Abstract
Mild encephalitis/encephalopathy with a reversible splenial lesion (MERS) is a clinicoradiological entity with varied aetiologies and having a typical course of evolution. We present a case of MERS evaluated with diffusion-weighted and diffusion tensor imaging along with various conventional sequences of MRI. At the time of presentation, the lesions in the splenium of corpus callosum and bilateral cerebral white matter showed diffusion restriction with reduced apparent diffusion coefficient and no reduction in fractional anisotropy (FA) values on diffusion tensor imaging; on follow-up diffusion restriction completely resolved with normalisation of the apparent diffusion coefficient. The normal to slightly increased FA values in the lesions may indicate that MERS is a non-degenerative disorder.
Background
A reversible splenial lesion is an uncommon entity which is seen in a number of clinical conditions with varied aetiologies. Initially it was described in patients with epilepsy and therefore thought to be associated with seizure or its therapy. Mild encephalitis/encephalopathy with a reversible splenial lesion (MERS) is an uncommon entity; awareness of its imaging features allows us to differentiate it from other common infective and non-infective aetiologies. Diffusion tensor imaging (DTI) and fractional anisotropy (FA) values are potential tools to differentiate the early and late phases of MERS from other non-reversible ischaemic and non-ischaemic causes.
Case presentation
A 28-year-old female patient presented with fever and vomiting for the past 1 week and altered sensorium since 72 h. On examination, fever was of high grade with chills. Central nervous system examination showed that the patient was drowsy with neck rigidity and up going plantar reflex. The Glasgow Coma Scale was 6 at the time of admission.
Investigations
The cerebrospinal fluid (CSF) analysis showed lymphocytosis (white cell count 60 cells/mm3, lymphocytes 89%, neutrophils 9%), acid-fast bacilli negative and cryptococcosis negative. CSF virology for herpes simplex virus (HSV)-1/2; enterovirus, mumps, varicella zoster and Japanese encephalitis were negative. Blood culture and serology for dengue were negative.
Electroencephalography showed slow activity, non-specific left>right frontal sharp wave suggestive of encephalopathy.
MRI was performed on Philips Acheiva 1.5 T MRI scanner. The routine MR sequences included T2-weighted images (T2WI), fluid attenuated inversion recovery (FLAIR), T1WI, postcontrast fat saturated T1WI, diffusion-weighted images (DWI) and apparent diffusion coefficient (ADC) maps.
A Reg DTI-high isoSENSE sequence was used for DTI (echo planar imaging (EPI), DWI spin echo (SE), repetition time: 13 513 ms; excitation time: 106 ms), with measurement of 33 diffusion directions (including one on B0). Sensitivity-encoded reconstruction was used to reduce the length of the EPI-train, hence minimising susceptibility-related distortions. A field of view (FOV) of 224 mm. Number of b-values: 2, with a maximum b-factor of 800 mm2/s and an ascending b-factor order. Voxel-size: 2.0×2.0×2.0 mm. A total of 70 slices of 2 mm thickness with no interslice gaps were obtained with a scan duration of 15 min.
The DTI data were analysed using the FibreTrak software (version R2.6.3.1). Quantitative values of FA and ADC were measured by manually placing regions of interest (ROIs) onto DWIs. Freehand ROIs were placed in the splenium of corpus callosum such that they encompassed as much of the lesion as possible on DWIs, and care was taken to avoid grey matter and CSF. Single-point ROIs were placed bilaterally in the posterior limb of the internal capsule, centrum semiovale and white matter of frontal lobes. On follow-up imaging the ROIs were placed similarly in the same location as the initial scan.
MRI with DWI and DTI at admission revealed
Areas of high signal intensity on DWI with low ADC symmetrically involving centrum semiovale, corona radiata, posterior limbs of internal capsule, anterior commissure and the splenium of corpus callosum (figure 1). On T2WI and FLAIR image subtle hyperintensities were noted in the splenium of corpus callosum and bilateral centrum semiovale (figure 2A–D), on T1WI (figure 2E, F) and postcontrast T1WI (figure 2G, F) images no significant signal intensity changes or enhancements were noted in the areas of diffusion restriction. The FA values were normal to increased and the ADC values were reduced at these locations when compared to those of the normal-appearing white matter (figure 3 and table 1).
