Abstract
Background
Recent studies suggest that the supply of primary care physicians and generalist physicians in other specialties may be inadequate to meet the needs of the US population. Data on the numbers and types of physicians-in-training, such as those collected by the Accreditation Council for Graduate Medical Education (ACGME), can be used to help understand variables affecting this supply.
Objective
We assessed trends in the number and type of medical school graduates entering accredited residencies, and the impact those trends could have on the future physician workforce.
Methods
Since 2004, the ACGME has published annually its data on accredited institutions, programs, and residents to help the graduate medical education community understand major trends in residency education, and to help guide graduate medical education policy. We present key results and trends for the period between academic years 2003–2004 and 2012–2013.
Results
The data show that increases in trainees in accredited programs are not uniform across specialties, or the types of medical school from which trainees graduated. In the past 10 years, the growth in residents entering training that culminates in initial board certification (“pipeline” specialties) was 13.0%, the number of trainees entering subspecialty education increased 39.9%. In the past 5 years, there has been a 25.8% increase in the number of osteopathic physicians entering allopathic programs.
Conclusions
These trends portend challenges in absorbing the increasing numbers of allopathic and osteopathic graduates, and US international graduates in accredited programs. The increasing trend in subspecialization appears at odds with the current understanding of the need for generalist physicians.
Editor's Note: The ACGME News and Views section of JGME includes data reports, updates, and perspectives from the ACGME and its review committees. The decision to publish the article is made by the ACGME.
Introduction
Many experts agree that the United States is facing a physician shortage, particularly in the areas of primary care, generalist care across a range of specialties, and physicians in rural practice.1,2 While there is acknowledgement that a shortage of physicians could be at least partially addressed by increased staffing and training of non-MD health professionals,3,4 it seems clear that there are insufficient residency slots to meet the future demand for physicians.5 This shortfall could be particularly acute, given the number of individuals with new or expanded health care coverage under the Patient Protection and Affordable Care Act (ACA).6
In addition to the pressures on graduate medical education (GME) programs to produce increasing numbers of physicians, there are also pressures to accept increasing numbers of US medical graduates. After nearly 20 years of osteopathic undergraduate medical education expansion, and a decade of allopathic undergraduate medical education expansion, there now is growing concern that qualified domestic medical graduates may not find adequate GME opportunities.5 Also affecting the situation are international medical school graduates, both US and non-US citizens, who plan to enter US Accreditation Council for Graduate Medical Education (ACGME)–accredited residency programs. All of these trends give rise to concerns about the adequacy of the number of GME positions in the United States.
In light of discussions about pressures on the GME system, historical information from the ACGME about the number and capacity of accredited programs is particularly useful in understanding trends and influences affecting the supply of physicians in the United States.
Methods
Since 2004, the ACGME has produced annually a Data Resource Book (Databook) containing information on its accredited US residency programs and residents enrolled in those programs.7 The Databook is a concise reference for the GME community and policy makers that may be used to identify and clarify issues affecting accredited programs. The published information includes details on the number and types of programs and residents across all accredited core and subspecialty programs, as well as detail on the number of sponsoring institutions, accreditation status of programs, program director changes, and other deidentified data collected as part of the accreditation process.
The total number of physicians entering into clinical practice and the number of positions for entry into GME is determined by the number of positions available in pipeline specialties (those that lead to initial board certification). An examination of trends for pipeline specialties versus continuing GME subspecialties can help specify the scope and nature of projected physician shortages.
Since 2010, the Databook has been provided at no charge to the GME community and the public at large. The current version for academic year (AY) 2012–2013, as well as those for previous academic years, can be found on the ACGME website.7 We analyzed the longitudinal 10-year trend information, using this data to describe the changes in number and type of US residency programs and residents, and the potential effect of these changes on the number and type of physicians available to practice.
Results
Trend information from the most recent Databook (AY 2012–2013) shows the total number of continuing and pipeline GME programs has increased during the past decade, and now numbers 9157 programs—an increase of 1320 (16.8%) since AY 2003–2004.
figure 1 shows this growth by pipeline and continuing GME specialties for the past 10 years. The increase in the overall number of GME positions across the period is almost entirely explained by the growth in continuing GME specialty programs (programs that require the successful completion of a pipeline specialty residency program). Continuing GME programs show a 27.5% increase in number of programs over the decade, compared with a much smaller increase of 4.4% in the number of programs in pipeline specialties.
FIGURE 1.
