Abstract
Background
Mycosis fungoides (MF), the most common subtype of cutaneous T-Cell Lymphoma (CTCL), is a rare chronic skin neoplasia. Total skin electron irradiation has been employed along with a variety of other topical or systemic treatments for MF management.
Aim
To report the first case treated by TSEB irradiation protocol in Greece.
Materials and methods
A fractionated 36 Gy total skin electron beam (TSEB) therapy was prescribed to a 65-years-old male patient with mycosis fungoides (MF), stage IIB, refractory to several treatments during a 20-year period. Dose uniform delivery was monitored by thermo-luminescence dosimetry.
Results and discussion
The homogeneous skin dose distribution resulted in a complete clinical response. Limited, irradiation-oriented, side effects appeared.
Conclusions
The first TSEB irradiation prescription in Greek medical chronicles was proved effective in this case of tumor stage MF (T3-IIB), which had been refractory to several single or combination treatments.
Keywords: Mycosis fungoides, TSEB, Radiation therapy
1. Background
Mycosis fungoides (MF) is a cutaneous T-Cell Lymphoma (CTCL) that involves the skin and derives from malignant T-lymphocytes. It is a chronic, progressive, and quite rare non-Hodgkin lymphoma.1,2 The prevalence of MF in the United States of America is 3:106.3 The vast majority of patients are between 45 and 69 years of age at diagnosis,3 without excluding even childhood patients.1,4
Management of MF is stage-dependent and consists of a wide spectrum of treatments (corticosteroids, phototherapy, cytostatics, biologics, etc).1 An available treatment of the MF is radiation therapy all over the skin surface by utilizing low energy electrons (4–9 MeV), produced by a linear accelerator.3–8 This technique is referred in current literature as total skin electron beam (TSEB) therapy.3,8 This modality differs from conventional radiation protocols as the patient is irradiated at an off-couch setup.3 The creation of wide electron fields is achieved either by exploiting an extended source to skin distance (SSD) (≈7 m) or by the matching of two or more angled electron beams at a shorter SSD (≈2–4 m). TSEB irradiation can be performed mainly by applying three different treatment techniques, according to patient setup in respect to the enlarged static electron field: (a) standing patient techniques – patient takes at each session certain positions of treatment, (b) rotary techniques – with simultaneous rotation and irradiation of the skin, and (c) translational techniques – patient slides through the static broad electron beam. In addition, to accomplice these irregular setups of treatment, specially designed equipment should be provided for the modulation of the electron beam and a proper positioning and immobilization of the patient at each treatment session.3–8
2. Aim
This study presents the case of a 65-years-old male patient with mycosis fungoides (MF) stage IIB refractory to previous treatments, treated with total skin electron beam (TSEB) therapy who achieved a complete clinical response (CCR). This is the first case ever to be treated with TSEB irradiation protocol in Greece.
3. Materials and methods
In March 2011, a 65-year-old patient stage IIB9 MF, refractory to several treatments, as neotigason, interferon alpha (INFa), bexarotere, in combination with psoralen and ultraviolet A (PUVA) treatment, has been referred for TSEB therapy at the Radiation Therapy unit of the University General Hospital “Attikon”. From his medical history, he had a cutaneous basal-cell cancer in the region of the left supraorbital arch confronted by surgical removal and a 10-days radiation therapy Scheme 37 years ago. His MF was diagnosed 20 years ago. At the time of referral he had multiple ulcerated plaques on his trunk and thighs, and two large tumors at the inner site of his left knee, despite INFa treatment 3.000.000 × 3 times weekly, which was discontinued at the time of initiation of TSEB. He also suffered from severe pruritus. His modified severity weighted assessment tool (mSWAT) score10 was 194.5.
Additional investigations included biopsy from the recent tumor located in the inner thigh, flow cytometry and clonality of peripheral blood T cells and computed tomography (CT) scans. Histology from the skin biopsy revealed a tumor MF with cluster of differentiation (CD)3+, CD4+, CD8−, CD7+, CD30+ immunophenotype. Flow cytometry of the peripheral blood showed a Th2 immunophenotype with an increase of intracytoplasmic interleukin-4 (IL-4) and T-cell receptor TCR rearrangement of the CD3 gene was shown by polymerase chain reaction (PCR). He also had reactive inguinal lymphadenopathy. CT scans from his thorax, upper and lower abdomen were not consistent with extracutaneous spread. Lymph nodes were not drained and there was no involvement of any visceral organ. Bone marrow biopsy was normal.
