Abstract
The present study was aimed at documenting the detailed ethnomedicinal knowledge of an unexplored area of Pakistan. Semistructured interviews were taken with 55 informants randomly chosen regarding detailed ethnomedicinal and sociocultural information. The study exposed 67 medicinal plant species used to prepare 110 recipes and the major modes of herbal formulation were decoction and powdering (20% each). The disease categories with the highest Fic values were gastrointestinal and dermatological (0.87 each). The study determined 3 plant species, i.e., Acacia modesta Wall., Caralluma tuberculata R.Br., and Withania somnifera (L.) Dunal with a FL of 100%. DMR results showed that Olea ferruginea (Sol.) Steud. ranked first, Morus alba L. ranked second, and Melia azedarach L. ranked third. Among the 55 informants, the male concentration was high (61%) and most of them were over 40 years old while a leading quantity of respondents (45%) was uneducated. There is a dire need to take necessary steps for the conservation of important medicinal plants by inhibiting overgrazing and providing alternate fuel resources. Young generations should be educated regarding the importance of ethnomedicinal knowledge and plants with high Fic and FL values should be further checked chemically and pharmacologically for future exploration of modern medicine.
1. Introduction
Medicinal plants offer a real substitute in developing countries for the treatment of human and animal ailments [1]. Ethnomedicine is often the single easily reached and affordable therapy available. The world market for herbal medicines based on traditional knowledge is now estimated at US$ 60 billion [2]. Plant-based traditional medicine plays a key role in the development of novelties in drug discovery [3].
Pakistan has a rich medicinal plants history having more than 600 plants being used traditionally for medication [4]. The majority of the medicinal plants are confined to northwest regions of Pakistan due to the presence of Himalayas, Karakoram, Sulaiman, and Hindu Kush mountain ranges [5] that lie in association with Pak-Afghan border. Both countries Pakistan and Afghanistan share almost 2,500 kilometers of boundary, called Durand Line, which was demarcated in 1893 following an agreement between the British Empire and the Afghan king [6]. The Durand Line separates Pashtun ethnic group in the Pak-Afghan border areas. Culturally, Pashtuns represent the majority of the populace of Afghanistan and also have significant population in Pakistan. The local language of southeastern Afghanistan and northwestern Pakistan Pashtun ethnic group is Pashtu [7]. The majority of the northwest areas of Pakistan living in the proximity to border region are rural in nature with high illiteracy rate and greatly depend on medicinal plants for primary health care and for generating income. In Pakistan, various ethnobotanical studies have been conducted in the different regions [8, 9] (Akhtar et al. [9]; Mussarat et al. [10], Hassan et al. [11]; and Begum et al. [12]). Most of the ethnobotanical studies in Pakistan have documented just the uses of medicinal plants. Almost no studies have been documented on detailed ethnomedicines preparations in the border region villages. The current research is the first effort to provide a thorough overview on the ethnomedicines employed by conventional healers and their detailed appliance in the region. This research will offer baseline data for more comprehensive studies on effectiveness and security of these preparations, as well as the potential applications in the communal health system. Moreover, the region is very rich in medicinal plants due to its conductive climate but this area has never been touched so far. Therefore, it is imperative to document the vegetation and detailed home-grown information of people about medicinal plants of this area before it is lost due to changing cultures. The purpose of this study is to assess traditional medicinal plant knowledge specifically with regard to the traditional healer's demographic characteristics such as gender, age, and source of income and to document the knowledge and the uses of medicinal plants used by the traditional healers in the Hangu region, Pakistan, to provide baseline data for future pharmacological and phytochemical studies by the application of ethnobotanical indices.
2. Material and Methods
2.1. Study Area
The present study was conducted in Hangu district located in north of Khyber Pakhtunkhwa, Pakistan, near the border region with Afghanistan (Figure 1). Hangu is situated at 33.53 North latitude, 71.06 East longitude, and 858 m above the sea level comprising a total area of 1,097 km2 and total population of 314,529 [13]. The dominant vegetation in the study area is Acacia modesta, Olea ferruginea, Dodonaea viscosa (L.) Jacquin, Acacia nilotica L., Periploca aphylla Decne., Melia azedarach, and Morus alba. The temperature of the area rises gradually from the month of January to June and then slowly turns down up to December. The summer season is modest and warm but June and July are the hottest months. The mean highest temperature is 8.8°C and mean lowest temperature is 7°C in the months of December and January. This district also produces wheat and maize as major crops. The area is rural in nature and the majority of the population is illiterate and they are also deprived of modern health services; hence the locals rely on medicinal flora of the region for the healthcare and to balance their low earnings as well [14]. The inhabitants mostly rely on timber for fuel purposes due to lack of modern fuel resources [13].
Figure 1.
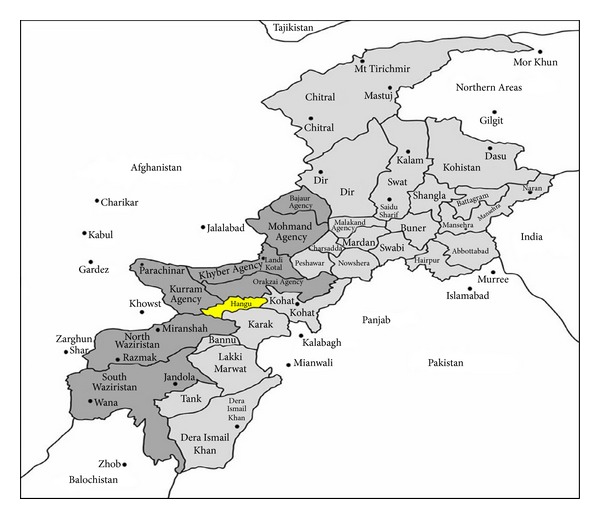
Map of the study area.
2.2. Data Collection
Field work was carried out from October 2012 to October 2013. Data was collected by making total eight frequent visits to the study area in four different seasons. Total 250 informants were recommended by knowledgeable elders, local authorities, and development agents. Out of 250, we have randomly selected 55 (34 men and 21 women) out of the total identified key informants. The selected informers were local inhabitants of the area aged between 20 and 89 years. Ethnobotanical survey was taken to gather information on traditional plants utilized by the local healers for the treatment of human ailments in the district following standard methods [15, 16]. The survey was done by using proper semistructured interviews and group discussions as well. A checklist of questions was prepared in English language for undertaking interviews and discussions. The questionnaire contained no strict questions and informants were allowed to speak spontaneously and without pressure. Key questions about medicinal plants were on local name of a particular medicinal plant, types of disease treated, mode and method of remedy preparation, parts of the plants used, use of fresh or dry plant parts, use of single or mixture of plants for remedy preparation, mode of administration, and dose requirement. Sociocultural information about informants was also collected during interview. The informants were interviewed in their local language Pashto. Ethically written acceptance was collected from the main office of the district and also from the head person of the village. The purpose of the present study was also explained to each informant in order to remove their hesitation and to encourage them that their knowledge will be a great contribution in the scientific literature.
