ABSTRACT
Avian H7 influenza viruses are recognized as potential pandemic viruses, as personnel often become infected during poultry outbreaks. H7 infections in humans typically cause mild conjunctivitis; however, the H7N9 outbreak in the spring of 2013 has resulted in severe respiratory disease. To date, no H7 viruses have acquired the ability for sustained transmission among humans. Airborne transmission is considered a requirement for the emergence of pandemic influenza, and advanced knowledge of the molecular changes or signature required for transmission would allow early identification of pandemic vaccine seed stocks, screening and stockpiling of antiviral compounds, and eradication efforts focused on flocks harboring threatening viruses. Thus, we sought to determine if a highly pathogenic influenza A H7N1 (A/H7N1) virus with no history of human infection could become capable of airborne transmission among ferrets. We show that after 10 serial passages, A/H7N1 developed the ability to be transmitted to cohoused and airborne contact ferrets. Four amino acid mutations (PB2 T81I, NP V284M, and M1 R95K and Q211K) in the internal genes and a minimal amino acid mutation (K/R313R) in the stalk region of the hemagglutinin protein were associated with airborne transmission. Furthermore, transmission was not associated with loss of virulence. These findings highlight the importance of the internal genes in host adaptation and suggest that natural isolates carrying these mutations be further evaluated. Our results demonstrate that a highly pathogenic avian H7 virus can become capable of airborne transmission in a mammalian host, and they support ongoing surveillance and pandemic H7 vaccine development.
IMPORTANCE The major findings of this report are that a highly pathogenic strain of H7N1 avian influenza virus can be adapted to become capable of airborne transmission in mammals without mutations altering receptor specificity. Changes in receptor specificity have been shown to play a role in the ability of avian influenza viruses to cross the species barrier, and these changes are assumed to be essential. The work reported here challenges this paradigm, at least for the influenza viruses of the H7 subtype, which have recently become the focus of major attention, as they have crossed to humans.
INTRODUCTION
Because of their extensive circulation around the globe, avian influenza A viruses of the H7 subtype are occasionally introduced from wild waterfowl into domestic poultry (i.e., chickens). Upon infection of chickens, H7 (and H5) viruses can develop mutations in the cleavage site of the hemagglutinin (HA) protein that render the virus highly pathogenic (HPAI) and lead to high mortality rates, significant economic loss, and further culling of birds to prevent the spread of disease (1).
During outbreaks of H7 influenza, poultry workers can become infected. Infection usually results in a self-limiting, mild conjunctivitis; however, H7 viruses have also caused respiratory infections. HPAI viruses of the H7N7 and H7N3 subtypes have infected humans (2–5), and in March 2013, a low-pathogenicity H7N9 virus emerged in China and was transmitted from poultry in live bird markets to humans. One hundred thirty-three human respiratory infections were reported in 2013, with 43 fatal cases (6–8), and in the fall and winter of 2014, a second wave of the outbreak occurred and is ongoing (9). Experimental studies have shown enhanced recognition of human-like receptors by some of the H7N9 strains, as well as partial airborne transmission in ferrets (10–12). The evolution and emergence of H7N9 highlights the need for continued surveillance and research on H7 viruses.
Influenza pandemics occur when a virus carrying an HA subtype, such as H5, H7, or H9, to which the human population has no preexisting immunity crosses the species barrier and is capable of sustained transmission in humans. Because of a lack of immunity, pandemics can result in severe disease in individuals of all ages. This is illustrated by the “Spanish flu” pandemic of 1918, which resulted in an estimated 50 million deaths worldwide (13); the H2N2 pandemic of 1957 that caused ∼1 million deaths (14); and the more recent 2009 H1N1 pandemic that resulted in increased mortality and hospitalization rates in children and adults relative to seasonal influenza (15). Given the relatively high proportion of individuals who become infected during H7 outbreaks (2–4, 7, 8), there is significant concern that an influenza virus of the H7 subtype could evolve to become capable of transmission among humans and initiate a pandemic. Through recent studies of H5N1, our knowledge of the adaptive traits required for airborne transmission has increased (16, 17); however, the changes required for an H7 isolate to become capable of airborne transmission are largely unknown. Identification of the molecular changes required for airborne transmission of H7 viruses will permit the early identification and preparation of vaccines, facilitate prescreening and stockpiling of antiviral medications, and direct eradication efforts toward flocks harboring viruses with pandemic qualities.
Ferrets represent one of the most suitable animal models of human influenza virus infection. Ferrets transmit seasonal influenza viruses via respiratory droplet and have a distribution of sialic acid receptors similar to that of humans (18). By using a combination of site-directed mutagenesis and serial passage in ferrets, the highly pathogenic avian isolate A/Indonesia/5/2005 (H5N1) was modified to become capable of airborne transmission (16). In addition, a reassortant virus containing the H5 HA with four mutations and seven genes from pH1N1 was also capable of airborne transmission in ferrets (17). Importantly, the mutations identified in these studies are naturally occurring mutations and have already begun to define molecular signatures in H5 viruses that potentiate transmission in mammals.
To identify mutations associated with the transmission of a fully avian H7 virus, we sought to determine if a highly pathogenic H7N1 virus, which carries the PB2 E627K mutation associated with respiratory tract adaptation (19–21), could become capable of airborne transmission in ferrets. For these experiments, the highly pathogenic avian isolate A/ostrich/Italy/2332/2000 (H7N1) (here wild-type [WT] H7N1) was purposely chosen because there were no reported cases of human infection with this virus during the 1999-2000 H7N1 outbreak in Italy (22, 23). In this regard, the present studies were aimed at understanding airborne transmission in a mammalian model while minimizing the chances that such a virus would have characteristics of human adaptation. Here we show that after serial passage, a highly pathogenic H7N1 virus can develop the ability to be transmitted to cohoused (CH) and airborne contact (AC) ferrets. We then proceed to sequence analysis and pathogenesis studies that show four amino acid changes in the internal genes and resolution of a mixed base in the HA-encoding gene were associated with transmission. Importantly, these studies aimed to build upon our understanding of the mechanisms that would permit sustained mammalian transmission. This knowledge will potentially lead to the identification of emerging H7 viruses with pandemic characteristics and enhance pandemic preparedness.
MATERIALS AND METHODS
Virus.
The highly pathogenic isolate A/ostrich/Italy/2332/2000 (H7N1) (22, 24) was used as the WT reference strain and to initiate serial-passage experiments. The virus was propagated in specific-pathogen-free 9-day-old embryonated hen eggs.
Biosafety, biocontainment, and information management.
The information provided in this report highlights the potential of an avian influenza virus of the H7 subtype to gain the capability of airborne transmission. “Gain-of-function” (GOF) studies are essential to understand molecular attributes that make avian influenza viruses potential public health threats and to guide the development of effective therapies. In this particular report, GOF is defined as the adaptation of a highly pathogenic avian influenza virus of the H7N1 subtype with no history of mammalian adaptation to become capable of airborne transmission in the ferret model of influenza virus infection. We have developed biosafety and biosecurity mitigation strategies that, in concert with the findings, provide important information regarding public health risks associated with H7 viruses while greatly minimizing the risk of accidental release and unwanted access to and misuse of this information. During our experiments and prior to the submission of this report for publication, the manuscript was subjected to dual-use research of concern review by the University of Maryland (UMD) Institutional Biosafety Committee and NIAID, NIH. After revisions to address recommendations, both groups supported publication of the findings.
In accordance with the rules and regulations for work with highly pathogenic influenza viruses in the United States, all experiments were conducted in a biosafety level 3 enhanced (BSL3+) facility at UMD. Experiments with both the WT isolate and serially passaged strains were registered and approved by the UMD Institutional Biosafety Committee (IBC 12-52 E-1098). Although the virus described in this study is not the HPAI H5N1 virus, the biosecurity measures taken were in compliance with the NIH guidelines for research involving transmissible strains of the HPAI H5N1 virus. The BSL3+ facility at UMD is maintained under negative pressure, and all exhaust air is passed through two high-efficiency particulate air (HEPA) filters prior to venting. All ventilation fans are redundant, and the facility has a dedicated electrical generator in the event of power loss. All work with tissue and cell cultures is conducted in a class 2 biosafety cabinet in a dedicated tissue culture room, and all animals are housed in separate rooms in animal isolators with both intake and exhaust HEPA filters. All animal handling is performed with a minimum of two authorized users present.
Access to the facility is restricted to users who have undergone extensive training. Prior to BSL3+ training, trainees must meet all requirements to work in both BSL2 and BSL2+ animal facilities and must pass an FBI background check. This is followed by 3 months of training at BSL3+ under an experienced BSL3+ user. While in training, trainees are regularly evaluated by their trainers on the use of all equipment and standard operating procedures. Only after recommendation by the trainer, the facility manager, and the facility director is the trainee permitted independent access to the facility.
Authorized BSL3+ users are subsequently required to complete both monthly departmental training sessions and a yearly training session with representatives from the Biosafety Office, the Fire and Police Departments, and Occupational Health. BSL3+ users must also participate in an Occupational Health plan, which consists of an annual medical exam to ensure that the user is capable of working at BSL3+ and can safely wear a powered air-purifying respirator (PAPR). The health plan also includes yearly vaccination against seasonal influenza. At each annual physical exam, blood is collected from each user and screened for seroconversion against H5, H7, and H9 influenza viruses.
All personnel working at BSL3+ must follow strict entry and exit procedures. Prior to entering the facility, users remove all of their clothing and don dedicated scrubs and a full Tyvek suit. All users are then required to wear a HEPA-filtered PAPR. Once inside the facility, additional personal protective equipment (PPE) and multiple pairs of gloves are worn over the Tyvek suit. Upon exiting the facility, all clothing and PPE is prepared for autoclaving and users are required to shower. To ensure that negative pressure is maintained, the facility is monitored electronically. Users must also check pressure gauges when entering and inside the facility and then log the pressure readings during the exit procedure. After exiting BSL3+, all authorized users must follow a strict quarantine procedure limiting contact with poultry and avian species for 5 days.