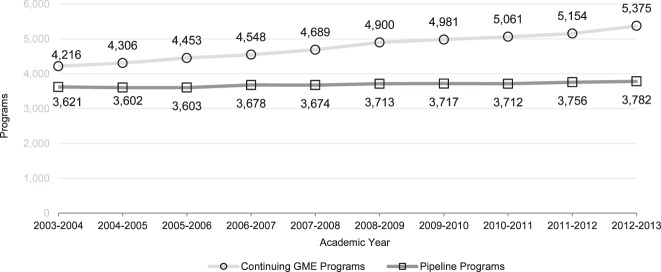
Number of Pipeline and Continuing GME Programs, by Academic Year
Abbreviation: GME, graduate medical education.
figure 2 shows the increase in the number of residents entering pipeline specialties and the number entering continuing GME programs across the 10-year period. While the increase in the number of residents between the 2 types of programs is similar, the 3111 additional residents entering pipeline specialties between AYs 2003–2004 and 2012–2013 represent a 13.0% increase, while the 3320 additional residents entering continuing GME programs represent an increase of 39.9%. In other words, the growth of subspecialty positions was more than 3 times the growth of pipeline positions.
FIGURE 2.
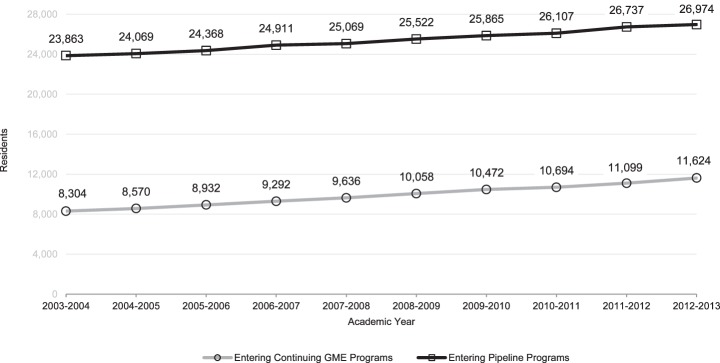
Number of Residents Entering Pipeline and Continuing GME Programs, by Academic Year
Abbreviation: GME, graduate medical education.
The growth in continuing GME positions results in a net increase in the subspecialization rate, with a growing number of residents extending their training through subspecialization, rather than entering clinical practice. These results are consistent with recent findings for obstetric graduates, as well as in the ACGME research that tracked residents in multiple specialties and programs.8,9
Additional information from the Databook (not shown) suggests that the modest increase in the number of residents entering the pipeline is due to 2 factors: (1) some growth in primary care programs, primarily in 2012, resulting from the Health Resources and Services Administration's Teaching Health Center Graduate Medical Education funding program;10 and (2) growth across all pipeline specialties resulting from an increase in program size. That is, residents in pipeline specialties are entering programs that have increased their capacity, with the size of pipeline specialty programs increasing from a mean of 21.3 residents per program in AY 2003–2004 to a mean of 23.8 residents per program in AY 2012–2013. This represents an increase of 11.7%. The increase in the average size of subspecialty programs is smaller at 8.1%, with programs increasing from a mean of 3.7 residents in AY 2003–2004 to a mean of 4.0 residents in AY 2012–2013.
figure 3 shows that the undergraduate medical education background of residents entering ACGME-accredited pipeline programs also has changed in the past 10 years, with an increasing proportion of osteopathic graduates entering pipeline specialties. Also, after an initial 5-year increase (AYs 2003–2004 to 2008–2009), there has been a stabilization or, in some cases, a reduction in the numbers of international medical graduates entering pipeline specialties. This observation is consistent with the findings reported for individual specialties.11,12 The most recent year also shows a reduction of 83 matriculating students rather than the anticipated continued increase in the number of graduates from Liaison Committee on Medical Education–accredited schools entering the pipeline. In contrast, the number of osteopathic graduates entering the same year increased by 262.
FIGURE 3.
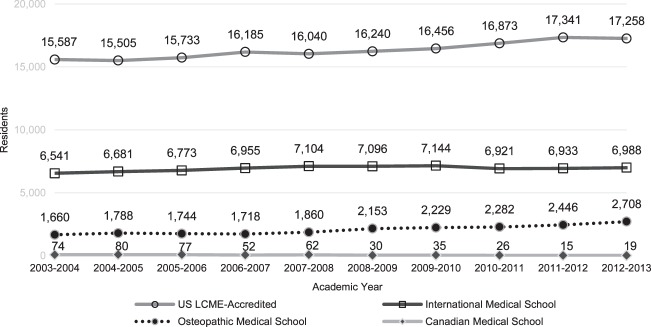
Number of Residents Entering the Pipeline, by Medical School Type and Academic Year
The growth in MD and DO graduates entering the pipeline reflects the increased output of US allopathic and osteopathic medical schools.13–15 The data in figure 3 show that for the past 5 years, the 25.8% growth rate (555 positions) of osteopathic graduates matriculating into pipeline programs outpaces the 6.3% growth rate (1018 positions) for graduates from allopathic schools. Further, in AY 2012–2013, while the number of osteopathic residents entering the pipeline increased by 262, and international graduates increased by 55, US allopathic graduates decreased by 83.
