Abstract
Those who have experienced abuse may be prone to engaging in risky sexual behavior and risky drug use. The relationship between sexual abuse and risky behavior has been well established in the literature, but the association between physical abuse and risky drug use has been equivocal. We hypothesize that the experience of PTSD symptoms following physical abuse leads to risky drug use. Therefore, we examined the associations among physical abuse history, PTSD symptoms, and HIV-related drug risk in a sample of 121 opioid-dependent persons to determine whether PTSD symptoms mediated the relationship between physical abuse history and drug risk. Participants were recruited during an acute care hospital inpatient stay. Physical abuse history was associated with increased drug risk, and PTSD symptoms were associated with increased drug risk. However, PTSD symptoms were not found to be a mediator of the association between physical abuse history and HIV-related drug risk. These findings highlight the importance of assessing abuse history in high-risk samples of opioid users.
Keywords: physical abuse, HIV, risky drug use, opiate dependence, PTSD
1.1 Introduction
The experience of physical and sexual abuse can lead to a variety of adverse health outcomes including increased risk for HIV (Cohen et al., 2000). Those exposed to abuse may be more prone to engage in risky sexual contact or risky drug use, the primary routes for HIV transmission in the United States (CDC, 2007). Understanding the development of risky behaviors that leads to HIV transmission can help produce targeted prevention interventions.
While the association of sexual abuse and increased risky sexual behavior has been established in a variety of populations (Chuang, Liebschutz, Horton, & Samet, 2006), the association between physical abuse and risky drug use has not been as well established, particularly within an opioid dependent population. Risky drug use includes such behaviors as injection drug use and the sharing of needles and drug paraphernalia without sterilization.
Kang and colleagues found that men and women with a history of physical abuse are more likely to use heroin than those not reporting such abuse, but did not find differences between the groups in terms of risky drug use (Kang et al., 2000). Also, in a sample of drug injecting women, physical abuse was not found to be associated with increased drug risk (Plotzker, Metzger, & Holmes, 2007). In contrast, Bensley and colleagues found that men with a history of physical abuse report up to a 3-fold increase in HIV-risk behaviors, including injection drug use, compared to those with no abuse history (Bensley, Eenwyk, & Simmons, 2000). We hypothesize these equivocal findings may be due to the variety of drugs being abused in the populations of interest and variability of the assessment of physical abuse. The unexplored mechanism by which physical abuse might lead to risky drug use remains unknown.
Chilcoat and Breslau tested the causal pathways between traumatic events, posttraumatic stress disorder (PTSD), and drug use disorders in a longitudinal sample of adults (1998). They found that exposure to traumatic events alone was not sufficient to increase the risk for drug use disorders in the absence of PTSD. They posited that symptoms of PTSD lead one to engage in drug use in order to ameliorate negative feelings after the experience of traumatic events (1998). Given that persons with substance use disorders report elevated rates of exposure to traumatic events such as abuse (Sansone, Whitecar, & Wiederman, 2009), they are at high conditional risk for developing PTSD. It stands to reason that PTSD symptoms might be a mechanism through which the experience of physical abuse contributes to increased drug risk.
The present investigation sought to establish the association between physical abuse and increased risky drug use (HIV-related drug risk) in a sample of opioid dependent persons. We hypothesized that physical abuse would be associated with increased PTSD symptoms, PTSD symptoms would be associated with increased risky drug use, and that physical abuse would be associated with increased risky drug use. Finally, we hypothesized that PTSD symptoms would mediate the relationship between physical abuse and risky drug use.
2.1 Material and Methods
The present study includes baseline assessment data from a randomized clinical trial examining inpatient buprenorphine detoxification vs. buprenorphine linkage to outpatient maintenance treatment (Reddy, Anderson, Liebschutz, & Stein, 2013). Hospitalized opioid dependent patients were recruited from the Boston Medical Center (BMC) from August 2009 and October 2012. Both the Butler Hospital and BMC Institutional Review Boards (IRB) approved the study. One-hundred and thirty- nine individuals consented to participation in the randomized trial, and 21 consented to a separate observation arm that included baseline and follow up assessments only. Of these 160, we limited our sample to 121 persons who had no history of sexual abuse victimization so as to avoid potential confounding with the effect of physical abuse.