2.3. Specimen Collection and Identification
The reported medicinal plants were collected from natural vegetation and home gardens during the field walks and habits of the plants were listed. The collected voucher specimens were taken to the Herbarium of Kohat University of Science and Technology, Kohat, Pakistan. Specimen identification and confirmation were undertaken by using Flora of Pakistan and taxonomic experts. Specimens with their label were stored at the Herbarium of Kohat University of Science and Technology, Kohat, Pakistan.
2.4. Data Organization
The collected ethnobotanical data were entered into Excel spreadsheet 2007 and summarized using graphical statistical methods such as percentages. The habit of the plants was categorized into three categories, that is, herbs, shrubs, and trees. The part used by the healers for the preparation of ethnomedicines was grouped under 11 classes, that is, leaves, whole plant, root, fruit, bark, and so forth. Human ailments treated in the study area were categorized into 18 categories like gastrointestinal, dermatological, skeletomuscular, antidiabetic, and so forth. Route of administration was divided into oral, dermal, and nasal. The basic categorization using questionnaire data regarding informants' sex, age groups, educational status or literacy rate, and occupation was also carried out.
3. Data Analyses
3.1. Informant Consensus Factor (Fic)
For the analysis of the general use of plants, factor informant consensus (Fic) was used to highlight plants of particular cultural relevance and agreement in the use of plants. Informants' consensus within a community and between cultural groups indicates which plants are widely used and thus aids in the selection of plants for pharmacological and phytochemical studies [17]. In order to use this tool, illnesses were classified into categories, as plants with high Fic are likely to be more pharmacologically efficient as compared to plants with low Fic [18]. Fic values lie between “0.00 and 1.00”. Fic values are always greater when single or few plants are documented to be used by large number of respondents to cure a specific disease, while low Fic values give an indication that informants do not agree over which plant to use [19, 20].
The Fic can be calculated using the formula as follows:
| (1) |
where Fic = informants consensus factor, nur = number of use citation in each category, and nt = number of species used.
3.2. Fidelity Level (FL)
Fidelity level is useful for identifying the key informants' most preferred species used for treating certain ailments. The medicinal plants that are widely used by the local people have higher FL values than those that are less popular. Fidelity level shows the percentage of informants claiming the use of a certain plant species for the same major purpose. This is designed to quantify the importance of the species for a given purpose. Before calculating the values of FL all of the ailments that were reported are grouped into major classes [21]. FL value was estimated using the formula FL = Ip/Iu × 100, where Ip is the number of respondents who reported the utilization of medicinal plants for a specific main ailment and Iu is the total number of respondents who mentioned the same plant for any ailment [22]. It is assumed that those medicinal plants which are plants that are used in some recurring manner for the same disease category are more likely to be biologically active [18].
3.3. Direct Matrix Ranking (DMR)
DMR [15, 16] was used to compare the use diversity of given plant species based on the data collected from the respondents. Total eight informants were selected for the collection of DMR data. Selected informants were asked to assign use values (5 = best, 4 = very good, 3 = good, 2 = less used, 1 = least used, and 0 = not used) to each species. The values (average scores) given to each medicinal plant were summed up and ranked.
4. Result and Discussion
4.1. Medicinal Plants Reported
The study revealed 67 medicinal plant species belonging to 55 genera and 39 families consisting of 65 angiosperms and 2 gymnosperms in Hangu district (Table 1). The investigated region has a rich diversity of medicinal plants and provides a conductive habitat and ideal climatic conditions for their growth as shown by the presence of 67 medicinal plant species. The majority of the medicinal plants reported were herbs (43%) followed by shrubs (30%) and trees (27%). The high usage of herbs in the study area could be an indication of their abundance and it might also be due to the fact that they are easily accessible near household and might have high effectiveness in the treatment of ailments in comparison to other growth forms [23]. The common use of herbs for medicinal purposes is also reported from other parts of the world [24, 25]. The dominant families in the study area were Asteraceae and Solanaceae represented by the highest number of species (4 species each, 6%) followed by Euphorbiaceae, Moraceae, Oleaceae, and Lamiaceae (3 species each, 4.47%). Other families with low number represented by 2 species each Amaranthaceae, Acanthaceae, Alliaceae, Poaceae, Papilionaceae, Zygophyllaceae, Arecaceae, and Rhamnaceae, while the remaining 22 families had only single species representation. The wider utilization of species from dominant families like Asteraceae and Solanaceae might relate to the presence of effective bioactive ingredients against ailments [26]. Our results are in line with other ethnomedicinal studies conducted in other regions of Pakistan [9, 27] where traditional healers mostly use Solanaceae and Asteraceae members for the preparation of ethnomedicines.
Table 1.
Medicinal plants and their preparation methods and administration.
| Scientific names | Local names | Families | Habit | Part used | Medicinal uses | Herbal formulation | Administration | Dosage |
|---|---|---|---|---|---|---|---|---|
| Acacia modesta Wall. | Palosa | Mimosaceae | Tree | Gum, leaves | Backache | Gum and powder of fresh leaves of Acacia modesta are mixed with wheat flour and desi ghee and make Halwa that is used for backache. | Oral | As needed |
|
| ||||||||
| Acacia nilotica (L.) Delile | Kikar | Mimosaceae | Tree | Whole plant | Narcotic | Extraction of fresh root and leaves are taken as alcohol (Sharab). | Oral | As needed |
| Aphrodisiac | Four grams of gum is taken as paste with water. | Oral | Once a day | |||||
| Earache | About 30 flowers are heated in 10 mL mustard oil and filtered. | Through ear | Two to four drops for 5 days | |||||
|
| ||||||||
| Allium cepa L. | Pyaaz | Alliaceae | Herb | Leaves | Antipyretic | Equal amount of extract of onion bulb and mint are mixed and used against cholera. | Oral | One teaspoon of this mixture is taken per hour for a period as needed. |
| Skin infection | Poultice of onion bulb is used against abscesses. | Topical | Two times a day for one week | |||||
|
| ||||||||
| Allium sativum Linn. | Ugga | Alliaceae | Herb | Leaves, roots | Blood disorders | Small pieces of Allium sativum are chewed to reduce blood pressure. | Oral | Twice a day |
