Abstract
Background
Global health programs that allow international experiences for US learners should also enable reciprocal learning experiences for international learners, particularly if that is a need identified by the partner institution.
Methods
A partnership between Indiana University and Moi University, Kenya, has successfully hosted 41 visiting Kenyan internal medicine and pediatrics registrars at Indiana University since 2006. The program's logistics, curriculum, and evaluation are described.
Results
The registrars rotated through nephrology, cardiology, hematology and oncology, infectious diseases, and intensive care, as well as related ambulatory experiences, functioning on a level comparable to fourth-year medical students. They showed significant improvement in pretest and posttest scores on a standardized National Board of Medical Examiners examination (P = .048). International learners experienced culture shock, yet they felt the Indiana University elective was helpful and would recommend it to future participants.
Conclusions
Global health programs can reciprocate the benefits derived for US students and residents by offering learning experiences to international learners if that is an expressed need from the international partner. Barriers to those experiences can be overcome, and the hands-on, elective experience has the potential to positively affect the knowledge and attitudes of participants as well as the home nation.
What was known
There has been significant growth in global health experiences for US learners, yet few opportunities exist for international learners to learn in a US health care context.
What is new
A partnership between a US institution and a Kenyan university allowed 41 registrars in internal medicine and pediatrics to gain subspecialty experiences not available in their home country.
Limitations
Small sample size and single institution study limit generalizability.
Bottom line
Reciprocal US experiences for learners from low-resource countries can offer learning experiences with a beneficial effect on the home country.
Editor's Note: The online version (567KB, doc) of this article contains the program evaluation form used in the study.
Introduction
There has been a dramatic increase in US institutional global health programs and partnerships. This increase has allowed first-hand experiences in global health to be increasingly available to health professionals at all levels of training. In 2010, 30% of graduating American medical students participated in a global health experience, compared with 6% in 1984.1,2 Global health electives and tracks have been developed to meet the needs of residents in graduate medical education across multiple disciplines.3–8 These opportunities may help prepare residents for the challenges of a rapidly changing world.9
For global health partnerships to be considered equitable, reciprocal learning opportunities for faculty and trainees from the resource-limited institution can be made available in the resource-rich institution.10–15 Such opportunities may help to facilitate the sustainable development of national educational and research capacity.16–19
The Working Group on Ethics Guidelines for Global Health Training (WEIGHT) group guidelines for global health training programs represent an important effort to codify ethics and best practices for global health experiences.15 Although many principles also apply to bidirectional trainee exchanges, the guidelines' primary focus is on ethical issues for programs sending trainees from resource-rich to resource-limited settings.15 This reflects current trends: Although 95% of programs offer educational activities for resource-rich institutional learners, only 28% (28 of 99) of the programs surveyed in 2010 described clinical opportunities for international residents at the host institutions.14,20 The disparity occurs in an increasingly globalized world and at a time when physicians in both resource-rich and resource-limited settings are expected to have broad knowledge of current approaches to diagnosis and management of a variety of acute and chronic health conditions.21,22 One mechanism of accomplishing that is through hosting international learners from institutional partners in resource-limited settings.
The challenges to creating programs include varying educational program structures, language barriers, cultural differences, the need for support personnel, and program costs.15,20 For example, the Masters of Medicine (MMED) program is a common approach to international graduate medical education, which involves clinical training, conducting a research project, and writing a dissertation. It is offered in both medical and surgical specialties by institutions in Africa,23–28 Southeast Asia,29,30 and the South Pacific.31–33 Trainees may have several years of independent practice after graduation from medical school before starting the MMED program. There is a need to bridge those differences in training and experience by establishing a legal framework for visiting MMED students.
To our knowledge, the logistics for successfully hosting visiting international physicians from international postgraduate medical education programs in graduate medical education in the United States have not been reported. In this article, we describe our logistics, curriculum, and program evaluation to assist other programs that are interested in hosting international learners.
