Abstract
We present a case of paraneoplastic limbic encephalitis, describing the presenting features, diagnosis and management plan. Limbic encephalitis is one differential of rapidly progressive dementia. We describe a rational approach to the diagnosis of the patient with rapid cognitive decline.
Background
We present the case of under-recognised condition—limbic encephalitis. For the patient presenting to hospital with acute/subacute confusion, once the initial delirium screen has been performed and proved unremarkable, there is limited guidance describing the next steps. We present guidance in the investigation of such complex patients.
Case presentation
A 73-year-old woman with a medical history of rheumatoid arthritis and pernicious anaemia was admitted with headaches, subacute confusion and seizures. On physical examination she was confused, feverish and found to have finger clubbing. Examination of the respiratory, cardiovascular and nervous systems did not demonstrate any significant abnormality. Initial blood tests were unremarkable and blood cultures negative. Chest X-ray was normal. CT of the brain demonstrated mild periventricular ischaemic change but was otherwise unremarkable. Cerebrospinal fluid analysis demonstrated a mild pleocytosis. A presumptive diagnosis of viral encephalitis was made and the patient started on intravenous acyclovir and phenytoin for seizure control.
A few weeks later she was readmitted with confusion, paranoid ideation and recurrent déjà vu experiences. On this occasion, blood tests revealed a sodium of 119 mmol/L, plasma osmolality of 242 mOsmol/kg, urine osmolarity of 682 mOsmol/kg and urine sodium of 43 mmol/L consistent with the syndrome of inappropriate antidiuretic hormone secretion (SIADH). The sodium corrected over the course of 2 weeks with fluid restriction and demeclocycline and her condition improved though not to her premorbid state. MRI of the brain and an EEG were also performed.
Investigations
PCR results from the lumbar puncture were negative for enterovirus, parechovirus, herpes simplex 1 and 2, varicella-zoster and Epstein-Barr viruses. Human herpes virus 6 was considered unlikely in an immunocompetent adult and was not tested.
MRI of the brain was performed demonstrating areas of high signal changes in the mesial temporal lobes bilaterally (figure 1) on fluid attenuation inversion recovery (FLAIR) and T2 sequences. A CT of the chest identified a 14 mm right middle lobe nodule with enlarged right hilar and subcarinal nodes, suggestive of primary lung malignancy (figure 2). The EEG was reported as normal.
Figure 1.
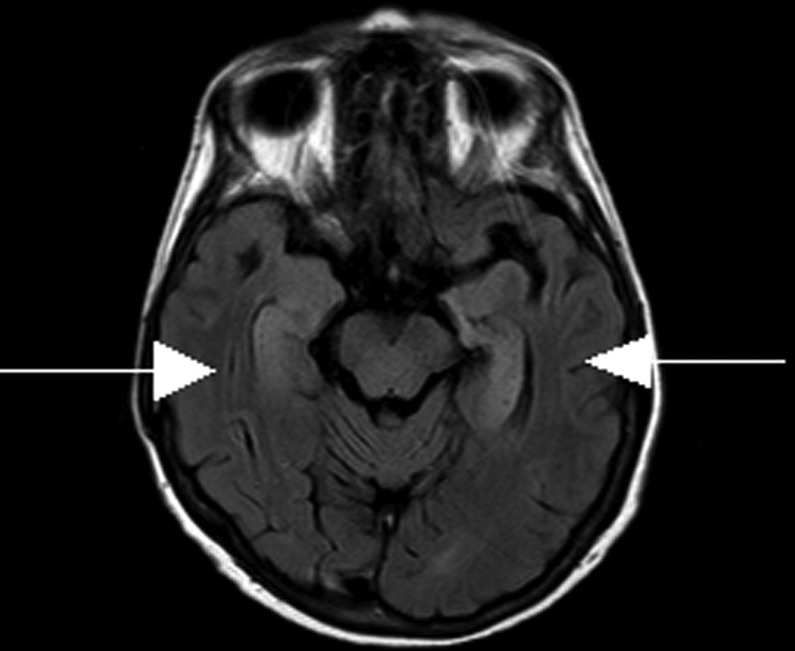
Axial MR T2 fluid attenuation inversion recovery of the brain demonstrating high signal changes in the mesial temporal lobes bilaterally.
Figure 2.
