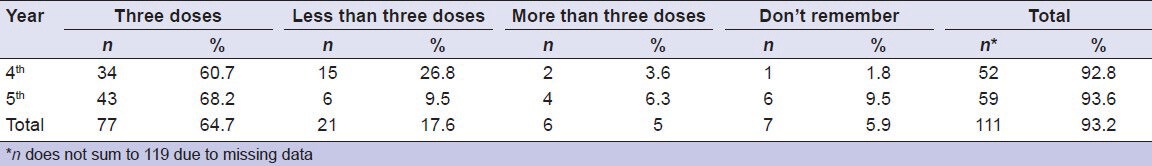
Vaccinations for HBV were 94.6% and 96.8% for year 4 and year 5 students respectively. Percentages of students distributed according to the doses of HBV immunization taken are shown in Table 2. There was a significant difference between 4th and 5th year students (P < 0.05). Only 55.4% of year 4 and 46% of year 5 students were tested for post HBV immunization serology (P > 0.05).
Table 2.
Frequency and percentage of hepatitis B vaccination doses taken by senior dental students P < 0.001
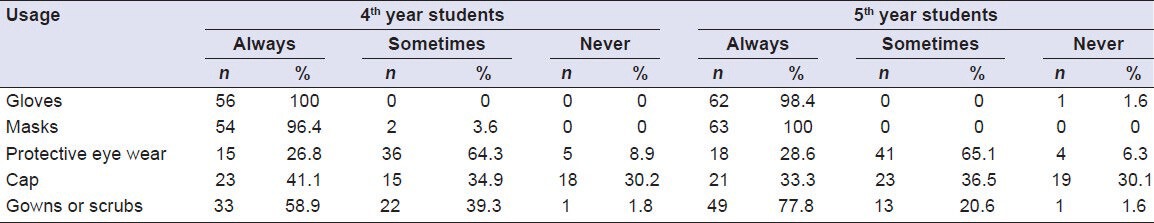
Barrier techniques
The uses of protective barrier techniques reported by dental students are shown in Table 3. Nearly, all of the year 4 and year 5 students mentioned wearing gloves and masks at all times, with the exception of 3.6% of year 4 students reportedly wearing masks only some of the time. Only 26.8% of year 4 students and 28.6% of year 5 students always used protective eyewear, while 64.3% of year 4 and 65% of year 5 students used it only occasionally. There were a reported 8.9% of year 4 and a 6.3% of year 5 students who claimed to have never used protective eyewear. Both 4th and 5th year students also reported similar percentages pertaining to the use of caps, ranging from 30% to 41%. There was no significant difference in the usage of gowns or scrubs between 4th and 5th year students. Overall 68.9% of students stated wearing gowns always, 28.6% sometimes and 1.7% never. When gowns were visibly contaminated, 85.7% mentioned they did change their gowns.
Table 3.
Use of protective barrier techniques reported by senior dental students
Nearly, 20.2% of students reported not removing their gloves upon leaving the immediate area of patient care. There was a statistically significant difference between year 4 and year 5 students regarding the changing of gloves after each procedure with the same patient. 75% of the 4th year students compared with 63.5% of the 5th year students changed their gloves after each procedure (P < 0.05). In general, only 47.9% of students reported washing hands after changing gloves.
Nearly, 95.8% reported sterilizing instruments after each dental procedure. This means 4.2% may not have sterilized their instrument after each procedure. 30.7% of students mentioned not removing their jewelry while working in the clinic and 33.3% reported keeping long fingernails.
Exposure to infectious diseases
Nearly, 87.1% thought that dental clinics were more prone to infectious contamination than other medical clinics. Statistically significant differences were observed between year 4 and year 5 students regarding the attitude and the number of patients treated with infectious diseases. Compared with 66% of the 4th year students, only 44% of the 5th year students did not mind treating patients with infectious diseases (P < 0.05). However, 20.6% of the 5th year students treated at least 1 patient with an infectious disease compared with none among 4th year students (P < 0.05). Among 5th year students, 9 of them reported to have treated patients with HBV, while 6 students reported they had treated patients with HCV. Only 1 student mentioned having treated patients with HBV and HCV and 4 students reported they had treated patients with herpes labialis infection.
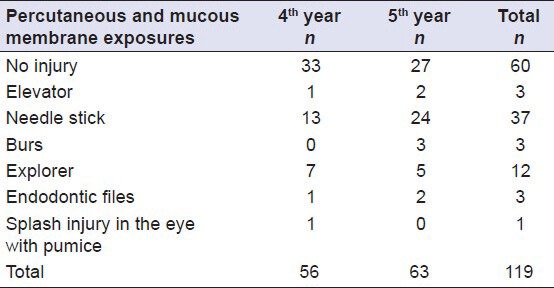
Percutaneous and mucous membrane exposures
The number of students who had occupational exposure to blood and other fluids while treating patients is shown in Table 4. The maximum number of reported exposures was related to the use of local anesthesia needles. There was a considerable difference between 4th and 5th year students (P < 0.05) who suffered from non-sterile percutaneous and mucous membrane exposures, with higher percentages reported among 5th year students (61.9%) compared with the 4th year students (44.6%).