Methods
Hosting MMED Registrars at the Indiana University
Indiana University (Indianapolis) and Moi University (Eldoret, Kenya) have a long-standing global health partnership, dating back to 1989.19,34 The program was initiated in 2006 in response to a need identified by the Moi University School of Medicine (MUSM) leadership for an away elective to meet gaps in the MUSM curriculum for specialty training in the pediatrics or internal medicine (IM) subspecialties of nephrology, intensive care, hematology/oncology, and cardiology. The Indiana University School of Medicine (IUSM), Departments of Internal Medicine and Pediatrics, began to host Moi MMED and Masters of Pediatrics (MPED) candidates (also referred to as registrars). As of the 2012–2013 academic year, IUSM has hosted 41 MMED and MPED registrars for 4 to 6 months in the second year of their postgraduate training.
The goal of the IU elective is to gain knowledge in specific pediatrics or IM subspecialties designated by the home institution and to obtain new perspectives on health systems, medical education and research, health care delivery, the registrars' communities, and the registrars' collective potential as physicians and future health care leaders in their home countries.
Prequalifications
To participate in the exchange, registrars must have completed a 6-year undergraduate Bachelor of Medicine and Surgery program, received a Bachelor of Medicine and Surgery degree (MBChB), and spent a postgraduate year as a house officer with rotations in 4 specialties—IM, general pediatrics, obstetrics and gynecology, and general surgery. The candidates are enrolled at MUSM in an accredited Masters of Medicine program and have successfully completed 1 year of training in pediatrics or IM.
The registrars also meet the US Department of State requirements for an Exchange Visitor (J-1) visa.35 The Exchange Visitor Skills List36 published by the US Department of State is a list of professions with specialized knowledge and skills necessary for the development of the exchange visitor's home country.
As the Kenyan registrars are considered bona fide students in Kenya, pursuing MMED degrees with the US elective as part of their curriculum, their Exchange Visitor J-1 category is College and University Students under 22 CFR § 62.23. Exchange visitors in the student category may participate in degree or nondegree programs by postsecondary, accredited institutions for