| Gastrointestinal | The powder of leaves and roots are also used against stomach problems. | Oral | As needed | |||||
|
| ||||||||
| Aloe barbadensis Mill. | Zarpati | Aloeaceae | Herb | Leaves | Veterinary (gastrointestinal) | Two leaves are made spineless and each one is divided lengthwise into 2 or 3 slices. These slices of leaves along with common salt are given to the animals for stomach disorders. | Oral | Three doses after every 48 hours period |
|
| ||||||||
| Amaranthus viridis L. | Sarkoomal. | Amaranthaceae | Herb | Leaves | Gastrointestinal | Leaves are crushed with sugar and taken along with black tea for curing constipation. | Oral | Four times a day |
| Skin infection | Poultice of leaf is prepared along with mustard oil for the treatment of abscesses. | Topical | As needed | |||||
|
| ||||||||
| Anagallis arvensis L. | Dhabbar | Primulaceae | Herb | Whole plant | Rheumatism | The whole plant is crushed into powder after drying. Two gm of the powder with 5 gm of wheat flour is mixed for the treatment of rheumatism. | Oral | Once a day for a week |
|
| ||||||||
| Cannabis sativa L. | Bhaang | Cannabaceae | Herb | Leaves, flowering tops, and seed | Narcotic | The fruit and leaves are used as narcotic, commonly called “Charas.” | Oral | As needed |
| Veterinary | The decoction of seeds is given to cattle for increasing milk. | Oral | As needed | |||||
|
| ||||||||
| Caralluma tuberculata R.Br | Pawany | Asclepiadaceae | Shrub | Whole plant | Antidiabetic and anticancer | Whole plant is dried, powdered, and taken with water. Fresh plant is directly eaten by diabetic patient and is very effective in cancer treatment as well. | Oral | Once a day |
|
| ||||||||
| Cuscuta reflexa Roxb. | Chum bud | Cuscutaceae. | Herb | Stem and seeds | Wound | A paste of the plant powder in butter is prepared and is externally applied for wounds. | Topical | As needed |
| Skin infection | The whole plant is crushed and then boiled in 8 liters of water for an hour. It is filtered and the patient is advised to take a bath with this decoction without using soap for scabies. | Topical | As needed | |||||
|
| ||||||||
| Carthamus oxycantha Co.Cr. | Spena zagai | Asteraceae | Herb | Seed oil | Jaundice | Seeds are collected, dried under shade, and ground to obtain powder and taken to treat jaundice. | Oral | 1 teaspoon of powder is taken twice a day for 3-4 weeks |
| Skin infection | Few drops of honey are added in seed powder to make paste. This paste is applied on the face. It is effective to remove white spots of skin. | Topical | As needed | |||||
|
| ||||||||
| Citrus sinensis | Malta | Rutaceae | Shrub | Fruit, leaves | Gastrointestinal | Fruit is eaten for reducing constipation. | Oral | 2 fruits per day |
|
| ||||||||
|
Cynodon dactylonvar. coursii (A. Camus) J.R. Harlan and de Wet |
Wakha | Poaceae | Herb | Whole plant | Wounds | The paste made of fresh leaves is applied on cuts and bleeding wounds. | Topical | As needed |
| Piles | Same as above | Topical | As needed | |||||
| Gastrointestinal | Juice of the plant is given in diarrhea. | Oral | Twice a day | |||||
| Antipyretic | Same as above | Oral | Twice a day | |||||
|
| ||||||||
| Dalbergia sissoo DC. | Shawa | Papilionaceae | Tree | Whole plant | Piles | 70 gm of young leaves of buds are crushed. One glass of water is added to it and strained. The strained decoction is taken daily. | Oral | Taken daily for 10 days |
| Jaundice | Same as above | Oral | Taken daily for 10 days | |||||
|
| ||||||||
| Datura stramonium L. | Tora torii. | Solanaceae | Herb | Whole plant | Earache | The juice of flower is useful for earache. | Oral | As needed |
| Narcotic | Seeds and leaves are smoked for their narcotic action. | Oral | As needed | |||||
|
| ||||||||
| Dicliptera bupleuroides Nees. | Somni | Acanthaceae | Herb | Whole plant | Skin infection | Poultice is used for scabies. | Topical | Once a day |
|
| ||||||||
| Digera muricata (L.) Mart. | Tandola | Amaranthaceae | Herb | Whole plant | Gastrointestinal | Juice is extracted from the whole plants and used as laxative. | Oral | As needed |
|
| ||||||||
| Dodonaea viscosa (L.) Jacquin | Zetawoni | Sapindaceae | Shrub | Leaves | Rheumatism | The leaves are warmed and kept on joints to relieve pains. | Topical | Once a day |
|
| ||||||||
| Eriobotrya japanica (Thunb.) Lindl. | Lokat | Rosaceae | Tree | Fruit | Chest problems | Fruit is taken directly to treat cough. | Oral | As needed |
|
| ||||||||
| Eucalyptus lanceolatus Dehnh. | Lachi | Myrtaceae | Tree | Whole plant | Gastrointestinal | Leaves and bark are boiled in water. Filtrate and decoction are used for abdominal pains. Fruit is added to green tea and taken as antiemetic. | Oral | Twice a day |
|
| ||||||||
| Euphorbia helioscopia L. | Katta saarai | Euphorbiaceae | Herb | Leaves | Gastrointestinal | Mature leaves (5 g) are mixed with 3 spoonfuls of sugar to prepare recipe to treat constipation | Oral | Twice a day |
|
| ||||||||
| Euphorbia hirta L. | Chapa tray. | Euphorbiaceae | Herb | Whole plant | Diabetes | Leaves juice is taken for diabetes | Oral | As needed |
|
| ||||||||
| Fagonia indica Burm.f. | Mazgha Kai. | Zygophyllaceae. | Herb | Aerial parts | Blood purifier | Extract of aerial parts is used | Oral | Thrice a day |
| Skin infection | Same as above | Topical | Thrice a day | |||||
| Diabetes | Same as above | Oral | Thrice a day | |||||
| Antipyretic | Half kg of the whole plant is boiled in 2 liters of water; patients with hepatitis are advised to take bath with this decoction. | Topical | Thrice a day | |||||
|
| ||||||||
| Ficus carica L. | Inzeer | Moraceae | Tree | Fruit | Piles | Two to four fruits are soaked in water or milk at night and used in the morning on empty stomach. | Oral | Daily for 10 days |
|
| ||||||||
| Ficus elastica Roxb. ex Hornem. | Rubber Plant | Moraceae | Tree | Leaves, Bark | Antipyretic | Leaves and bark are crushed and taken along honey in small quantity to reduce fever. | Oral | Once a day |
|
| ||||||||
| Ficus religiosa L. | Peppal | Moraceae | Tree | Whole plant | Vomiting | Decoction of bark is used. | Oral | As needed |
|
| ||||||||
| Foeniculum vulgare Mill. | Soonphf | Umbelliferae | Herb | Seeds and roots | Gastrointestinal | Take sonf with white zeera, grind it, and use after meal; it is good to remove ulcer and stomach pain | Oral | As needed |
|
| ||||||||
| Fumaria indica (Hausskn.) Pugsley | Khatee soii. | Fumariaceae | Herb | Aerial parts | Blood purification | Two kg of aerial parts is dried under shade and crushed to obtain powder; 2-3 gm powder with one glass of water is taken. | Oral | Twice a day for one week |
| Jaundice | Same as above | Oral | Twice a day for one week | |||||
| Gastrointestinal | Juice of fresh parts is used as laxative. | Oral | Once a day for four days | |||||
| Antipyretic | Juice of fresh parts is used to reduce fever. | Oral | Once a day for two days | |||||
|
| ||||||||
| Jasminum humile f.kensuense | Zeet chumbeli | Oleaceae | Shrub | Flower, root, and latex. | Skin infection | Flowers and roots are boiled to make paste and rub on skin for treating pimples. | Topical | Twice a day for one week |
