Abstract
Aim
A literature review was undertaken to identify current TSEB therapy in pediatric patients.
Background
Total skin electron beam (TSEB) therapy is a method of irradiation with low energy electron beam dedicated to patients who have superficial skin lesions all over their body. Such skin malignancies are sparse among adults and even more uncommon with pediatric population.
Materials and methods
In this study, all reported case reports were summed up with a special emphasis on techniques used, doses prescribed and special shielding of critical organs. Moreover, potential problems that were encountered during TSEB irradiation of very young patients were depicted.
Results
The literature has described only seven case reports of children undergoing TSEB therapy. Most of them were infants; however, two adolescents were also treated. For all infants, general anesthesia was provided to allow safe and accurate TSEB irradiation. The prescribed dose varied from 16 Gy to 28 Gy depending on the irradiation schedule and patient condition. Usually, boost fields were applied to the scalp and perineum. Typical shields for fingernails, toenails and lenses were usually used.
Conclusion
This paper revealed that TSEB therapy may be considered as a palliative treatment for pediatric patients with leukemia cutis. However, its role is still unclear and should be further investigated.
Keywords: Pediatric total skin electron beam therapy, TSEB, Leukemia cutis
1. Background
The idea of total skin electron beam (TSEB) therapy is to deliver a prescribed dose only to the patient's skin and to protect as much as possible healthy tissues inside the body. Electron beams of energy range 3–7 MeV are preferred for such task1,2 due to their depth dose distribution which is characterized by a rapid fall off after reaching its “peak” at a shallow depth. This technique has been used for adults for many years to treat rare skin diseases such as mycosis fungoides, Sezary syndrome or Kaposi sarcoma3–8; however, it is uncommon in the pediatric population. Many various techniques of TSEB therapy for adults have been described in the literature1,9–13 and lately two large reviews of all current techniques have been published by Diamantopoulos et al.14 and Piotrowski et al.15
TSEB therapy is also used to treat pediatric patients with leukemia cutis (LC). LC, also called a cutaneous granulocytic sarcoma, is a term for an extramedullary leukemia where malignant leukocytes infiltrate into the skin16. The disease manifests with widespread bluish purple papules, nodules or plaques17. They may be different in size and appear on patient's face, legs, arms and trunk18,19. LC is a very rare disease and usually associated with poor prognosis20. It can occur before or after establishment of systemic leukemia and is more common in children than adults16.
Literature on TSEB for pediatric patients is very limited and mostly described in brief case reports20–24. The first such description for a pediatric patient with LC was made by Rubin et al.21 in 1985. Then in 1995, a detailed paper was published by Earley et al.22 where the whole TSEB procedure for infants was depicted. In 2007, two more case reports were presented by Pepek et al.23 Lately, Bao et al.24 provided a report for a commissioning and quality assurance method of implementing TSEB therapy to a sedated infant, and Majd et al.20 provided another case report on LC treated with TSEB therapy. Although new technologies have revolutionized the field of radiation oncology,25–28 the TSEB irradiation of children has not changed so much since 1985.
1.1. Aim
The purpose of this study is to summarize the techniques applied in TSEB therapy for pediatric patients with LC and to report about common methods as well as potential problems of such therapy and how they have been solved in the literature.
2. Patients
To the best of my knowledge, only seven pediatric patients treated with TSEB have been reported in the literature. Most of them were infants (median age 14 months, range 12–17 months) and two patients were 13 and 18 years old. Among this group, there were three males and two females. The sex of two patients was not reported. The disease manifested with raised, violaceous nodules on the scalp, face, arms and back. Skin biopsy was done in all cases, LC was confirmed and TSEB treatment offered.