Table 4.
Number of students who had percutaneous and mucous membrane exposures during dental treatment and type of exposures
Around 93.3% of the participants in this study were keen to follow the same infection control procedures in their own clinics, upon graduation.
DISCUSSION
Vaccination status
The results of our study regarding HBV immunization of senior dental students, stood at 95.8%. This result proved similar to those carried out in other dental schools. De Souza et al.[10] reported that 90.8% of all senior students received vaccinations in 6 dental schools in Rio de Janeiro, Brazil. McCarthy and Britton's study showed 100% immunization among the final year undergraduate dental, medical and nursing students at the University of Western Ontario, Canada.[6] On the other hand, Singh et al.[11] stated that 61.2% of undergraduate students in a Dental School In Central India were not vaccinated for HBV even though it was mandatory. He concluded a positive attitude but poor compliance of infection control practices among dental students.
Among the vaccinated students in our study only 60.7% in year 4 and 68.2% in year 5 completed the minimum required dosage (three doses) needed to obtain adequate immunity. These numbers are quite below the percentage of students who have completed the required doses reported by De Souza et al. (83.3%).[10] The lower rate of complete HBV vaccination in our sample emphasizes the need to further encourage vaccination and serological testing to reduce the risk of acquiring HBV, in the light of recent infection control guidelines.[7]
In our survey, 50.4% of students who were immunized tested for post immunization serology. In comparing previous studies, although 83.3% took the required doses for immunity in De Souza's survey, only 27.5% of participants reported post HBV immunization serology.[10] In McCarthy and Britton's study, a significant proportion failed to confirm the adequacy of post immunization anti-HB titer.[6] There is a concern that since HBV immunization does not always produce a sufficient response, the immunization may give students a false feeling of safety even if they did not have an adequate response.
Barrier techniques
The use of gloves among the dental students in our study was 99.2% and the use of masks was 98.3%. These results are comparable with previous studies assessing the use of PPE among dental students.[6,7] Compliance with the use of protective eyewear was quite low, only 30%, when compared with 59.7%,[8] 93.5%[6] and 84.2%[10] use of protective eyewear reported in other studies. Students should be reminded that neglecting the use of protective eyewear puts them at risk of transmission of infectious diseases through exposed membranes. There was a 40% compliance with the use of caps by dental students at the University of Sharjah, which is lower than the previous studies.[7,8] Personal protective clothing such as gowns or scrubs are worn as a barrier to prevent transmission of microorganisms between patients and dental health-care workers. Research has shown that aerosol and splatter containing pathogens can contaminate clinical wear, targeting the chest and forearms and remain alive for several days.[12,13] The majority of subjects in our study mentioned changing their scrubs when it was visibly contaminated. It has been recommended that dental uniforms be worn only in dental clinics, changed daily and immediately after a blood splatter to prevent cross contamination.[12] Furthermore, Leivers et al.[14] and Qureshi et al.[12] suggested that the uniforms should be washed separately and stressed the importance of using disposable gowns.
Nearly half of the students mentioned washing hands between each glove change. Similar to our findings de-Amorim-Finzi et al. (2010) reported only 45% compliance of hand hygiene among the graduation students.[15] The low compliance with regular hand washing necessitates stricter measures to remind the students of the importance of hand washing. Hand washing signs can be placed near each basin in dental clinics since hand washing is a significant element in infection control. In our college, a newly appointed infection control officer, other than the scheduled instructors of the clinics, makes rounds in every clinical session to ascertain implementation of infection control in students’ clinics.
The significant difference between the 4th and 5th year students who suffered from accidental injuries may be due to the fact that fifth year students had longer clinical exposure when compared with the 4th year students. McCarthy and Britton[6] reported 82% accidental injuries whereas De Souza et al.[10] reported 31% accidental injuries. In our survey 53.8% accidental injuries were reported. Non-sterile occupational injuries may pose a risk of transmission of bloodborne pathogens especially HBV, C and HIV.[6,9,16] At University of Sharjah, there is a post exposure management program for non-sterile occupational injuries during the students’ clinical training. The majority of injuries were due to needle sticks. Recapping the needles with both hands was found to be the most common cause of percutaneous injuries.[17] When multiple injections of local anesthetic are needed for one patient, dentists may recap the needles even when it is not recommended. At University of Sharjah, College of Dentistry of recent, every local anesthetic syringe is paired with artery forceps in a pouch to enable the removal of needles after usage, without direct hand contact.