2.2 Measures
Physical abuse was assessed using one question (Were you ever abused or physically attacked (not sexually) by someone you knew (for example, a parent, boyfriend, or husband) who hit, slapped, choked, burned, or beat you up?) from the Life Stressor Checklist- Revised (LSC-R) (McHugo et al., 2005). Respondents endorsed whether or not they had experienced this type of abuse any time in their life. Symptoms of PTSD were assessed with the Posttraumatic Checklist- Civilian Version (PCL-C). It is a self-report measure comprised of 17 items that correspond to the 17 symptoms of PTSD as diagnosed by the DSM-IV-TR (Weathers, Litz, Herman, Huska, & Keane, 1993). Respondents rated their symptoms in the past month on a 1 (not at all) to 5 (extremely) scale. Scores range from 17 to 85. The National Center for PTSD suggests a cut-point of 36–44 on the PCL in a specialized medical clinic setting for estimating probable PTSD (2012). The internal consistency (.94) and test-retest reliability (.88) are adequate (Weathers et al., 1993). We used drug-risk scale of the Risk Assessment Battery (RAB) as our HIV-related drug-risk index (Navaline et al., 1994). It assesses engaging in 8 items related to drug-risk behaviors such as injection use and the sharing of needles and other drug paraphernalia over the past three months with a maximum score of 22 (Navaline et al., 1994). The RAB has demonstrated adequate concurrent, discriminant, and predictive validity (Tourian et al., 1997) and been correlated with HIV serostatus and seroconversion (Metzger & Navaline, 2003).
2.3 Analytical Methods
We present descriptive statistics to summarize background characteristics and product-moment correlation coefficients to summarize bivariate associations. A two equation structural equation model (SEM) was specified to estimate the adjusted association of physical abuse victimization on PTSD symptomatology and drug-risk, and to test the hypothesis that PTSD mediates the effect of physical abuse victimization on HIV-related drug risk. Models were estimated using MPlus 5.1. To test hypotheses, we used bias-corrected bootstrap resampling with 5000 replications to estimate 95% confidence interval estimates for the unstandardized parameter estimates. Parameter estimates with 95% confidence intervals not including 0 are considered statistically significant. Simulation studies have shown that this method provides good coverage of single indirect effect population parameters with samples as small as 100 (MacKinnon, Lockwood, & Williams, 2004). Additionally, Fritz and MacKinnon (2007) found this method had greater statistical power to detect mediational effects than traditional methods such as Baron and Kenny’s (1986) causal steps test or joint significance test, or Sobel’s (1982) first-order test. Fritz and MacKinnon (2007) estimated the required sample size to detect mediated effects under a variety of conditions; our sample had sufficient power (1 – β > .8) to detect a mediated effect if one standardized path coefficient was ≥ .26, and the other standardized path coefficient was ≥ .39 (the latter is a “medium” effect and the former is between a “small and medium” effect based on Cohen’s (1988) suggested guidelines. We present the results as a path diagram with fully standardized (βyx) coefficients. Unstandardized coefficients (byx) and 95% confidence interval estimates are reported in the text for significant coefficients. The estimated mediation model is just-identified and perfectly reproduces the observed covariance matrix; thus we do not report fit statistics commonly reported when estimating models with over-identifying restrictions.
3.1 Results
Participants averaged 41.9 (± 12.1) years of age, 101 (83.5%) were male, 46 (38.0%) were non-Hispanic Caucasian, 36 (29.8%) were African-American, 29 (24.0%) were Hispanic, and 10 (8.3%) were of other racial or ethnic origins (in multivariate analysis dummy indicators for non-Hispanic Caucasian and African-American were entered as covariates) (Table 1). The mean scores on the RAB drug-risk index was 4.4 (± 5.8) and the mean score on the PCL-C index of PTSD symptomatology was 44.3 (± 17.6).
Table 1.
Descriptive Statistics and Product-Moment Correlations (n = 121).