|
| ||||||||
| Jasminum officinale L. | Chumbeli | Oleaceae | Shrub | Whole plant. | Gastrointestinal | Decoction of leaves and roots are prepared and used as anthelmintic. | Oral | Once a day |
| Kidney problems | Crushed leaves are mixed with flour and taken along water to treat kidney stones. | Oral | Twice a day for one month | |||||
|
| ||||||||
| Justicia adhatoda L | Shna Baza | Acanthaceae | Shrub | Leaves | Diabetes | Half kg of fresh leaves of this plant is extracted with 500 mL water and used against diabetes. | Oral | 10 mL of extract is used twice a day |
| Blood purification | Same as above | Oral | 10 mL of extract is used twice a day | |||||
| Chest infection | Leaves and flowers are plucked, dried under shade, ground to obtain powder; 50 gm of this powder is mixed in 15 mL of honey. | Oral | Half teaspoon twice a day for 15 days | |||||
| Skin infection | Half kg leaves are boiled in 4 liters of water and decoction is used. | Oral | Twice a day | |||||
|
| ||||||||
| Lathyrus aphaca L. | Jee Wareen | Papilionaceae | Herb | Seed and flower | Skin infection | Decoction is used for skin problems. | Topical | As needed |
|
| ||||||||
| Malva neglecta Wallr. | Panderak | Malvaceae | Herb | Whole plant | Kidney problems | Roots are taken and boiled in 2 glasses of water and after boiling when 1 glass of water remains, it is taken for kidney stones. | Oral | Once a day for 40 days |
|
| ||||||||
| Melia azedarach L. | Tora Draka | Meliaceae | Tree | Whole plant | Diabetes | Powder of seeds is used. | Oral | As needed |
| Gastrointestinal | Fruit is ground and its juice is mixed with oil and taken as anthelmintic. | Oral | As needed | |||||
|
| ||||||||
| Mentha arvensis L. | Podeena. | Lamiaceae. | Herb | Leaves | Gastrointestinal | 70 gm dried leaves of wild mint and 30–40 gm of bishops' weed are ground together and 10–12 gm of common salt is also added. It is used for gas problems and stomach pain. | Oral | Thrice a day after meal |
| Vomiting | Tea of dried leaves is taken to stop vomiting. | Oral | As needed | |||||
|
| ||||||||
| Mentha longifolia L. | Venalai | Lamiaceae | Herb | Leaves | Gastrointestinal | Decoction of leaves is used as carminative. | Oral | As needed |
|
| ||||||||
| Monotheca buxifolia (Falc.) A. DC. | Gorgola | Sapotaceae | Shrub | Fruit, stem | Skin infection | Poultice is used against skin infection. | Topical | As needed |
|
| ||||||||
| Morus alba L. | Toot | Moraceae | Tree | Fruit, leaves | Gastrointestinal | Crushed leaves are taken along honey to treat diarrhea. | Oral | Twice a day |
|
| ||||||||
| Morus nigra L. | Tor Toot | Moraceae | Tree | Fruit, leaves | Kidney problems | Fruit is directly eaten as diuretic. | Oral | Twice a day |
|
| ||||||||
| Nannorrhops ritchiana. (Griff.) Aitch. | Mazzari | Arecaceae/Palmae | Shrub | Leaves | Gastrointestinal | Crushed leaves are used as carminative. | Oral | As needed |
| Veterinary | Fresh leaves are given to animals as purgative. | Oral | As needed | |||||
|
| ||||||||
| Nerium oleander L. | Gand derai | Apocynaceae | Shrub | Leaves | Dental pain Wound |
The fresh leaves are washed and crushed, and then 3 cups of water are added. The filtrate is given to the patients suffering from dental pain. | Oral | Twice a day for 5 days |
| Poultice of leaves is applied externally to reduce swelling. | Topical | Twice a day | ||||||
|
| ||||||||
| Olea ferruginea (Sol.) Steud. | Kawwaan | Oleaceae. | Tree |
Fruit, leaves, seeds, and bark |
Dental | Decoction is used for toothache. | Oral | The decoction of fresh leaves is kept in the mouth at night till recovery. |
| Rheumatism | The oil extracted from the fruits is used as massage in the treatment of rheumatism. | Topical | As needed | |||||
| Skeletomuscular | Same as above | Topical | As needed | |||||
|
| ||||||||
| Otostegia limbata Benth. | Spin azghai | Lamiaceae | Shrub | Whole plant | Throat infection | 50 gm fresh leaves are ground and 3-4 teaspoons of water are added to it. This mixture is filtered through a cloth and is given to the patient suffering from mouth gums and throat pains. | Oral | As needed |
| Wound | Crushed leaves are applied for curing of wounds. | Topical | Once a day | |||||
|
| ||||||||
| Oxalis corniculata L. | Tokee pi. | Oxalidaceae | Herb | Leaves, root | Gastrointestinal | Juice of leaves and roots are used against stomach problem. | Oral | As needed |
|
| ||||||||
| Peganum harmala L. | Spin nali | Zygophyllaceae | Herb | Seeds | Spiritual | The smoke from burning seeds and leaves is believed to be devil repellent and also used as protection against evil eyes. | ||
|
| ||||||||
| Periploca aphylla Decne. | Barada | Periplocaceae | Shrub | Stem, bark, and latex. | Gastrointestinal | Branches and flower are dried under shade, ground to obtain powder, and taken along water for constipation and stomach ulcer. | Oral | 2–4 gm of is powder twice a day |
|
| ||||||||
| Phoenix dactylifera L. | Khajoor | Arecaceae | Tree | Fruit, leaves | Gastrointestinal | Take four dried khobani and three khajoor and keep it in milk and boil it. After cooling take it on an empty stomach with 1 teaspoon of isapagul; it is good for controlling constipation. | Oral | As needed |
| Sex power | Same as above | Oral | As needed | |||||
|
| ||||||||
| Pinus roxburghii Sarg. | Nakthar | Pinaceae | Tree | All aerial | Dental | Juice is extracted from fresh leaves and bark by grinding. This is mixed with water and taken for toothache. | Oral | Twice a day before meal and at bed time |
| Gastrointestinal | Similarly, the bark and leaves of Pinus are dried and crushed, and then the powder is dissolved in cold water and taken for diarrhea. | Oral | Twice a day before meal and at bed time | |||||
| Skin infection | Leaves of the plant are boiled and the extract is obtained and taken before meal as remedy for scabies. | Oral | As needed | |||||
|
| ||||||||
| Pistacia chinensis Bunge. | Shenai | Tree | Whole plant | Gastrointestinal | Powdered galls fried with ghee are given internally in dysentery. | Oral | Once a day | |
| Skin infections | The stem gum is added to the mustard oil, warmed, and mixed. The prepared poultice is then applied to the ruptured heels at night. | Topical | At night for once | |||||
|
| ||||||||
| Plantago lanceolata L. | Gwayo zhabe | Plantaginaceae | Herb | Whole plant | Dental | Leaves are crushed and kept in mouth to relieve toothache. | Oral | As needed |
| Gastrointestinal | Seeds and fruits are drunk as purgative and laxative. | Oral | As needed | |||||
| Skin infections | Fresh leaves are crushed for athlete's foot. | Topical | As needed | |||||
|
| ||||||||
| Plantanus orientalis L. | Chenar | Platanaceae | Tree | Whole plant | Gastrointestinal | The peel of the fruit is dried, soaked, and ground. The powder so formed, called “Narsaway,” is mixed in small quantity in a cup of curd and is used for dysentery. | Oral | Twice in a day till recovery for the treatment |
|
| ||||||||