The number of physicians entering the pipeline has a direct effect on the number of physician graduates. Comparing the number of residents entering the pipeline with other data available in the Databook (not shown), it is clear that the percentage of individuals who graduate after completing subspecialty training has shown a marked increase in the past 10 years. In AY 2002–2003, 20.4% of all individuals completing an accredited program graduated from a subspecialty program. By AY 2011–2012 that number had risen to 27.7%.
Discussion
The changes in the number and composition of individuals entering GME programs over the past decade suggest several pronounced and concerning trends. As the total number of accredited programs has increased over the past decade, the increases have been concentrated almost exclusively in continuing GME (subspecialty) programs, with the increase in the total number of individuals enrolled in ACGME-accredited programs disproportionately found in continuing GME programs. The net result of these changes is a 35.9% increase in the subspecialization rate for graduates of pipeline programs (from 20.4% to 27.2%).
This is a concerning finding given that the United States appears to be experiencing a shortfall in primary care physicians and generalist physicians across a range of specialties. It is estimated that 7 million Americans live in a region that lacks adequate access to primary care,16 with a projected need for an additional 52 000 primary care physicians by 2025—in part to meet the new or expanded coverage for individuals expected under the ACA.6 In addition, the growth and aging of the population suggest a significant need for additional generalist physicians in areas such as neurology, surgery, and in surgical specialties such as orthopaedic surgery and otolaryngology.17–21 Our findings suggest that if current trends continue, these needs are unlikely to be met.
From the perspective of medical students seeking to enter residency, the increase in allopathic and osteopathic medical schools13–15 and the relatively unchanging number of positions in pipeline programs is of concern, as a growing number of medical school graduates will compete for the same or even a reduced number of positions. The match rates for US allopathic medical graduates have not yet shown a downward trend (the rate for 2012 was an all-time high of 95.1% and the match rate for 2013 was 93.7%).22 However, the increase in US citizens graduating from US allopathic and osteopathic schools, as well those completing medical school abroad, combined with the largely flat number of pipeline positions, suggests a trend that will reduce opportunities and limit trainee flexibility for entry into residency education.
The increase in the average size of programs in pipeline specialties suggests that GME leadership may be aware of this trend, and that pipeline programs are seeking to educate a larger number of physicians within their existing structure. This finding is of concern, if a limited number of pipeline programs are stretching resources to accommodate a larger number of residents. As patient volume and faculty availability, as well as other program assets important to high-quality education may be finite, quality could be compromised by further expansion, suggesting that new program creation will be an important dimension of any GME pipeline expansion.
Having an adequate future supply of physicians is important to the health of the nation.23,24 There is evidence to suggest that even seemingly intractable health disparities, such as racial-ethnic differences in access to care, are significantly ameliorated in regions with an adequate supply of generalist physicians.25 Our findings suggest that trends in GME, including the shift to additional subspecialty training for a sizable number of trainees, may undermine efforts to ensure an adequate future medical workforce, and has the potential to exacerbate the current inequitable distribution of physicians, such as the undersupply of surgeons and other generalist physicians in rural areas.26 There are data to suggest that physicians with subspecialty training are less likely to enter rural practice,27,28 and only 4.8% of all GME graduates located their practice in rural areas.29
A limitation of our findings is that the data in the Databook are confined to accredited residencies and specialties, and the proportion of residents entering non–ACGME-accredited fellowship programs is not accounted for. Sources indicate this number is increasing,30–32 and inclusion of these data would show even greater subspecialization rates for graduates of pipeline specialty programs.
Conclusion
Trends over the past decade demonstrate substantial increases in the total number of ACGME-accredited residency programs and enrolled residents. However, the increases in programs are not uniform across pipeline and continuing GME disciplines, and the distribution of occupants of these positions by medical school origin has changed. The observed flat number of positions in pipeline specialties likely will reduce the opportunities for entering residency for the growing number of US medical school graduates. The trend in subspecialization observed appears to be at odds with the current understanding of the needs of the American public for generalist physicians in most specialties.