3. Techniques of irradiation
TSEB therapy has a long history in treating skin diseases. There are three main techniques of TSEB irradiation that have been well described in the literature.29,30 Apart from them, there are many modified techniques that are combinations of the above mentioned ones. All modified techniques are well summarized in the paper by Diamantopoulos et al.14
For children, the most popular TSEB was a modified Stanford technique which was applied in four out of seven patients. In a paper presented by Pepek et al.,23 a rotational TSEB technique was used, while Rubin et al.21 used a multiple-field pendulum-arc technique. In the two cases described by Pepek et al.,23 utilizing a rotational technique was possible as the patients were 13 and 18 years old. Thus, it was possible for them to stand on a spinning platform during irradiation with electrons. The rest of the patients were infants that were not able to stand on their own during the treatment. For this reason, some children20,21,24 were placed in a custom-made harness which was attached to a special frame. Arm positions were secured with velcro strips and tape. Earley et al.22 proposed infants to be irradiated in a lying position. The patient was positioned on a Plexiglas platform that was used for lifting and moving. For anterior and posterior fields, the child was irradiated lying on the floor with gantry angle set at 0°. For oblique fields it was lying on a table with gantry angle set at 60°. Arms and legs were adjusted appropriately for each field. The source-skin distance (SSD) was set to 200 cm. Fig. 1 provides a schematic picture of most popular TSEB techniques for children. To allow safe and accurate TSEB irradiation for all infants, general anesthesia was provided.
Fig. 1.
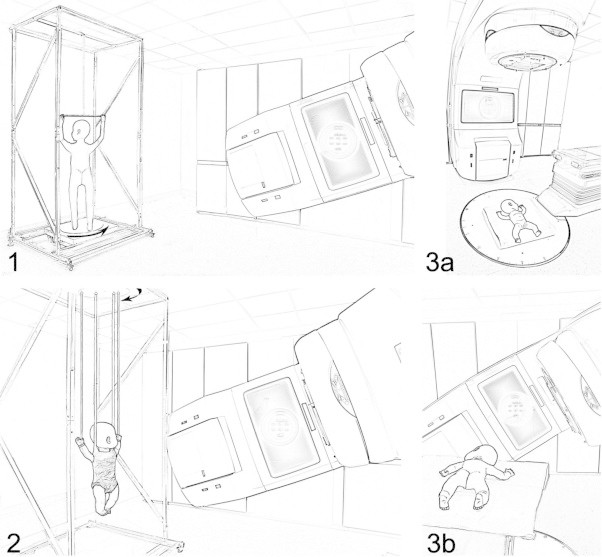
The most popular patient positioning for total skin electron beam therapy for children: (1) rotational technique – possible only for children who can stand on their own; (2) modified Stanford technique in vertical position – the infant was placed in a custom made harness attached to a special frame; (3) modified Stanford technique in horizontal position: (3a) treatment of the anterior and posterior fields – the gantry is set at 0° (3b) treatment of the oblique fields – the gantry is rotated 60° off vertical. For (2) and (3) arms were positioned to match the standard positioning.
4. Dose prescription
TSEB therapy for children was planned mostly with 6 MeV; however, Rubin et al.21 used 8 MeV degraded electron fields. The prescription doses varied from 16 Gy to 28 Gy. The irradiation schedule differed across radiotherapy centers and patient conditions (Table 1).
Table 1.
Published case series of TSEB therapy for pediatric patients.
| References | Age | Sex | Total dose [Gy] | Fractionation | Local boost |
|---|---|---|---|---|---|
| Rubin et al. [21] | 13 months | Female | 19 | 1.12 Gy/fx | 12 Gy to perineun (3 Gy/fx) |
| Earley et al. [22] | 14 months | Male | 28 | 2 Gy/fx (2 treatments per week) | Not reported |
| Pepek et al. [23] | 13 years | Male | 16 | 2 Gy/fx (3 treatments per week) | 6 Gy to scalp (2 Gy/fx) |
| 18 years | Male | 18 | None | ||
| Bao et al. [24] | 17 months | Not reported | 16 | 2 Gy/cyclea (2 days per cyclea) | None |
| 12 months | 16 | To scalp (dose not reported) | |||
| Majd et al. [20] | 15 months | Female | 16 | To perineum and plantar surfaces (dose not reported) |
Each cycle consists of 2 treatment days with 3 dual fields each.
Additional boost fields were added to irradiate areas that received low doses from a normal TSEB treatment. Usually, boost fields were applied to the scalp and perineum. A boost dose can be assessed based on the underdosage of each region during a main TSEB treatment. Only in one case,24 a bolus of 1 cm was used to boost the top of the head with 6 MeV electron beam energy. In the other case reports, no bolus was used during the treatment.
