Abstract
A 54-year-old Caucasian woman presented with a 6 week history of periscapular pain and a T1 radiculopathy associated with Horner's syndrome. MRI of her cervicothoracic spine revealed an intervertebral disc herniation at the level of T1–2. During investigation she experienced some improvement in her symptoms and a conservative approach was pursued. At 6 months her pain and radiculopathy had resolved, and there was mild residual ptosis.
Background
Less than 1% of intervertebral disc herniation (IDH) affect the thoracic spine and those above the level of T3 represent only 4% of all thoracic prolapses.1 A pubmed search reveals 29 documented cases of T1–2 IDH since the first case in 1954.2 Upper thoracic IDH can cause Horner's syndrome by impinging on the sympathetic chain within the T1 root, leading to ipsilateral sympathetic deficiency. Only 24% of documented T1–2 IDH were found to be associated with Horner's syndrome, and reminds us of the rarer causes of Horner's syndrome to be included in a differential. Of the documented cases only two cases (7%) were managed conservatively, and neither case was associated with Horner's syndrome, making this case the first conservatively managed case of T1–2 disc herniation with Horner's syndrome.
Case presentation
A previously well 54-year-old Caucasian woman presented with a 6-week history of periscapular pain radiating into the medial forearm and paraspinal region. In the previous weeks she had experienced a burning sensation within the medial forearm and noticed difficulty with intricate motor skills in her dominate right hand. Her husband had recently noticed her eyelid drooping. She had been systemically well with no constitutional symptoms.
On examination her upper limb tone and reflexes were normal. Power of the intrinsic muscles was weak, Medical Research Council grade 4. Reduced sensation in the T1 dermatome was elicited. Examination of the cranial nerves was normal, except for a right sided partial ptosis and miosis.
Peripheral blood was unremarkable. Radiograph of her chest did not reveal an apical mass. MRI of the cervicothoracic spine revealed a lesion at the level of T1–2 with compression of the right T1 root as demonstrated in (figures 1 and 2).
Figure 1.

Sagittal section of T2-weighted MRI of the cervicothoracic spine, revealing large T1–2 disc prolapse.
Figure 2.
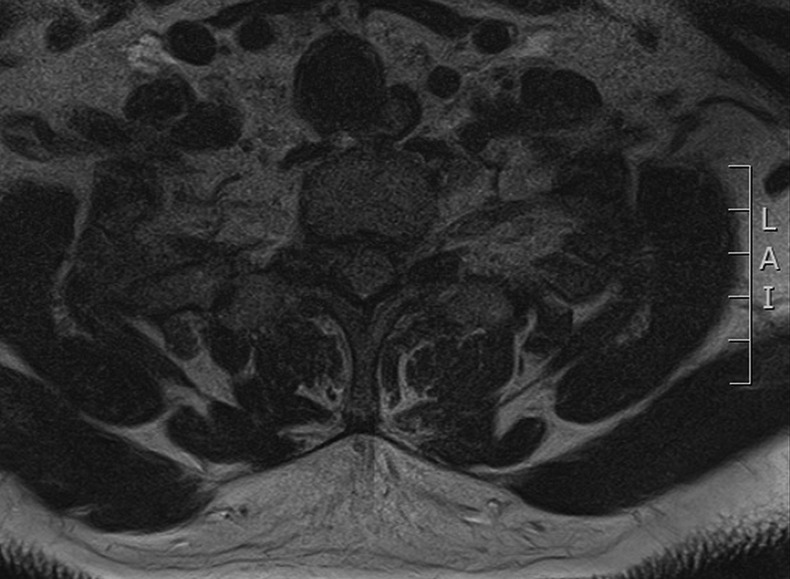
Axial T1 MRI demonstrating compression of the T1 root.
Outcome and follow-up
During her investigation she had already experienced some improvement from her periscapular pain and was keen to avoid surgery. A trial of conservative management by means of analgesia and physiotherapy was pursued with relief of her pain at 3 months, and functional improvement. At 6 months she had not had recurrence and there was only a mild residual ptosis. Overall the patient was pleased with the outcome.
Discussion
Symptomatic herniation at the level of T1–2 is rare due to the relative stability of the spine at this level. Of all thoracic IDHs, 79% presented with radiculopathy due to root compression. T1 converges with C8 to form the medial cord of the brachial plexus, contributing to the median and ulnar nerve and giving rise to the medial cutaneous nerve of the forearm. The nerve root of C8 is located within the C7-T1 intervertebral foramen, and the C7-T1 root within the T1/T2 foramen. It can therefore be difficult to differentiate a T1 from a C8 radiculopathy. Compared to a C8 radiculopathy, the power of the deep finger flexors is preserved in a T1 radiculopathy, however the intrinsics will be affected.
Horner's syndrome was associated with 24% of cases of T1–2 IDH on pubmed. Horner's syndrome occurs when there is sympathetic deficiency due to interruption at any point along the sympathetic chain either central, preganglionic or postganglionic in nature. For this reason there is a vast differential diagnosis to be considered along the sympathetic route. Pressure on the T1 root by a disc prolapse for example, may cause disruption of the sympathetic chain, with unopposed parasympathetic activity resulting in ipsilateral pupillary constriction, and relaxation of the superior tarsal muscle causing ptosis. Owing to the vast differential for Horner's syndrome, investigations should be based on history and examination findings. Suspicion of IDH should be raised with radicular symptoms in the presence of Horner's syndrome, and as a result adequate imaging should be arranged to include the upper thoracic spine.
Literature review demonstrates that operative management has usually been sought for symptomatic upper thoracic IDH, with only two cases (7%) successfully managed conservatively.3 Neither of these cases were associated with Horner's syndrome, and so this case report is the first conservatively managed T1–2 IDH associated with Horner's syndrome.
Although IDH affecting the upper thoracic spine is rare, it is an important differential diagnosis for a patient presenting with Horner's syndrome. Traditionally these cases have been managed surgically, however we have seen as in this case that conservative management can also be successful.
Learning points.
Upper thoracic disc prolapse is rare.
Upper thoracic disc prolapse is a recognised cause of Horner's syndrome.
A trial of conservative management for thoracic disc prolapse associated with Horner's syndrome could be considered before operative intervention.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Davies P, Kaar G. High thoracic disc prolapse in a rugby player. Br J Sports Med 1993;27:177–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Svien HJ, Karavitis AL. Multiple protrusions of intervertebral disc in the upper thoracic region: report of case. Proc Staff Meet Mayo Clinic 1954;29:375–8 [PubMed] [Google Scholar]
- 3.Gille O, Razafimahandry HJC, Soderlund C, et al. Hernie discale thoracique T1-T2. Rev Chir Orthop Reparatrice Appar Mot 2006;92:715–18 [DOI] [PubMed] [Google Scholar]


