Abstract
Summary
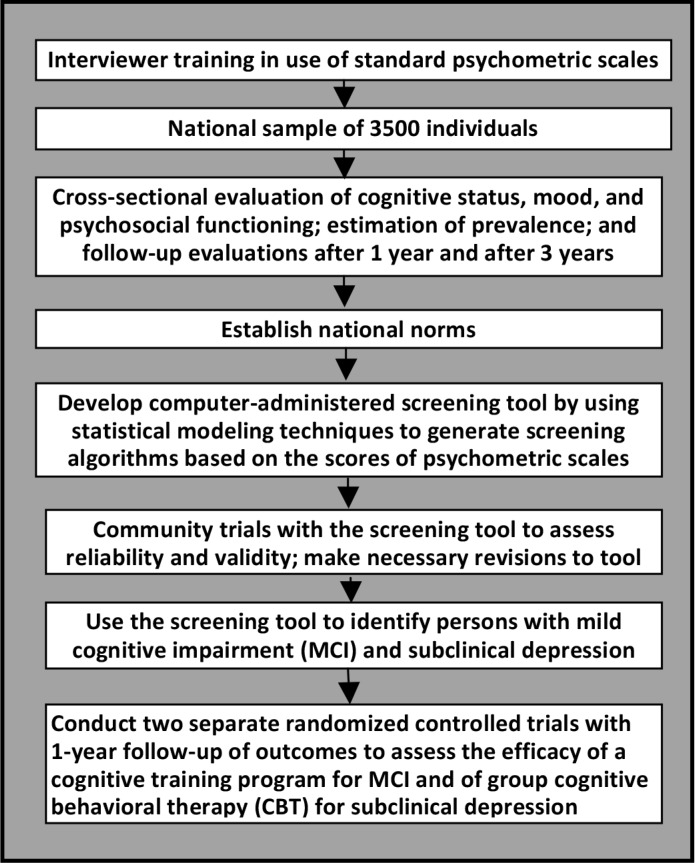
Cognitive and depressive disorders are common in elderly Chinese and are becoming an increasingly important public health problem, partly because of the rapid aging of the population. To help address this issue China's national government has funded a major study to establish national standards for the early identification, evaluation and treatment of common psychological disorders in the elderly. The present paper describes the overall methodology of this study. Fifteen centers in eight provinces will recruit representative samples of subjects aged 60 and over, collect a detailed history, conduct a physical and neurological examination, administer a comprehensive battery of psychological tests, and carry out a diagnostic exam using the Structured Clinical Interview for DSM-IV (SCID). These subjects will participate in follow-up evaluations one year and three years after the initial evaluation. Subsamples of subjects with mild cognitive impairment (MCI) and subclinical depression will be enrolled in randomized controlled trials of a cognitive training program (for MCI) or group cognitive behavioral therapy (for subclinical depression). The results of the study will be used to estimate the prevalence of cognitive and affective disorders in the elderly, to develop a standard screening procedure for these conditions that can be promulgated nationally, and to promote the use of specific interventions that can prevent the development of dementia in persons with MCI and the development of depressive episodes in elderly individuals with subclinical depression.
Abstract
认知和抑郁障是中国老年人常见的心理障碍,已成为严重的公共卫生问题,主要原因是快速的老龄化。为解决这一问题,中国政府资助了一项重大研究,以建立老年人常见心理障碍的早期识别、评估和非药物治疗标准。本文介绍了此研究的总体方法学。来自于8个省市的15个研究中心将从60岁以上老年人群中招募有代表性的研究样本,收集详细的病史资料,完成躯体和神经系统检查,进行全套神经心理测验和临床评定量表评估,采用DSM-IV定式临床访谈作出诊断。初始评估结束后第1年和第3年,将对研究对象进行随访评估。轻度认知损害(mild cognitive impairment, MCI)和亚临床抑郁者会被纳入随机对照研究,接受认知训练(MCI者)或团体认知行为治疗(亚临床抑郁者)。研究结果将用于估计老年人的认知和情感障碍的患病率,制定标准的筛查程序在全国推广应用,并促进采用针对性的干预措施来预防MCI发展为痴呆及老年亚临床抑郁进展为抑郁症。
1. Background
Improvement in the health status of China's population has led to substantial increases in life expectancy. The resultant rapid aging of China's population will inevitably lead to an increased prevalence of Alzheimer's disease,[1] which occurs in 3 to 5% of persons 60 years of age and above, and in 20% of those 80 years of age and above.[2],[3] A meta-analysis summarizing studies of dementia conducted in China between 1980 and 2010 found that the prevalence of dementia was 3% among people who were at least 60 years of age and 6% in those who were at least 65 years of age, somewhat lower than the prevalence reported in high-income countries.[4] Estimated conservatively, there are six million individuals currently living with dementia in China and this number is projected to reach 10 million by 2050. Dementia is already one of the most important causes of disability and death among China's elderly.