In addition, the BSL3+ facility has an information management program. Under this program, all data are stored on password-protected servers that require quarterly password updates. All computers are protected by antivirus software that automatically installs new upgrades as they become available. Servers are further equipped with anti-intrusion software to detect attacks and security breaches and are routinely backed up at remote locations. Furthermore, servers are located behind multiple locked barriers to limit access by nonauthorized personnel.
The BSL3+ facility at UMD complies with all federal and state laws and regulations. The facility is inspected regularly and is also subject to unscheduled inspections by the U.S. Department of Agriculture to ensure compliance with all required procedures and regulations. The most recent inspection was completed in February 2013. All training records, personnel records, and inventories are maintained and are available for inspection by the USDA and/or the UMD Biosafety Office.
Ferret studies.
All ferret studies were performed with approval from the UMD Institutional Animal Care and Use Committee (protocols R-09-93 and R-12-101) and were performed under BSL3+ conditions in HEPA-filtered poultry isolators as previously described (25–28). BSL3+ animal rooms are equipped with motion sensor digital video cameras in order to monitor animal behavior, as well as entry and exit of personnel. For all experiments, 23-week-old, female ferrets (Triple F Farms) were used and all ferrets were seronegative by anti-nucleoprotein (anti-NP) influenza virus enzyme-linked immunosorbent assay (Symbiotic Technologies) prior to infection. Five days prior to experimentation, ferrets were sedated and a subcutaneous transponder (Bio Medic Data Systems) was implanted to identify each animal and provide temperature readings. Ferrets were monitored daily for clinical signs and weight loss. Animals showing weight loss greater than 20%, severe lethargy and diarrhea, or neurological symptoms were euthanized immediately. Several ferret experiments were performed as outlined below.
Experiment 1: transmission of WT A/ostrich/Italy/2332/2000 (H7N1).
Four ferrets were sedated and intranasally inoculated with 1 × 106 50% tissue culture infective doses (TCID50) in 1 ml of phosphate-buffered saline. At 24 h postinoculation, a naive ferret (CH contact) was placed in the same cage with each of the directly inoculated animals and a second naive ferret (AC) was placed in an adjacent cage such that the animal shared the same air space but could not have contact with the other ferrets. Ferrets were monitored for weight loss and clinical signs, and nasal wash fluid samples were collected daily from day 1 postinoculation and day 1 postcontact. Animals were maintained for 21 days, and then blood was collected via cardiac puncture and animals were euthanized. At the completion of the experiment, all nasal wash fluid samples were titrated by TCID50 with an HA assay as the readout (28).
Experiment 2: serial passage and adaptation of two virus lines.
The serial-passage schema used in this experiment is shown in Fig. 1.
FIG 1.
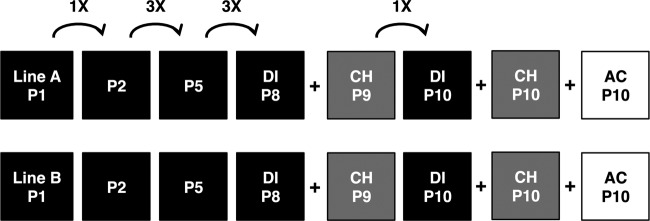
Schematic representation of serial-passage experimental design. Experiment 2 in the ferret study section of Materials and Methods is represented. In serial-passage experiments with each line, passage and evaluation of transmission were limited (n = 1).
Part I.
Two ferrets were inoculated with 1 × 106 TCID50 of WT H7N1 and designated line A or B. Ferrets were nasally washed daily, and extensive precautions (multiple glove changes and disinfection of PPE, tools, and surfaces) were taken between handlings of ferrets. On day 3 or 4 postinoculation, the nasal wash fluid collected from each ferret was subsequently used to inoculate an additional ferret housed in a separate isolator. All ferrets were nasally washed for at least 7 days postinoculation. At the cessation of nasal washing, ferrets were maintained for 21 days and blood was collected prior to euthanasia. Serial passage was performed for eight passages. On the eighth passage, a naive ferret (CH) was introduced into the cage with the infected animal at 24 h postinoculation. With both lines, the CH ferret became infected. The nasal wash fluid samples from the CH ferrets were designated line A or B p9 CH nasal wash fluid.
Part II.
One naive ferret was inoculated with 1 × 105 TCID50 of either line A or B CH p9 nasal wash fluid. This experiment was designated passage 10 (p10). At 24 h postinfection (hpi), both CH and AC ferrets were introduced. Animals were nasally washed daily and monitored for clinical signs.
Experiment 3: airborne transmission with p10 line A virus.
Nasal wash fluid samples from days 2, 3, and 4 postinoculation from the directly infected (DI) line A p10 ferret were combined such that the titer from each day was equivalent. Three ferrets were then inoculated with 1 × 105 TCID50 of this virus solution. At 24 h postinoculation, a CH and an AC animal were introduced to each DI animal. Ferrets were nasally washed daily for 13 days postcontact. Any ferrets showing severe disease (>20% weight loss) and/or neurological symptoms were euthanized immediately. Two AC ferrets developed neurological symptoms and were subjected to necropsy. Brain and lung tissue samples were collected from these two animals for histopathology analysis and virus titrations.
Experiment 4: histopathology and systemic viral load.
To compare the histopathologies and viral loads due to the WT and mammal-adapted viruses, we generated a virus stock designated ACp11 from AC ferret 3 in experiment 3 nasal wash fluid. Six ferrets were then inoculated with 1 × 105 TCID50 of either WT or mammal-adapted ACp11 virus. On days postinfection (dpi) 3, 5, and 7, various tissues were collected for titration and histopathology analysis, including large and small intestine, kidney, liver, spleen, lung, trachea, nasal turbinate, brain, and olfactory bulb tissues. Virus titrations were performed with all of the tissue samples. Fixed tissues were subsequently embedded in paraffin, sectioned, subjected to hematoxylin-and-eosin (H&E) staining, and read by a pathologist who was blind to the sample identities.
Sanger and deep sequencing of virus quasispecies.
We performed Sanger sequencing of the WT A/ostrich/Italy/2332/2000 (H7N1) virus used to initiate the serial-passage studies and the nasal wash fluid of the AC p10 line A ferrets that became infected. Reverse transcription-PCR was performed with sequence-specific primers to generate overlapping fragments 500 to 1,000 nucleotides in length. Fragments were then sequenced with the BigDye Terminator v 3.1 Cycle Sequencing kit (Applied Biosystems, Grand Island, NY) and a 3500XL Sequencer (Applied Biosystems).
Deep sequencing analysis was performed with the following samples: (i) pooled line A DI p10 ferret nasal wash fluid used to initiate p11, (ii) line A AC p10 nasal wash fluid, (iii) one DI p11 ferret nasal wash fluid sample (from F795, which was transmitted to F797), (iv) AC 1 p11 (F797) nasal wash fluid, and (v) AC 3 p11 (F803) nasal wash fluid. Prior to sequencing, nasal wash fluid samples were used to infect MDCK cells at a multiplicity of infection of 0.25. At 24 hpi, the supernatants were collected and RNA was purified with an RNeasy minikit (Qiagen). Subsequently, libraries were constructed (29) and the samples were subjected to GS Junior Titanium Rapid Library Preparation and Emulsion PCR and sequenced according to the manufacturer's protocol (emPCR Amplification Method; Roche) on a Junior 454 Sequencer.
On the basis of sequence information, the ACp10 and ACp11 viruses obtained do not contain mutations known to result in drug resistance and thus would likely remain sensitive to the two most common anti-influenza drugs, i.e., neuraminidase (NA) inhibitors and adamantanes.
RESULTS
Serial passage of H7N1 yields a virus capable of airborne transmission.
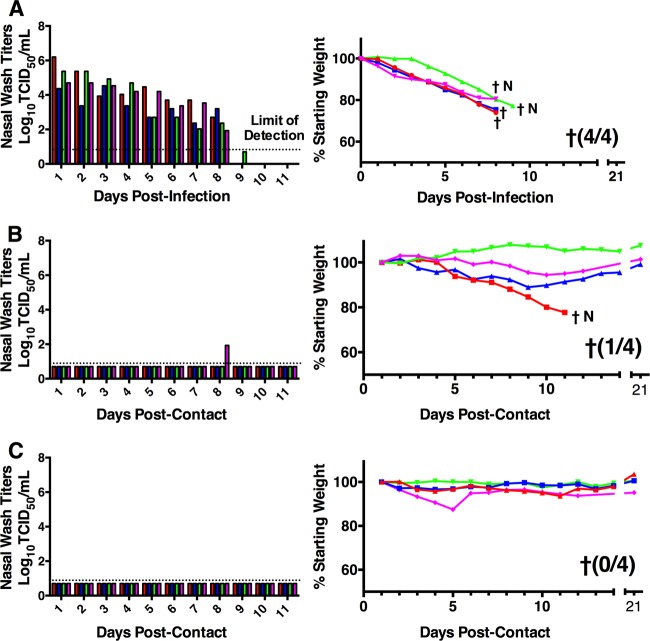
To evaluate the transmissibility of WT H7N1, four ferrets were infected and at 24 hpi, naive CH and AC ferrets were introduced to each inoculated animal. All four DI animals shed high virus titers and developed severe disease, indicated by weight loss, requiring euthanasia by 9 dpi (Fig. 2). Two DI ferrets also displayed neurological signs at the time of euthanasia.
FIG 2.
WT H7N1 shows limited transmission to CH animals in the absence of virus shedding. Four ferrets received 1 × 106 TCID50 of WT H7N1 virus. At 24 hpi, a CH and an AC ferret were introduced to each DI animal. Nasal wash fluid samples were collected daily for virus titration. Viral titers and weight losses of DI (A), CH (B), and AC (C) ferrets. Red (blue, green, or pink) corresponds to one experimental cage setup consisting of three ferrets (one DI, one CH, and one AC ferret) housed in the same isolator. In parentheses is the proportion of ferrets that succumbed to infection or were euthanized. Daggers denote animals that were euthanized or succumbed to infection. N denotes neurological symptoms.