5. Shields
During TSEB therapy for children, some parts of the body should be shielded. This applies mostly to finger tips and toes since those areas are very thin and can experience much higher dose than the rest of the skin. Another organ that may be shielded during TSEB therapy are lenses since they are very sensitive to radiation dose. Depending on the degree of skin involvement, shields are included throughout or during part of the treatment course.
Pepek et al.23 reported that eye shields were used for both patients throughout the treatment. Fingernails as well as toenails were also covered during the whole TSEB therapy for one of the patients (the younger one). The other patient received shielding of the nails after 12 Gy. Majd et al.20 used only shields for fingernails. An interesting shielding was provided by Earley et al.22 Beside external eye shields, special wax compensators around hands and feet were attached with lead shields for nail beds. Since the volume of infant's hand and foot is very small, the danger of overdosage to those areas is highly probable. For this reason, extra wax was added until the fist and foot had diameters of at least 5 cm. The authors showed that this is the minimum thickness that should be provided to prevent high doses.
6. Potential problems
TSEB therapy for children can be administered without problems to adolescents as described by Pepek et al.,23 because the patient can stand on their own and cooperate with the radiotherapy staff. The problem begins when a very young pediatric patient has to be irradiated. The most difficult part was to set up an infant for the time of treatment. In all cases where infants underwent TSEB therapy, the staff decided that anesthesia was necessary for proper immobilization. Due to this fact, the vital signs of the patient had to be monitored; however, the staff should always remember that such equipment should not shield the skin of the patient. To smear out the shielding effect of blood pressure cuff, it should be placed in different positions during the course of treatment.24
The infants were mostly irradiated in a custom made harness attached to a specially constructed frame.20,21,24 As a result, the child was suspended above the floor and its trunk was rotated from above when necessary with arms positioned using velcro strips and tape as in the Stanford technique. In this setup, the harness covers the whole trunk and should be made from a fabric that does not attenuate the electron beam while being able to support the child. This problem does not exist when an infant is irradiated in a lying position as described by Earley et al.22 In such case, the patient is naked, so, to maintain the body's temperature, a heat lamp should be present (outside the treatment field).
TSEB therapy in the case of infants brings also the problem of overdosage in very small volumes such as fingers and toes. Earley et al.22 measured dose uniformity with thermoluminescent dosimeters (TLDs) and specially designed phantoms of different sizes, their diameters ranging from 1 cm to 7.5 cm. The results showed that the dose to the smallest phantom was approximately 4 times higher than that delivered to the skin of the trunk. The overdosage of small body parts can cause a bone growth disorder resulting in structural asymmetry. As a result, they suggested that any body part that is smaller than 5 cm in diameter should be compensated with wax.
7. Toxicity
TSEB therapy was always well tolerated by the patients. However, some mild skin toxicity appeared – it consisted of hyperpigmentation, dryness and minimal erythema. Only for one case, desquamation was reported.21 Pepek et al.23 noted that one of the patients developed grade 2 oral mucositis. Moreover, a mild fatigue could often be observed during the treatment.
8. Results of the treatment
In most publications regarding TSEB therapy for children, a significant improvement in skin lesions was noticed.20–23 Rubin et al.21 reported that all skin nodules disappeared and 12 months after the treatment the child remained in complete remission. Earley et al.22 noted that 3 months after TSEB therapy the skin remained free of disease and healthy in appearance. However, the child relapsed of his initial disease so the prognosis was poor. Significant improvement of the skin lesions after TSEB treatment was also reported by Pepek et al.23 Both patients did not develop any skin recurrence after 4 and 19.5 months after TSEB therapy, respectively, before dying due to complications of sepsis. A relapse of initial disease during the course of treatment was noted by Majd et al.20 Although, radiation therapy improved skin lesions, the infant died due to leukemia progression.
9. Conclusions
All case reports mentioned that improvement of patient's skin lesions and nodules could be observed after TSEB therapy. Unfortunately, most of these patients died from sepsis after bone marrow transplant or due to the relapse of the initial disease in the bone marrow. However, based on the published case reports, one may assume that TSEB therapy might be used as a palliative treatment of young patients with LC.