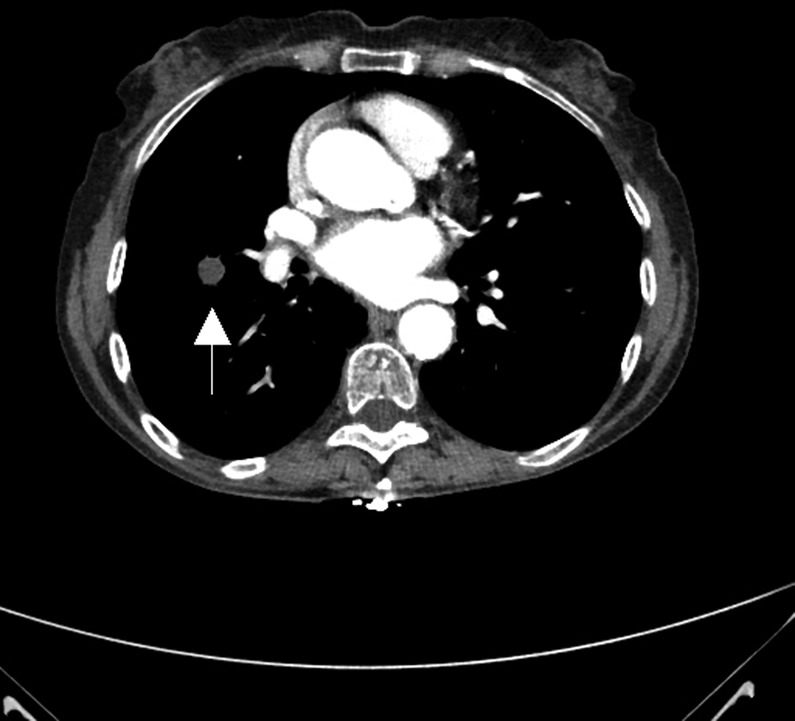
CT of the chest demonstrating a 14 mm right middle lobe nodule.
Additional tests for rapidly progressive dementia including paraneoplastic antibodies (including anti-Yo, anti-Hu, anti-Ri) and antineuronal antibodies were negative including antivoltage-gated potassium channel antibodies (VGKC). Thyroid peroxidase was elevated while thyroid receptor antibodies were normal. Tissue transglutaminase was negative.
Differential diagnosis
An infective cause, for instance herpes simplex, neurosyphilis, Creutzfeldt-Jakob disease (CJD), were considered unlikely as was a metabolic/toxic disorder (eg, coeliac associated neurological disorders and Wernicke-Korsakoff syndrome). Degenerative conditions (eg, dementia) were unlikely due to the rapid progression of her symptoms as were systemic autoimmune disorders (eg, Sjogren's and systemic lupus erythematosus). Positive thyroid peroxidase antibodies without thyroid receptor antibodies is a common feature of Hashimoto encephalopathy (HE). In the majority of such patients, thyroid function tests are normal or decreased. Clinical features of HE include resistant seizures, confusion, hallucinations and disturbance of consciousness. MRI findings in HE may demonstrate medial temporal lobe hyperintensities on FLAIR/T2 sequences, however, more common findings include ischaemic areas, granulomas or other degenerative processes. Of note, thyroid peroxidase may be falsely elevated in a number of conditions including rheumatoid arthritis.1 SIADH is well recognised to occur in association with certain subtypes of limbic encephalitis, for instance VGKC antibody-medicated encephalitis. The presentation and illness trajectory coupled with the imaging findings made paraneoplastic limbic encephalitis (PLE) the most likely diagnosis.
Treatment
A diagnosis of paraneoplastic limbic encephalitis was made and the patient started on high-dose parenteral followed by a tapering dose of oral steroids over a period of a few months.
Outcome and follow-up
At follow-up her condition had stabilised and she was beginning a phased return to work in a charity shop with close supervision. She declined a positron emission tomography (PET) scan to further evaluate the lung lesion. Although she lacked capacity to refuse investigation and management of the suspected underlying lung malignancy, multidisciplinary assessment deemed further investigation to be too challenging to perform without full cooperation and consent. As a consequence of being unable to manage the underlying cause of the limbic encephalitis she continued to experience intermittent exacerbations in her cognition.
Discussion
Rapidly progressive dementia refers to a unique set of disorders resulting in cognitive, behavioural and motor decline within 2 years.1 The differentials are wide and include inflammatory, neurodegenerative, toxic-metabolic conditions and infective conditions including CJD. While some features of our patient's presentation share features with those seen in HE, the lack of a dramatic and sustained response to steroids made this condition unlikely.
A number of antibodies are involved in autoimmune limbic encephalitis. These can be directed against intracellular antigens when they tend to be associated with an underlying malignancy, or directed against surface proteins when there is lower risk of malignancy, and carries a better prognosis.