With respect to the CH and AC ferrets, one CH ferret shed virus on a single day (day 8 postcontact) and none of the AC animals shed virus in their nasal wash fluid samples. Another CH ferret showed significant weight loss and developed neurological signs requiring euthanasia. None of the AC animals displayed weight loss or signs of disease. To further determine if the CH and AC ferrets had become infected, hemagglutination inhibition (HI) assays with chicken red blood cells were performed and showed no seroconversion (HI titers of ≤40) by any of the DI, CH, or AC animals (data not shown). This is consistent with previous reports on limited seroconversion against H7 and H5 viruses (30, 31). Collectively, the results of the WT H7N1 transmission study suggest that the virus has a limited ability to be transmitted to CH ferrets and is not capable of airborne transmission, consistent with similar studies of H7N3 viruses (5, 26). A prominent feature of this experiment was the finding that two DI animals and one CH ferret developed neurological disease. Given that the CH ferret did not shed virus, the presence of neurological disease may indicate infection through the ocular route (5). It should be noted that in experimental ferret studies, ocular infection also leads to infection of the upper respiratory tract; however, it is possible that the ability to spread directly from the eye to the brain is a result of the neurotropism of this isolate (24). To further verify a lack of airborne transmission, we performed an additional transmission experiment with three DI and three AC ferrets (i.e., no CH animals). In this experiment, all of the DI animals shed high titers of virus, while none of the AC animals showed signs of disease or shed virus (data not shown). Throughout all ferret studies, we did not observe an increase in sneezing, and a febrile response (i.e., elevation of body temperature) was inconsistent and was not a prominent feature of infection. All infected animals became lethargic, and the neurological symptoms observed included one or more of the following: tremors, tics, uncontrolled shivering, ataxia, and/or hind-limb paralysis.
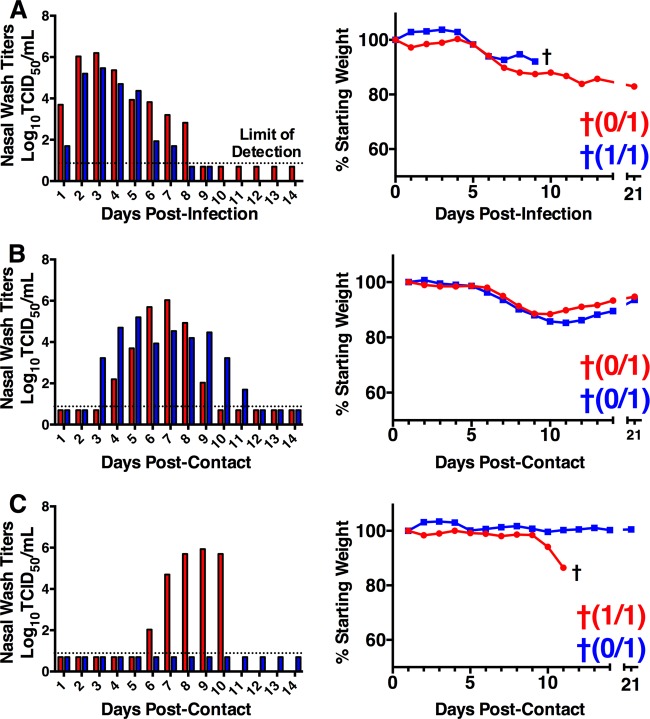
To determine if the WT H7N1 isolate could develop enhanced transmission to CH animals and become capable of airborne transmission, serial passage in ferrets was performed. Two ferrets were inoculated with WT H7N1, and the nasal wash fluid from each ferret was used to inoculate another naive ferret. Two separate lines, designated A and B, were maintained for the duration of the experiment. At passage 5, a limited (n = 1) airborne transmission experiment was performed with each line. Both DI animals shed virus; however, neither of the AC animals became infected (data not shown). Subsequently, three additional serial passages were performed. During the eighth passage, a CH ferret was introduced to each line and both of these ferrets became infected and shed high virus titers (data not shown). Next, the CH passage 9 nasal wash fluid was used to initiate a passage 10 transmission study (Fig. 1 and 3). For each line, one ferret was infected, and at 24 hpi, single CH and AC ferrets were introduced. The DI ferrets for both lines became infected and shed high virus titers (Fig. 3). Both animals showed significant disease, as evident by weight loss, and the line B animal was humanely euthanized. The CH ferrets exposed to both lines became infected and survived. On day 6 postcontact, the line A-exposed AC ferret began to shed virus and continued to do so until day 10, when it succumbed to the infection (Fig. 3C). The line B-exposed AC animal did not become infected or show any signs of disease and was negative by HI assay (data not shown).
FIG 3.
Serial passage yields an H7N1 virus capable of direct and airborne transmission. Two ferrets received 1 × 106 TCID50 of WT H7N1 virus. Serial passage was initiated with nasal wash fluid samples from infected ferrets to inoculate an additional two ferrets. Eight serial passages were performed and maintained as two separate lines, A (red) and B (blue). On the eighth passage, CH animals were introduced and became infected. The nasal wash fluid samples from CH animals were then used to initiate passage 10 (p10). At 24 hpi, a CH and an AC ferret were introduced. Viral titers and weight losses of p10 DI (A), CH (B), and AC (C) animals are shown. In parentheses is the proportion of animals that were euthanized or that succumbed to infection (†).
To determine if there were any mutations associated with airborne transmission, Sanger sequencing of the line A AC nasal wash fluid and WT H7N1 was performed. Eight amino acid changes and several silent mutations were identified in the AC line A nasal wash fluid (Table 1). Of particular interest was the observation that there were minimal amino acid changes in the HA- and NA-encoding surface genes.
TABLE 1.
Sanger sequencing and deep sequencing of DI and infected AC ferretsa
| Protein | Nucleotide change (position) | Amino acid position | Function or domain of mutation (reference[s]) | Frequency (%), line A |
||||
|---|---|---|---|---|---|---|---|---|
| Expt 2, p10 |
Expt 3, p11 |
|||||||
| DI | AC | DI | AC 1 | AC 2 | ||||
| PB2 | C(242)T | T81Ib | NP interaction domain (38) | 100 | 100 | 100 | 100 | 100 |
| PB1 | 750 | G250c | 58 | 86 | 98 | |||
| 2157 | V719c | 28 | 19 | 100 | ||||
| PA | G(204)A | P68b,c | 98 | 100 | 88 | 99 | 100 | |
| G(243)A | G81b,c | 99 | 100 | 90 | 96 | 100 | ||
| HA | G/A(938)G | K/R313Rb | HA stalk globular head (34, 69) | 95 | 100 | 46 | 96 | 100 |
| G583A | G195R | 62 | 40 | 100 | 100 | |||
| NP | G(850)A | V284Mb | PB2 interaction domain (38) | 100 | 100 | 100 | 100 | 100 |
| C(1249)A | L417Ib | PB2 interaction domain (38) | 98 | |||||
| G(546)A | V182b,c | 100 | 100 | 100 | 100 | 98 | ||
| C(1188)T | N396b,c | 100 | 100 | 100 | 100 | 100 | ||
| A(633)G | G211b,c | 100 | ||||||
| NA | T(786)A | D262Eb | Adjacent to NA binding pocket (33) | 42 | 100 | 35 | 100 | |
| G/A(408)A | L136c | 99 | 100 | 100 | 100 | 100 | ||
| A(972)G | V324c | 53 | 99 | 34 | 100 | |||
| A(1071)G | G357c | 41 | 100 | 28 | 100 | |||
| M1 | G(284)A | R95Kb | Spherical virion morphology (62) | 100 | 100 | 100 | 100 | 100 |
| G(632)A | R211Qb | RNP binding domain (63) | 100 | 100 | 100 | 100 | 100 | |
| NS1 | A(328)G | K110Eb | Host protein eIF4GI interaction (70) | 46 | 100 | 56 | 98 | |
Nucleotide and amino acid changes are compared to the published A/ostrich/Italy/2332/2000 (H7N1) sequence that was verified by Sanger sequencing. The changes shown were present at >20% frequency in two or more samples, excluding NP L417I and the silent mutation at NP G211 reported during initial Sanger sequencing of AC p10 line A. Numbering reflects that of the full-length H7N1 amino acid sequence. HA numbering refers to H7 numbering starting at methionine. Absence of a frequency indicates 0% and no changes were found in M2 and NS2. Five mutations present in all DI and AC ferrets are in bold. Mutations also found in A/Anhui/1/2013 and A/Shanghai/2/2013 (H7N9) are underlined.
Amino acid and/or nucleotide change found during Sanger sequencing of p10 line A AC.
Silent or synonymous mutation.
To more fully characterize the transmission of the ferret-adapted virus and to maintain quasispecies diversity, a larger transmission study was performed with a pool of nasal wash fluid samples from the DI line A p10 animal. This was designated passage 11 (p11). As described above, at 24 hpi, CH and AC animals were introduced. At 1 dpi, all three DI animals shed virus in their nasal wash fluid (Fig. 4) and continued to shed virus for at least 6 days. By day 5 postcontact, all of the CH animals had become infected and similarly shed virus for at least 5 days. All infected animals showed weight loss and clinical disease; two of three DI animals and one of three CH animals were euthanized because of severe disease. On days 6 and 8 postcontact, two separate AC ferrets (no. 1 and 3) began to shed virus in their nasal wash fluid (Fig. 4C). Both ferrets shed increasing titers of virus until they developed severe neurological signs requiring euthanasia. Both of these animals were subjected to necropsy, with brain tissue showing high levels of replicating virus consistent with neurological disease, while only one animal had virus detected in the lung (Fig. 5). The remaining AC ferret (no. 2) did not become infected and was negative by HI assay.
FIG 4.
Ferret-adapted H7N1 is transmitted to CH and AC animals in a larger transmission study. Three ferrets received a pool of nasal wash fluid samples from line A p10 DI ferret (1 × 105 TCID50 of pooled virus). At 24 hpi, a CH and an AC ferret were introduced to the DI animals. Viral titers and percent weight losses of DI (A), CH (B), and AC (C) animals are shown. Red (blue or green) corresponds to one experimental cage setup consisting of three ferrets (one DI, one CH, and one AC) housed in the same isolator. Shown in parentheses is the proportion of ferrets that developed severe disease and were euthanized or succumbed to infection (†). N denotes neurological symptoms.
FIG 5.