Geriatric depression is another important cause of morbidity and mortality in the elderly. Studies from China and elsewhere report that 12.5 to 14.8% of elderly have symptoms of depression and 3.9% meet criteria of a major depressive disorder.[5],[6] Estimated conservatively, there are seven million individuals currently living with geriatric depression in China.[7] Moreover, suicide risk is considerably higher among elderly individuals with depression than among younger persons with depression. In China the estimated suicide rate in the elderly (47/100 000) is twice that in the general population (22/100 000), making China one of the countries with very high suicide rates in the elderly.[8],[9]
Mild cognitive impairment (MCI) and subclinical depression are prodromal conditions of clinical dementia and geriatric depression. The early detection of these prodromal conditions is one of the most important steps in the prevention and treatment of geriatric dementia and depression but there has been relatively little research about these conditions in China and there are, as yet, no national norms that clinicians can use to identify and treat preclinical cases. Screening procedures for other types of psychological problems in the elderly (including other types of dementia, anxiety disorders, and so forth) are also lacking.
To address this important public health problem China's national government funded a major study to establish the psychological norms that can be used in a national service network for the elderly aimed at the early recognition and treatment of MCI, subclinical depression and other psychological disorders. This report describes the overall methodology used in this national study. Subsequent papers will provide details of the methodology, implementation, quality control, and statistical analysis of the project.
2. Aims of the project
Estimate the prevalence of dementia and other mental disorders in the Chinese elderly.
Establish national norms for measures of cognitive functioning, psychological symptoms, quality of life, social support and subjective hap piness in the Chinese elderly and assess fluctua tions in these parameters over a one-year period.
Develop a screening program for MCI and sub clinical depression that uses a mathematical algorithm which integrates both psychological and biological measures
Implement the screening procedures in a con sultative network including community phy sicians, psychiatrists and clinical psychologists to determine the sensitivity and specificity of the algorithm for identifying prodromal cases of dementia and depression.
Develop standardized, China-specific treatment protocols for the non-pharmacological treatment of MCI (using cognitive training) and subclinical depression (using group cognitive behavior therapy).
Establish a bank of biological samples and norms for brain volumes and other measures obtained from magnetic resonance imaging (MRI) assess ments for elderly individuals in China.
3. Research Methods
Figure 1 provides an overview of the project.
Figure 1. Flowchart of the overall project.
3.1. Cross-sectional survey of common psychological problems among Chinese elderly
This survey was a joint effort of 15 institutions located in the eastern, middle, and western parts of China. Each institution identified one or more target communities; a total of 20 target communities (18 urban and 2 rural) participated in the project. The 15 304 individuals at least 60 years old registered in the 2010 national census as permanent residents of these communities were entered into a database and a simple random sample of 4411 of them were selected as potential participants in the survey. Among those selected, 3514 (80%) completed the baseline survey. The 897 non-responders included 99 who were not located, 712 who refused to participate, 26 who did not come for the appointment, 53 who only completed part of the survey, and 7 with a serious medical condition that made participation impossible.