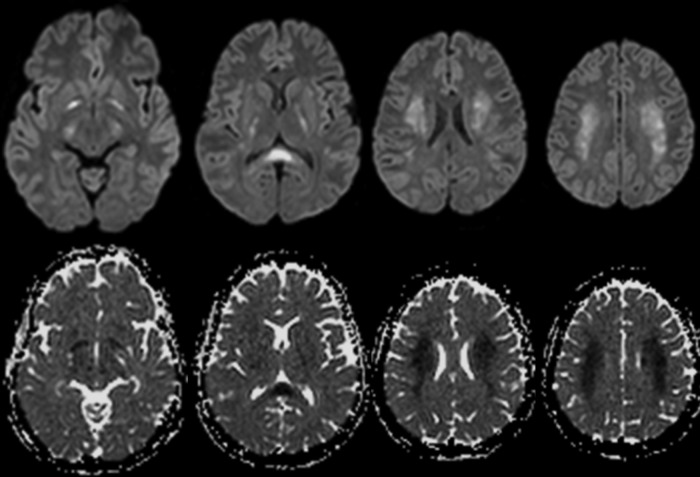
Figure 1.
At admission: serial axial diffusion-weighted images and their corresponding apparent diffusion coefficient maps showing restricted diffusion involving centrum semiovale, corona radiata, posterior limbs of internal capsule, anterior commissure and the splenium of corpus callosum.
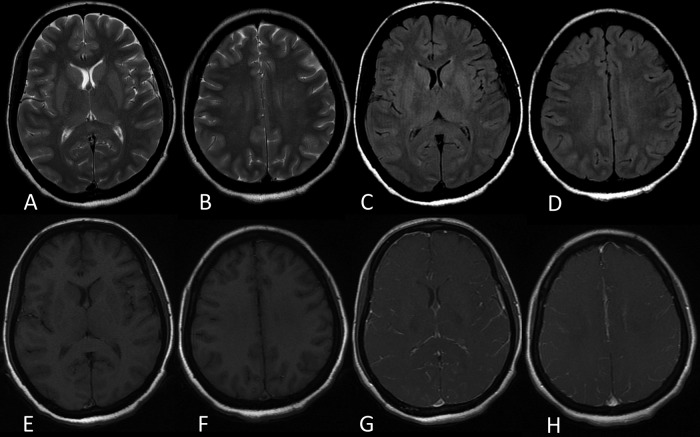
Figure 2.
At admission: axial T2-weighted image (WI) (A and B) and fluid attenuated inversion recovery image (C and D) showing subtle hyperintensities involving the splenium of corpus callosum and bilateral centrum semiovale. Axial T1WI (E and F) showing no abnormal areas of altered signal intensities. Postcontrast T1W fat saturated images showing no abnormal enhancement in areas of diffusion restriction.
Figure 3.
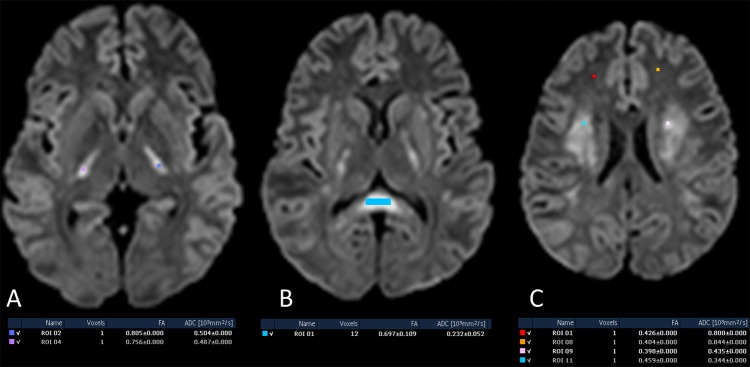
At admission: axial diffusion-weighted images with estimation of fractional anisotropy (FA) values; at splenium of corpus callosum (A), posterior limbs of internal capsule (B) and centrum semiovale (C) showing normal or mildly increased FA values with reduced apparent diffusion coefficient (ADC) values as compared to normal-appearing white matter in bilateral frontal lobes (C).