| Punica granatum L. | Anar | Punicaceae | Shrub | Fruit, bark | Gastrointestinal | The fruit pericarp is dried, powdered, mixed with sugar, and used for diarrhea and dysentery. | Oral | As needed |
| Chest infections | The fruit pericarp is mixed with tea and is given for whooping cough. | Oral | As needed | |||||
| Blood purifier | Fruit is directly eaten. | Oral | As needed | |||||
|
| ||||||||
| Rumex dentatus L. | Reen zakai | Polygonaceae | Herb | Leaves | Sex enhancer | Decoction of leaves is used. | Oral | Once at night |
| Skeletomuscular | Same as above | Oral | As needed | |||||
|
| ||||||||
| Ricinus communis L. | Raanda | Euphorbiaceae | Shrub | Seeds, leaf, bark, and root. |
Gastrointestinal | The small quantity of oil is rubbed on the abdomen, which is slowly and gradually absorbed through sweat glands to release constipation. | Topical | Twice a day for one day |
|
| ||||||||
| Sageretia thea (Osbeck) M.C. Johnst. | Mamoti | Rhamnaceae | Shrub | Fruit, roots | Jaundice | The extraction of roots is used as cooling agent in jaundice. | Oral | Once a day |
|
| ||||||||
| Saccharum spontaneum L. | Shaat | Poaceae | Herb | Whole plant | Chest infection | Juice of whole plants is mixed with milk for the treatment of cough. | Oral | Twice a day for two days |
|
| ||||||||
| Solanum incanum L. | Tarkha Mowtngee | Solanaceae | Shrub | Leaves and roots | Kidney problems | Decoction of leaves and roots are used to break kidney stones. | Oral | As needed |
|
| ||||||||
| Solanum villosum Miller. | Koot soab | Solanaceae | Herb | Whole plant | Kidney problems | Decoction of leaves and roots are used to break kidney stones. | Oral | As needed |
|
| ||||||||
| Sonchus arvensis L. | Kroo Konai | Asteraceae | Herb | Whole plant | Wounds | The whole plant is crushed to form a paste. The paste is applied as a poultice on wounds and boils. | Topical | As needed |
|
| ||||||||
| Silybummarianum (L.) | Azghai | Asteraceae | Herb | Leaves, seeds, and flowers head | Antipyretic Jaundice Liver problems |
Seeds are collected, dried under shade, and roasted in vegetable oil. Roasted seeds are ground to obtain powder. This is used to treat hepatitis. | Oral | Half teaspoon of this powder is taken thrice a day for a month |
| Same as above | Oral | Same as above | ||||||
| Same as above | Oral | Same as above | ||||||
|
| ||||||||
| Taraxacum officinale F.H. Wigg. | Asteraceae | Herb | Leaves, root | Jaundice | 20–30 gm dried aerial parts are boiled in 1 liter of water for 15–20 min to which 15–20 gm sugar is added. This decoction is filtered and used against jaundice. | Oral | Half cup is given twice a day | |
| Diabetes | Half kg dried aerial parts are boiled in 2 liters water and decoction is filtered and used for diabetes. | Oral | One cup of this decoction is taken twice a day | |||||
|
| ||||||||
| Terminalia arjuna L. | Combretaceae | Tree | Bark, fruits, and leaves | Cardiovascular | Fruits and leaves are ground to make powder and mix with essential additives. | Oral | Once a day | |
|
| ||||||||
| Vitex negundo L. | Marmandi | Verbenaceae | Shrub | Leaves, root, stem, and seeds | Gastrointestinal | 60 gm dried seeds of this plant, 30 gm Bishop's weed, and 2-3 teaspoon of common salt are ground together to powder. | Oral | As needed |
| Antipyretic | Same as above | Oral | As needed | |||||
| Jaundice | The decoction of leaves is used for jaundice. | Oral | As needed | |||||
| Kidney problem | The seeds are ground to obtain powder and are taken with water for kidney stone. | Oral | Half spoon once a day | |||||
|
| ||||||||
| Withania somnifera (L.) Dunal | Kapyanga | Solanaceae | Herb | Leaves, roots, and seeds | Kidney problems | The decoction of leaves is taken to break kidney stones. | Oral | As needed |
|
| ||||||||
| Ziziphus mauritiana var. abyssinica (Hochst. ex A. Rich.) Fiori | Bera | Rhamnaceae | Tree | Fruit, root, and leaves | Gastrointestinal | The decoction of fruit and bark is taken with a cup of milk to treat constipation and dysentery. | Oral | As needed |
|
| ||||||||
| Ziziphus nummularia (Burm. f.) Wight and Arn. | Karkata | Rhamnaceae | Shrub | Fruit, leaves | Gastrointestinal | Powder of fruits and leaves are used to treat constipation. | Oral | Thrice a day for 2 days |
4.2. Common Ailments in the Study Area
Traditional healers use 67 medicinal plants for the treatment of a variety of disorders in the studied region. These were grouped into 18 major disease categories like gastrointestinal, dermatological, antipyretic, blood disorders, and so forth. The natives of the region use total 25 plant species for gastrointestinal disorders followed by 13 for dermatological infections. The results are in agreement with other studies conducted in other parts of Pakistan and other countries [28, 29]. The use of a large number of medicinal plants for the treatment of gastrointestinal and dermatological ailments in the region could be due to the high occurrence of these problems in the study area due to bad hygiene, fuel wood smoke inside houses, and other factors like water and air pollution [30]. Informant consensus results have also shown a high degree of consensus for gastrointestinal and dermatological (0.87 each) ailments, which were followed by blood disorder like diabetes (0.84) (Table 2). The highest plant use citation was for gastrointestinal (200) followed by dermatological ailments (100). High Fic value gives an indication that these diseases are more prevalent in the Hangu region that might be due to the poor socioeconomic and sanitary conditions of the people. According to Heinrich et al. [19], high Fic values are very useful in the selection of specific plants for further search of bioactive compounds. The medicinal plants that are widely used by the local people have higher FL values than those that are less popular. The present study revealed 20 medicinal plants having high FL value. FL values in this study varied from 1.0% to 100%. The study determined 3 plant species (Acacia modesta, Caralluma tuberculata, and Withania somnifera) with a FL of 100% followed by 7 (Allium sativa L., Mentha arvensis L., Mentha longifolia L., Cannabis sativa L., Punica granatum L., Morus alba, and Morus nigra L.) species with more than 90% and less than 100%, which might be taken as a signal of the excellent curative potential of the plants (Table 3). All these plants that reported higher FL values are not only being frequently used in study region but also in other regions of the Pakistan [8, 31]. These plants possess different phytochemicals responsible for their therapeutic actions. Withania somnifera contains compound withanolides, which are believed to account for its extraordinary medicinal properties [32]. Caralluma tuberculata contains pregnane glycosides, flavones glycosides, and other phytochemical responsible for its antidiabetic and anticancer activities [33]. It is understood that plants used in recurring manner are more phytochemically active [16]. High FL value plants might be selected for further chemical screening to investigate the bioactive compounds responsible for their high curative potential [34, 35].
Table 2.