The survey was conducted in local community centers for the elderly or, if this was inconvenient for the respondent, in the respondent's home. Data collected included general demographic information (including name, sex, date of birth, home address, zip code, home phone number, ethnicity, years of education, current occupation, occupation before retirement [if retired], and permanent residence) and information about daily living (including hobbies, dietary preferences, sleeping pattern, and histories of smoking, consumption of alcohol and tea, and physical activities). Several psychological and psychosocial measures were assessed by a psychologist: the Mini-Mental State Examination (MMSE),[10] the Montreal Cognitive Assessment (MoCA),[11] the Neuropsychological Test Battery (NTB),[12] the Self-rating Anxiety Scale (SAS),[13] the Geriatric Depression Scale (GDS),[14] the Life Event Scale (LES),[15] and the Social Support Rating Scale (SSRS). [16] Attending-level psychiatrists collected information on the current and past history of diseases, conducted physical examinations, evaluated functioning and determined the diagnosis using the Neuropsychiatric Inventory (NPI),[17] the Activities of Daily Living scale (ADL),[18] the Clinical Dementia Rating scale (CDR),[19] the Global Deterioration Scale (GDS),[20] the Clinical Global Impression scale (CGI), [21] the Hachinski Ischemia Scale (HIS)[22] and the depression and anxiety disorder sections of the Structured Clinical Interview for DSM (SCID).[23]
Two diagnostic methods were used in the study. Clinical assessments classified subjects as follows: no diagnosis, amnestic mild cognitive impairment (AMCI), vascular mild cognitive impairment (VMCI), Alzhiemer's Disease, vascular dementia, mixed dementia, depressive disorder, normal aging, and successful aging. The other diagnostic classification based on the results of the SCID included the following categories: no diagnosis, current major depressive episode, subclinical depression, current and past history of manic episode, primary or secondary depressive disorder, dysthymia, subclinical dysthymia, panic attack, generalized anxiety disorder, pain disorder, hypochondria, and primary insomnia. (Two of these diagnoses are not included in DSM-IV. The criteria for ‘subclinical depression’ were as follows: two or more simultaneous symptoms of depression, present most or all of the time for at least 2 weeks that are associated with social dysfunction in individuals who do not meet criteria for minor depression, major depression or dysthymia. The criteria for ‘subclinical dysthymia’ were as follows: one or two simultaneous symptoms of dysthymia, present most or all of the time for at least 2 years that are associated with evidence of social dysfunction in individuals who do not meet criteria minor depression, major depression, or dysthymia.) If there is a conflict between the clinical diagnosis and the SCID-based diagnosis the clinical diagnosis is given precedence. These results will be used to estimate the prevalence of common cognitive and psychological problems in the Chinese elderly population.
The 3514 individuals who completed the baseline evaluation will be re-evaluated using the same procedures one year and three years after initial entry into the project.
3.2. Establish national norms for common psycho logical measures in the elderly and develop an early detection screening program for elderly individuals using these norms
Based on the baseline and follow-up surveys described above, we will establish national norms for elderly Chinese of common psychological measures of memory, cognition, mood, quality of life, social support and subjective happiness (including MMSE, MoCA, NTB, SAS, GDS, LES, SSRS, NPI, ADL, CDR, GDS, etc.). Using this data, mathematical modeling methods will be used to identify sensitive, age-specific indices that can be integrated into a screening battery for common mental health problems in the elderly, particularly dementia and depression. The screening battery–to be administered by psychiatrists, psychologists and primary care physicians–will be pilot tested, revised accordingly and then promulgated nationally. Long-term follow-up studies with the battery will be used to assess the developmental course of different mental health indices in different age cohorts of elderly individuals.
At the demonstration sites psychiatrists, psychologists and primary care physicians will work collaboratively to establish mental health records (to be integrated with the overall medical record) for elderly individuals that include information on cognitive functioning, mood, behavioral functioning, social support, subjective happiness and so forth. Based on this information elderly individuals will be classified into five categories: ‘successful aging’, ‘good mental health’, ‘high risk’, ‘subclinical state’, and ‘mental disorder.’ Pilot projects by our group have already established a large database of elderly subjects that has been employed to identify reliable and valid measures of ‘successful aging.’ Periodical follow-up with the elderly at these demonstration sites will assess the trends in these mental health indices and be used to identify risk factors and protective factors for negative trajectories. Individuals classified as ‘subclinical state’ will be enrolled in prospective cohort trials of a cognitive training intervention (CTI) for MCI or a group cognitive behavioral therapy (CBT) intervention for subclinical depression.
3.3. Assess the effectiveness of cognitive training for MCI and group CBT for subclinical depression in preventing progression to Alzheimer's Disease and Major Depressive Disorder
As stated earlier, dementia and geriatric depression are the two conditions associated with the heaviest disease burden among elderly people so the aim of the current project is to prevent (or delay) the onset of these conditions by intervening with individuals who have subclinical versions of the conditions – MCI and subclinical depression. The use of pharmaceutical treatment in subclinical conditions is debatable but the use of CTI for MCI and group CBT for subclinical depression is well accepted.