up to 24 months. Such a program must be carried out under a written agreement between an American and foreign educational institution. There is a cooperative agreement between IUSM and MUSM, which fulfills that criterion. The sponsor (IUSM) needs to verify that the student has sufficient academic credentials for the program. The registrars hold an MBChB degree from a Kenyan medical school but attend a nondegree program of study in a US medical school. To meet that requirement, the registrars are affiliated with IU and engaged full-time in a prescribed course of study that includes learning activities for 4 to 6 months, which overlaps with the curricular objectives of senior medical students in a pediatrics or IM elective. The curricular body for Moi University has reviewed and approved the US elective as part of the MUSM graduate curriculum, which allows the registrars to function in a student role on par with fourth-year medical students while in the United States.
Logistics
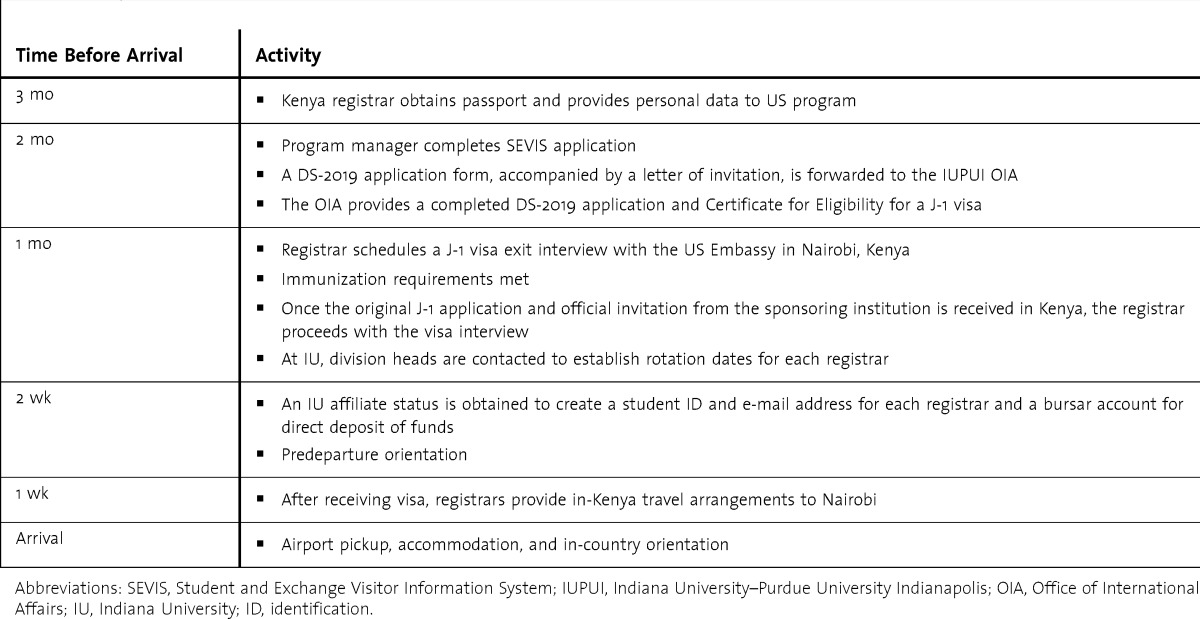
The arrangements are made several weeks to months before the registrars' arrival with the assistance of the IU Office of International Affairs, and are summarized in table 1. That timing is critical because of the 30-day window for verification of arrival in the United States from the date of visa appointment. A registrar's return to Kenya is scheduled immediately upon completion of the required electives, and the program coordinator arranges for transportation to the airport.
TABLE 1.
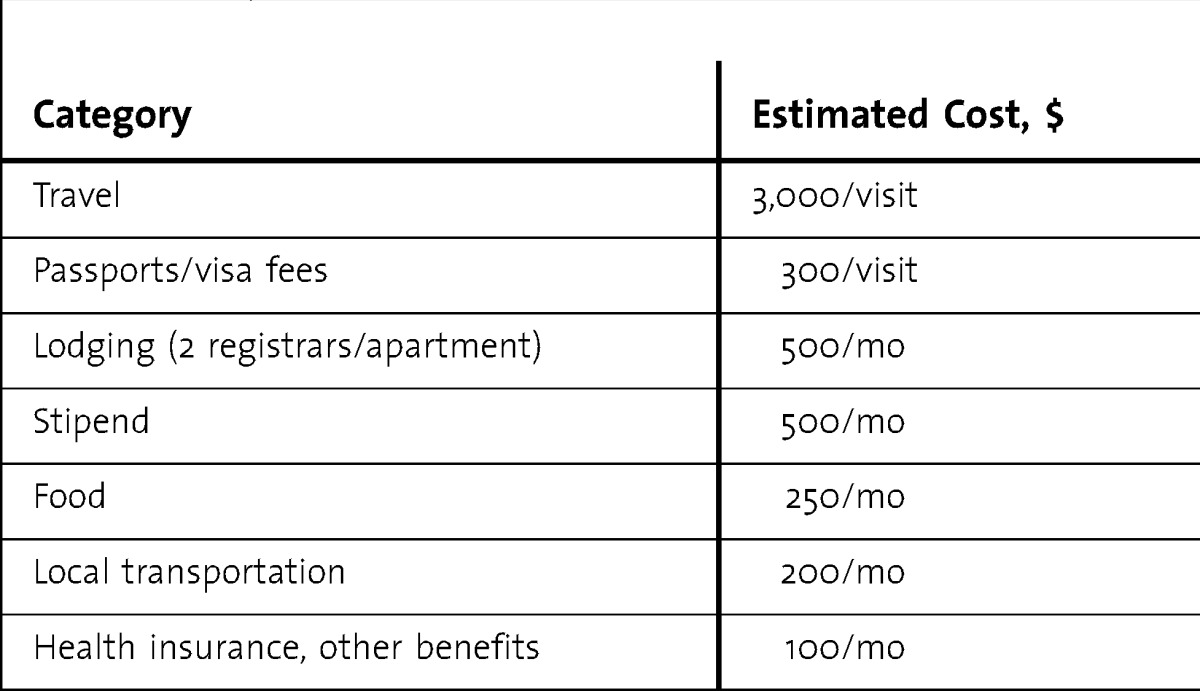
Itemized Estimated Expenses Per Registrar
Program Expenses
International travel expenses, apartment rental fees, local transportation, and health and auto insurance are covered by the host program from internal funds of the departments of IM and pediatrics and from donations from private philanthropy. These expenses average $3,000 for travel and $5,000–$8,000 for the 4- to 6-month stay. Itemized, estimated expenses are listed in table 2. The registrars receive a stipend for food, prepaid cellular phones, gasoline (if an IU vehicle is used), and incidentals. State and federal taxes are automatically deducted at the bursar's office. The Indiana Institute for Global Health Inc owns a donated vehicle, which the registrars share. Limiting the registrar's clinical activities to those of a supervised, fourth-year medical student allows for student-level malpractice coverage.
