Abstract
A 56-year-old man who had a history of repeated previous treatment for cystitis was admitted with abdominal distension, dysuria, pollakiuria, nocturia and sensation of urine retention after emptying the bladder. A CT scan showed a 10 cm irregularly shaped soft tissue mass abutting the anterosuperior aspect of the urinary bladder with wall thickening and a soft tissue component in the caecum. Colonoscopy revealed an encircling huge fungating mass on the caecum. The tumour was removed surgically. Histological examination showed moderately differentiated adenocarcinoma extending to the caecal wall and the bladder mucosa, the origin of the mass was consistent with that of a urachal cyst. The epicentre of the tumour was located in the bladder wall, with a distinct margin as a pathological feature. The patient was diagnosed with urachal cancer and concurrent direct caecal invasion.
Background
Urachal cancer develops in the urachus, which is an embryological remnant of the urogenital sinus and the allantois. Urachal cancer is a rare disease, accounting for 0.01% of all the adult cancers and 0.17–0.34% of all bladder cancers.1 2 At the time of making a diagnosis, urachal cancer is usually in the progressive phase resulting in poor prognosis. Histologically, urachal cancer is known to develop due to the malignant transformation of the columnar metaplasia of the transitional cell lining of the urachus. The cancer may also progress due to the enteric rest at the embryonic development stage.3 The most common urachal cancer cases are adenocarcinoma and mucinous, and histologically include transitional cell carcinoma and squamous cell carcinoma. Urachal cancer may be misinterpreted as the cancer that originated from other adjacent organs because it can invade into the surrounding organs. The present case is about the mass that was incidentally discovered at the bladder dome and caecum, and was diagnosed with urachal cancer with a direct caecal invasion.
Case presentation
A 56-year-old man was admitted to our hospital because of a distended abdomen. His abdominal distension had developed gradually during 1 month before admission. Approximately 20 years before the present medical admission, the patient had received treatment for urethritis and prostatitis secondary to aggravation of urethritis. The patient had consumed 80 g of alcohol daily and had not visited a hospital for treatment of his urinary symptoms and abdominal discomfort for 10 years. There was no history of fever, sweating, vomiting or weight loss. On admission, the blood pressure was 100/70 mm Hg; pulse rate, 115/min; respiration rate, 22/min and body temperature, 36.5°C. The patient was consciously alert, with an appearance of acute illness. The abdomen was distended, with shifting dullness to palpation and decreased bowel sounds in the absence of objective tenderness or rebound tenderness. There was no hepatosplenomegaly or palpable mass. Periumbilical discharge was not apparent. Positive 1+ pitting oedema was present in the lower legs. Findings of rectal examination and other physical examinations were within normal limits.
Investigations
Initial laboratory findings were as follows: haemoglobin 9.4 g/dL, haematocrit 28.5%, white cell count 15 490/mm3, platelet count 46 000/mm3 on complete blood counts. Prothrombin time was 48.2 s; activated partial thromboplastin time, 50.9 s. Levels of carcinoembryonic antigen (0.67 ng/mL) and cancer antigen 19–9 (20.62 U/mL) were within the normal range. Urinalysis showed the presence of blood (2+), and urine cytology showed cells that were highly suggestive of malignancy. CT revealed a 10 cm irregularly shaped soft tissue mass abutting the anterosuperior aspect of the bladder and large amounts of ascites. This mass was presumed to be a malignant lesion arising from the urachal remnant. The mass lesion further demonstrated wall thickening with a soft tissue component in the caecum and terminal ileum consistent with the presence of a possible metastatic lesion of urachal malignancy or a primary colon cancer (figure 1). Furthermore, CT showed hypertrophy of the left lobe and caudate lobe of the liver, with surface irregularity; these findings suggested the presence of chronic liver disease or cirrhosis. Ascitic fluid analysis showed a serum-ascites albumin gradient of 2 mg/dL, and ascitic fluid cytology was negative for malignant cells. Cystoscopy performed for the evaluation of the bladder mass showed a 5 cm mass lesion on the anterior wall of the bladder, but biopsy could not be performed because of the risk of bleeding due to coagulopathy. Therefore, we planned surgical resection immediately after correction of coagulopathy. Colonoscopy performed for determining the resection range before surgery revealed a huge fungating mass encircling the caecum (figure 2).