Recent studies provide convincing evidence of the effectiveness of CTI in the treatment of dementia and in the treatment of cognitive changes after stroke or brain trauma among elderly people.[24] Ball and colleagues[25] conducted a large randomized controlled trial and found that the CTI improved cognitive functioning among healthy elderly and might prevent the decline of daily functioning that often comes with aging. Comprehensive, multi-component CTIs have been shown to be superiorto single-method approaches to cognitive training both in China and elsewhere.[26],[27] A previous prospective study by our group assessed the mechanisms of successful aging and tested a CTI based on strategies to compensate for brain aging and, thus, maintain executive functioning in persons 71 to 75 years of age.[28]
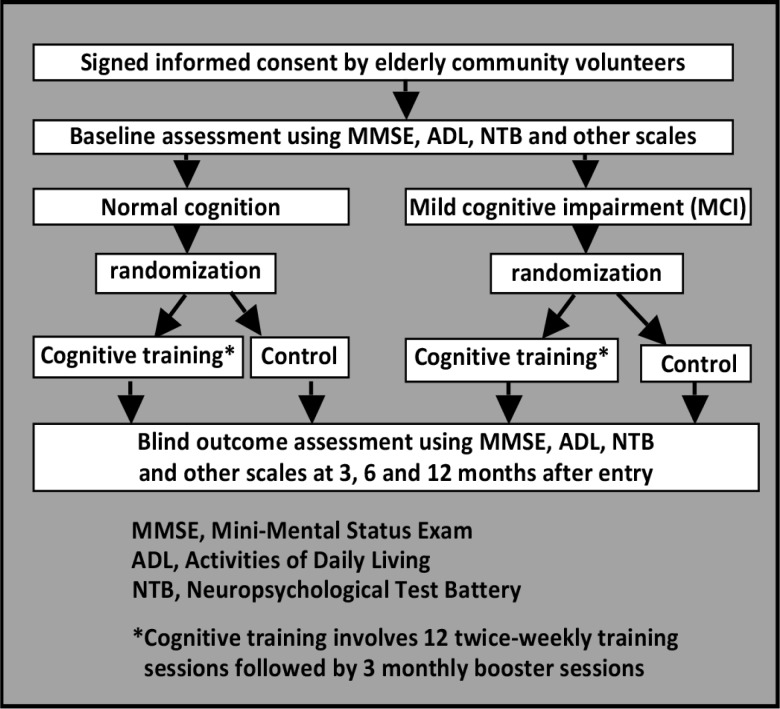
The CTI developed for the current project will be pilot tested and revised in Shanghai and subsequently employed in all 15 sites. The flowchart for the CTI intervention is shown in Figure 2. The sample for this study is independent from that identified in the cross-sectional study described above. Elderly individuals with MCI and those without any cognitive impairment will be separated into separate subsamples (persons with comorbid MCI and mild depression will be excluded). Each subsample will be randomly assigned (using computer algorithms) to the CTI group or to a treatment as usual (control) group. The CTI intervention includes a training phase and a reinforcing phase. The training phase includes three days of training sessions per week for 12 weeks. The reinforcing training–with one one-hour face-to-face session per month – will last for three months. Based on relevant methods reported by Chinese and foreign research groups, our research group developed a training protocol including both face-to-face training and self-training by the study participant. Face-to-face training includes: (a) memory training, (b) logical thinking training, (c)strategictraining, (d) using a map of Shanghai, (e) workshop of computer skills, (f) handcrafting, (g) aerobics, (h) calligraphy and painting, and (i) group discussion. Self-training includes reading material about health, calligraphy, painting and so forth. The participant will practice self-training at home according to their own interests. The participants are encouraged to do physical activities, such as a daily walk lasting 30 min. Process measures include level of participation in the training sessions, satisfaction with training, self-report of completion of homework tasks. Outcome is assessed by raters who are blind to the treatment status of subjects at the completion of the 3-month training phase, at the completion of the 3-month reinforcement phase (i.e., 6 months after initiation of treatment), and 6 months after completion of treatment (i.e., 12 months after initiation of treatment). The measures assessed at these times include MMSE, NTB,ADL, and other measures that assess clinical characteristics, social functioning, psychological status, quality of life, and self-efficacy.
Figure 2. Flowchart of the cognitive training intervention (CTI).
Many studies have demonstrated the effectiveness of individual CBT for depressed elderly.[29] A web-based randomized control trial of CBT for subclinical geriatric depression by Spek and colleagues[30] proved that this method can be effective. But community-based individual CBT or web-based interventions may not be practical in China. In urban China elderly individuals are relatively concentrated in communities and are willing to participate in group activities so group CBT may be a more appropriate approach.
