Summary
We report a case of cerebral aspergilloma in a 25-year-old immunoincompetent man admitted to a general intensive care unit. Monitoring of intracranial pressure was instigated and revealed hour-long epochs of severe intracranial hypertension, despite a normal opening pressure, with decreases in cerebral perfusion pressure. We documented that this was associated with cerebral hypoperfusion by transcranial Doppler ultrasound. The present case illustrates that severe intracranial hypertension may evolve despite a normal opening pressure; it furthermore shows that continuous monitoring of intracranial pressure may be used to predict changes in cerebral haemodynamics in critically ill patients with neuroinfection.
Background
Although controversial, monitoring of intracranial pressure (ICP) may be advantageous for ensuring an adequate cerebral perfusion pressure (CPP) in critically ill patients with intracranial hypertension due to neuroinfection.1 2 Since CPP is determined by inflow pressure (mean arterial blood pressure) and outflow pressure (ICP),3 ICP monitoring allows for continuous assessment and optimisation of CPP. We report a case of cerebral aspergilloma complicated by severe intracranial hypertension in an immunoincompetent patient, in whom ICP and CPP were continuously monitored in the intensive care setting. For the first time, we document the impact of a declining CPP due to severe intracranial hypertension on cerebral perfusion in this context as evaluated by transcranial Doppler ultrasound (TCD) and near-infrared spectroscopy (NIRS).
Case presentation
A 25-year-old man with a 1-year history of T-cell prolymphocytic leukaemia and a suspected neuroinfection was transferred to our intensive care unit (ICU), which is a tertiary general ICU, due to a declining consciousness level. The patient had undergone bone marrow transplantation (BMT) 3 weeks earlier, and had subsequently developed graft-versus-host disease (GVHD) in the bowel.
Four days prior to transferral to the ICU, the patient had presented with malaise, headache, nuchal rigidity and a temperature of 40°C. A lumbar puncture showed elevated cerebrospinal fluid (CSF) neutrophil count (639 × 106/L; reference interval <1×106/L), lymphocyte count (36×106/L; reference interval <5×106/L) and protein levels (1.6 g/L; reference interval 0.15–0.50 g/L), as well as a low CSF glucose level (1.6 mM; reference interval 2.2–3.9 mM). Empirical antibiotic therapy with ceftriaxone and ampicillin combined with dexamethasone was instigated due to the suspicion of acute bacterial meningitis. An acute CT of the brain subsequently showed multiple abscesses in the left hemisphere and midline displacement (figure 1). The antibiotic therapy was supplied with amphotericin B to cover for aspergillosis, and pyrimetanine combined with clindamycine to cover for toxoplasmosis.
Figure 1.

CT of the cerebrum obtained on the second day after admission to the intensive care unit. The scan shows multiple abscesses (white arrows) in the parieto-occipital part of the left hemisphere, the largest process measuring 18 mm, surrounded by oedema and midline displacement towards the right of 6 mm.
As the Glasgow Coma Scale score suddenly dropped to 5 after 4 days of treatment, the patient was transferred to the ICU to undergo mechanical ventilation. Blood and CSF cultures showed no growth of any microorganisms. Once in the ICU, the lumbar puncture was repeated. While the leucocyte counts were normal, and there were no visible microorganisms, there was evidence of disseminated aspergillosis; the galactomannan test for Aspergillus was positive in CSF and serum (6.9 and 8.4, respectively, calculated as the ratio between the measured value and an internal standard; positive at a value ≥0.5). The antibiotic therapy was therefore shifted to meropenem and ciproxine, and the antifungal treatment was shifted to voriconazole and caspofungin.
Despite all therapeutic efforts, the patient's clinical condition deteriorated, and the left pupil became dilated and unresponsive to light. The attending neurosurgeon considered the patient too ill for neurosurgical intervention, but an external ventricular drain was established to allow for monitoring of ICP, CPP and therapeutical drainage of CSF. Furthermore, the head was kept elevated at 45° and positioned straight ahead to secure optimal venous return. Adequate sedation was ensured with midazolam, in an attempt to alleviate intracranial hypertension. By simultaneously maintaining the mean arterial blood pressure by norepinephrine infusion, an attempt was made to keep CPP at 65–70 mm Hg. Although the opening pressure at placement of the external ventricular drain was normal (7 mm Hg; reference interval 5–15 mm Hg), and despite therapeutical efforts, ICP monitoring revealed hour-long epochs of severe intracranial hypertension with pressures up to 75 mm Hg. During these epochs, it was not possible to maintain CPP, which decreased to values as low as 30 mm Hg.