| Product-Moment Correlations | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Mean (SD) | 1. | 2. | 3. | 4. | 5. | 6. | 7. |
| 1. RAB Drug Risk | 4.35 (5.83) | 1.00 | ||||||
| 2. PCL-C | 44.31 (17.64) | .29** | 1.00 | |||||
| 3. Gender (Male) | 0.83 (0.37) | −.17 | −.15 | 1.00 | ||||
| 4. Years Age | 41.88 (12.10) | −.32** | −.08 | .05 | 1.00 | |||
| 5. Non-Hispanic Caucasian (Yes) | 0.38 (0.49) | .31** | .05 | −.11 | −.41** | 1.00 | ||
| 6. African-American (Yes) | 0.30 (0.46) | −.33** | 0.30** | .09 | .46** | −.51** | 1.00 | |
| 7. Physical Abuse (Yes) | 0.31 (0.46) | .22** | .22* | −.09 | −.01 | .03 | −.24** | 1.00 |
p < .05,
p < .01
Bivariate analysis (product-moment correlations) (Table 1) indicated that the RAB drug-risk index was positively and significantly correlated with the PCL-C (r = −.29, p < .01), inversely and significantly associated with age (r = −.32, p < .01), significantly higher among non-Hispanic Caucasians (r = .31, p < .01), significantly lower among African-Americans (r = −.33, p < .01), and significantly higher among persons who reported physical abuse victimization (r = .22, p < .01) (Table 1). Without adjusting for background characteristics, PCL-C scores were significantly higher among person reporting physical abuse victimization (r = .22, p < .05) and, compared to all other ethnic groups, African-Americans had significantly higher PCL-C scores (r = .30, p < .01). Product-moment correlations among all variables included in the multivariate regression model are also reported in Table 1.
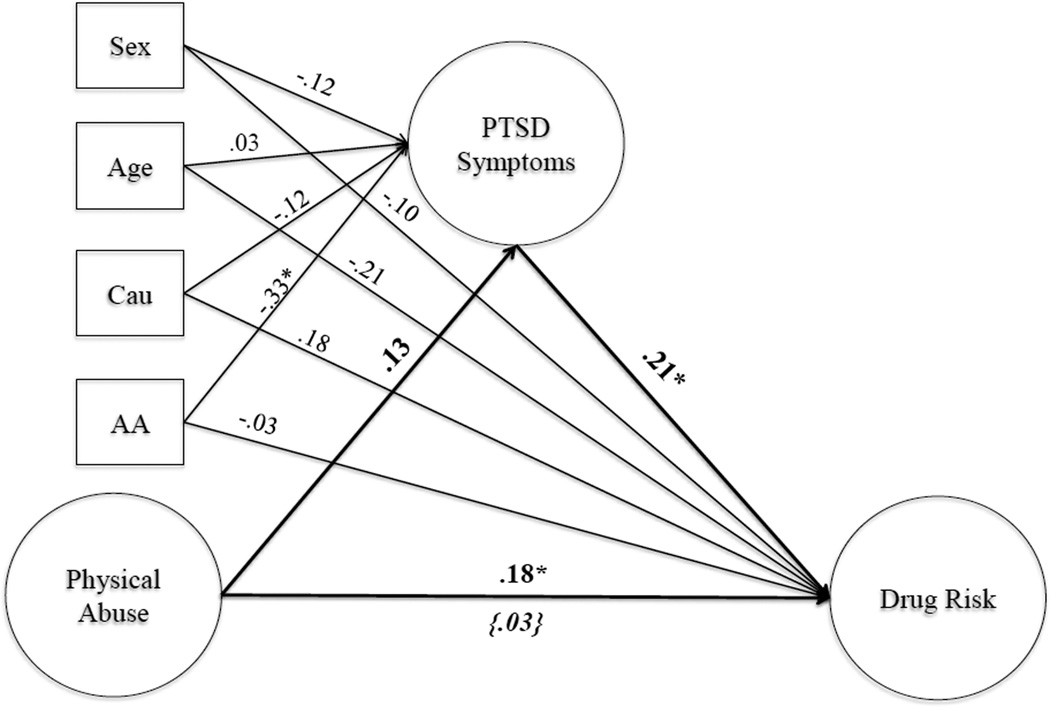
Figure 1 gives fully standardized coefficients for the two equation SEM. After controlling for demographic characteristics, physical abuse victimization did not have a statistically significant association with PTSD symptomatology, as measured by the PCL-C (byx = 5.10, 95%CI − 1.48; 11.69, p > .05). Compared to non-Hispanic Caucasians, African-Americans had significantly lower mean PCL-C scores ((byx = −12.56, 95%CI −21.55; −4.00, p < .05), but PCL-C scores were not associated significantly with either gender or age. Adjusted mean HIV drug-risk index scores were higher among persons reporting a history of physical abuse victimization (byx = 2.29, 95%CI 0.02; 4.54, p < .05) and positively associated with the PCL-C (byx = 0.07, 95%CI 0.02; 0.13). The fully standardized indirect of physical abuse on drug-risk, as mediated by PCL-C, is substantively very small (βyx = .03) and is given as the product of the direct effect of physical abuse on PCL-C (βyx = .13) times the direct effect of PCL-C on drugrisk (βyx = .21). The formal test for the mediation hypothesis was not statistically significant (byx = 0.35, 95%CI −0.16; 1.18, p > .05).