Further data are needed to verify if TSEB therapy affects overall survival for pediatric patients. Moreover, before such treatment, one has to consider the long-term toxicity since tolerance for irradiation of total skin in very young patients is still unknown.
Conflict of interest
All authors have no actual or potential conflict of interest including any financial, personal or other relationships with other people or organizations within three years of beginning the submitted work that could inappropriately influence, or be perceived to influence, their work.
Financial disclosure statements
None declared.
References
- 1.Piotrowski T., Malicki J. The rotary dual technique for total skin irradiation in the treatment of mycosis fungoides – a description of the applied method. Rep Pract Oncol Radiother. 2006;11(1):29–37. [Google Scholar]
- 2.Piotrowski T., Fundowicz D., Pawlaczyk M., Malicki J. Thermoluminescent dosimetry in rotary-dual technique of the total skin electron irradiation. Neoplasma. 2003;50(2):41–46. [PubMed] [Google Scholar]
- 3.Jones G.W., Rosenthal D., Wilson L.D. Total skin electron radiation for patients with erythrodermic cutaneous T-cell lymphoma (mycosis fungoides and the Sezary syndrome) Cancer. 1999;85(9):1985–1995. doi: 10.1002/(sici)1097-0142(19990501)85:9<1985::aid-cncr16>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 4.Jones G., Wilson L.D., Fox-Goguen L. Total skin electron beam radiotherapy for patients who have mycosis fungoides. Hematol Oncol Clin North Am. 2003;17:1421–1434. doi: 10.1016/s0889-8588(03)00108-4. [DOI] [PubMed] [Google Scholar]
- 5.Funk A., Hensley F., Krempien R., Neuhof D., Van Kampen M., Treiber M. Palliative total skin electron beam therapy (TSEBT) for advanced cutaneous T-cell lymphoma. Eur J Dermatol. 2008;18(3):308–312. doi: 10.1684/ejd.2008.0394. [DOI] [PubMed] [Google Scholar]
- 6.Nisce L.Z., Safai B., Poussin-Rosillo H. Once weekly total and subtotal skin electron beam therapy for Kaposi's sarcoma. Cancer. 1981;47:640–644. doi: 10.1002/1097-0142(19810215)47:4<640::aid-cncr2820470403>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 7.Batycka-Baran A., Reich A., Jankowska-Konsur A., Maj J. Nowe trendy w leczeniu ziarniniaka grzybiastego i zespołu Sezary’ego. Post Dermatol Alergol. 2009;1:41–55. [Google Scholar]
- 8.Grzanka A., Placek W. Współczesna diagnostyka skórnych chłoniaków T-komórkowych. Post Dermatol Alergol. 2004;5:220–225. [Google Scholar]
- 9.Karzmark C.J. Large-field superficial electron therapy with linear accelerators. Br J Radiol. 1964;37:302–305. doi: 10.1259/0007-1285-37-436-302. [DOI] [PubMed] [Google Scholar]
- 10.Podgorsak E.B., Pla C., Pla M., Lefebvre P.Y., Heese R. Physical aspects of a rotational total skin electron irradiation. Med Phys. 1983;10:159–168. doi: 10.1118/1.595296. [DOI] [PubMed] [Google Scholar]
- 11.Karzmark C.J., Anderson J., Fessenden P., Svensson G., Buffa A., Khan F.M., Wright K.A. Report of Task Group 30; 1987. Total skin electron therapy: technique and dosimetry. [Google Scholar]
- 12.Wu J.M., Leung S.W., Wang C.J., Chui C.S. Lying-on position of total skin electron therapy. Int J Radiat Oncol Biol Phys. 1997;39:521–528. doi: 10.1016/s0360-3016(97)00141-7. [DOI] [PubMed] [Google Scholar]
- 13.Wu J.M., Yeh S.A., Hsiao K.Y., Chao M.M., Hargrove I. A conceptual design of rotating board technique for delivering total skin electron therapy. Med Phys. 2010;37:1449–1458. doi: 10.1118/1.3315390. [DOI] [PubMed] [Google Scholar]