The limitation of our study was that responses were based on students’ self-assessments rather than under the supervision by investigators of the study in a clinical environment. Therefore, the responses may not accurately reflect the actual infection control practices of dental students.
CONCLUSION
It is necessary to effectively communicate to students the associated risks and importance of transmission of infectious diseases and exposures during dental treatments. Efforts are needed to improve attitudes, to implement information and motivate students in the correct and routine use of infection control measures. With all infection control protocols already implemented in dental schools, the challenge remains on improving compliance with infection control recommendations.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Milward MR, Cooper PR. Competency assessment for infection control in the undergraduate dental curriculum. Eur J Dent Educ. 2007;11:148–54. doi: 10.1111/j.1600-0579.2007.00439.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Santosh K, Jyothi S, Prabu D, Suhas KK. Infection control practices among undergraduate students from a private dental school in India. Rev. Odonto Ciênc. 2009;24:124–8. [Google Scholar]
- 3.Shah R, Collins JM, Hodge TM, Laing ER. A national study of cross infection control: ‘Are we clean enough?’. Br Dent J. 2009;207:267–74. doi: 10.1038/sj.bdj.2009.824. [DOI] [PubMed] [Google Scholar]
- 4.Merchant VA. Herpesviruses and other microorganisms of concern in dentistry. Dent Clin North Am. 1991;35:283–98. [PubMed] [Google Scholar]
- 5.Lin SM, Svoboda KK, Giletto A, Seibert J, Puttaiah R. Effects of hydrogen peroxide on dental unit biofilms and treatment water contamination. Eur J Dent. 2011;5:47–59. [PMC free article] [PubMed] [Google Scholar]
- 6.McCarthy GM, Britton JE. A survey of final-year dental, medical and nursing students: Occupational injuries and infection control. J Can Dent Assoc. 2000;66:561. [PubMed] [Google Scholar]
- 7.Kohn WG, Collins AS, Cleveland JL, Harte JA, Eklund KJ, Malvitz DM, et al. Guidelines for infection control in dental health-care settings - 2003. MMWR Recomm Rep. 2003;52:1–61. [PubMed] [Google Scholar]
- 8.Freire DN, Pordeus IA, Paixão HH. Observing the behavior of senior dental students in relation to infection control practices. J Dent Educ. 2000;64:352–6. [PubMed] [Google Scholar]
- 9.King TB, Muzzin KB. A national survey of dental hygienists› infection control attitudes and practices. J Dent Hyg. 2005;79:8. [PubMed] [Google Scholar]
- 10.de Souza RA, Namen FM, Galan J, Jr, Vieira C, Sedano HO. Infection control measures among senior dental students in Rio de Janeiro state, Brazil. J Public Health Dent. 2006;66:282–4. doi: 10.1111/j.1752-7325.2006.tb04084.x. [DOI] [PubMed] [Google Scholar]
- 11.Singh A, Purohit BM, Bhambal A, Saxena S, Singh A, Gupta A. Knowledge, attitudes, and practice regarding infection control measures among dental students in Central India. J Dent Educ. 2011;75:421–7. [PubMed] [Google Scholar]
- 12.Qureshi UM, Siddiqui S, Macfarlane TV. Cross infection: How do dentists change into a clean set of clinical clothing? Health Educ J. 2005;64:101–9. [Google Scholar]
- 13.Bentley CD, Burkhart NW, Crawford JJ. Evaluating spatter and aerosol contamination during dental procedures. J Am Dent Assoc. 1994;125:579–84. doi: 10.14219/jada.archive.1994.0093. [DOI] [PubMed] [Google Scholar]
- 14.Leivers M, Tangri E, Kanji NN, Hirji SK, Hernandez G, Kaminska BD, et al. Uniform contamination in the dental environment. Can J Dent Hyg. 2012;46:50–7. [Google Scholar]
- 15.de Amorim-Finzi MB, Cury MV, Costa CR, Dos Santos AC, de Melo GB. Rate of compliance with hand hygiene by dental healthcare personnel (DHCP) within a dentistry healthcare first aid facility. Eur J Dent. 2010;4:233–7. [PMC free article] [PubMed] [Google Scholar]
- 16.Hersey JC, Martin LS. Use of infection control guidelines by workers in healthcare facilities to prevent occupational transmission of HBV and HIV: Results from a national survey. Infect Control Hosp Epidemiol. 1994;15:243–52. [PubMed] [Google Scholar]
- 17.Younai FS, Murphy DC, Kotelchuck D. Occupational exposures to blood in a dental teaching environment: Results of a ten-year surveillance study. J Dent Educ. 2001;65:436–48. [PubMed] [Google Scholar]