TABLE 2.
Program Evaluation by Participants
The Registrars' Curriculum
The focus of the curriculum is experiential learning with learning goals similar to those for US senior medical students. Personal and program goals and expectations are discussed during orientation, and registrars also receive education on the Cerner PowerChart (Cerner Corp, Kansas City, MO) electronic health records system. Access to educational resources is provided through the IUSM library. Orientation information includes social and cultural aspects to the practice of medicine in the United States, available through the Educational Commission for Foreign Medical Graduates.36
The registrars rotate through the subspecialties of nephrology, cardiology, hematology and oncology, infectious diseases, and intensive care. Those rotations address areas identified by the MUSM faculty as needing additional exposure and training. Registrars may elect to spend 1 to 2 weeks in electives after satisfactory completion of required rotations. Clinical rotations take place at the IU Health University Hospital, IU Health Riley Hospital for Children, and the Eskenazi Hospital (Indianapolis).
Outpatient experiences present different perspectives of patient acuity and disease progression. Where available, such experiences are evenly balanced with inpatient experiences. In their role as fourth-year medical students, the registrars are required to have the supervision of the team's senior resident and faculty, but they are able to participate actively in the care of their assigned patients. Attendance at regular educational conferences and conferences scheduled for global health track residents constitutes the didactic element of the curriculum.
The registrars meet with the program coordinator each month to help shape each registrar's experience. At the conclusion of the rotation, the program coordinator receives written evaluations on the registrars' performances, which are sent to the primary institution at the conclusion of the international experience.
Learners were evaluated using a standardized, written pretest and posttest. From 2009 to 2013, 15 pediatrics registrars took the standardized National Board of Medical Examiners (NBME) pediatrics subject examination, administered as a pretest of knowledge before the start of, and at the completion of, their IU elective. Program evaluation was done with postelective debriefing sessions and program evaluation forms.
The study was approved by the Indiana University Institutional Review Board and the Moi University Institutional Review Committee.
Results
Learner Evaluation
The NBME scores were obtained for 15 pretests and 13 posttests. Scores were evaluated using mean and standard deviation and the 2-tailed paired t test. The mean overall pretest score was 62.1 ± 8.6, and the mean overall posttest score was 68.2 ± 7.0 points (P = .048). The range of minimum acceptable passing scores was 59 to 67. The standard error of measurement was 4. Performance profiles were assessed in the areas of immunologic disorders and diseases of the blood; nutritional and digestive disorders; renal, urinary, and male reproductive systems; and cardiovascular disorders and diseases of the respiratory system. Improved performance was noted in all areas but only reached statistical significance in cardiovascular disorders and diseases of the respiratory system (P = .02).