- 14.Diamantopoulos S., Platoni K., Dilvoi M. Clinical implementation of total skin electron beam (TSEB) therapy: a review of the relevant literature. Phys Med. 2011;27:62–68. doi: 10.1016/j.ejmp.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 15.Piotrowski T., Milecki P., Skórska M., Fundowicz D. Total skin electron irradiation techniques a review. Post Dermatol Alergol. 2013;1:50–55. doi: 10.5114/pdia.2013.33379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cho-Vega J.H., Medeiros L.J., Prieto V.G., Vega F. Leukemia cutis. Am J Clin Pathol. 2008;129:130–142. doi: 10.1309/WYACYWF6NGM3WBRT. [DOI] [PubMed] [Google Scholar]
- 17.Su W.P., Buechner S.A., Li C.Y. Clinicopathologic correlations in leukemia cutis. J Am Acad Dermatol. 1984;11:121–128. doi: 10.1016/s0190-9622(84)70145-9. [DOI] [PubMed] [Google Scholar]
- 18.Paydas S., Zorludemir S. Leukaemia cutis and leukaemic vasculitis. Br J Dermatol. 2000;143:773–779. doi: 10.1046/j.1365-2133.2000.03774.x. [DOI] [PubMed] [Google Scholar]
- 19.Longacre T.A., Smoller B.R. Leukemia cutis, Analysis of 50 biopsy-proven cases with an emphasis on occurrence in myelodysplastic syndromes. Am J Clin Pathol. 1993;100:276–284. doi: 10.1093/ajcp/100.3.276. [DOI] [PubMed] [Google Scholar]
- 20.Majd N.K., Jain S.K., Murphy M.C., Dugas J.P., Hager F., Abdulrahman R. Total skin electron beam radiation in a pediatric patient with leukemia cutis: a case report. J Pediatr Hematol Oncol. 2012;34(October (7)):556–558. doi: 10.1097/MPH.0b013e3182678e9f. [DOI] [PubMed] [Google Scholar]
- 21.Rubin C.M., Arthur D.C., Meyers G., McClain K.L., Kim T.H., Woods W.G. Leukemia cutis treated with total skin irradiation. Cancer. 1985;55:2649–2652. doi: 10.1002/1097-0142(19850601)55:11<2649::aid-cncr2820551120>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 22.Earley L., Moeller J., O’Rear J., Leavitt D.D. A method for total skin electron treatment for infants. Med Dosim. 1995;20(4):243–248. doi: 10.1016/0958-3947(95)02010-1. [DOI] [PubMed] [Google Scholar]
- 23.Pepek J.M., Paulino A.C., Briones M.A. Marcus RB Jr, Esiashvili N, Role of total skin electron beam therapy for leukemia cutis in pediatric patients. Pediatr Blood Cancer. 2008;50:1054–1055. doi: 10.1002/pbc.21390. [DOI] [PubMed] [Google Scholar]
- 24.Bao Q., Hrycushko B.A., Dugas P.J., Hager F.H., Solberg T.D. A technique for pediatric total skin electron irradiation. Radiat Oncol. 2012;7:40. doi: 10.1186/1748-717X-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Malicki J. The importance of accurate treatment planning: delivery, and dose verification. Rep Pract Oncol Radiother. 2012;17(2):63–65. doi: 10.1016/j.rpor.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Filippi A.R., Franco P., Ciammella P. Role of modern radiation therapy in early stage Hodgkin's lymphoma: A young radiation oncologists’ perspective. Rep Pract Oncol Radiother. 2012;17(5):246–250. doi: 10.1016/j.rpor.2012.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Syam Kumar S.A., Vivekanandan N., Sriram P. A study on conventional IMRT and RapidArc treatment planning techniques for head and neck cancers. Rep Pract Oncol Radiother. 2012;17(3):168–175. doi: 10.1016/j.rpor.2012.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Leszczyński W. Ślosarek K: Szlag M, Comparison of dose distribution in IMRT and RapidArc technique in prostate radiotherapy. Rep Pract Oncol Radiother. 2012;17(6):347–351. doi: 10.1016/j.rpor.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karzmack C.J. 1987. AAPM report No. 23, total skin electron therapy: technique and dosimetry, report of group 30 radiation therapy committee AAPM. [Google Scholar]
- 30.Podgorsak E.B. I.A.E. Agency; Vienna, Austria: 2003. Review of radiation oncology physics: a handbook for teachers and students. [Google Scholar]