Fic values of traditional medicinal plants for treating human ailments in district Hangu.
| S. Number | Disease categories | Nur | Nt | Fic |
|---|---|---|---|---|
| 1 | Gastrointestinal | 200 | 25 | 0.87 |
| 2 | Dermatological | 100 | 13 | 0.87 |
| 3 | Skeletomuscular | 7 | 2 | 0.83 |
| 4 | Blood disorders | 58 | 10 | 0.84 |
| 5 | Chest infections | 24 | 7 | 0.73 |
| 6 | Jaundice | 14 | 7 | 0.53 |
| 7 | Ear nose throat problems | 12 | 3 | 0.81 |
| 8 | Antipyretic | 32 | 7 | 0.80 |
| 9 | Narcotic | 3 | 2 | 0.54 |
| 10 | Sex power | 8 | 3 | 0.71 |
| 11 | Kidney problems | 22 | 7 | 0.71 |
| 12 | Wounds | 3 | 2 | 0.54 |
| 13 | Rheumatism | 9 | 3 | 0.75 |
| 14 | Veterinary | 9 | 3 | 0.75 |
| 15 | Dental | 12 | 4 | 0.71 |
| 16 | Piles | 9 | 3 | 0.75 |
| 17 | Liver problems | 7 | 1 | 1 |
| 18 | Cardiovascular | 9 | 1 | 1 |
Table 3.
Fidelity level value of medicinal plants commonly reported against a given ailment.
| Number | Medicinal plants | Ailments | lp | lu | FL value % |
|---|---|---|---|---|---|
| 01 | Acacia modesta | Skeletomuscular | 19 | 19 | 100 |
| 02 | Caralluma tuberculata | Antidiabetic | 19 | 19 | 100 |
| 03 | Withania somnifera | Gastrointestinal | 26 | 26 | 100 |
| 04 | Allium sativum | Blood pressure | 18 | 19 | 94.7 |
| 05 | Mentha arvensis | Gastrointestinal | 23 | 25 | 92 |
| 06 | Mentha longifolia | Gastrointestinal | 23 | 25 | 92 |
| 07 | Cannabis sativa | Narcotic | 11 | 12 | 91.6 |
| 08 | Punica granatum | Blood purifier | 21 | 23 | 91.3 |
| 09 | Morus alba | Respiratory tract | 19 | 21 | 90.4 |
| 10 | Morus nigra | Respiratory tract | 19 | 21 | 90.4 |
| 11 | Oxalis corniculata | Gastrointestinal | 17 | 19 | 89.4 |
| 12 | Fagonia indica | Dermatological | 17 | 19 | 89.4 |
| 13 | Fagonia indica | Blood purifier | 26 | 30 | 86.6 |
| 14 | Ricinus communis | Pregnancy | 06 | 08 | 75 |
| 15 | Olea ferruginea | Dermatological | 12 | 16 | 75 |
| 16 | Olea ferruginea | Sore throat | 11 | 15 | 73.3 |
| 17 | Justicia adhatoda | Skeletomuscular | 07 | 10 | 70 |
| 18 | Cuscuta reflexa | Dermatological | 11 | 16 | 68.7 |
| 19 | Ziziphus nummularia | Antidiabetic | 06 | 10 | 60 |
| 20 | Sageretia thea | Antidiabetic | 08 | 14 | 57.1 |
4.3. Ethnomedicinal Preparations
Traditional healers mostly use leaves (40%) of the plants followed by whole plant (28%) and fruits (19%) for the preparation of different ethnomedicines. The current investigation showed (Figure 2) that leaves (40%) are the most collected plant parts for medicinal purposes. This might be due to easy availability and containing high amount of chemicals and could be easily extracted and used in different forms but it needs biochemical analysis and pharmaceutical screening to cross-check the local information. Use of leaves of plants does not cause damaging effect on the plant life cycle as compared with other parts like roots and flower, and so forth. Due to good rainfall conditions about eight months in the year, the leaves remain green and abundant for most of the months. Our findings of the frequent use of green leaves in the preparation of remedies corroborate the results of [36, 37]. Traditional healers are involved in preparation of 110 recipes preparation and the major modes of ethnomedicines preparation in the studied region were decoction (20%), powdering (20%), crushing (12%), extracting juice (10%), and so forth (Figure 3). Decoction and grinding of medicinal plants for the preparation of ethnomedicines could be due to their high effectiveness for the curing of various ailments. According to Deeba [38], decoction, grinding or crushing, and boiling methods are the most commonly followed methods for the extraction of active compounds. Monotherapy preparations using single medicinal plant were found to be more abundant in comparison with herbal concoction that was prepared by mixing two or three species; for example, healers take equal amount of extract of onion bulb and mint and mix them for the treatment of cholera. Another example is taking 70 gm dried leaves of wild mint and 30–40 g of “bishops” weed and grinding them together and 10–12 gm of common salt is also added to them and taken for the treatment of gastric problem and stomach pain. The use of mixture of plants has recently been shown to increase the effectiveness of the herbal medicine [39]. Out of total 110 ethnomedicines, 91% were prepared by using fresh plant materials, whereas 9% were prepared using dried parts (Table 1). The high usage of freshly prepared ethnomedicines is an indication of the high abundance of medicinal plants in the surrounding areas to be harvested anytime. These findings are in line with other studies conducted in other areas [40, 41]. The other reason behind the repeated use of fresh plant material could be due to the fact that the drying process contributes to the loss of volatile oil and sometimes due to the fact that high temperature protein becomes denature. Higher use of fresh plant material on the other hand is not a sustainable practice as it may threaten the plants due to recurrent harvesting.
Figure 2.
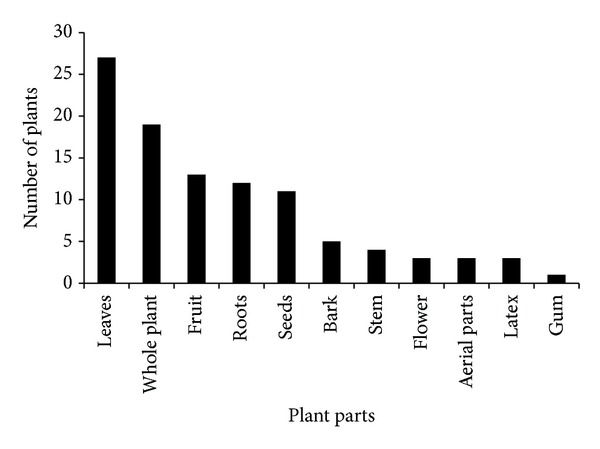
Plant parts used for remedy preparation.
Figure 3.
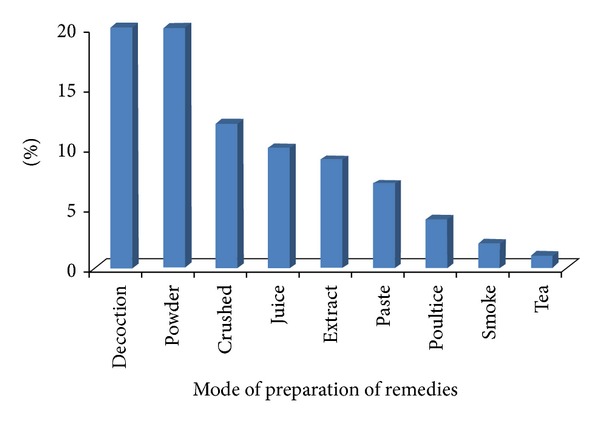
Methods of preparation of ethnomedicines.