Table 1.
Summary of FA and ADC values
| Normal-appearing white matter | Splenium of corpus callosum | Posterior limb of internal capsule | Centrum semiovale | |
|---|---|---|---|---|
| At admission | ||||
| FA | 0.426 | 0.697 | 0.756 | 0.459 |
| ADC (10−3 mm2/s) | 0.800 | 0.232 | 0.487 | 0.344 |
| 15th day | ||||
| FA | 0.373 | 0.722 | 0.829 | 0.480 |
| ADC (10−3 mm2/s) | 0.867 | 0.760 | 0.664 | 0.752 |
ADC, apparent diffusion coefficient; FA, fractional anisotropy.
Follow-up MRI on 15th day
MRI showed complete resolution of areas of restricted diffusion (figure 4) and subtle T2WI and FLAIR hyperintensities (figure 5). The FA and ADC values were comparable to those of the normal-appearing white matter (figure 6 and table 1).
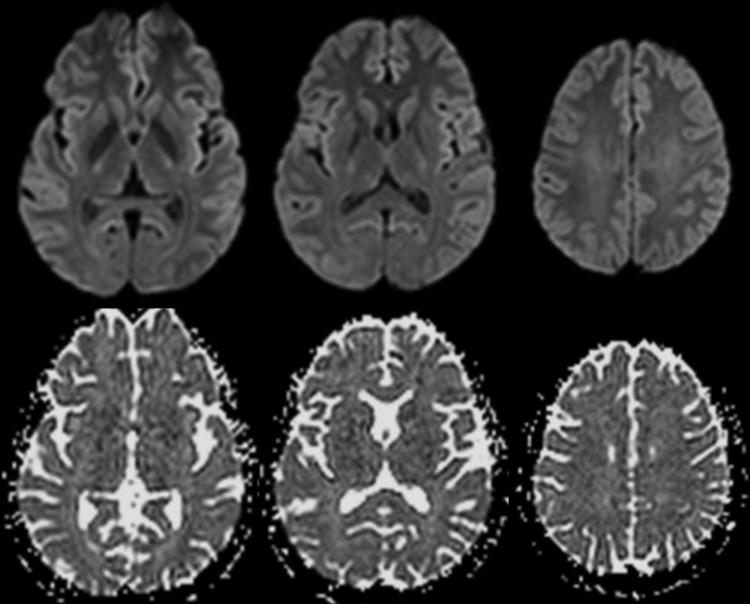
Figure 4.
Fifteenth day after admission: serial axial diffusion-weighted images and their corresponding apparent diffusion coefficient maps showing complete resolution of areas of diffusion restriction.
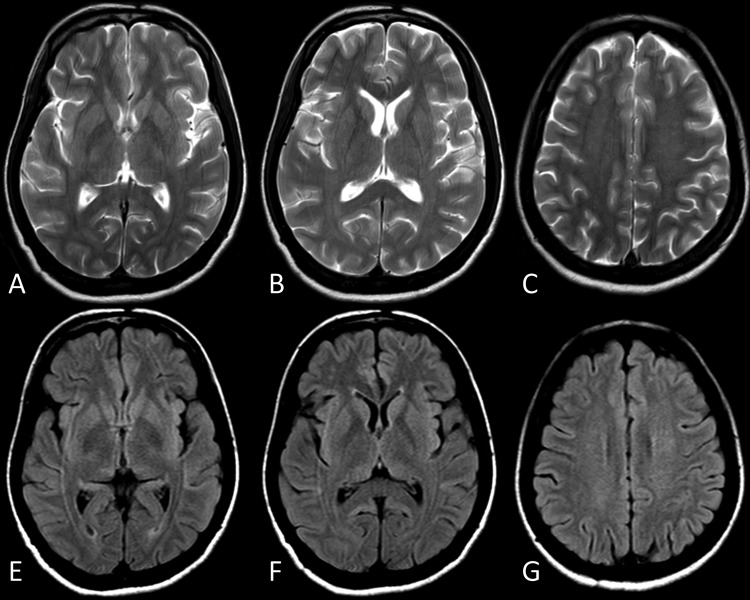
Figure 5.