Pre-treatment CT scan and laboratory examinations revealed no essential differentiation in his clinical condition since 2008, good thyroid functions, and normal hematology, with limited leucopenia due to IFNa treatment (white blood cell (WBC) count: 2600, neutrophil (Neut) count: 1600).
Total skin electron beam therapy was initiated.3,9,11 The patient was irradiated by utilizing the recently established in our unit 6-dual field TSEB irradiation technique, as described by Platoni et al.12 An enlarged and uniform electron field of 200 cm × 80 cm is formed by two individual, angled (252.5° and 287.5°), 36 cm × 36 cm, 6 MeV electron fields. The ability of producing such large electron fields without any electron applicator is provided by the high dose total skin electron (HDTSe−) mode which is available on our Clinac 2100C (Varian Medical Systems, Palo Alto, CA) linear accelerator. Dose rate is automatically set at almost 2500 MU/min at isocenter. The treatment plane is located at 2.8 m from the linear accelerator's isocenter. A large polymethyl methacrylate (PMMA) panel (203 cm × 111 cm and thickness of 0.5 cm), homogenates the produced field 30 cm before treatment plane. This attenuator is attached to a home-made patient support-system. In this system, patient is aligned in respect to the gantry of the linear accelerator and treatment can be performed at 240°, 0°, 120°, 300°, 180° and 60°, by patient's gradual rotation, resulting in total skin irradiation.
Due to extent of skin involvement, the prescribed dose was 3600 cGy,12–14 fractionated in a daily dose of 200 cGy, following a two-day irradiation cycle, in order to fully cover his body surface (Fig. 1). The treatment course, started on the 6th of June 2011, was completed in nine weeks without any interval and consisted of two irradiation cycles (four days) per week. During beam-on time, the eyes, nails, and genitals were shielded by lead blocks of at least 0.4 cm in thickness, till the completion of the treatment, in order to avoid radiation side effects. The nails were covered due to the lack of MF lesions but mainly to protect them from radiation induced toxicity (e.g. melanonychia). The shields were taped on the nails at each session. Eyes were protected by a lead-filled pair of goggles (1.5 cm of lead), and genitals by a 0.4 cm lead sheet attached to the inner surface of a jockstrap.
Fig. 1.
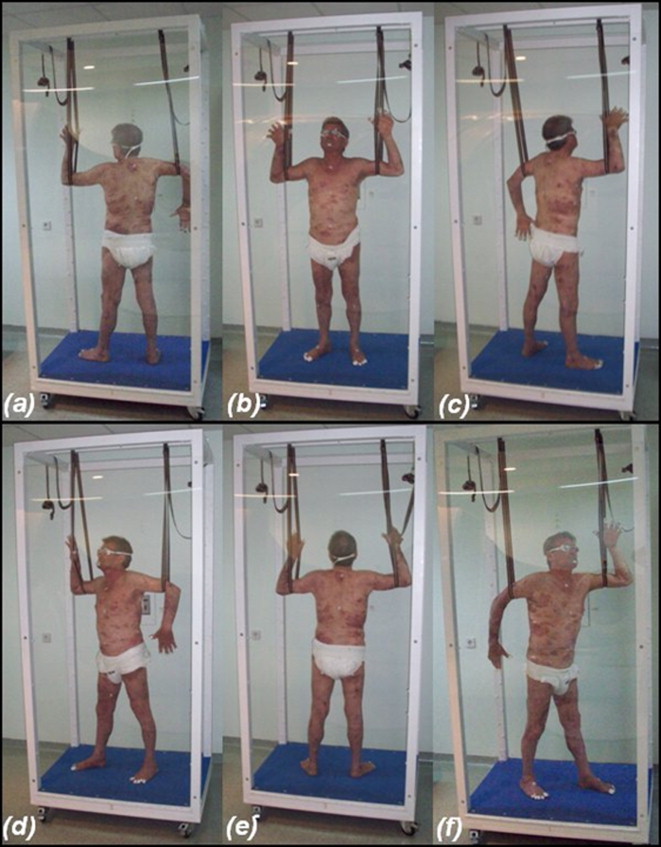
TSEB therapy positions during (a)–(c) first day of treatment cycle and (d)–(f) second day of treatment cycle.