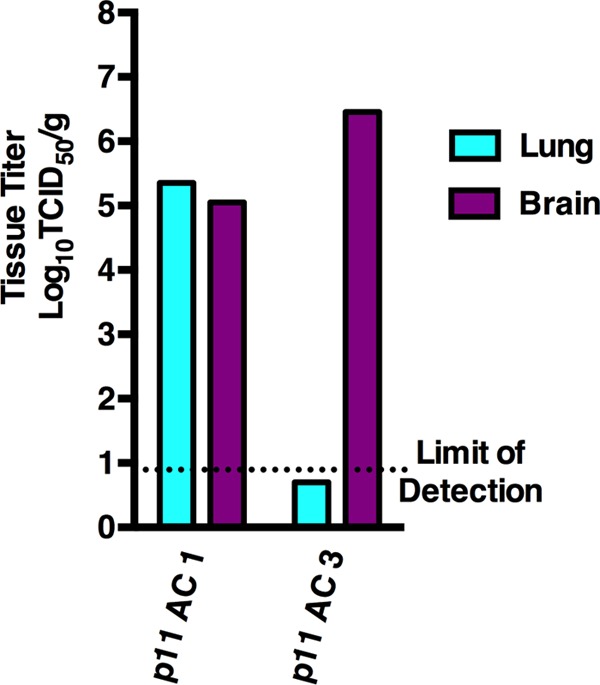
Titration of brain and lung samples from AC animals shows high virus titers in the brain. In experiment 3, two AC animals became infected and developed neurological disease requiring euthanasia. Both ferrets were subjected to necropsy. Brain and lung samples were collected for titration. Shown above are viral titers in the lungs and brains of both animals. Both animals had replicating virus in the brain, while only one animal had detectable virus in the lungs.
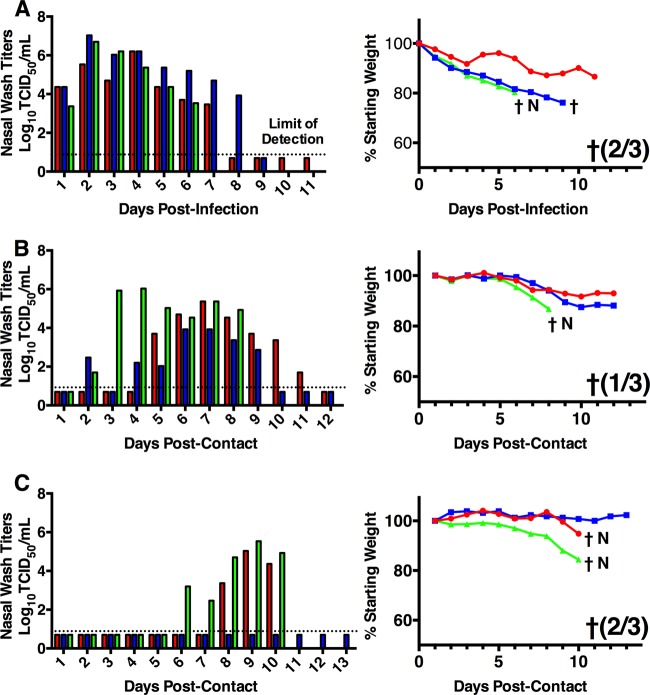
Pathogenesis and tissue viral loads due to WT and airborne transmission-capable H7N1.
To evaluate systemic infection and determine if transmission was associated with respiratory tract viral load differences, six ferrets were inoculated with either WT H7N1 or ACp11 H7N1 (virus stock generated from p11 AC 3 (green in Fig. 4C) and tissues were collected at 3, 5, and 7 dpi. Upon virus titration, no virus was detected in the large or small intestine or in the kidney, spleen, or liver; however, at 3 and 5 dpi, virus was consistently isolated from the nasal turbinates, trachea, and lungs (Fig. 6). Given the limited number of ferrets used for these studies, no significant differences between the WT and ACp11 virus-infected animals were found; however, when the viral loads in the nasal turbinates and trachea were examined, there appeared to be slightly higher titers of ACp11 than WT virus on dpi 3 and 5. In contrast, in the lungs, there was up to a 1-log increase in WT virus levels over ACp11 virus levels. On dpi 7, no WT-infected animals and only one ACp11-infected animal had virus in the trachea, while none of the ACp11-infected animals and only one WT-infected animal had virus in the lungs. This suggests that serial passage may have enhanced replication in the upper respiratory tract, while the WT virus appears to replicate preferentially in the lungs.
FIG 6.
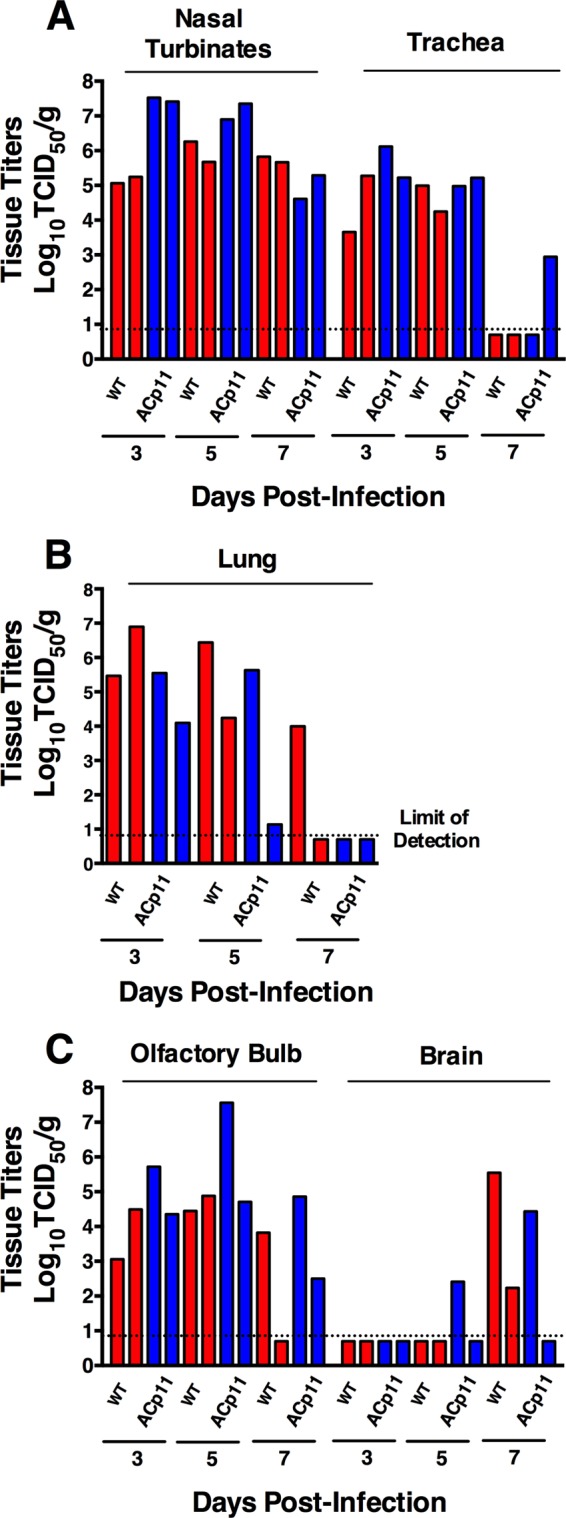
Viral loads in the respiratory tract and nervous system tissues of WT H7N1- and ferret-adapted ACp11-infected ferrets. Six ferrets were inoculated with 1 × 105 TCID50 of either WT H7N1 or ACp11 H7N1 (virus stock generated from p11 AC 3). Tissue samples were collected from the large and small intestines, kidneys, spleen, liver, lungs, trachea, nasal turbinates, brain, and olfactory bulb. Tissue samples were titrated and normalized to the weight of input tissue. No virus was isolated from the intestines, kidneys, spleen, or liver. Each bar represents the viral load of an individual ferret. Viral titers are shown for upper respiratory tract tissue (nasal turbinates and trachea) (A), the lower respiratory tract or lungs (B), and nervous system tissue (olfactory bulb and brain) (C).
Evaluation of virus replication in nervous tissues reveals that both the WT and ACp11 viruses grew to high titers in the olfactory bulb and the ACp11 virus shows titers equivalent to or slightly higher than (although not significantly different from) those of the WT virus. With respect to viral loads in brain tissue, one ACp11-infected animal was positive on day 5, another was positive on day 7, and two WT-infected animals were positive on day 7. During this experiment, no animals exhibited signs of neurological disease. The variation in viral loads in brain tissue is consistent with the general variation in clinical signs observed throughout these studies and may reflect the outbred nature of ferrets.
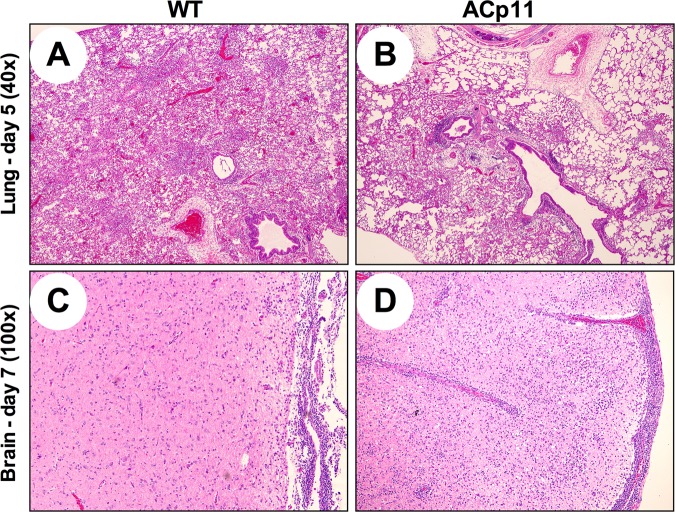
On day 3, animals infected with WT or ACp11 virus showed minimal pathology in the lungs, trachea, and brain (Table 2). At 5 dpi, WT virus-infected animals had severe lung disease characterized by diffuse alveolar edema, while the trachea and brain remained largely unaffected (Fig. 7). In all tissues from animals infected with ACp11 virus, minimal disease and pathology were observed on day 5. By day 7, both WT- and ACp11-infected animals showed comparable mild or moderate disease in the lungs and trachea; however, they differed in disease severity in the brain. ACp11-infected animals exhibited marked focal meningitis and encephalitis with lymphocytes in the thalamus, while WT-infected animals also showed meningitis but with reduced severity (Fig. 7 and Table 2). These findings of more pronounced lung disease with WT virus are in agreement with the observation of slightly higher viral loads in the lungs. However, the findings in the brain are in contrast to the viral load data. Only one ACp11-infected animal had virus isolated from the brain (Fig. 6). This may reflect sampling, as only a small amount (∼0.5 g) of brain tissue was tested for virus while an entire section of the left hemisphere of the brain was examined for histopathology.