Program Evaluation
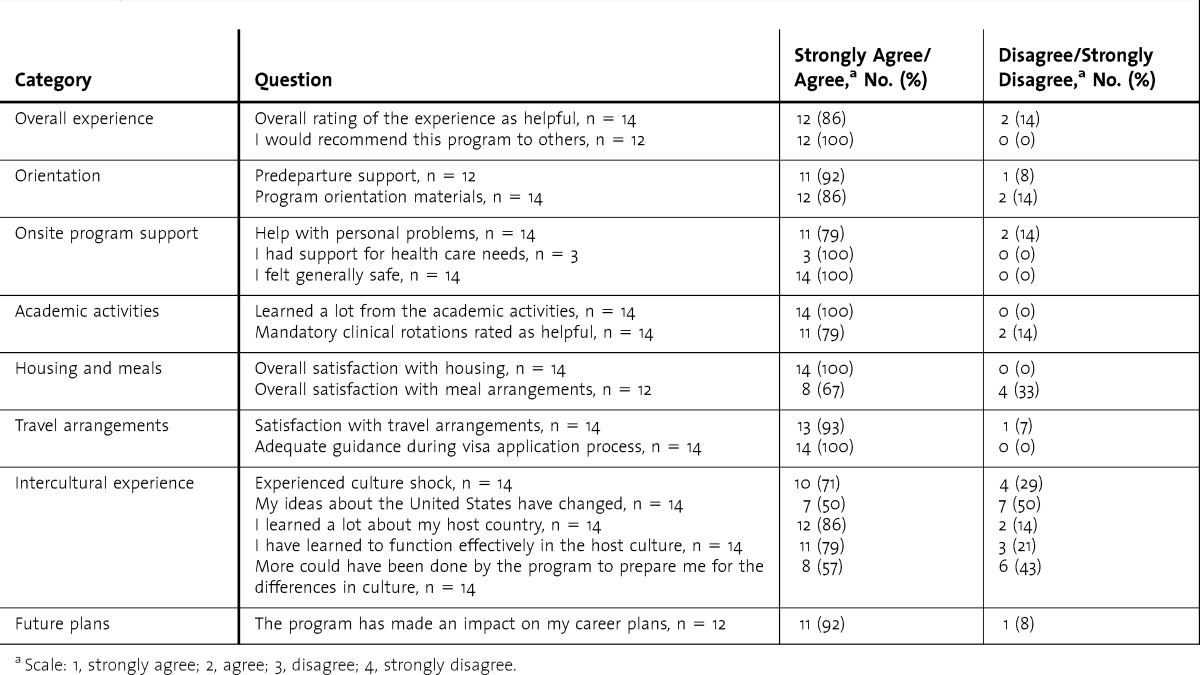
Feedback from the registrars was obtained through postelective, debriefing sessions and program evaluation forms. Overall, registrars expressed a high level of satisfaction with the organization of the program, including visa arrangements, orientation, housing, and transportation (table 3). All expected the elective experience to fulfill requirements for their home program, and all would recommend the elective to other colleagues.
TABLE 3.
Program Evaluation by Participants
Although specific feedback was not solicited from US residents on the registrars' assigned teams, the US residents were encouraged to share any positive or negative experiences in working with the visitors. Comments by the US residents working with the registrars offered added evidence of the potential benefits of fully integrating the registrars into the health care team.
All program participants returned to their institution to complete their training. Program records show that graduates have gone on to work in the Moi Referral and Teaching Hospital, the Kenya Ministry of Health facilities, the Academic Model Providing Access to Healthcare program, and private practice in Kenya.
Discussion
The results of the learner evaluation indicate that, for the pediatrics registrars studied, there was a statistically significant improvement in posttest scores. Although the registrars have a limited scope of practice during their visit, they are able to participate in patient care to a greater degree than an observer status would permit. This fosters a better understanding of the US health care system and greater engagement with the medical team. One lesson learned is that the composition of the team is essential to creating a positive hosting environment. As more IU faculty and residents have become aware of, or involved in, the IU-Kenya partnership, there has been increasingly positive feedback on their interactions with their host teams.
This awareness has also led to extra efforts to make the registrars feel welcome. Invitations for dinner and other events have helped to ease culture shock related to not only the social aspects of the US culture but also the differences between medical systems. In the program evaluation, 71% (10 of 14) of respondents reported experiencing culture shock, and 57% (8 of 14) felt that more could have been done by the program to prepare them for the differences in culture. Plans for program improvement include additional resources to ease culture shock and to address reverse-culture shock as they reintegrate into the home setting.