Virtually all cancer types have been associated with PLE. Malignancies and their associated antibodies (in decreasing order of frequency) include small cell lung carcinoma (anti-Hu, anti-α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (anti-AMPAR), anti-Collapsin Response Mediator Protein 5 (CRMP5), antiamphiphysin), testicular germinal cell tumours (anti Ma2/Ta), thymoma (anti-CRMP5), breast cancer (antiamphiphysin) and Hodgkin's lymphoma.2 Although antineuronal antibodies are not invariably present they may help determine the nature of the malignancy. The tumour is undiagnosed in 50–80% of patients at the time neurological symptoms manifest.2 Immunosuppressive treatment is unlikely to be beneficial in these patients and removal of the tumour is critical for neurological improvement.
The Paraneoplastic Neurological Syndrome Euronetwork3 has identified four criteria for the diagnosis of PLE, all of which must be met:
Subacute onset of seizures, short term memory loss, confusion and psychiatric symptoms;
Neuropathological or radiological evidence of involvement of the limbic system;
Exclusion of other possible pathologies of limbic dysfunction;
Demonstration of a cancer within 5 years of the diagnosis of the neurological symptoms or development of classic symptoms of limbic dysfunction in association with a well-characterised paraneoplastic antibody.
Antibodies to cell membrane antigens include the glutamic acid decarboxylase (GAD) antibody, VGKC antibody, N-methyl-d-aspartate receptor (NMDAR) antibody, AMPAR, and γ-aminobutyric acid receptor (GABA) antibody. In general, these antibodies are non-paraneoplastic, however, they can be associated with tumours. These autoimmune causes of limbic encephalitis tend to be less severe and complete recovery is possible with immunosuppressive/immunomodulatory therapy (eg, high-dose corticosteroids, immunoglobulins, plasma exchange, cyclophosphamide, etc).2
In summary, the patient presenting with confirmed acute confusion should be investigated for a cause of delirium in the first instance. Where the presentation is more subacute or involving rapid deterioration in cognitive function, associated personality changes or involuntary movements including seizures, a rapidly progressive dementia should be suspected and a comprehensive search for the cause undertaken.4 In such situations clinical assessments including medication reviews, measurements of electrolytes, vitamins B12/folate, thyroid function, chest X-ray and urine testing are routinely performed. Early identification and treatment of an infective cause is essential and a lumbar puncture with opening pressure, checking of protein, glucose (with paired serum glucose), cell count, protein 14–3–3 and sending for cytology should be performed. Following this, investigations should be targeted to the most likely cause of the deterioration with allowance made for the marked overlap of clinical features of the various conditions mentioned. Autoantibody testing for coeliac and thyroid disease, syphilis serology and HIV are good initial low-risk, low-cost tests. More advanced investigations for limbic encephalitis include autoantibody testing already described. Identification of onconeuronal antibodies should direct the search towards finding an underlying malignancy using CT imaging, testicular ultrasound in men, mammography/mammary ultrasound in women and PET imaging. The finding of autoantibodies against membrane antigens would hasten the need for treatments targeting the immune system. MRI of the brain with T1, T2, diffusion-weighted (DWI) and FLAIR sequences may reveal pathology in a characteristic distribution (eg, cortical and subcortical hyperintensities on FLAIR and DWI in CJD, a mass occupying lesion in lymphoma or, as in the case described, predominant involvement of the limbic system). An EEG is helpful in determining the location of a lesion and the presence of cortical irritability. Some disorders have characteristic findings on EEG, for instance the spike and wave pattern in CJD or triphasic waves in hepatic encephalopathy.
The diagnosis of the patient with rapidly progressive dementia is challenging. We have presented a comprehensive and systematic approach to the investigation of such patients. Using such a strategy confers on patients the best chance of early diagnosis, effective treatment and a better outcome.
Learning points.
Patients presenting with acute confusion should be screened for commonly occurring conditions in the acute period.
A subacute or atypical presentation should prompt a more advanced cognitive impairment screen.
Antibodies against onconeuronal antigens are sensitive for underlying malignancy and extensive screening should be performed.
In those with limbic encephalitis associated with antibodies against membrane antigens, prompt treatment with immunsuppressive/immunomodulatory therapy may be curative.
Footnotes
Contributors: JB and KC were responsible for collecting patient information and creating an initial draft. LT was responsible for performing a literature search and summarising the data. KM was responsible for summarising the information and obtaining patient consent.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Rosenbloom MH, Atri A. The evaluation of rapidly progressive dementia. Neurologist 2011;17:67–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhang H, Zhou C, Wu L, et al. Are onconeural antibodies a clinical phenomenology in paraneoplastic limbic encephalitis? Mediators Inflamm 2013;2013:172986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Graus F, Delattre JY, Antoine JC, et al. Recommended diagnostic criteria for paraneoplastic neurological syndromes. JNNP 2004;75:1135–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Geschwind MD, Shu H, Haman A, et al. Rapidly progressive dementia. Ann Neurol 2008;64:97–108 [DOI] [PMC free article] [PubMed] [Google Scholar]