Figure 1.
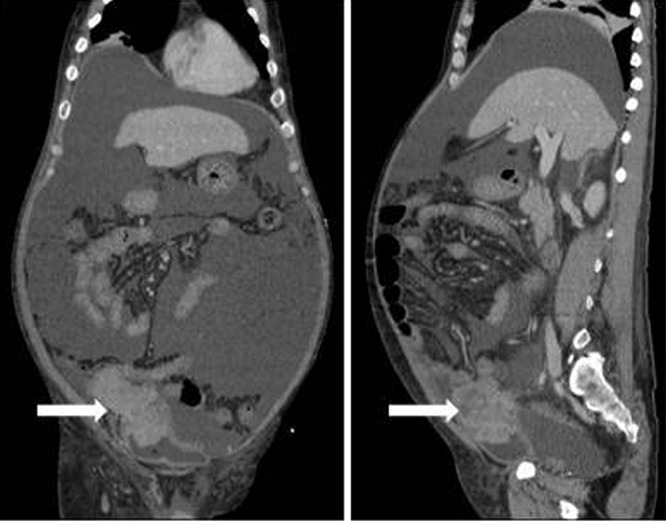
Abdominal and pelvic CT. Irregularly shaped soft tissue mass abutting the anterosuperior aspect of the urinary bladder with wall thickening and a soft tissue component in the caecum.
Figure 2.
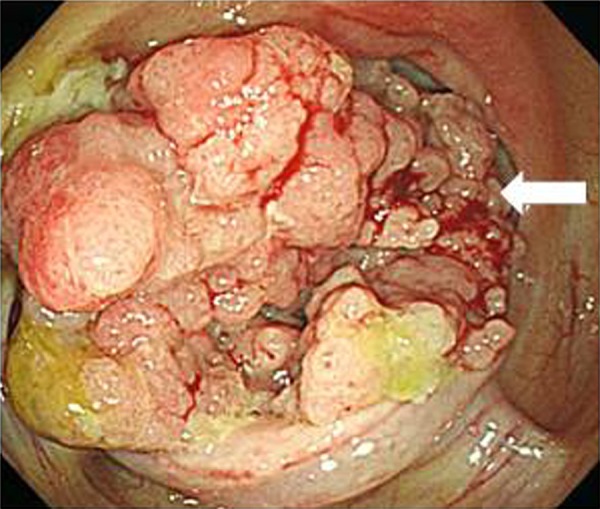
Colonoscopy. An encircling huge fungating mass on the caecum is noted.
Differential diagnosis
The patient was a heavy drinker and was presumed to have alcoholic liver cirrhosis with ascites. The findings of CT were consistent with primary colon cancer with bladder invasion or urachal cancer with direct caecal invasion.
Treatment
The patient underwent ileocecectomy to remove the caecal mass and partial cystectomy to remove the bladder mass with an R0 resection of pelvic lymph nodes. On gross inspection of the resection specimen, an ulcerofungating necrotic mass extended to the caecal wall (7.5 cm×5.5 cm×4 cm) and bladder mucosa was present between the caecum and the bladder, just above the ileocaecal junction. A polypoid protrusion measuring 5 cm at the greatest dimension was present at the bladder wall (figure 3). Pathological examination confirmed moderately differentiated intestinal-type adenocarcinoma extending to the caecal wall and bladder mucosa, considered to be compatible with origination from a urachal cyst (figure 4). The margins of tumour were negative and no metastases were seen in all regional lymph nodes. Results of immunochemical staining were as follows: cytokeratin (CK) 7 negative, CK20 positive, CDX-2 positive and β-catenin positive. The epicentre of the tumour was located at the anterior wall of the bladder with a distinct margin between the tumour and the normal bladder wall margin. On the basis of CT findings that the mass located anterosuperior aspect of the bladder was presumed to be a malignant lesion arising from the urachal remnant and pathologist's report, the tumour was confirmed to be urachal cancer with direct invasion of the caecum that was not a primary colon cancer.