Investigations
During one of the hour-long epochs of intracranial hypertension, on the second day of admission to the ICU, we continuously recorded the unilateral middle cerebral artery blood flow velocity (MCAv) by means of a 2 MHz pulsed TCD ultrasound system (Ez-Dop and Doppler-Box, Compumedics DWL GmbH, Singen, Germany). The TCD ultrasound system was secured over the patient's left transtemporal window by means of a fixation rack. The insonation depth for MCAv was 55 mm. Changes in MCAv reflects changes in cerebral perfusion, assuming that the diameter of the middle cerebral artery remains unchanged.4 Our measurements revealed the 1-h epoch of intracranial hypertension during which ICP doubled (from 31 to 65 mm Hg). This was associated with a concomitant reduction in CPP and MCAv to almost half their values at the onset of the epoch (figure 2). In contrast, there were no observed changes in cerebral oximetry during the epoch as evaluated by NIRS (INVOS Cerebral Oximeter, Somanetics, Troy, Michigan, USA) (figure 2). The NIRS optode was attached to the patient's forehead ipsilateral to the TCD probe.
Figure 2.
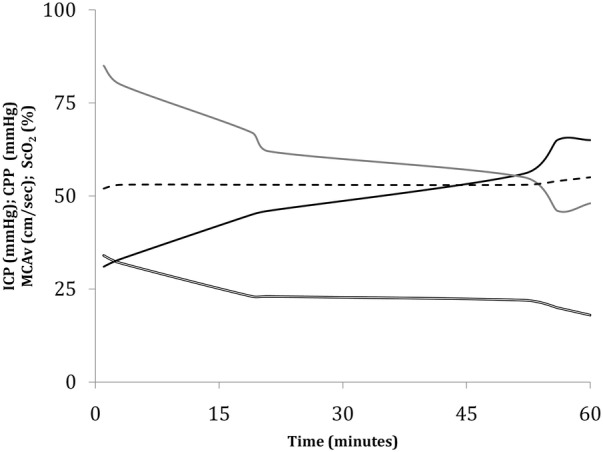
Monitoring of intracranial pressure (ICP; black), cerebral perfusion pressure (CPP; grey), middle cerebral artery blood flow velocity (MCAv; double line) and near-infrared spectroscopy-based measurements of cortical oxygenation (ScO2, dotted line) over a period of 1 h.
Outcome and follow-up
On the third day after transferral to the ICU, further treatment was considered futile; active treatment was discontinued and the patient died a few hours later due to incarceration.
Discussion
We report a fatal case of cerebral aspergilloma in an immunoincompetent BMT recipient with GVHD. Monitoring of ICP revealed hour-long epochs of intracranial hypertension that were resistant to any therapeutic efforts. As theoretically predicted, we documented that the subsequent decline in CPP was associated with cerebral hypoperfusion. Although the feasibility of ICP monitoring in the ICU is still debated, and has not yet been documented to have a positive effect on outcome in prospective clinical trials,2 5 the present case demonstrates the applicability of continuous ICP monitoring in the general ICU setting.
Cerebral aspergillosis is a rare and often lethal infection.6 The incidence is currently increasing, presumably because of an increased number of immunoincompetent patients.7 The course is frequently fulminant, and the patients die within a few days after occurrence of the first neurological symptoms.7 The main predisposing factor to cerebral aspergillosis is BMT.7 Hence, it has been reported that 16% of BMT patients suffer from an invasive mold infection, of which Aspergillus species account for two-thirds and 73% have CNS infection.8 Among BMT recipients, GVHD is an established risk factor that is adversely associated with outcome.8
The mortality rate in patients with cerebral aspergillosis who are immunoincompetent has been reported to be as high as 100%,8 9 while mortality rates of 60% and 25% have been reported for immunocompetent patients treated medically and neurosurgically, respectively.9 It has previously been reported that ICP monitoring ensured early craniotomy in a case of acute bacterial meningitis.10 Although timely left decompression could possibly have affected the outcome of our patient, his clinical condition was so poor once admitted to the ICU that neurosurgery was not considered feasible.