TABLE 2.
Histopathology scores at dpi 3, 5, and 7 of lung, bronchus/bronchiole, alveolar, pulmonary vasculature, tracheal, and brain tissues from ferrets infected with WT H7N1 or ACp11
| Time, virus, and ferret | Histopathology scorea of tissue from: |
|||||
|---|---|---|---|---|---|---|
| Lungs | Bronchi/bronchioles | Alveoli | Vascular tissue | Trachea | Brain | |
| 3 dpi | ||||||
| WT | ||||||
| F828 | − | − | − | − | − | − |
| F829 | + | − | + | − | − | + |
| ACp11 | ||||||
| F834 | ++ | ++ | ++ | − | ++ | − |
| F835 | − | − | − | + | + | + |
| 5 dpi | ||||||
| WT | ||||||
| F830 | ++++ | +++ | ++++ | ++ | ++ | + |
| F831 | +++ | ++ | +++ | ++ | + | + |
| ACp11 | ||||||
| F836 | ++ | ++ | ++ | + | + | + |
| F837 | − | − | − | − | − | + |
| 7 dpi | ||||||
| WT | ||||||
| F832 | +++ | +++ | +++ | ++ | ++ | ++ |
| F833 | ++ | ++ | ++ | ++ | ++ | ++ |
| ACp11 | ||||||
| F838 | ++ | ++ | ++ | + | ++ | +++ |
| F839 | +++ | +++ | ++ | ++ | + | +++ |
Tissues were collected from two animals at each time point and scored by a veterinary pathologist blinded to the identity of the virus strain. Lesion grading: −, normal; +, minimal; ++, mild; +++, moderate; ++++, severe.
FIG 7.
Histopathology of lung and brain samples showing differences in inflammation between animals infected with WT H7N1 or ACp11 virus on dpi 5 and 7. Ferrets (n = 6/virus) were infected with either WT H7N1 or ACp11. On dpi 3, 5, and 7, lung, trachea, and brain samples were collected for evaluation of histopathology. All sections were fixed and subjected to H&E staining. Sections were viewed and scored by a veterinary pathologist blinded to the virus strain's identity. Shown are representative images of dpi 5 lung sections from WT H7N1 (A)- and ACp11 (B)-infected ferrets and dpi 7 brain sections from WT H7N1 (C)- and ACp11 (D)-infected ferrets.
Molecular changes associated with airborne transmission.
To further evaluate the mutations associated with respiratory transmission and the quasispecies present in the animals that became infected via airborne transmission, deep sequencing of ferret nasal wash fluid samples was performed. Sequences were obtained from the pooled line A DI p10 nasal wash fluid used to initiate p11, the single line A ACp10 ferret nasal wash fluid sample, one DI p11 nasal wash fluid sample, and the nasal wash fluid samples from the two AC p11 ferrets that became infected. Five amino acid mutations were found at high frequencies of 96 to 100% in all of the AC animals and were also present in the DI animals (Table 1). These mutations were PB2 T81I, HA K/R313R (304 H3 numbering), NP V284M, and M1 R95K and R211Q and are consistent with those found by Sanger sequencing. In all of the ferret nasal wash fluid samples examined, the PB2 E627K mutation was maintained. Three mutations (NP L417I, NA D262E, and NS1 K110E) in the ACp10 line A nasal wash fluid were not consistently maintained in the other AC ferrets, indicating that they were not required for airborne transmission. The deep sequencing results also indicate that only one minimal change in the surface gene for HA, K/R313R, resulted from the serial-adaptation studies, while several changes in the internal genes became fixed during this process.
There were also additional mutations at various prevalences (i.e., in 2/3 AC ferrets) and frequencies (i.e., 40 to 100%) in the HA- and NA-encoding genes. Both p11 AC ferrets display a G195R mutation in HA (relative to methionine and position 186 H3 numbering). This mutation was not present in the line A ACp10 nasal wash fluid, indicating that it is not required for airborne transmission; however, its presence at a frequency of 100% in the p11 AC ferrets suggests ongoing adaptation. Continued adaptation is also illustrated by the NA mutation D262E (D284E when correcting for a 22-amino-acid [aa] deletion in the stalk) (32). This mutation is located in close proximity to conserved amino acids (E276, E277, and R292 in N1) in the NA binding pocket and may influence NA activity (33). This mutation was present at a frequency of 100% in the line A ACp10 nasal wash fluid and in one of the two p11 AC ferrets, also suggesting a degree of selection. It is possible that these two additional mutations, along with the other five mutations found in all of the nasal wash fluid samples, may lead to enhanced transmission. Importantly, none of the mutations are known to change the susceptibility of influenza viruses to NA inhibitors or adamantanes.
DISCUSSION
In this report, a fully avian H7N1 virus was adapted to become capable of airborne transmission in ferrets. The virus also showed transmission to all CH animals, suggesting that transmission via direct contact was also enhanced; however, it is possible that airborne transmission could also occur in CH animals. The findings are consistent with those on the adaptation of highly pathogenic H5N1 (16), as no reassortment event was required to yield a virus capable of airborne transmission. In agreement with studies on H9N2 and H5N1, a limited number of amino acid mutations (five or six) were associated with airborne transmission and serial passage leads to mammalian adaptation (16, 25, 27). In the HA-encoding gene, we identified a single mutation present in all AC ferrets, resolution of K/R313R. This mutation is located in the stalk region of H7 HA. Thus, it is unlikely to influence receptor binding. The receptor-binding preference of WT H7N1 was previously characterized and shown to be consistent with typical avian H7 HA proteins displaying an α2,3 sialic acid binding preference (34). From studies on transmissible H5 viruses, the stabilizing mutations T318I and H103Y (H3 numbering) in the stalk were reported (17). These mutations did not alter receptor-binding preference, and the T318I mutation was shown to stabilize the HA protein when combined with destabilizing/loss of a glycosylation site mutation N158D. Furthermore, transmission studies with HA-stabilizing mutations alone resulted in inefficient transmission in ferrets (35, 36). Thus, in the context of the ferret-adapted H7 virus, the stalk mutation alone is unlikely to be sufficient to result in airborne transmission and the internal genes potentially play a more significant role.
The viral ribonucleoprotein (vRNP) genes are also known to harbor host range determinants (37, 38). For example, PB2 mutations E627K and D701N have been well characterized and enhance polymerase activity and growth in mammalian cells at 33°C (21, 39, 40). PB2 and NP have been shown to enter the nucleus by the classical importin-α/β1 nuclear import pathway (41). The importin pathway is thought to represent a mechanism of host switching, as the PB2 E627K mutation changes the preferred importin isotype from importin-α3 to importin-α7, which are utilized by avian and human isolates, respectively (42, 43). In our airborne-transmission-capable H7N1 virus, we found two mutations in the vRNP-encoding genes, PB2 T81I and NP V284M. Sequence variation at position 81 in PB2 has previously been identified by bioinformatic approaches (37, 44). Results obtained by these approaches show an association between the polar amino acid threonine at position 81 in avian viruses, while the nonpolar amino acids, valine or methionine, are prevalent in human viruses. The T81I mutation causes a similar change to a nonpolar amino acid and may reflect mammalian adaptation. Importantly, we also compared the PB2 sequence of WT H7N1 to that of an H5N1 virus that acquired virulence after serial passage in mice (45). We found that all six mutations in the serially passaged H5N1 virus (L89V, G309D, T339K, R477G, I495V, and A676T) were also present in PB2 of the WT H7N1 isolate, indicating that in addition to PB2 E627K, the H7N1 virus already carries mutations indicative of mammalian adaptation.
The mutation V284M identified in NP has not been previously reported; however, this mutation is in the C-terminal PB2 interaction domain and is adjacent (aligns with position 285 in NP from H1N1) to position 283, at which a lysine is associated with avian viruses and a proline is associated with human viruses (44, 46). Importantly, this change in the NP C-terminal PB2 interaction domain occurs in parallel with the T81I change in the PB2 N-terminal NP interaction domain (33), indicating that these may be compensatory mutations modulating NP-PB2 binding. Combined, these two mutations may further promote nuclear import by importin-α7 and/or may enhance polymerase activity and growth at lower temperatures in mammalian cells. Importantly, the combination of PB2 D701N and NP N319K in an H7N7 isolate led to importin-α7 dependency in human cells (42, 43). The NP mutation V284M is in proximity to the N319K mutation and thus, alone or combined with the E627K mutation, may further promote switching to use of the importin-α7 isotype. Furthermore, the vRNP genes have also been shown to interact with several other host factors (47–49) and the mutations in NP and PB2 could also alter these interactions. Lastly, we also found two silent mutations at high frequencies in PA and two silent mutations in NP. The high prevalence of these mutations suggests a role for adaptation of genes at the nucleotide level.
The prevalence of both silent and amino acid mutations in the viral polymerase genes underscores the need for ongoing development of new antiviral strategies. While our transmissible H7N1 virus does not harbor mutations that confer resistance to existing antivirals, amantadine resistance is prevalent in circulating human influenza viruses and oseltamivir-resistant viruses are being isolated with increasing frequency (50–52). The mutations in NP and PB2 highlight the need for strategies that specifically target the viral polymerase, and several compounds are currently under development (53–58). For example, nucleozin causes NP oligomerization in the cytoplasm, limiting nuclear import and assembly of vRNPs (55), and cycloheptathiophene-3-carboxamide derivatives inhibit PB1-PA interactions (56). Importantly, as mutations in the internal genes appear to be a determinant in the evolution of the transmission phenotype, the use of antiviral agents targeting the viral polymerase during outbreaks could slow or prevent the emergence of a virus capable of airborne transmission and/or causing a pandemic.