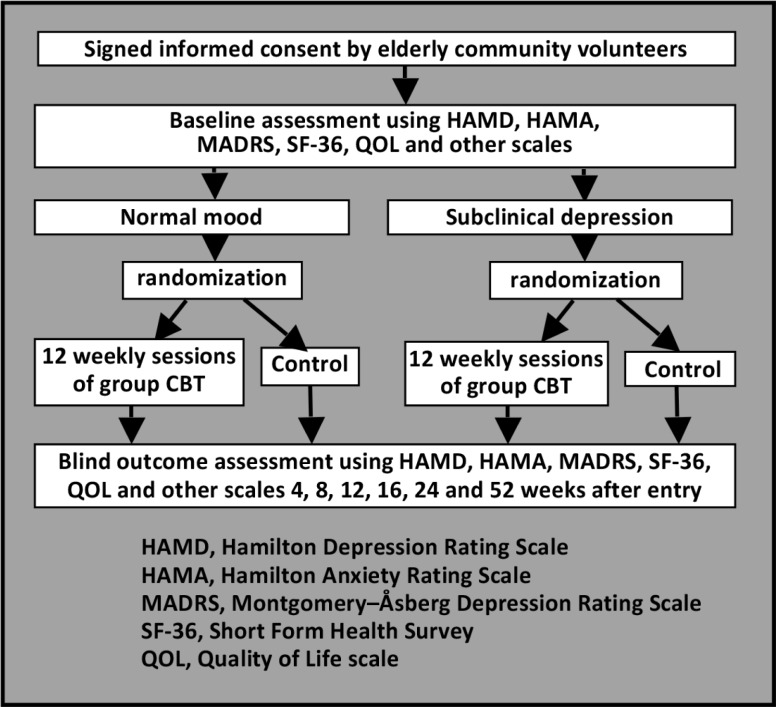
The group CBT employed in this project – which will first be pilot tested in Shanghai and then employed in all 15 sites – will be an adaptation of the method described in the Group Therapy Manual for Cognitive-Behavioral Treatment Depression (GCBT) by Ricardo F. Muñoz and Jeanne Miranda.[31] The flowchart for the group CBT intervention is shown in Figure 3. The sample for this study is independent from that identified in the cross-sectional study described above. Screened elderly will first be subdivided into two subsamples, those without depression and those with subclinical depression (those with comorbid depression and MCI will be excluded). Each subsample will be randomly assigned (using computer algorithms) to the GCBT group or a treatment as usual (control) group. GCBT involves 12 weekly sessions divided into three four-session components. Enrollment in the study will be continued for one year or until 30 subjects have completed the treatment; a minimum of 4 subjects will be in the group at a time and new members can join the group at the beginning of the second and third components. There will be a homework assignment after each session and the homework will be checked at the beginning of the next session. The clinical status and quality of life of participants will be assessed using the 17-item Hamilton Depression Rating Scale (HAMD),[32] the Hamilton Anxiety Rating Scale (HAMA),[33] the Montgomery–Åsberg Depression Rating Scale (MADRS)[34] the Short Form Health Survey (SF-36) [35] and the Quality of Life scale for use in dementia (QOL-AD)[36] at entry and 4, 8, 12, 16, 24 and 52 weeks after entry into the study.
Figure 3. Flowchart of the group cognitive behavioral therapy (CBT) intervention.
3.4. Establishing a database of geriatric biosamples
Blood samples (5ml) were collected from all participants recruited for the community-based cross-sectional survey in Shanghai and at a few of the other sites. This blood draw will be repeated at one-year and three-year follow-up visits. A regular blood panel was conducted to measure white blood cells, neutrophil granulocytes, red blood cells, hemoglobin, mean cell volume and platelets. Biochemical tests assessed total proteins, alanine transaminase, aspartate transaminase, bilirubin, potassium, sodium, chloride, blood urea nitrogen, creatinine, glucose, triglyceride, cholesterol, high density lipoprotein, low density lipoprotein, apolipoprotein A, apolipoprotein B, and lipoprotein. Separated plasma and serum (200ul each) were stored in -70°C freezers.