Figure 1.
Path analysis of PTSD symptoms as a mediator of the association between physical abuse (independent variable) and drug risk (dependent variable). Covariates are sex, age, and two ethnicity variables (Non-Hispanic Caucasian and African American) and are denoted by squares in the model. Cau = Dummy variable Non-Hispanic Caucasian. AA = dummy variable African-American. The indirect or mediated effect is bracketed and italicized. * denotes significant path coefficient.
4.1 Discussion
In this out-of-treatment, opiate-dependent cohort with high rates of HIV-related drug risk, we examined the associations among physical abuse history, PTSD symptoms, and risky drug use and tested whether PTSD symptoms mediated the relationship between physical abuse history and risky drug use. Our hypotheses were partially supported. We found that physical abuse history was significantly associated with risky drug use but not PTSD symptoms. Also, risky drug use was significantly associated with physical abuse history and PTSD symptoms. However, PTSD symptoms did not mediate the relationship between physical abuse history and HIV-related drug risk, indicating that the experience of PTSD is not always a catalyst to engage in high-risk HIV behaviors. The experience of physical abuse is enough to confer additional HIV-related drug risk for participants in this sample.
Of note is the high prevalence of PTSD symptoms reported here, in keeping with the high rate of PTSD reported among opioid dependent persons (Liebschutz et al., 2007). It has been estimated that one-third of all persons with an opioid use disorder have met criteria for PTSD in their lifetime (Mills, Teesson, Ross, Darke, & Shanahan, 2005), yet even with a high co-occurrence of PTSD in this population, PTSD does not appear to confer additional risk for risky drug use.
Given the sparse literature examining physical abuse history and drug use and the lack of support for PTSD as a mediator, we can only speculate as to the nature of the association between physical abuse history and HIV-related drug risk. We venture that physical abuse history may limit impulse control and decrease attention to risk protection. That is, persons with abuse histories may have difficulty resisting offers to share equipment. Relatedly, history of physical abuse may leave survivors with a sense of already being at risk in the world, producing fatalism that increases risk-taking. Finally, it could be that those who engage in risky drug use are more likely to find themselves in physically harmful situations, which may perpetuate PTSD symptoms by re-exposure to threatening stimuli.
There are some limitations to the present study. First, the study was cross-sectional and therefore directionality of results cannot be confirmed. Second, our lifetime measure of physical abuse also does not allow us to comment on recency or extent of physical abuse. Third, our measures rely on self-report. Fourth, these results might not generalize to other populations since the focus of the present study was on opioid dependent, hospitalized persons who are not receiving substance abuse treatment. Because our interest was in the understudied and distinct role of physical abuse in risky drug use, we excluded persons with sexual abuse, which could have confounded our findings. Despite these limitations, replication and longitudinal designs are needed to further clarify the associations among physical abuse history, PTSD symptoms, and risky drug use.
4.2. Conclusions
These results underscore the need for prevention efforts in this vulnerable population. Development of interventions, whether delivered during hospitalization or in the community, that specifically target the history of physical abuse, is imperative in light of the public health burden associated with opiate users’ elevated risk for HIV and other drug-related infectious diseases.
Highlights.
Sample consisted of opioid-dependent persons.
Physical abuse history was associated with increased HIV-related drug risk.
PTSD symptoms were associated with increased HIV-related drug risk.
PTSD symptoms did not mediate association of abuse history and drug risk.
Acknowledgments
Role of Funding Sources
This study was supported by NIDA grant R01 DA026223. NIDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Dr. Reddy conceptualized the present study and wrote the first draft of the manuscript. Dr. Anderson performed the statistical analyses and contributed to manuscript preparation. Dr. Liebschutz supervised data collection and provided edits of the manuscript. Dr. Stein conceptualized the present study, provided edits of the manuscript, and is the Principal Investigator of the parent study from which these data were collected.
Conflict of Interest
No conflicts of interest noted.