The process of setting up a program to host registrars involves detailed planning and engages personnel in both institutions. Both internal and external sources of funding were needed to sustain the program during the past 6 years. At $8,000 per visitor for international travel and a 4-month stay, the direct program costs are considerably less than those described for the Oxford/Duke resident exchange of $35,000 per visitor per year.37 However, our estimates do not include the indirect costs of the support personnel and faculty.
All registrars returned to their home country on completion of the IU elective. Preventing “brain drain” is essential to supporting the health infrastructure of the resource-limited home country.38,39 Embedding the exchange in the second year of their MMED training program means that the registrars need to return to complete their third year of training. They are also subject to the 2-year home-residence requirement under the Exchange Visitor J1 category INA 212(e), which requires them to return to their home country for a minimum of 2 years.
Limitations of our approach include the small sample size and the single nature of our intervention. In addition, the NBME examination used is aimed at medical students. It was used because it was a more accessible, standardized test than the residency in-training examination because of the registrars' designation in the program. Additional follow-up to determine what effect, if any, the elective had on the participants' individual career plans and their practice of medicine is needed.
Conclusion
It is important for global health programs based on international partnerships to reciprocate by offering learning experiences to international learners if that is an expressed need from the international partner. Many of the barriers to hosting visiting registrars can be overcome, and a well-structured experience can have positive educational outcomes, provide professional opportunities, and potentially affect medical practice at home.
Footnotes
Rachel A. Umoren, MBBCh, MS, is Assistant Professor of Clinical Pediatrics, Indiana University School of Medicine, and Visiting Scientist Scholar, Center for Health Information and Communication, Regenstrief Institute Inc; Robert M. Einterz, MD, is Professor of Clinical Medicine and Associate Dean for Global Health, Indiana University School of Medicine; Debra K. Litzelman, MD, is the D. Craig Brater Professor of Global Health Education, Director of Education, Indiana University Center for Global Health, Indiana University School of Medicine, and Senior Scientist, Regenstrief Institute Inc; Ronald K. Pettigrew, BS, is Director of Operations, Indiana University Center for Global Health; Samuel O. Ayaya, MBChB, MMED, is Professor of Child Health, Pediatrics, and Dermatology, Moi University School of Medicine, Eldoret, Kenya; and Edward A. Liechty, MD, is Professor of Pediatrics, Indiana University School of Medicine.
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
The authors would like to thank the Indiana University faculty and residents for their contributions toward the success of this program.
References
- 1.AAMC. Medical School Graduation Questionnaire: All Schools Report. Washington, DC: Association of American Medical Colleges; 1984. [Google Scholar]
- 2.AAMC. Medical School Graduation Questionnaire: All Schools Report. Washington, DC: Association of American Medical Colleges; 2010. [Google Scholar]