The matrix gene has also previously been associated with transmission, particularly in the context of pH1N1 reassortant viruses (59–61). In our transmissible H7N1 virus, two mutations in M1, R95K and R211Q, became fixed. The R95K mutation has been shown to change virion morphology from filamentous to spherical (62), and electron microscopy studies are required to verify a change in morphology. The R211Q mutation is in the region responsible for binding the RNPs (63). The defined RNP binding domain of M1 is large (aa 165 to 212); thus, it is difficult to determine if the R211Q mutation would influence the function of M1.
Given the transmission phenotype identified, one may postulate that modifying other influenza viruses with the same mutations would confer a similar phenotype. While these mutations may be associated with respiratory transmission, such an occurrence would likely be limited to other similar H7 viruses, as other characteristics of a virus strain are also expected to influence transmission. The present findings show that adaptation of the H7N1 isolate does not appear to substantially decrease the virulence of the virus. It is tempting to speculate that the neurotropic phenotype of this virus is more likely an inherent property of this isolate (24) rather than a result of adaptation or infection via the airborne route. The findings of limited changes on the surface genes of the H7N1 virus also stand in contrast to the paradigm that host receptor switching and adaptive changes in the HA are required for respiratory transmission and mammalian adaptation. It is conceivable that the polybasic cleavage site in combination with the ability of H7 viruses to more readily cross the species barrier may overcome the requirement for additional changes in the HA-encoding gene.
Regardless, our findings emphasize the requirement for continued development of H7 pandemic vaccine seed stocks. Current H7 vaccines under development are directed against A/Netherlands/219/2003 (H7N7). In clinical trials, inactivated H7N7 vaccines have been poorly immunogenic (64); however, live-attenuated vaccines against H7N7 have shown protection in mice, ferrets, and monkeys (31), and human trials evaluating immunogenicity of the live-attenuated H7N7 vaccine are under way (65, 66). Given that the HA from A/ostrich/Italy/2332/2000 (H7N1) is from clade 1.1 and is closely related to that of A/Netherlands/219/2003 (H7N7) (34), it is likely that the H7N7 vaccines would also confer protection against H7N1.
Given the public health concern about H7N9, we analyzed the amino acid sequences of two prototypic H7N9 isolates (A/Anhui/1/2013 and A/Shanghai/2/2013) for the five mutations consistently identified in our studies. The two mutations we found in M1 were also found in the H7N9 isolates. In addition, both the WT H7N1 and serially passaged H7N1 viruses have the PB2 E627K mutation in common with the H7N9 isolates. Since the H7N9 isolates have caused human infections and showed limited airborne transmission in ferrets (10–12), the mutations in M1 may be indicative of adaptation to growth in a mammalian host; however, the internal genes of the H7N9 isolates are derived from an H9N2 virus (67) and M1 mutations in the H9N2 background have not been described. The role of these mutations in airborne transmission cannot be negated, and further studies should be conducted to determine if these mutations influence the transmission of both H7 and H9 viruses. Furthermore, given that two amino acid changes identified were also found in H7N9 isolates, we propose that an H7 genetic change inventory, analogous to the H5N1 inventory maintain by the CDC, be generated and describe mutations associated with H7 transmission. With this in mind, both low- and high-pathogenicity H7 isolates should be monitored for these mutations. Any isolates identified with two or more mutations should be evaluated for transmission potential in ferrets, and further studies evaluating the efficacy of existing vaccines and antiviral agents should also be performed.
Considering that only one change in the gene for HA, in combination with several mutations in the internal genes, was required for airborne transmission of the H7N1 virus, our findings suggest that reassortment with other influenza viruses may yield an H7 virus capable of mammalian transmission with minimal adaptation. This is perhaps illustrated by the recent H7N9 outbreak, in which a reassortant between an H7 and an H9N2 virus resulted in a virus capable of transmission from birds to humans, although without human-to-human transmission (8). This is also supported by our previous work in which reassortment of an avian H9N2 virus with a seasonal H3N2 virus or pandemic H1N1 yielded viruses capable of transmission in ferrets (25, 27).
It is important to note that transmission to AC animals occurs relatively late during infection, usually on day 6 or 7. This is in contrast to infection with either pandemic H1N1 or seasonal influenza virus strains that display faster transmission kinetics, usually being transmitted on day 3 or 4 (68). This suggests that while the H7N1 isolate was capable of airborne transmission, it may not have acquired the transmission efficiency required to become pandemic. Further work is required to define the mechanism and contribution of each mutation to transmission. This work, in conjunction with studies on the airborne transmission of other influenza virus subtypes, will, we hope, yield a transmission roadmap that characterizes adaptive changes in the virus rather than amino acid mutations. Such a roadmap will enhance pandemic preparedness and permit the development of vaccines against novel influenza virus strains as they emerge.
ACKNOWLEDGMENTS
We acknowledge J. B. Kimble for advice and Andrea Ferrero for support of the BSL3+ facility. T.C.S., C.F., and D.R.P. planned all of the animal experiments, performed data analysis, and wrote the manuscript. T.C.S. and C.F. performed all of the animal experiments with assistance from H.S. M.A. assisted with deep sequencing. H.C., M.A., and H.S. assisted with data analysis and manuscript preparation. I.C., G.C., and I.M. provided reagents and assisted with data analysis and manuscript preparation.
This research was funded by NIH NIAID contract HHSN26620070001.
Footnotes
Published ahead of print 2 April 2014
REFERENCES
- 1.Palese P, Shaw ML. 2007. Orthomyxoviridae: the viruses and their replication, p 1648–1692 In Knipe DM, Howley PM. (ed), Fields virology, 5th ed, vol 1 Lippincott Williams and Wilkins, Philadelphia, PA [Google Scholar]
- 2.Fouchier RA, Schneeberger PM, Rozendaal FW, Broekman JM, Kemink SA, Munster V, Kuiken T, Rimmelzwaan GF, Schutten M, Van Doornum GJ, Koch G, Bosman A, Koopmans M, Osterhaus AD. 2004. Avian influenza A virus (H7N7) associated with human conjunctivitis and a fatal case of acute respiratory distress syndrome. Proc. Natl. Acad. Sci. U. S. A. 101:1356–1361. 10.1073/pnas.0308352100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koopmans M, Wilbrink B, Conyn M, Natrop G, van der Nat H, Vennema H, Meijer A, van Steenbergen J, Fouchier R, Osterhaus A, Bosman A. 2004. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet 363:587–593. 10.1016/S0140-6736(04)15589-X [DOI] [PubMed] [Google Scholar]
- 4.Tweed SA, Skowronski DM, David ST, Larder A, Petric M, Lees W, Li Y, Katz J, Krajden M, Tellier R, Halpert C, Hirst M, Astell C, Lawrence D, Mak A. 2004. Human illness from avian influenza H7N3, British Columbia. Emerg. Infect. Dis. 10:2196–2199. 10.3201/eid1012.040961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Belser JA, Davis CT, Balish A, Edwards LE, Zeng H, Maines TR, Gustin KM, Martinez IL, Fasce R, Cox NJ, Katz JM, Tumpey TM. 2013. Pathogenesis, transmissibility, and ocular tropism of a highly pathogenic avian influenza A (H7N3) virus associated with human conjunctivitis. J. Virol. 87:5746–5754. 10.1128/JVI.00154-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO. 2013. Report 8: number of confirmed human cases of avian influenza A(H7N9) reported to the WHO. World Health Organization, Geneva, Switzerland [Google Scholar]
- 7.Chen Y, Liang W, Yang S, Wu N, Gao H, Sheng J, Yao H, Wo J, Fang Q, Cui D, Li Y, Yao X, Zhang Y, Wu H, Zheng S, Diao H, Xia S, Chan KH, Tsoi HW, Teng JL, Song W, Wang P, Lau SY, Zheng M, Chan JF, To KK, Chen H, Li L, Yuen KY. 2013. Human infections with the emerging avian influenza A H7N9 virus from wet market poultry: clinical analysis and characterisation of viral genome. Lancet 381:1916–1925. 10.1016/S0140-6736(13)60903-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gao R, Cao B, Hu Y, Feng Z, Wang D, Hu W, Chen J, Jie Z, Qiu H, Xu K, Xu X, Lu H, Zhu W, Gao Z, Xiang N, Shen Y, He Z, Gu Y, Zhang Z, Yang Y, Zhao X, Zhou L, Li X, Zou S, Zhang Y, Yang L, Guo J, Dong J, Li Q, Dong L, Zhu Y, Bai T, Wang S, Hao P, Yang W, Han J, Yu H, Li D, Gao GF, Wu G, Wang Y, Yuan Z, Shu Y. 2013. Human infection with a novel avian-origin influenza A (H7N9) virus. N. Engl. J. Med. 368:1888–1897. 10.1056/NEJMoa1304459 [DOI] [PubMed] [Google Scholar]
- 9.WHO. 2014. Human infection with avian influenza A(H7N9) virus–update. World Health Organization, Geneva, Switzerland: http://www.who.int/csr/don/2014_04_04/en/ [Google Scholar]