Fifteenth day after admission: serial axial T2-weighted (A–C) and fluid attenuated inversion recovery (E–G) images showing complete resolution of the subtle hyperintensities.
Figure 6.
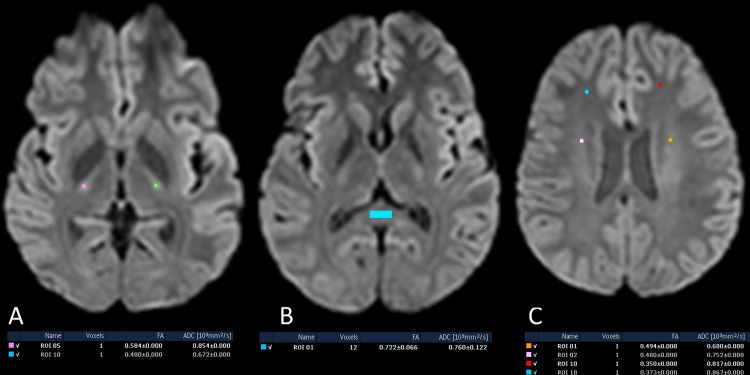
Fifteenth day after admission showing normal fractional anisotropy (FA) and apparent diffusion coefficient (ADC) values.
Differential diagnosis
Acute disseminated encephalomyelitis was excluded radiologically because it presents as asymmetrical white matter lesions which persist for months on MRI beyond the clinical resolution of the disease.
Treatment
In view of CSF findings supportive of viral aetiology, the patient was empirically put on corticosteroids and acyclovir which was stopped after negative CSF virology for HSV.
Outcome and follow-up
The patient made a complete clinical recovery with no residual neurological deficit in 15 days. Follow-up MRI at 15 days showed complete resolution of diffusion restriction, normalisation of ADC values and no significant change in FA values.
Discussion
MERS was initially described as a clinicoradiological entity, with a mild clinical course and complete recovery of isolated lesions affecting the splenium of corpus callosum, excluding lesions affecting the parenchyma.1
Although commonly seen in paediatric age group, cases of MERS have been reported in adult populations. Tada et al1 reported 15 cases of MERS in patients between the ages of 2–59, of which 5 cases were above the age of 19.1
Currently the spectrum of MERS has been widened to include symmetrical lesions affecting the white matter of frontal and parietal lobes.2
We present a case of MERS with symmetrical involvement of deep white matter of frontal and parietal lobes with signal intensity characteristics and reversibility mirroring the transient splenial lesion. Near-normal FA values during the course of the disease indicates a non-degenerative process.3
The diffusion restriction with normal FA values may be explained by intramyelenic or interstitial oedema.3
Learning points.
Reversible symmetrical white matter lesions in addition to reversible corpus callosal lesion can be a part of spectrum of mild encephalitis/encephalopathy with a reversible splenial lesion (MERS).
MERS presents as a typical clinical course with complete radiological resolution in 10–15 days.
Normal or mildly increased fractional anisotropy values in areas of diffusion restriction may indicate the preservation of white matter architecture.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Tada H, Takanashi J, Barkovich AJ, et al. Clinically mild encephalitis/encephalopathy with a reversible splenial lesion. Neurology 2004;63:1854–8 [DOI] [PubMed] [Google Scholar]
- 2.Takanashi J, Barkovich AJ, Shiihara T, et al. Widening spectrum of a reversible splenial lesion with transiently reduced diffusion. AJNR Am J Neuroradiol 2006;27:836–8 [PMC free article] [PubMed] [Google Scholar]
- 3.Osuka S, Imai H, Ishikawa E, et al. Mild encephalitis/encephalopathy with a reversible splenial lesion: evaluation by diffusion tensor imaging. Three case reports. Neurol Med Chir (Tokyo) 2010;50:1118–22 [DOI] [PubMed] [Google Scholar]