- 3.Henry JA, Groen RS, Price RR, Nwomeh BC, Kingham TP, Hardy MA, et al. The benefits of international rotations to resource-limited settings for U.S. surgery residents. Surgery. 2013;153(4):445–454. doi: 10.1016/j.surg.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 4.Tupesis JP, Babcock C, Char D, Alagappan K, Hexom B, Kapur GB. Optimizing global health experiences in emergency medicine residency programs: a consensus statement from the Council of Emergency Medicine Residency Directors 2011 Academic Assembly global health specialty track. Int J Emerg Med. 2012;5(1):43. doi: 10.1186/1865-1380-5-43. doi:10.1186/1865-1380-5-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tahvildari AM, Atnafu A, Cosco D, Acosta A, Gupta D, Hudgins PA. Global health and radiology: a new paradigm for US radiology resident training. J Am Coll Radiol. 2012;9(7):516–519. doi: 10.1016/j.jacr.2012.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Sekhar A, Eisenberg RL, Yablon CM. Enhancing the resident experience with global health electives. AJR Am J Roentgenol. 2012;198(2):W118–W121. doi: 10.2214/AJR.11.7104. doi: 10.2214/AJR.11.7104. [DOI] [PubMed] [Google Scholar]
- 7.Matar WY, Trottier DC, Balaa F, Fairful-Smith R, Moroz P. Surgical residency training and international volunteerism: a national survey of residents from 2 surgical specialties. Can J Surg. 2012;55(4):191–199. doi: 10.1503/cjs.005411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta A, Talavlikar R, Ng V, Chorny Y, Chawla A, Farrugia M, et al. Global health curriculum in family medicine: resident perspective. Can Fam Physician. 2012;58(2):143–146, e82–e86. [PMC free article] [PubMed] [Google Scholar]
- 9.Ackerly DC, Udayakumar K, Taber R, Merson MH, Dzau VJ. Perspective: global medicine: opportunities and challenges for academic health science systems. Acad Med. 2011;86(9):1093. doi: 10.1097/ACM.0b013e318226b455. [DOI] [PubMed] [Google Scholar]
- 10.Chiverton A. Ethics of international medical electives in the developing world: helping those in need or helping ourselves. Columbia Univ J Bioeth. 2009;8(1):46–49. [Google Scholar]
- 11.Conard CJ, Kahn MJ, DeSalvo KB, Hamm LL. Student clinical experiences in Africa: who are we helping. Virtual Mentor. 2006;8(12):855–858. doi: 10.1001/virtualmentor.2006.8.12.oped2-0612. [DOI] [PubMed] [Google Scholar]
- 12.Crump JA, Sugarman J. Ethical considerations for short-term experiences by trainees in global health. JAMA. 2008;300(12):1456. doi: 10.1001/jama.300.12.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hamadani F, Sacirgic L, McCarthy A. Ethics in global health: the need for evidence-based curricula. Mcgill J Med. 2009;12(2):120. [PMC free article] [PubMed] [Google Scholar]
- 14.Umoren RA, James JE, Litzelman DK. Evidence of reciprocity in reports on international partnerships. Educ Res Int. 2012;2012:603270. doi:10.1155/2012/603270. [Google Scholar]
- 15.Crump JA, Sugarman J. Working Group on Ethics Guidelines for Global Health Training (WEIGHT). Ethics and best practice guidelines for training experiences in global health. Am J Trop Med Hyg. 2010;83(6):1178–1182. doi: 10.4269/ajtmh.2010.10-0527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fluehr-Lobban C. Globalization of research and international standards of ethics in anthropology. Ann N Y Acad Sci. 2000;925:37–44. doi: 10.1111/j.1749-6632.2000.tb05582.x. doi:10.1111/j.1749-6632.2000.tb05582.x. [DOI] [PubMed] [Google Scholar]
- 17.Bateman C, Baker T, Hoornenborg E, Ericsson U. Bringing global issues to medical teaching. Lancet. 2001;358(9292):1539–1542. doi: 10.1016/S0140-6736(01)06586-2. [DOI] [PubMed] [Google Scholar]
- 18.Bernstein M. Ethical dilemmas encountered while operating and teaching in a developing country. Can J Surg. 2004;47(3):170–172. [PMC free article] [PubMed] [Google Scholar]
- 19.Einterz RM, Kelley CR, Mamlin JJ, Van Reken DE. Partnerships in international health: the Indiana University-Moi University experience. Infect Dis Clin North Am. 1995;9(2):453–455. [PubMed] [Google Scholar]