Footnotes
All authors are at the Accreditation Council for Graduate Medical Education (ACGME). Kathleen D. Holt, PhD, is Senior Analyst and Director of Special Projects; Rebecca S. Miller, MS, is the Senior Vice President of Applications and Data Analysis; Ingrid Philibert, PhD, MBA, is Senior Vice President for Field Activities; and Thomas J. Nasca, MD, MACP, is Chief Executive Officer, ACGME and ACGME International, and Professor of Medicine (vol), Jefferson Medical College, Thomas Jefferson University.
References
- 1.Jolly P, Erikson C, Garrison G. US graduate medical education and physician specialty choice. Acad Med. 2013;88(4):468–474. doi: 10.1097/ACM.0b013e318285199d. [DOI] [PubMed] [Google Scholar]
- 2.Whitcomb ME. Commentary: meeting future medical care needs: a perfect storm on the horizon. Acad Med. 2011;86(12):1490–1491. doi: 10.1097/ACM.0b013e318235d5d4. [DOI] [PubMed] [Google Scholar]
- 3.Green LV, Savin S, Lu Y. Primary care physician shortages could be eliminated through use of teams, nonphysicians, and electronic communication. Health Aff (Millwood) 2013;32(1):11–19. doi: 10.1377/hlthaff.2012.1086. [DOI] [PubMed] [Google Scholar]
- 4.Chen PG, Mehrotra A, Auerbach DI. Do we really need more physicians: responses to predicted primary care physician shortages. Med Care. 2014;52(2):95–96. doi: 10.1097/MLR.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 5.Iglehart JK. The residency mismatch. N Engl J Med. 2013;369(4):297–299. doi: 10.1056/NEJMp1306445. [DOI] [PubMed] [Google Scholar]
- 6.Petterson SM, Liaw WR, Phillips RL, Jr, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010–2025. Ann Fam Med. 2012;10(6):503–509. doi: 10.1370/afm.1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Accreditation Council for Graduate Medeical Education. Data Resource Book, Academic Year 2012–2013. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/PublicationsBooks/2012-2013_ACGME_DATABOOK_DOCUMENT_Final.pdf. Accessed March 13, 2014. [Google Scholar]
- 8.Rayburn WF, Gant NF, Gilstrap LC, Elwell EC, Williams SB. Pursuit of accredited subspecialties by graduating residents in obstetrics and gynecology, 2000–2012. Obstet Gynecol. 2012;120(3):619–625. doi: 10.1097/AOG.0b013e318265ab0a. [DOI] [PubMed] [Google Scholar]
- 9.Byrne LB, Holt KD, Richter T, Miller RS, Nasca TJ. Tracking residents through multiple residency programs: a different approach for measuring residents' rates of continuing graduate medical education in ACGME-accredited programs. J Grad Med Educ. 2010;2(4):616–623. doi: 10.4300/JGME-D-10-00105.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.2011. HR 3590, Patient Protection and Affordable Care Act, §5508, Increasing Teaching Capacity, Part C of Title VII of the Public Health Service Act (42 USC. 293k et seq), as amended by §5303, as further amended by inserting after §749 the following: §749A. Teaching Health Centers Development Grants, [Google Scholar]
- 11.Biggs WS, Bieck AD, Crosley PW, Kozakowski SM. Entry of US medical school graduates into family medicine residencies: 2011–2012. Fam Med. 2012;44(9):620–626. [PubMed] [Google Scholar]
- 12.Terhune KP, Zaydfudim V, Abumrad NN. International medical graduates in general surgery: increasing needs, decreasing numbers. J Am Coll Surg. 2010;210(6):990–996. doi: 10.1016/j.jamcollsurg.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 13.Association of American Medical Colleges. AAMC Databook, Table 27: Total Graduates by US Medical School and Sex, 2009–2013. http://www.aamc.org/data/databook/tables. Accessed January 31, 2014. [Google Scholar]
- 14.American Association of Colleges of Osteopathic Medicine. Trends in osteopathic medical school applicants, enrollment and graduates. http://www.aacom.org/data/Documents/Trends-apps-enroll-grads.pdf. Accessed January 31, 2014. [Google Scholar]
- 15.Iglehart JK. The uncertain future of Medicare and graduate medical education. N Engl J Med. 2011;365(14):1340–1345. doi: 10.1056/NEJMhpr1107519. [DOI] [PubMed] [Google Scholar]