After the first 2000 cGy, the vertex of the scalp was also covered by a lead helmet of 0.4 cm in thickness in order to restrain hair loss. The shielding of the scalp was decided after considering the results of the daily “in vivo” dosimetry, as in this region an excess amount of 120% (average) of the prescribed dose was delivered continually.
For accurate determination of the dose delivered to the patient, 80 thermo-luminescence (TL) detectors (GR200A) were distributing to patient's body uniformly on a daily basis, for the first four weeks of treatment. After this period and until the completion of the treatment, only a district number of TL detectors (60) were utilized, for practical reasons. Dosimeters were placed on certain positions every day, focusing especially on areas of irregular beam incidence. For further assistance, a human-figure drawing with premarked numbered spots was guiding TL detectors’ positioning every day. Moreover, the points of “in vivo” dosimetry were dyed with fuchsine on the skin to ensure reproducibility of our measurements. The detectors were placed on spots of increased interest, such as potential underdosed regions on the body (axillae, perineum, various body folds, etc.). In addition, ten of the dosemeters were always pasted at reference and normalization point (umbilicus) and at plane surfaces of the body (chest, back, limbs, etc.). Results were retrieved from the daily dose mapping procedure (36 measurements in total at 60 premarked spots on the skin). The detectors were handled within opaque and numbered paper envelopes. Calibration, annealing and signal acquirement were performed by an ETT annealing oven (Fimel, Vélizy, France) and a Manual thermo-luminescence dosimetry (TLD) reader (Fimel, Vélizy, France).
The calibration of the detectors occurred at an on-couch setup, utilizing a 10 cm × 10 cm electron applicator, SSD of 1 m, build-up and backscatter PMMA of 0.8 cm and 15 cm, respectively, irradiated at the same nominal energy (6 MeV) of TSEB therapy performance, which resulted in mean electron energy at treatment plane of 3.4 MeV. To confirm the validity of calibration for TSEB irradiation setting, 10 randomly selected detectors from the already calibrated patch were also irradiated in TSEB therapy setup (positioned vertically in relation to the 270° gantry angle position). The dose delivered to the detectors was 1 Gy. The corresponding monitor units (MU) were calculated by utilizing a parallel plate ionization chamber Roos® (PTW, Freiburg, Germany) connected to a Unidos® electrometer (PTW, Freiburg, Germany). The mean value of the acquired readings was compared to the mean reading retrieved by the on-couch dose delivery.
The coincidence of dosemeters’ response in the different setups was calculated by the formula:
| (1) |
where D is the percentage deviation of the two measurements; is mean TL detector reading acquired at TSEB irradiation conditions; is mean TL detector reading acquired at standard calibration conditions.
The deviation between the two dose measurements was less than 1% (0.4%). Thus, the initial calibration was considered reliable to be used for the “in vivo” dose determination.
4. Results and discussion
“In vivo” measurements revealed quite a homogeneous dose distribution on the skin (Fig. 2). Mean percentage dose on the skin was 101% of the prescription, showing a standard deviation of ±10.5%. The maximum percentage dose value was 138% (region of the feet) and the minimum 85% (arms).
Fig. 2.
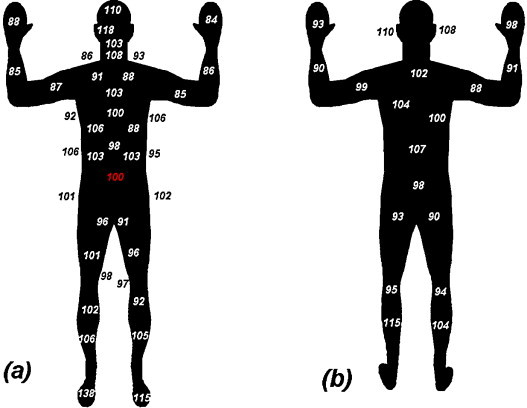
Percentage mean dose distribution on patient skin from all irradiation sessions. (a) Anterior side. (b) Posterior side.
The majority of underdosed areas appeared in the neck and supraclavicular area, armpits, hands, bubonic area and gluteal creases, as it was expected due to human body curvature. Conversely, the head and the lower part of the legs (tibiae and feet) seemed to be overdosed.