References
- Baron RM, Kenny DA. The moderator-mediator distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bensley LS, Eenwyk JV, Simmons Self-reported childhood sexual and physical abuse and adult HIV-risk behaviors and heavy drinking. American Journal of Preventative Medicine. 2000;18:151–158. doi: 10.1016/s0749-3797(99)00084-7. [DOI] [PubMed] [Google Scholar]
- CDC. HIV AIDS Surveillance Report. 2007 Jun;17:1–54. [Google Scholar]
- Chilcoat HD, Breslau N. Posttraumatic stress disorder and drug disorders: Testing Causal Pathways. Archives of General Psychiatry. 1998;55:913–917. doi: 10.1001/archpsyc.55.10.913. [DOI] [PubMed] [Google Scholar]
- Chuang CH, Liebschutz JM, Horton NJ, Samet JH. Association of violence victimization with inconsistent condom use in HIV-infected persons. AIDS and Behavior. 2006;10(2):201–217. doi: 10.1007/s10461-005-9046-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, MJ: Erlbaum; 1988. [Google Scholar]
- Cohen M, Deamant C, Barkan S, Richardson J, Young M, Holman S, Melnick S. Domestic violence and childhood sexual abuse in HIV-infected women and women at risk for HIV. American Journal of Public Health. 2000;90(4):560–565. doi: 10.2105/ajph.90.4.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang S, Deren S, Goldstein MF. Relationships between childhood abuse and neglect experience and HIV risk behaviors among methadone treatment drop-outs. Child Abuse & Neglect. 2002;26:1275–1289. doi: 10.1016/s0145-2134(02)00412-x. [DOI] [PubMed] [Google Scholar]
- Liebschutz J, Saitz R, Brower V, Keane TM, Lloyd-Travaglini C, Averbuch T, Samet JH. PTSD in urban primary care: high prevalence and low physician recognition. Journal of General Internal Medicine. 2007;22(6):719–726. doi: 10.1007/s11606-007-0161-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon D, Lockwood C, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39(1):1–24. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugo GJ, Caspi Y, Kammerer N, Mazelis R, Jackson EW, Russell L, Kimerling R. The assessment of trauma history in women with co-occurring substance abuse and mental disorders and a history of interpersonal violence. The Journal of Behavioral Health Services & Research. 2005;32(2):113–127. doi: 10.1007/BF02287261. [DOI] [PubMed] [Google Scholar]
- Metzger DS, Navaline H. Human immunodeficiency virus prevention and the potential of drug abuse treatment. Clinical Infectious Diseases. 2003b;37(Suppl 5):S451–S456. doi: 10.1086/377548. [DOI] [PubMed] [Google Scholar]
- Mills KL, Teesson M, Ross J, Darke S, Shanahan M. The costs and outcomes of treatment for opioid dependence associated with posttraumatic stress disorder. Psychiatric Services. 2005;56(8):940–945. doi: 10.1176/appi.ps.56.8.940. [DOI] [PubMed] [Google Scholar]
- Navaline HA, Snider EC, Petro CJ, Tobin D, Metzger D, Alterman AI, Woody GE. An automated version of the Risk Assessment Battery (RAB): Enhancing the assessment of risk behaviors. AIDS Research and Human Retroviruses. 1994;10S:281–283. [PubMed] [Google Scholar]
- National Center for PTSD. Using the PTSD Checklist. 2012 http://www.ptsd.va.gov/professional/pages/assessments/ptsd-checklist.asp.
- Plotzker RE, Metzger DS, Holmes WC. Childhood sexual and physical abuse histories, PTSD, depression, and HIV risk outcomes in women injection drug users: A potential mediating pathway. The American Journal on Addictions. 2007;16:431–438. doi: 10.1080/10550490701643161. [DOI] [PubMed] [Google Scholar]
- Reddy MK, Anderson BJ, Liebschutz J, Stein MD. Factor structure of PTSD symptoms in opioid-dependent patients rating their overall trauma history. Drug and Alcohol Dependence. 2013;32:597–602. doi: 10.1016/j.drugalcdep.2013.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sansone Ra, Whitecar P, Wiederman MW. The prevalence of childhood trauma among those seeking buprenorphine treatment. Journal of Addictive Diseases. 2009;28(1):64–67. doi: 10.1080/10550880802545101. [DOI] [PubMed] [Google Scholar]
- Tourian K, Alterman A, Metzger D, Rutherford M, Cacciola JS, McKay JR. Validity of three measures of antisociality in predicting HIV riks behaviors in methadone-maintenance patients. Drug and Alcohol Dependence. 1997;47:99–107. doi: 10.1016/s0376-8716(97)00076-8. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz B, Herman D, Huska J, Keane T. The PTSD Checklist (PCL): Reliability, Validity and Diagnostic Utility. Paper presented at the annual meeting of the International Society for Traumatic Stress Studies, Chicago. 1993 [Google Scholar]