- 16.Huang ES, Finegold K. Seven million Americans live in areas where demand for primary care may exceed supply by more than 10 percent. Health Aff (Millwood) 2013;32(3):614–621. doi: 10.1377/hlthaff.2012.0913. [DOI] [PubMed] [Google Scholar]
- 17.Freeman WD, Vatz KA, Griggs RC, Pedley T. The Workforce Task Force report: clinical implications for neurology. Neurology. 2013;81(5):479–486. doi: 10.1212/WNL.0b013e31829d8783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dall TM, Chakrabarti R, Storm MV, Elwell EC, Rayburn WF. Estimated demand for women's health services by 2020. J Womens Health (Larchmt) 2013;22(7):643–648. doi: 10.1089/jwh.2012.4119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fraher EP, Knapton A, Sheldon GF, Meyer A, Ricketts TC. Projecting surgeon supply using a dynamic model. Ann Surg. 2013;257(5):867–872. doi: 10.1097/SLA.0b013e31826fccfa. [DOI] [PubMed] [Google Scholar]
- 20.Williams TE, Jr, Ellison EC. Population analysis predicts a future critical shortage of general surgeons [discussion in Surgery. 2008;144(4):554–556] Surgery. 2008;144(4):548–554. doi: 10.1016/j.surg.2008.05.019. [DOI] [PubMed] [Google Scholar]
- 21.Dall TM, Gallo PD, Chakrabarti R, West T, Semilla AP, Storm MV. An aging population and growing disease burden will require a large and specialized health care workforce by 2025. Health Aff (Millwood) 2013;32(11):2013–2020. doi: 10.1377/hlthaff.2013.0714. [DOI] [PubMed] [Google Scholar]
- 22.National Resident Matching Program. Results and Data: 2013 Main Residency Match. Vol. 2013. Washington, DC: National Resident Matching Program; p. 1. [Google Scholar]
- 23.Continelli T, McGinnis S, Holmes T. The effect of local primary care physician supply on the utilization of preventive health services in the United States. Health Place. 2010;16(5):942–951. doi: 10.1016/j.healthplace.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 24.Grover A, Niecko-Najjum LM. Building a health care workforce for the future: more physicians, professional reforms, and technological advances. Health Aff (Millwood) 2013;32(11):1922–1927. doi: 10.1377/hlthaff.2013.0557. [DOI] [PubMed] [Google Scholar]
- 25.Soneji S, Armstrong K, Asch DA. Socioeconomic and physician supply determinants of racial disparities in colorectal cancer screening. J Oncol Pract. 2012;8(5):e125–e134. doi: 10.1200/JOP.2011.000511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen C, Petterson S, Phillips RL, Mullan F, Bazemore A, O'Donnell SD. Toward graduate medical education (GME) accountability: measuring the outcomes of GME institutions. Acad Med. 2013;88(9):1267–1280. doi: 10.1097/ACM.0b013e31829a3ce9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Valentine RJ, Jones A, Biester TW, Cogbill TH, Borman KR, Rhodes RS. General surgery workloads and practice patterns in the United States, 2007 to 2009: a 10-year update from the American Board of Surgery [discussion in Ann Surg. 2011;254(3):525–526] Ann Surg. 2011;254(3):520–525. doi: 10.1097/SLA.0b013e31822cd175. [DOI] [PubMed] [Google Scholar]
- 28.Basco WT, Rimsza ME Committee on Pediatric Workforce; American Academy of Pediatrics. Pediatrician workforce policy statement. Pediatrics. 2013;132(2):390–397. doi: 10.1542/peds.2013-1517. [DOI] [PubMed] [Google Scholar]
- 29.Matsumoto M, Inoue K, Bowman R, Noguchi S, Toyokawa S, Kajii E. Geographical distributions of physicians in Japan and US: impact of healthcare system on physician dispersal pattern. Health Policy. 2010;96(3):255–261. doi: 10.1016/j.healthpol.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 30.Pack QR, Keteyian SJ, McBride PE. Subspecialty training in preventive cardiology: the current status and discoverable fellowship programs. Clin Cardiol. 2012;35(5):286–290. doi: 10.1002/clc.21959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Balistreri WF. Growth and development of a new subspecialty: pediatric hepatology. Hepatology. 2013;58(2):458–476. doi: 10.1002/hep.26580. [DOI] [PubMed] [Google Scholar]
- 32.Rattner DW, Apelgren KN, Eubanks WS. The need for training opportunities in advanced laparoscopic surgery. Surg Endosc. 2001;15(10):1066–1070. doi: 10.1007/s004640080021. [DOI] [PubMed] [Google Scholar]