First side effects appeared at the second week of irradiation. The response of the skin to the treatment was acute: skin erythema, lesion exaltation, bleeding, wet desquamation, moderate edema, epilation, local pruritus, and fatigue. These symptoms continued until the sixth week of irradiation, when they started to withdraw. At the middle of the treatment, the patient had topical alopecia. Until the ninth week, all lesions were transformed into white patches on a lightly browned skin (Figs. 3 and 4a and b). The region that seemed to resist treatment was the skin of the left loin (Fig. 4c and d). On this anatomical area, two pairs of 6 MeV electron boost fields, sized 10 cm × 10 cm, were applied after the completion of the whole skin irradiation in order to deliver a total of 100 cGy to this region. The soles of the feet (although under-dosed) were not further irradiated due to the lack of MF lesions.
Fig. 3.
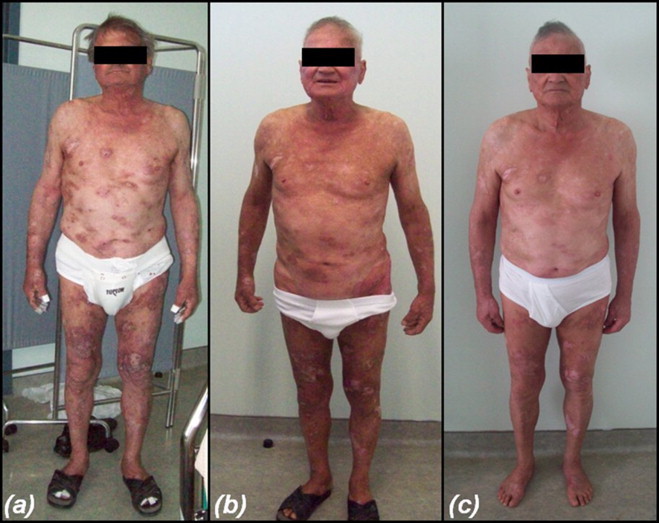
Clinical condition of patient at (a) the 4th week of irradiations (b) the end of the treatment (c) one month after the completion of TSEB procedure.
Fig. 4.
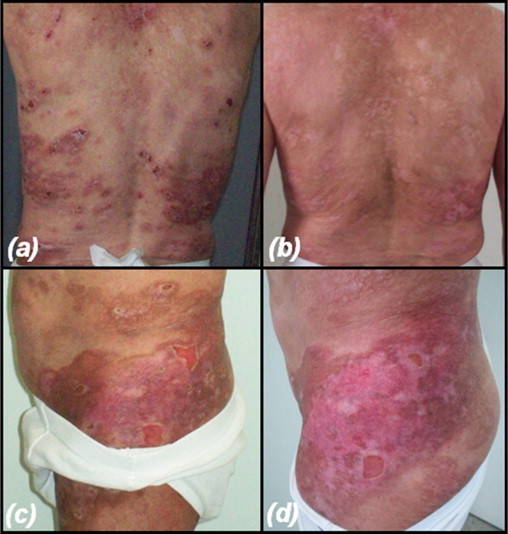
(a) Mycosis fungoides on the back of the patient (4th week of treatment). (b) Complete regression of the disease on the back one month after the end of the treatment. (c) Region that resisted treatment (end of TSEB irradiation procedure). (d) Residual disease, 1 month after the completion of irradiations.
One month later, the face of the patient remained erythematic and the loss of fingernails was observed. Moreover, the patient reported lacrimation. The disease in the treatment-resisting area of the left loin did not regress, while the rest of the skin responded positively in total to radiation. The problematical area, related to underdosed lesions (<90% of prescribed dose) was re-irradiated with one additional session of 600 cGy, delivered by regional electron boost fields of 6 MeV.
After the initiation of TSEB therapy, he gradually showed improvement in ulceration and reduction of tumors and at the end of the 36 sessions of treatment had a CCR which means a complete disappearance of his lesions. Four months later, he was otherwise well with only a few new small pruritic nodules on his arms mimicking prurigo nodularis, which histologically were consistent with MF. These lesions are currently treated with topical steroids. He is feeling well and fit. According to the patient, this is the best result comparing to any previous treatment. However, one year post TSEB treatment he had a bigger relapse and was restarted on IFNa until today.
5. Conclusion
This is an interesting case of tumor stage MF (T3-IIB) which had been refractory to all medical treatments including combination treatment, showed progression despite treatment (T2 to T3) and was an absolute indication for full dose of 36 Gy of TSEB therapy.