4.4. Route of Administration and Dosage
The current survey revealed that most of the plant remedies are taken orally and topically in the investigated region while only single recipe is taken through ear (Table 1). As mentioned earlier, gastrointestinal and skin problems are common in the region and that might be the reason why the majority of the plants are being used orally and topically while some of the plants are being used through ears. Ethnomedicines are taken along different types of additives generally called vectors like honey, salt, sugar, milk, desi ghee, and wheat flour for the purpose of increasing flavor and to reduce the astringent taste of the remedies. This means that since traditional medicines could have sour or bitter tastes in most cases, the additives reduce such tastes and may even improve the efficacy of the medicine. The measurements used to determine the dosages are not standardized and depend on the age and physical appearance of the patient, sociocultural explanation of the illness, diagnosis, and experience of individual herbalist [42]. Mostly the treatment of the patient is completed within a single day or couple of days. When the patients did not show any indication of improvement from their sickness following treatment completion, they were recommended to modern health centres in urban area for further examination by the physician.
4.5. Multipurpose Medicinal Plants and Threats to Their Extinction
The results of the DMR implementation on multipurpose medicinal plants enabled us to recognize which of the multipurpose plants are more under stress in the area and the causes that threaten the plant (Table 4). Accordingly, Olea ferruginea ranked first, Morus alba ranked second, Melia azedarch ranked third, and Acacia modesta ranked fourth while Acacia nilotica ranked fifth. These multipurpose species are basically trees and therefore these species are facing great pressures as the local people are unsustainably harvesting these species for a variety of purposes. The factors responsible for the declining of these species abundance in the area were their overharvesting for agricultural tool, construction, fodder, and fire wood purposes. Beside these major threats, locals of the region also use these plants for handicrafts manufacturing. Free grazing is the common practice in the area. Before the commencement of winter, the grasses are harvested, dried, and put into a stake. The harvesting is done collectively, and then during the bare and cold months of winter, these are fed to the domestic animals. Fuel consumption per home in the studied area is often considered more than the consumption on feeding and other requirements because of severe winters. Thus, the results require urgent conservation strategies to save the declining population of multipurpose plant species in the study region. References [43, 44] have also stated the identical pattern of maximum exploitation of multipurpose medicinal plants for uses other than their traditional medicinal importance in southeastern Ethiopia. Traditional healers mostly use the whole plant of these multipurpose species or individual roots (Table 1) of some species for the preparation of ethnomedicinal recipes and this is an unsustainable practice as compared to leaves. Therefore, there is a dire need to take necessary steps for the conservation of these species before their extinction.
Table 4.
DMR score of fifteen key informants for eleven medicinal plants species with additional uses besides medicinal value.
| Use diversity |
A. modesta | P. chinensis | D. viscosa | D. sissoo | M. azedarach | M. alba nigra | O. ferruginea | F. religiosa | P. roxburghii | A. nilotica | Z. mauritiana | Total | Rank |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Agricultural tool |
2 | 0 | 3 | 0 | 4 | 5 | 5 | 0 | 1 | 5 | 0 | 25 | 4 |
| Construction | 0 | 4 | 0 | 5 | 5 | 5 | 5 | 5 | 4 | 3 | 2 | 38 | 3 |
| Fodder | 5 | 3 | 0 | 0 | 0 | 5 | 3 | 3 | 0 | 0 | 4 | 23 | 5 |
| Fire wood | 5 | 3 | 5 | 3 | 5 | 4 | 5 | 4 | 3 | 5 | 3 | 45 | 1 |
| Medicine | 5 | 3 | 3 | 3 | 4 | 5 | 5 | 2 | 3 | 3 | 3 | 39 | 2 |
| Total | 17 | 13 | 11 | 11 | 18 | 20 | 23 | 14 | 11 | 16 | 12 | ||
| Rank | 4 | 7 | 9 | 9 | 3 | 2 | 1 | 6 | 9 | 5 | 8 |
Based on use criteria (5 = best; 4 = very good; 3 = good; 2 = less used; 1 = least used; and 0 = no value).
4.6. Indigenous Knowledge Associated with Gender, Age, and Socioeconomic Status of the People
Among the 55 informants, 34 (61.81%) were male and 21 (38.18%) were female (Table 5). It is witnessed that males had better knowledge regarding ethnomedicines than females. The reason behind that men have well indigenous knowledge than women might be due to the fact that the men are usually favoured in the shift of the knowledge; however, in many cultures women are responsible for the family's health. The highest number of informants aged above 40 years. The result shows that traditional knowledge is prevalent among the community members; however, it is under threat of transferring to the younger generation to come. The decreasing rate of transfer of indigenous knowledge might be due to the lack of interest among the younger generation to learn and practice it, which might be attributed to the ever increasing influence of modernization [8]. Almost half of the respondents interviewed were illiterate (45.45%), whilst most of those with an education had merely primary (29.09%) which reflect the unavailability of standard educational institution in the area (Table 5). Literate people in the study area were found to have less knowledge of medicinal plants as compared to illiterate ones as the former are more likely to be exposed to modernization as also revealed by studies conducted elsewhere [8, 45, 46]. The inhabitants of the study area are not very well off due to less literacy rate and therefore they are heavily dependent on medicinal plants for a variety of purposes in order to compensate their income.
Table 5.
Gender, age group and literacy level frequencies, and occupation of the interviewed people in the region.
| Total | Percentage | |
|---|---|---|
| Gender | ||
| Male | 34 | 61.81 |
| Female | 21 | 38.18 |
| Age groups | ||
| 20–29 | 2 | 3.63 |
| 30–39 | 3 | 5.45 |
| 40–49 | 7 | 12.72 |
| 50–59 | 7 | 12.72 |
| 60–69 | 15 | 27.27 |
| 70–79 | 12 | 21.81 |
| 80–89 | 9 | 16.3 |
| Educational attainment | ||
| Illiterate | 25 | 45.45 |
| Primary | 16 | 29.09 |
| Middle | 10 | 18.18 |
| Secondary | 2 | 3.63 |
| University | 2 | 3.63 |
| Occupation | ||
| Females | ||
| House wives | 19 | 90.47 |
| Primary teacher | 2 | 9.52 |
| Males | ||
| Shopkeepers | 10 | 29.4 |
| Farmers | 13 | 38.2 |
| Labours | 6 | 17.6 |
| Primary teachers | 5 | 14.7 |
5. Conclusions
The present study has recorded 67 medicinal plants used for the treatment of a variety of human ailments in the rural area near Pak-Afghan border region. In the study area herbs constituted the highest proportion of medicinal plants to be utilized. Mostly the leaves of the plants are harvested for different ethnomedicines preparation. Decoction and powdering are the most common methods of drug preparation and remedies are mostly taken orally in the studied region. A high number of plants have been reported to treat gastrointestinal and dermatological problems. The medicinal plants in the region are also facing some threats like unsustainable collection method of some plants, collection for fuel wood, for construction, and for fodder, and agricultural tools. For sustainable utilization of medicinal plants and to avoid further loss, the District Agricultural Office needs to team up with the local people, by providing the community with planting materials of the most threatened and preferred medicinal and multipurpose species so that they can grow them in their home gardens. Moreover, the documented medicinal plants with high degree of consensus can serve as a basis for future investigation of modern drug.