Figure 3.
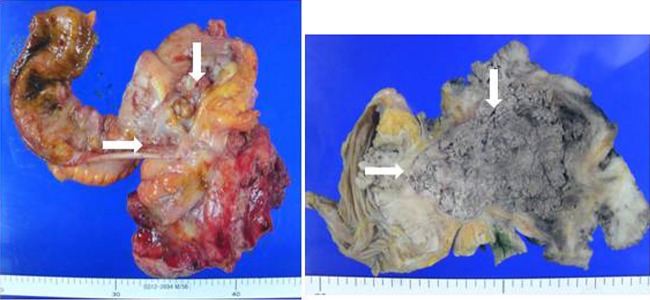
Macroscopic aspect. An ulcerofungating necrotic mass measuring 7.5 cm×5.5 cm×4 cm is present at the caecum, just above the ileocaecal junction, and an apolypoid protrusion (5 cm in the greatest dimension) is present at the bladder wall.
Figure 4.
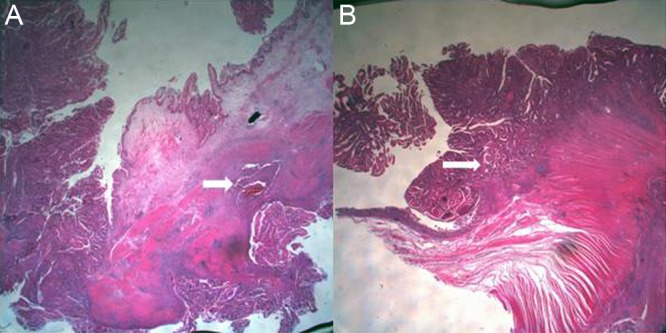
Pathological findings. (A) Urachal adenocarcinoma invading the mucosa and smooth muscle tissue of the bladder (H&E stain, ×10). (B) Urachal adenocarcinoma invading the caecal wall (H&E stain, ×10).
Outcome and follow-up
Complications associated with surgery were not observed, but wound healing was delayed because of cirrhotic ascites. We recommended adjuvant chemotherapy, but the patient was discharged 4 weeks postoperatively without chemotherapy, and conservative treatment was planned according to the patient's decision. After discharge, the patient did not visit the hospital for follow-up examination.
Discussion
The urachus is a vestigial musculofibrous band located between the bladder dome and umbilicus, or in the space of Retzius, which means the space between the transversalis fascia and the peritoneum.1 2 The pathogenesis of the urachal cancer has not been fully understood; however, the malignant transformation of the columnar or glandular metaplastic epithelia seems to be the cause for concern. Most urachal cancers are mucin-producing adenocarcinoma showing the forms of signet ring cells and an enteric-type histology that is often seen in colorectal cancer.1 3 4 The important factors in making a diagnosis with urachal cancer include the location of the lesion at the bladder dome/anterior wall, the tumour epicentre on the bladder wall, the absence of a widespread cystitis or cystic/glandularis and no other presence of primary tumours. Urachal cancer can be strongly suspected with the presence of a calcified supravesicular mass on the midline in the imaging tests including CT scan, but not pathognomonic tests.4 The evidence of a sharp line of demarcation between the tumour and normal urothelium of the bladder helps make the diagnosis.5 The present case was confirmed as intestinal-type adenocarcinoma through the biopsy samples and resection specimens.