Participants recruited in Shanghai are eligible for 3D-MRI brain scans. Consenting participants will be scanned at the end of the first year of the study using a MRI machine with a 3-tesla field strength. All MRI data will be saved in the DICOM format. This MRI data will be used to explore the structural brain changes during aging, and to obtain reference values for normal aging brains in elderly Han individuals.
Biography

Professor Shifu Xiao graduated from the Shanghai No. 2 Medical University and is currently working as the director of the Alzheimer's Disease and Related Disorders Center and of the Department of Geriatric Psychiatry at the Shanghai Mental Health Center in the Shanghai Jiao Tong University. He has been a visiting professor at the University of Melbourne and the University of New South Wales and done short-term fellowships at several international centers. Professor Xiao has held leadership positions in several professional organizations, been responsible for several national and local projects related the mental health and well-being of older citizens, and received several awards for his contributions. His research interests are dementia and MCI.
Footnotes
Conflict of interest: The authors report no conflict of interest related to this project.
Funding: The Ministry of Science and Technology, National Pillar Program 2009BAI77B03; National Key Clinical Disciplines at Shanghai Mental Health Center (Office of Medical Affairs, Ministry of Health, 2011-873; OMA-MH, 2011-873)
References
- 1.Flaherty JH, Liu ML, Ding L, Dong B, Ding Q, Li X, et al. China: the aging giant. J Am Geriatr Soc. 2007;55(8):1295–1300. doi: 10.1111/j.1532-5415.2007.01273.x. [DOI] [PubMed] [Google Scholar]
- 2.Zhang MY, Katzman R, Salmon D, Jin H, Cai GJ, Wang ZY, et al. The prevalence of dementia and Alzheimer's disease in Shanghai, China: Impact of age, gender, and education. Ann Neurol. 1990;27(4):428–437. doi: 10.1002/ana.410270412. [DOI] [PubMed] [Google Scholar]
- 3.Zhang ZX, Zahner GE, Roman GC, Liu J, Hong X, Qu QM, et al. Studies on the prevalence of subtype of dementia in Beijing, Xi'an, Shanghai and Chengdu. Chinese Journal of Contemporary Neurology and Neurosurgery. 2005;5(3):156–157. (in Chinese) [Google Scholar]
- 4.Zhang Y, Xu Y, Nie H, Lei T, Wu Y, Zhang L, et al. Prevalence of dementia and major dementia subtypes in the Chinese populations: A meta-analysis of dementia prevalence surveys, 1980-2010. J Clin Neurosci. 2012;19(10):1333–1337. doi: 10.1016/j.jocn.2012.01.029. [DOI] [PubMed] [Google Scholar]
- 5.Chen R, Copeland JRM, Wei L. A metaanalysis of epidemiological studies in depression of older people in the People's Republic of China. Int J Geriatr Psychiatry. 1999;14(10):821–830. doi: 10.1002/(sici)1099-1166(199910)14:10<821::aid-gps21>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 6.Chi I, Yip PS, Chiu HF, Chou KL, Chan KS, Kwan CW, et al. Prevalence of depression and its correlates in Hong Kong's Chinese older adults. Am J Geriatr Psychiatry. 2005;13(5):409–416. doi: 10.1176/appi.ajgp.13.5.409. [DOI] [PubMed] [Google Scholar]
- 7.Chen CH. Epidemiology of elderly depression. Practical Geriatrics. 2001;15(1):3–6. (in Chinese) [Google Scholar]
- 8.Li X, Xiao Z, Xiao S. Suicide among the elderly in mainland China. Psychogeriatrics. 2009;9(2):62–66. doi: 10.1111/j.1479-8301.2009.00269.x. [DOI] [PubMed] [Google Scholar]
- 9.Phillips MR, Li X, Zhang Y. Suicide rates in China,1995-99. Lancet. 2002;359(9309):835–840. doi: 10.1016/S0140-6736(02)07954-0. [DOI] [PubMed] [Google Scholar]
- 10.Folstein MF, Folstein SE, McHugh PR. Mini Mental State Examination: A practical method for grating the cognitive state of patients for the clinician. J Psychiat Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 11.Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 12.Gilman S, Koller M, Black RS, Jenkins L, Griffith SG, Fox NC, et al. Clinical effects of Abeta immunization (AN 1792) in patients with AD in an interrupted trial. Neurology. 2005;64(9):1553–1562. doi: 10.1212/01.WNL.0000159740.16984.3C. [DOI] [PubMed] [Google Scholar]