The use of continuous ICP monitoring in a case of cerebral aspergilloma has not previously been reported. The present case stresses that monitoring of ICP and CPP is applicable in this context, in that it may reflect the concomitant changes in cerebral haemodynamics. No changes could be detected by NIRS, despite a doubling of ICP with pronounced reductions in CPP and MCAv.
Therefore, the present case does not support the use of NIRS for continuous monitoring of cerebral haemodynamics in this context.
The present case illustrates that severe intracranial hypertension may evolve despite a normal opening pressure, changes that would otherwise not have been detected. In other cases of cerebral aspergilloma, monitoring of ICP and CPP may thus favourably affect outcome by allowing the clinician to optimise cerebral haemodynamics and prompt timely neurosurgical intervention. A prospective randomised trial is however required before any definitive conclusions on this matter can be made.
Learning points.
Cerebral aspergillosis is a rare and frequently lethal neuroinfection with mortality rates in immunoincompetent patients as high as 100%.
The major underlying diseases of cerebral aspergillosis are haematological malignancies, and the main predisposing factors are bone marrow transplantation and graft-versus-host disease.
Severe intracranial hypertension may evolve in patients with neuroinfection, even with a normal opening pressure and a decrease in cerebral perfusion pressure due to intracranial hypertension causes a decrease in cerebral perfusion.
Monitoring of intracranial pressure and cerebral perfusion pressure is feasible in patients with neuroinfection, and may be used to predict changes in cerebral haemodynamics.
Future prospective studies should assess whether optimising cerebral haemodynamics through invasive monitoring may improve outcome in patients with neuroinfection.
Footnotes
Contributors: LNT, RRP and RMGB contributed towards conception and design. RRP and RMGB collected the data. LNT and RMGB drafted the manuscript. LNT, RRP and RMGB analysed the data, prepared the figures, edited and revised the manuscript and approved the final version of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Zhong J, Dujovny M, Park HK, et al. Advances in ICP monitoring techniques. Neurol Res 2003;25:339–50 [DOI] [PubMed] [Google Scholar]
- 2.Steiner LA, Andrews PJ. Monitoring the injured brain: ICP and CBF. Br J Anaesth 2006;97:26–38 [DOI] [PubMed] [Google Scholar]
- 3.Miller JD, Stanek A, Langfitt TW. Concepts of cerebral perfusion pressure and vascular compression during intracranial hypertension. Prog Brain Res 1972;35:411–32 [DOI] [PubMed] [Google Scholar]
- 4.Willie CK, Colino FL, Bailey DM, et al. Utility of transcranial Doppler ultrasound for the integrative assessment of cerebrovascular function. J Neurosci Methods 2011;196:221–37 [DOI] [PubMed] [Google Scholar]
- 5.Cremer OL, van Dijk GW, van Wensen E, et al. Effect of intracranial pressure monitoring and targeted intensive care on functional outcome after severe head injury. Crit Care Med 2005;33:2207–13 [DOI] [PubMed] [Google Scholar]
- 6.Walsh TJ, Hier DB, Caplan LR. Aspergillosis of the central nervous system: clinicopathological analysis of 17 patients. Ann Neurol 1985;18:574–82 [DOI] [PubMed] [Google Scholar]
- 7.Guermazi A, Gluckman E, Tabti B, et al. Invasive central nervous system aspergillosis in bone marrow transplantation recipients: an overview. Eur Radiol 2003;13:377–88 [DOI] [PubMed] [Google Scholar]
- 8.Baddley JW, Stroud TP, Salzman D, et al. Invasive mold infections in allogeneic bone marrow transplant recipients. Clin Infect Dis 2001;32:1319–24 [DOI] [PubMed] [Google Scholar]
- 9.Kourkompetis TK, Desalermos A, Muhammed M, et al. Central nervous system aspergillosis: a series of 14 cases from a general hospital and review of 123 cases from the literature. Medicine (Baltimore) 2012;91:328–36 [DOI] [PubMed] [Google Scholar]
- 10.Baussart B, Cheisson G, Compain M, et al. Multimodal cerebral monitoring and decompressive surgery for the treatment of severe bacterial meningitis with increased intracranial pressure. Acta Anaesthesiol Scand 2006;50:762–5 [DOI] [PubMed] [Google Scholar]