Urachal cancer accounts for less than 1% of all bladder cancers and about 10% of all primary adenocarcinoma of the bladder.5 Patients with urachal cancer are usually diagnosed at the advanced phase because the mass grows in the outer area of the bladder without specific symptoms at the early stage, and it is detected when it caused an invasion into the adjacent organs. The symptoms of urachal cancer include haematuria, pyuria and dysuria, in addition to abdominal pain, abdominal mass or umbilical discharge.1 2 5
The treatments of urachal cancer include complete or partial cystectomy, which can secure a negative or disease-free margin, and the en bloc resection of the urachal ligament and umbilicus.6 7 In the present case, partial cystectomy, the resection of the urachus and pelvic lymph nodes and ileocecectomy for the caecal mass were performed.
If urachal cancer has partially progressed or a metastasis is observed, then the median survival period of the patients is known to be within 12–24 months. Mayo Clinic's Ashely reported a 49% of the 5-year cancer-specific survival rate in patients with urachal cancer.5 7 These poor prognoses of urachal cancer are associated with the clinical manifestations that often appear late and result in a delay in making diagnoses that are usually performed at the progressive phase, and with early partial invasions and distant metastases.1 Unlike the other types of cancer, no standard chemotherapy regimen for urachal cancer has been established. Chemotherapy and radiotherapy for urachal cancer have not been reported as a significant improvement in the overall survival rate.2 8
In the definite diagnosis of urachal cancer that invaded into the adjacent organs, the differential diagnosis of the primary tumours originated from the adjacent organs is important. It is important to confirm the location of the tumour epicentre on the bladder wall as well as the correlation between the clinical–radiological findings and pathological features. In the present case, the patient presented with urological symptoms for several years, the tumour was located at the anterosuperior bladder and midline on radiological tests, and the epicentre of the tumour, which is an enteric-type adenocarcinoma, was located at the anterior wall of the bladder, not at the caecum, on pathological examination. On the basis of the correlation among clinical manifestations, radiological findings and pathological features, definite diagnosis for urachal cancer with a direct caecal invasion was confirmed.
Learning points.
Urachal cancer is a rare disease and urachal cancer with direct colon invasion is a far less common condition.
For the diagnosis of urachal cancer, pathological finding is the mainstay and tumour epicentre in the bladder wall is the strongest criterion.
The correlation of clinical–radiological features, pathological features and immunohistochemical examination is important for a definitive diagnosis of urachal cancer versus differential diagnosis from other primary origins in adjacent organs.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Scabini S, Rimini E, Romairone E, et al. Urachal tumour: case report of a poorly understood carcinoma. World J Surg Oncol 2009;7:82. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 2.Elser C, Sweet J, Cheran SK, et al. A case of metastatic urachal adenocarcinoma treated with several different chemotherapeutic regimens. Can Urol Assoc J 2012;6:E27–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schnur J, Nguyen S, Divino C, et al. Coexisting rectal and urachal carcinoma: a case report. Am J Clin Oncol 2009;32:220–1 [DOI] [PubMed] [Google Scholar]
- 4.Gopalan A, Sharp DS, Fine SW, et al. Urachal carcinoma: a clinicopathologic analysis of 24 cases with outcome correlation. Am J Surg Pathol 2009;33:659–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siefker-Radtke A. Urachal carcinoma: surgical and chemotherapeutic options. Expert Rev Anticancer Ther 2006;6:1715–21 [DOI] [PubMed] [Google Scholar]
- 6.Sheldon CA, Clayman RV, Gonzalez R, et al. Malignant urachal lesions. J Urol 1984;131:1–8 [DOI] [PubMed] [Google Scholar]
- 7.Ashley RA, Inman BA, Sebo TJ, et al. Urachal carcinoma: clinicopathologic features and long-term outcomes of an aggressive malignancy. Cancer 2006;107:712–20 [DOI] [PubMed] [Google Scholar]
- 8.Siefker-Radtke AO, Gee J, Shen Y, et al. Multimodality management of urachal carcinoma: the M. D. Anderson Cancer Center experience. J Urol 2003;169:1295–8 [DOI] [PubMed] [Google Scholar]