- 13.Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 14.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982-1983;17(1):37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 15.Yang DS, Zhang YL. Life event Scale. In: Yang DS, editor. Behavior Medicine. Changsha: Hunan Normal University Press; 1990. p. p. 285. (in Chinese) [Google Scholar]
- 16.Xiao SY, Yang DS. Role of social support in well-being. Chinese Mental Health Journal. 1987;1:184–187. (in Chinese) [Google Scholar]
- 17.Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J. The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology. 1994;44(12):2308–2314. doi: 10.1212/wnl.44.12.2308. [DOI] [PubMed] [Google Scholar]
- 18.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- 19.Morris JC. The Clinical Dementia Rating (CDR):Current version and scoring rules. Neurology. 1993;43:2412–2414. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- 20.Reisberg B, Ferris SH, de Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139(9):1136–1139. doi: 10.1176/ajp.139.9.1136. [DOI] [PubMed] [Google Scholar]
- 21.Guy W, editor. ECDEU Assessment Manual for Psychopharmacology (revised) Rockville, MD: National Institute of Mental Health; 1976. [Google Scholar]
- 22.Hachinski VC, Iliff LD, Zilhka E, Du Boulay GH, McAllister VL, Marshall J, et al. Cerebral blood flood flow in dementia. Arch Neurol. 1975;32(9):632–637. doi: 10.1001/archneur.1975.00490510088009. [DOI] [PubMed] [Google Scholar]
- 23.Steinberg M. Interviewers Guide to the Structured Clinical Interview for DSM-IV Dissociative Disorders (SCID-D) Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- 24.Landreville P, Landry J, Baillargeon L, Guerette A, Matteau E. Older adults acceptance of psychological and pharmacological treatments for depression. J Gerontol B Psychol Sci Soc Sci. 2001;56(5):P285–291. doi: 10.1093/geronb/56.5.p285. [DOI] [PubMed] [Google Scholar]
- 25.Ball K, Berch DB, Helmers KF, Jobe JB, Leveck MD, Marsiske M, et al. Effects of cognitive training intervention with older adults: A randomized controlled trial. JAMA. 2002;288(18):2271–2281. doi: 10.1001/jama.288.18.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oswald WD, Gunzelmann T, Rupprecht R, Hagen B. Differential effects of single versus combined cognitive and physical training with older adults: the SIMA study in a 5-year perspective. Eur J Ageing. 2006;3:179–192. doi: 10.1007/s10433-006-0035-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Acevedo A, Loewenstein DA. Nonpharmacological cognitive interventions in aging and dementia. J Geriatr Psychiatry Neurolo. 2007;20(4):239–249. doi: 10.1177/0891988707308808. [DOI] [PubMed] [Google Scholar]
- 28.Li C, Wu W, Jin H, Zhang X, Xue H, He Y, et al. Successful aging in Shanghai, China: definition, distribution and related factors. Int Psychogeriatr. 2006;18(3):551–563. doi: 10.1017/S1041610205002966. [DOI] [PubMed] [Google Scholar]
- 29.Serfaty MA, Haworth D, Blanchard M, et al. Clinical effectiveness of individual cognitive behavioral therapy gor depressed older people in primary care:randomized controlled trial[J].Arch Gen Psychiatry. 2009;66(12):1332–1340. doi: 10.1001/archgenpsychiatry.2009.165. [DOI] [PubMed] [Google Scholar]
- 30.Spek V, Nyklícek I, Smits N, Cuijpers P, Riper H, Keyzer J, et al. Internet-based cognitive behavioural therapy for subthreshold depression in people over 50 years old: a randomized controlled clinical trial. Psychol Med. 2007;37(12):1797–1806. doi: 10.1017/S0033291707000542. [DOI] [PubMed] [Google Scholar]
- 31.Muñoz RF, Miranda J. Group Therapy Manual for Cognitive-Behavioral Treatment of Depression. Santa Monica, CA: RAND; 2000. [Google Scholar]
- 32.Hamilton M. A Rating Scale for Depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hamilton M. The assessment of anxiety by rating scale. Br J Med Psychol. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 34.Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 35.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 36.Hoe J, Katona C, Roch B, Livingston G. Use of the QOL-AD for measuring quality of life in people with severe dementia-the LASER-AD study. Age Ageing. 2005;34(2):130–135. doi: 10.1093/ageing/afi030. [DOI] [PubMed] [Google Scholar]