- 10.Zhu H, Wang D, Kelvin DJ, Li L, Zheng Z, Yoon SW, Wong SS, Farooqui A, Wang J, Banner D, Chen R, Zheng R, Zhou J, Zhang Y, Hong W, Dong W, Cai Q, Roehrl MH, Huang SS, Kelvin AA, Yao T, Zhou B, Chen X, Leung GM, Poon LL, Webster RG, Webby RJ, Peiris JS, Guan Y, Shu Y. 2013. Infectivity, transmission, and pathology of human-isolated H7N9 influenza virus in ferrets and pigs. Science 341:183–186. 10.1126/science.1239844 [DOI] [PubMed] [Google Scholar]
- 11.Watanabe T, Kiso M, Fukuyama S, Nakajima N, Imai M, Yamada S, Murakami S, Yamayoshi S, Iwatsuki-Horimoto K, Sakoda Y, Takashita E, McBride R, Noda T, Hatta M, Imai H, Zhao D, Kishida N, Shirakura M, de Vries RP, Shichinohe S, Okamatsu M, Tamura T, Tomita Y, Fujimoto N, Goto K, Katsura H, Kawakami E, Ishikawa I, Watanabe S, Ito M, Sakai-Tagawa Y, Sugita Y, Uraki R, Yamaji R, Eisfeld AJ, Zhong G, Fan S, Ping J, Maher EA, Hanson A, Uchida Y, Saito T, Ozawa M, Neumann G, Kida H, Odagiri T, Paulson JC, Hasegawa H, Tashiro M, Kawaoka Y. 2013. Characterization of H7N9 influenza A viruses isolated from humans. Nature 501:551–555. 10.1038/nature12392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Belser JA, Gustin KM, Pearce MB, Maines TR, Zeng H, Pappas C, Sun X, Carney PJ, Villanueva JM, Stevens J, Katz JM, Tumpey TM. 2013. Pathogenesis and transmission of avian influenza A (H7N9) virus in ferrets and mice. Nature 501:556–559. 10.1038/nature12391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson NP, Mueller J. 2002. Updating the accounts: global mortality of the 1918-1920 “Spanish” influenza pandemic. Bull. Hist Med. 76:105–115. 10.1353/bhm.2002.0022 [DOI] [PubMed] [Google Scholar]
- 14.Potter CW. 2001. A history of influenza. J. Appl. Microbiol. 91:572–579. 10.1046/j.1365-2672.2001.01492.x [DOI] [PubMed] [Google Scholar]
- 15.Chowell G, Bertozzi SM, Colchero MA, Lopez-Gatell H, Alpuche-Aranda C, Hernandez M, Miller MA. 2009. Severe respiratory disease concurrent with the circulation of H1N1 influenza. N. Engl. J. Med. 361:674–679. 10.1056/NEJMoa0904023 [DOI] [PubMed] [Google Scholar]
- 16.Herfst S, Schrauwen EJ, Linster M, Chutinimitkul S, de Wit E, Munster VJ, Sorrell EM, Bestebroer TM, Burke DF, Smith DJ, Rimmelzwaan GF, Osterhaus AD, Fouchier RA. 2012. Airborne transmission of influenza A/H5N1 virus between ferrets. Science 336:1534–1541. 10.1126/science.1213362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, Li C, Kawakami E, Yamada S, Kiso M, Suzuki Y, Maher EA, Neumann G, Kawaoka Y. 2012. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 486:420–428. 10.1038/nature10831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Munster VJ, de Wit E, van den Brand JM, Herfst S, Schrauwen EJ, Bestebroer TM, van de Vijver D, Boucher CA, Koopmans M, Rimmelzwaan GF, Kuiken T, Osterhaus AD, Fouchier RA. 2009. Pathogenesis and transmission of swine-origin 2009 A(H1N1) influenza virus in ferrets. Science 325:481–483. 10.1126/science.1177127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Wit E, Munster VJ, van Riel D, Beyer WE, Rimmelzwaan GF, Kuiken T, Osterhaus AD, Fouchier RA. 2010. Molecular determinants of adaptation of highly pathogenic avian influenza H7N7 viruses to efficient replication in the human host. J. Virol. 84:1597–1606. 10.1128/JVI.01783-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hatta M, Gao P, Halfmann P, Kawaoka Y. 2001. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science 293:1840–1842. 10.1126/science.1062882 [DOI] [PubMed] [Google Scholar]
- 21.Subbarao EK, London W, Murphy BR. 1993. A single amino acid in the PB2 gene of influenza A virus is a determinant of host range. J. Virol. 67:1761–1764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Capua I, Mutinelli F, Pozza MD, Donatelli I, Puzelli S, Cancellotti FM. 2002. The 1999-2000 avian influenza (H7N1) epidemic in Italy: veterinary and human health implications. Acta Trop. 83:7–11. 10.1016/S0001-706X(02)00057-8 [DOI] [PubMed] [Google Scholar]
- 23.Puzelli S, Di Trani L, Fabiani C, Campitelli L, De Marco MA, Capua I, Aguilera JF, Zambon M, Donatelli I. 2005. Serological analysis of serum samples from humans exposed to avian H7 influenza viruses in Italy between 1999 and 2003. J. Infect. Dis. 192:1318–1322. 10.1086/444390 [DOI] [PubMed] [Google Scholar]
- 24.Rigoni M, Shinya K, Toffan A, Milani A, Bettini F, Kawaoka Y, Cattoli G, Capua I. 2007. Pneumo- and neurotropism of avian origin Italian highly pathogenic avian influenza H7N1 isolates in experimentally infected mice. Virology 364:28–35. 10.1016/j.virol.2007.02.031 [DOI] [PubMed] [Google Scholar]
- 25.Kimble JB, Sorrell E, Shao H, Martin PL, Perez DR. 2011. Compatibility of H9N2 avian influenza surface genes and 2009 pandemic H1N1 internal genes for transmission in the ferret model. Proc. Natl. Acad. Sci. U. S. A. 108:12084–12088. 10.1073/pnas.1108058108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Song H, Wan H, Araya Y, Perez DR. 2009. Partial direct contact transmission in ferrets of a mallard H7N3 influenza virus with typical avian-like receptor specificity. Virol. J. 6:126. 10.1186/1743-422X-6-126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sorrell EM, Wan H, Araya Y, Song H, Perez DR. 2009. Minimal molecular constraints for respiratory droplet transmission of an avian-human H9N2 influenza A virus. Proc. Natl. Acad. Sci. U. S. A. 106:7565–7570. 10.1073/pnas.0900877106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pena L, Sutton T, Chockalingam A, Kumar S, Angel M, Shao H, Chen H, Li W, Perez DR. 2013. Influenza viruses with rearranged genomes as live-attenuated vaccines. J. Virol. 87:5118–5127. 10.1128/JVI.02490-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Djikeng A, Halpin R, Kuzmickas R, Depasse J, Feldblyum J, Sengamalay N, Afonso C, Zhang X, Anderson NG, Ghedin E, Spiro DJ. 2008. Viral genome sequencing by random priming methods. BMC Genomics 9:5. 10.1186/1471-2164-9-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beato MS, Monne I, Mancin M, Bertoli E, Capua I. 2010. A proof-of-principle study to identify suitable vaccine seed candidates to combat introductions of Eurasian lineage H5 and H7 subtype avian influenza viruses. Avian Pathol. 39:375–382. 10.1080/03079457.2010.513376 [DOI] [PubMed] [Google Scholar]
- 31.Min JY, Vogel L, Matsuoka Y, Lu B, Swayne D, Jin H, Kemble G, Subbarao K. 2010. A live attenuated H7N7 candidate vaccine virus induces neutralizing antibody that confers protection from challenge in mice, ferrets, and monkeys. J. Virol. 84:11950–11960. 10.1128/JVI.01305-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Banks J, Speidel ES, Moore E, Plowright L, Piccirillo A, Capua I, Cordioli P, Fioretti A, Alexander DJ. 2001. Changes in the haemagglutinin and the neuraminidase genes prior to the emergence of highly pathogenic H7N1 avian influenza viruses in Italy. Arch. Virol. 146:963–973. 10.1007/s007050170128 [DOI] [PubMed] [Google Scholar]
- 33.Colman PM, Varghese JN, Laver WG. 1983. Structure of the catalytic and antigenic sites in influenza virus neuraminidase. Nature 303:41–44. 10.1038/303041a0 [DOI] [PubMed] [Google Scholar]
- 34.Gambaryan AS, Matrosovich TY, Philipp J, Munster VJ, Fouchier RA, Cattoli G, Capua I, Krauss SL, Webster RG, Banks J, Bovin NV, Klenk HD, Matrosovich MN. 2012. Receptor-binding profiles of H7 subtype influenza viruses in different host species. J. Virol. 86:4370–4379. 10.1128/JVI.06959-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zaraket H, Bridges OA, Duan S, Baranovich T, Yoon SW, Reed ML, Salomon R, Webby RJ, Webster RG, Russell CJ. 2013. Increased acid stability of the hemagglutinin protein enhances H5N1 influenza virus growth in the upper respiratory tract but is insufficient for transmission in ferrets. J. Virol. 87:9911–9922. 10.1128/JVI.01175-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shelton H, Roberts KL, Molesti E, Temperton N, Barclay WS. 2013. Mutations in haemagglutinin that affect receptor binding and pH stability increase replication of a PR8 influenza virus with H5 HA in the upper respiratory tract of ferrets and may contribute to transmissibility. J. Gen. Virol. 94:1220–1229. 10.1099/vir.0.050526-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Naffakh N, Tomoiu A, Rameix-Welti MA, van der Werf S. 2008. Host restriction of avian influenza viruses at the level of the ribonucleoproteins. Annu. Rev. Microbiol. 62:403–424. 10.1146/annurev.micro.62.081307.162746 [DOI] [PubMed] [Google Scholar]
- 38.Mänz B, Schwemmle M, Brunotte L. 2013. Adaptation of avian influenza A virus polymerase in mammals to overcome the host species barrier. J. Virol. 87:7200–7209. 10.1128/JVI.00980-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brown EG, Liu H, Kit LC, Baird S, Nesrallah M. 2001. Pattern of mutation in the genome of influenza A virus on adaptation to increased virulence in the mouse lung: identification of functional themes. Proc. Natl. Acad. Sci. U. S. A. 98:6883–6888. 10.1073/pnas.111165798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gabriel G, Czudai-Matwich V, Klenk HD. 2013. Adaptive mutations in the H5N1 polymerase complex. Virus Res. 178:53–62. 10.1016/j.virusres.2013.05.010 [DOI] [PubMed] [Google Scholar]