Conflict of interest
No conflict of interest, financial or other, exists.
Financial disclosure
None declared.
References
- 1.Keehn C.A., Belongie I.P., Shistik G., Fenske N.A., Glass L.F. The diagnosis, staging, and treatment options for mycosis fungoides. Cancer Control. 2007;14:102–111. doi: 10.1177/107327480701400203. [DOI] [PubMed] [Google Scholar]
- 2.Jones G., Wilson L.D., Fox-Goguen L. Total skin electron beam radiotherapy for patients who have mycosis fungoides. Hematol Oncol Clin North Am. 2003;17:1421–1434. doi: 10.1016/s0889-8588(03)00108-4. [DOI] [PubMed] [Google Scholar]
- 3.Karzmack C. 1987. Total skin electron therapy: technique and dosimetry. Report No. 23. [Google Scholar]
- 4.Pope E., Weitzman S., Ngan B. Mycosis fungoides in the pediatric population: report from an international Childhood Registry of Cutaneous Lymphoma. J Cutan Med Surg. 2010;14(Jan-Feb (1)):1–6. doi: 10.2310/7750.2009.08091. [DOI] [PubMed] [Google Scholar]
- 5.Marinello G., Jaffre F., Ślosarek K., le Bourgeois J.P. Total skin electron irradiation. Rep Prac Oncol Radiother. 1998;3(1):19–22. [Google Scholar]
- 6.Piotrowski T. The rotary-dual technique of the total skin electron irradiation. Rep Prac Oncol Radiother. 2004;9(S2) 239-239. [Google Scholar]
- 7.Piotrowski T., Malicki J. The rotary dual technique for total skin irradiation in the treatment of mycosis fungoides – a description of the applied method. Rep Prac Oncol Radiother. 2006;11(1):29–37. [Google Scholar]
- 8.Diamantopoulos S., Platoni K., Dilvoi M. Clinical implementation of total skin electron beam (TSEB) therapy: a review of the relevant literature. Phys Med. 2011;27(April (2)):62–68. doi: 10.1016/j.ejmp.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 9.Stevens S.R., Ke M.S., Parry E.J., Mark J., Cooper K.D. Quantifying skin disease burden in mycosis fungoides-type cutaneous T-cell lymphomas: the severity-weighted assessment tool (SWAT) Arch Dermatol. 2002;138(January (1)):42–48. doi: 10.1001/archderm.138.1.42. [DOI] [PubMed] [Google Scholar]
- 10.Olsen E., Vonderheid E., Pimpinelli N. ISCL/EORTC Revisions to the staging and classification of mycosis fungoides and Sezary syndrome: a proposal of the International Society for Cutaneous Lymphomas (ISCL) and the cutaneous lymphoma task force of the European Organization of Research and Treatment of Cancer (EORTC) Blood. 2007;110(September (6)):1713–1722. doi: 10.1182/blood-2007-03-055749. [DOI] [PubMed] [Google Scholar]
- 11.ICRU. International Commission on Radiation Units and Measurements. Prescribing, recording, and reporting electron beam therapy. ICRU Report 71, J ICRU 2004; 4(1).
- 12.Platoni K., Diamantopoulos S., Panayiotakis G. First application of total skin electron beam irradiation in Greece: setup, measurements and dosimetry. Phys Med. 2011 doi: 10.1016/j.ejmp.2011.03.007. Apr 22. [DOI] [PubMed] [Google Scholar]
- 13.Quiros P.A., Kacinski B.M., Wilson L.D. Extent of skin involvement as a prognostic indicator of disease free and overall survival of patients with T3 cutaneous T-cell lymphoma treated with total skin electron beam radiation therapy. Cancer. 1996;77(May (9)):1912–1917. doi: 10.1002/(SICI)1097-0142(19960501)77:9<1912::AID-CNCR23>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 14.Kamstrup M.R., Lindahl L.M., Gniadecki R., Iversen L., Skov L., Petersen L.M. Low-dose total skin electron beam therapy as a debulking agent for cutaneous T-cell lymphoma: an open-label prospective phase II study. British Journal of Dermatology. 2012;166(January (2)):399–404. doi: 10.1111/j.1365-2133.2011.10670.x. [DOI] [PubMed] [Google Scholar]