- 20.McKinley D, Williams S, Norcini J, Anderson M. International exchange programs and US medical schools. Acad Med. 2008;83(10):53. doi: 10.1097/ACM.0b013e318183e351. [DOI] [PubMed] [Google Scholar]
- 21.Drain PK, Primack A, Hunt DD, Fawzi WW, Holmes KK, Gardner P. Global health in medical education: a call for more training and opportunities. Acad Med. 2007;82(3):226–230. doi: 10.1097/ACM.0b013e3180305cf9. [DOI] [PubMed] [Google Scholar]
- 22.Hossain P, Kawar B, El Nahas M. Obesity and diabetes in the developing world—a growing challenge. N Engl J Med. 2007;356(3):213–215. doi: 10.1056/NEJMp068177. [DOI] [PubMed] [Google Scholar]
- 23.Balfour C. Emergency medicine—a new era in South African medicine [comment] S Afr Med J. 2008;96(1):47–48. [PubMed] [Google Scholar]
- 24.Enright A. Anesthesia training in Rwanda. Can J Anaesth. 2007;54(11):935–939. doi: 10.1007/BF03026799. [DOI] [PubMed] [Google Scholar]
- 25.Pust R, Dahlman B, Khwa-Otsyula B, Armstrong J, Downing R. Partnerships creating postgraduate family medicine in Kenya. Fam Med. 2006;38(9):661–666. [PubMed] [Google Scholar]
- 26.Hussey GD, Hawkridge A. The state and future of research at the University of Cape Town's Faculty of Health Sciences. S Afr Med J. 2012;102(6):412–414. doi: 10.7196/samj.5622. [DOI] [PubMed] [Google Scholar]
- 27.Evans C. Rahima Dawood Memorial Lecture 2002: Surgical training in Africa. East Cent Afr J Surg. 2005;10(2):5–9. [Google Scholar]
- 28.Madzimbamuto FD. Comparison between MMed anaesthesia programmes in the SADC. Afr J Health Prof Educ. 2012;4(1):22–27. [Google Scholar]
- 29.Lee TS, Ng BY, Lee WL. Neuropsychiatry: an emerging field. Ann Acad Med Singapore. 2008;37(7):601–605. [PubMed] [Google Scholar]
- 30.Wong TY, Koh GCh, Lee EH, Cheong SK, Goh LG. Family medicine education in Singapore: a long-standing collaboration between specialists and family physicians. Ann Acad Med Singapore. 2008;37(2):132–135. [PubMed] [Google Scholar]
- 31.Watters DA, Theile DE. Progress of surgical training in Papua New Guinea to the end of the 20th century. Aust N Z J Surg. 2000;70(4):302–307. doi: 10.1046/j.1440-1622.2000.01808.x. [DOI] [PubMed] [Google Scholar]
- 32.Vince JD. Medical postgraduate education in child health in Papua New Guinea. P N G Med J. 2000;43(1–2):54–59. [PubMed] [Google Scholar]
- 33.Clunie GJ, McCaig E, Baravilala W. The Fiji School of Medicine postgraduate training project. Med J Aust. 2003;179(11–12):631–632. doi: 10.5694/j.1326-5377.2003.tb05724.x. [DOI] [PubMed] [Google Scholar]
- 34.Oman K, Khwa-Otsyula B, Majoor G, Einterz R, Wasteson A. Working collaboratively to support medical education in developing countries: the case of the Friends of Moi University Faculty of Health Sciences. Educ Health (Abingdon) 2007;20(1):12. [PubMed] [Google Scholar]
- 35.US Department of State Bureau of Consular Affairs. Exchange Visitor Visa. http://travel.state.gov/content/visas/english/study-exchange/exchange.html. Accessed June 1, 2013. [Google Scholar]
- 36.Educational Commission for Foreign Medical Graduates. ECHO: ECFMG certificate holders office. http://www.ecfmg.org/echo/index.html. Updated June 4, 2012. Accessed January 7, 2013. [Google Scholar]
- 37.Miller WC, Corey GR, Lallinger GJ, Durack DT. International health and IM residency training: the Duke University experience. Am J Med. 1995;99(3):291–297. doi: 10.1016/s0002-9343(99)80162-4. [DOI] [PubMed] [Google Scholar]
- 38.Scott ML, Whelan A, Dewdney J, Zwi AB. “Brain drain” or ethical recruitment. Med J Aust. 2004;180(4):174–176. doi: 10.5694/j.1326-5377.2004.tb05862.x. [DOI] [PubMed] [Google Scholar]
- 39.Hagopian A, Thompson MJ, Fordyce M, Johnson KE, Hart LG. The migration of physicians from sub-Saharan Africa to the United States of America: measures of the African brain drain. Hum Resour Health. 2004;2(1):17. doi: 10.1186/1478-4491-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]