- 41.Gabriel G, Herwig A, Klenk HD. 2008. Interaction of polymerase subunit PB2 and NP with importin alpha1 is a determinant of host range of influenza A virus. PLoS Pathog. 4:e11. 10.1371/journal.ppat.0040011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hudjetz B, Gabriel G. 2012. Human-like PB2 627K influenza virus polymerase activity is regulated by importin-alpha1 and -alpha7. PLoS Pathog. 8:e1002488. 10.1371/journal.ppat.1002488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gabriel G, Klingel K, Otte A, Thiele S, Hudjetz B, Arman-Kalcek G, Sauter M, Shmidt T, Rother F, Baumgarte S, Keiner B, Hartmann E, Bader M, Brownlee GG, Fodor E, Klenk HD. 2011. Differential use of importin-alpha isoforms governs cell tropism and host adaptation of influenza virus. Nat. Commun. 2:156. 10.1038/ncomms1158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Miotto O, Heiny AT, Albrecht R, Garcia-Sastre A, Tan TW, August JT, Brusic V. 2010. Complete-proteome mapping of human influenza A adaptive mutations: implications for human transmissibility of zoonotic strains. PLoS One 5:e9025. 10.1371/journal.pone.0009025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li J, Ishaq M, Prudence M, Xi X, Hu T, Liu Q, Guo D. 2009. Single mutation at the amino acid position 627 of PB2 that leads to increased virulence of an H5N1 avian influenza virus during adaptation in mice can be compensated by multiple mutations at other sites of PB2. Virus Res. 144:123–129. 10.1016/j.virusres.2009.04.008 [DOI] [PubMed] [Google Scholar]
- 46.Chen GW, Chang SC, Mok CK, Lo YL, Kung YN, Huang JH, Shih YH, Wang JY, Chiang C, Chen CJ, Shih SR. 2006. Genomic signatures of human versus avian influenza A viruses. Emerg. Infect. Dis. 12:1353–1360. 10.3201/eid1209.060276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jorba N, Juarez S, Torreira E, Gastaminza P, Zamarreno N, Albar JP, Ortin J. 2008. Analysis of the interaction of influenza virus polymerase complex with human cell factors. Proteomics 8:2077–2088. 10.1002/pmic.200700508 [DOI] [PubMed] [Google Scholar]
- 48.Shapira SD, Gat-Viks I, Shum BO, Dricot A, de Grace MM, Wu L, Gupta PB, Hao T, Silver SJ, Root DE, Hill DE, Regev A, Hacohen N. 2009. A physical and regulatory map of host-influenza interactions reveals pathways in H1N1 infection. Cell 139:1255–1267. 10.1016/j.cell.2009.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tafforeau L, Chantier T, Pradezynski F, Pellet J, Mangeot PE, Vidalain PO, Andre P, Rabourdin-Combe C, Lotteau V. 2011. Generation and comprehensive analysis of an influenza virus polymerase cellular interaction network. J. Virol. 85:13010–13018. 10.1128/JVI.02651-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hurt AC, Deng YM, Ernest J, Caldwell N, Leang L, Iannello P, Komadina N, Shaw R, Smith D, Dwyer DE, Tramontana AR, Lin RT, Freeman K, Kelso A, Barr IG. 2011. Oseltamivir-resistant influenza viruses circulating during the first year of the influenza A(H1N1) 2009 pandemic in the Asia-Pacific region, March 2009 to March 2010. Euro Surveill. 16:19770 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19770 [PubMed] [Google Scholar]
- 51.Lackenby A, Moran Gilad J, Pebody R, Miah S, Calatayud L, Bolotin S, Vipond I, Muir P, Guiver M, McMenamin J, Reynolds A, Moore C, Gunson R, Thompson C, Galiano M, Bermingham A, Ellis J, Zambon M. 2011. Continued emergence and changing epidemiology of oseltamivir-resistant influenza A(H1N1)2009 virus, United Kingdom, winter 2010/11. Euro Surveill. 16:19784 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=19784 [PubMed] [Google Scholar]
- 52.Ujike M, Ejima M, Anraku A, Shimabukuro K, Obuchi M, Kishida N, Hong X, Takashita E, Fujisaki S, Yamashita K, Horikawa H, Kato Y, Oguchi A, Fujita N, Tashiro M, Odagiri T. 2011. Monitoring and characterization of oseltamivir-resistant pandemic (H1N1) 2009 virus, Japan, 2009-2010. Emerg. Infect. Dis. 17:470–479. 10.3201/eid1703.101188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kao RY, Yang D, Lau LS, Tsui WH, Hu L, Dai J, Chan MP, Chan CM, Wang P, Zheng BJ, Sun J, Huang JD, Madar J, Chen G, Chen H, Guan Y, Yuen KY. 2010. Identification of influenza A nucleoprotein as an antiviral target. Nat. Biotechnol. 28:600–605. 10.1038/nbt.1638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cheng H, Wan J, Lin MI, Liu Y, Lu X, Liu J, Xu Y, Chen J, Tu Z, Cheng YS, Ding K. 2012. Design, synthesis, and in vitro biological evaluation of 1H-1,2,3-triazole-4-carboxamide derivatives as new anti-influenza A agents targeting virus nucleoprotein. J. Med. Chem. 55:2144–2153. 10.1021/jm2013503 [DOI] [PubMed] [Google Scholar]
- 55.Gerritz SW, Cianci C, Kim S, Pearce BC, Deminie C, Discotto L, McAuliffe B, Minassian BF, Shi S, Zhu S, Zhai W, Pendri A, Li G, Poss MA, Edavettal S, McDonnell PA, Lewis HA, Maskos K, Mortl M, Kiefersauer R, Steinbacher S, Baldwin ET, Metzler W, Bryson J, Healy MD, Philip T, Zoeckler M, Schartman R, Sinz M, Leyva-Grado VH, Hoffmann HH, Langley DR, Meanwell NA, Krystal M. 2011. Inhibition of influenza virus replication via small molecules that induce the formation of higher-order nucleoprotein oligomers. Proc. Natl. Acad. Sci. U. S. A. 108:15366–15371. 10.1073/pnas.1107906108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Massari S, Nannetti G, Goracci L, Sancineto L, Muratore G, Sabatini S, Manfroni G, Mercorelli B, Cecchetti V, Facchini M, Palu G, Cruciani G, Loregian A, Tabarrini O. 2013. Structural investigation of cycloheptathiophene-3-carboxamide derivatives targeting influenza virus polymerase assembly. J. Med. Chem. 56:10118–10131. 10.1021/jm401560v [DOI] [PubMed] [Google Scholar]
- 57.Tintori C, Laurenzana I, Fallacara AL, Kessler U, Pilger B, Stergiou L, Botta M. 2014. High-throughput docking for the identification of new influenza A virus polymerase inhibitors targeting the PA-PB1 protein-protein interaction. Bioorg. Med. Chem. Lett. 24:280–282. 10.1016/j.bmcl.2013.11.019 [DOI] [PubMed] [Google Scholar]
- 58.Lejal N, Tarus B, Bouguyon E, Chenavas S, Bertho N, Delmas B, Ruigrok RW, Di Primo C, Slama-Schwok A. 2013. Structure-based discovery of the novel antiviral properties of naproxen against the nucleoprotein of influenza A virus. Antimicrob. Agents Chemother. 57:2231–2242. 10.1128/AAC.02335-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Angel M, Kimble JB, Pena L, Wan H, Perez DR. 2013. In vivo selection of H1N2 influenza virus reassortants in the ferret model. J. Virol. 87:3277–3283. 10.1128/JVI.02591-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lakdawala SS, Lamirande EW, Suguitan AL, Jr, Wang W, Santos CP, Vogel L, Matsuoka Y, Lindsley WG, Jin H, Subbarao K. 2011. Eurasian-origin gene segments contribute to the transmissibility, aerosol release, and morphology of the 2009 pandemic H1N1 influenza virus. PLoS Pathog. 7:e1002443. 10.1371/journal.ppat.1002443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Campbell PJ, Danzy S, Kyriakis CS, Deymier MJ, Lowen AC, Steel J. 2014. The M segment of the 2009 pandemic influenza virus confers increased NA activity, filamentous morphology and efficient contact transmissibility to A/Puerto Rico/8/1934-based reassortant viruses. J. Virol. 88:3802–3814. 10.1128/JVI.03607-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bourmakina SV, Garcia-Sastre A. 2003. Reverse genetics studies on the filamentous morphology of influenza A virus. J. Gen. Virol. 84:517–527. 10.1099/vir.0.18803-0 [DOI] [PubMed] [Google Scholar]
- 63.Baudin F, Petit I, Weissenhorn W, Ruigrok RW. 2001. In vitro dissection of the membrane and RNP binding activities of influenza virus M1 protein. Virology 281:102–108. 10.1006/viro.2000.0804 [DOI] [PubMed] [Google Scholar]
- 64.Couch RB, Patel SM, Wade-Bowers CL, Nino D. 2012. A randomized clinical trial of an inactivated avian influenza A (H7N7) vaccine. PLoS One 7:e49704. 10.1371/journal.pone.0049704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Krammer F, Albrecht RA, Tan GS, Margine I, Hai R, Schmolke M, Runstadler J, Andrews SF, Wilson PC, Cox RJ, Treanor JJ, Garcia-Sastre A, Palese P. 2014. Divergent H7 immunogens offer protection from H7N9 challenge. J. Virol. 88:3976–3985. 10.1128/JVI.03095-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Treanor J. 2013, posting date Evaluating the safety and immune response of an H7N7 vaccine in healthy adults. http://www.clinicaltrials.gov/ct2/show/NCT01534468
- 67.Liu D, Shi W, Shi Y, Wang D, Xiao H, Li W, Bi Y, Wu Y, Li X, Yan J, Liu W, Zhao G, Yang W, Wang Y, Ma J, Shu Y, Lei F, Gao GF. 2013. Origin and diversity of novel avian influenza A H7N9 viruses causing human infection: phylogenetic, structural, and coalescent analyses. Lancet 381:1926–1932. 10.1016/S0140-6736(13)60938-1 [DOI] [PubMed] [Google Scholar]
- 68.Perez DR, Sorrell E, Angel M, Ye J, Hickman D, Pena L, Ramirez-Nieto G, Kimble B, Araya Y. 2009. Fitness of pandemic H1N1 and seasonal influenza A viruses during co-infection: evidence of competitive advantage of pandemic H1N1 influenza versus seasonal influenza. PLoS Curr. 1:RRN1011. 10.1371/currents.RRN1011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yang H, Chen LM, Carney PJ, Donis RO, Stevens J. 2010. Structures of receptor complexes of a North American H7N2 influenza hemagglutinin with a loop deletion in the receptor binding site. PLoS Pathog. 6:e1001081. 10.1371/journal.ppat.1001081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hale BG, Randall RE, Ortin J, Jackson D. 2008. The multifunctional NS1 protein of influenza A viruses. J. Gen. Virol. 89:2359–2376. 10.1099/vir.0.2008/004606-0 [DOI] [PubMed] [Google Scholar]