Acknowledgments
The authors are thankful to the Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia, for funding the work through the research Group project No RGP-VPP-210. The authors are thankful to the local people for sharing their valuable indigenous knowledge.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
Authors' Contribution
Muhammad Adnan and Akash Tariq have designed the research project. Imran Khan conducted the field work and wrote the draft of the paper. Akash Tariq has equally contributed in writing the paper with Imran Khan. Muhammad Adnan, Naser M. AbdElsalam, and Riaz Ullah provided comments on the draft and helped in finalizing the paper. All the authors read and approved the final paper.
References
- 1.Feo DV. Medicinal and magical plants in the northern Peruvian Andes. Fitoterapia. 1992;63(5):417–440. [Google Scholar]
- 2.Breevort P. The booming U.S. botanical market: a new overview. Herbal Gram. 1998;44:33–46. [Google Scholar]
- 3.Wright CW. Plant derived antimalarial agents: new leads and challenges. Phytochemistry Reviews. 2005;4(1):55–61. [Google Scholar]
- 4.Hamayun M, Khan SA, Kim HY, Leechae IJ. Traditional knowledge and ex-situ conservation of some threatened medicinal plants of Swat Kohistan. Pakistan Journal of Botany. 2006;38:205–209. [Google Scholar]
- 5.Hamayun S. Structural diversity, vegetation dynamics and anthropogenic impaction Lesser Himalayan subtropical Forests of Bagh District, Kashmir. Pakistan Journal of Botany. 2011;43:1861–1866. [Google Scholar]
- 6.Mohammad S. Pakistan-Afghanistan: The Conjoined Twins. Kabul, Afghanistan: Department of Embassy of Pakistan; 2010. [Google Scholar]
- 7.Barnett RR, Abubakar S. Resolving Pakistan-Afghanistan Stalemate. Washington, DC, USA: United States Institute of Peace; 2006. [Google Scholar]
- 8.Adnan M, Ullah I, Tariq A, et al. Ethnomedicine use in the war affected region of northwest Pakistan. Journal of Ethnobiology and Ethnomedicine. 2014;10, article 16 doi: 10.1186/1746-4269-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akhtar N, Rashid A, Murad B, Bergmeier E. Diversity and use of ethnomedicinal plants in the region of Swat, North Pakistan. Journal of Ethnobiology and Ethnomedicine. 2013;9, article 25 doi: 10.1186/1746-4269-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mussarat S, AbdElsalam NM, Tariq A, Wazir SM, Ullah R, Adnan M. Use of ethnomedicinal plants by the people living around Indus River. Evidence-Based Complementary and Alternative Medicine. 2014;2014:14 pages. doi: 10.1155/2014/212634.212634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hassan IH, Murad W, Tariq A, Ahmad A. Ethnoveterinary study of medicinal plants in Malakand Valley, District Dir (Lower), Khyber Pakhtunkhwa, Pakistan. Irish Veterinary Journal. 2014;67(1, article 6) doi: 10.1186/2046-0481-67-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Begum S, AbdElsalam NM, Adnan M, Tariq A, Yasmin A, Hameed R. Ethnomedicines of highly utilized plants in temperate Himalaya region. African Journal of Traditional Complementary and Alternative Medicine. 2014;11(3):132–142. doi: 10.4314/ajtcam.v11i3.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khan I. Ethnobotanical and ecological study of Hangu district, Pakistan [M.S. thesis] Kohat, Pakistan: Kohat University of Science and Technology; 2013. [Google Scholar]
- 14.Mustafa G. Islamabad, Pakistan: UNESCO; 2009. Education policy analysis report of Khyber Pakhtunkhwa. [Google Scholar]
- 15.Martin GJ. Ethnobotany: A Method Manual. London, UK: Chapman & Hall; 1995. [Google Scholar]
- 16.Cotton CM. Ethnobotany: Principles and Applications. Chichester, UK: John Willey & Sons; 1996. [Google Scholar]
- 17.Giday M, Teklehaymanot T, Animut A, Mekonnen Y. Medicinal plants of the Shinasha, Agew-awi and Amhara peoples in northwest Ethiopia. Journal of Ethnopharmacology. 2007;110(3):516–525. doi: 10.1016/j.jep.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 18.Trotter RT, Logan MH. Informants consensus: a new approach for identifying potentially effective medicinal plants. In: Etkin NL, editor. Plants in Indigenous Medicine and Diet. Bedford Hill, NY, USA: Redgrave; 1986. pp. 91–112. [Google Scholar]
- 19.Heinrich M, Ankli A, Frei B, Weimann C, Sticher O. Medicinal plants in Mexico: healers’ consensus and cultural importance. Social Science and Medicine. 1998;47(11):1859–1871. doi: 10.1016/s0277-9536(98)00181-6. [DOI] [PubMed] [Google Scholar]
- 20.Canales M, Hernandez T, Caballero J, et al. Informant consensus factor and antibacterial activity of the medicinal plants used by the people of San Rafael Coxcatlán, Puebla, México. Journal of Ethnopharmacology. 2005;97(3):429–439. doi: 10.1016/j.jep.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 21.Giday M, Asfaw Z, Woldu Z, Teklehaymanot T. Medicinal plant knowledge of the Bench ethnic group of Ethiopia: an ethnobotanical investigation. Journal of Ethnobiology and Ethnomedicine. 2009;5, article 34 doi: 10.1186/1746-4269-5-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Friedman J, Yaniv Z, Dafni A, Palewitch D. A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. Journal of Ethnopharmacology. 1986;16(2-3):275–287. doi: 10.1016/0378-8741(86)90094-2. [DOI] [PubMed] [Google Scholar]
- 23.Singh GA, Kumar A, Tewari DD. An ethnobotanical survey of medicinal plants used in Terai forest of western Nepal. Journal of Ethnobiology and Ethnomedicine. 2012;8, article 19 doi: 10.1186/1746-4269-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tabuti JRS, Lye KA, Dhillion SS. Traditional herbal drugs of Bulamogi, Uganda: plants, use and administration. Journal of Ethnopharmacology. 2003;88(1):19–44. doi: 10.1016/s0378-8741(03)00161-2. [DOI] [PubMed] [Google Scholar]
- 25.Uniyal SK, Singh KN, Jamwal P, Lal B. Traditional use of medicinal plants among the tribal communities of Chhota Bhangal, Western Himalaya. Journal of Ethnobiology and Ethnomedicine. 2006;2, article 14 doi: 10.1186/1746-4269-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gazzaneo LRS, Lucena RFP, Albuquerque UP. Knowledge and use of medicinal plants by local specialists in an region of Atlantic Forest in the state of Pernambuco (Northeastern Brazil) Journal of Ethnobiology and Ethnomedicine. 2005;1, article 9 doi: 10.1186/1746-4269-1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Adnan M, Begum S, Latif A, Tareen AM, Lee LJ. Medicinal plants and their uses in selected temperate zones of Pakistani Hindukush-Himalaya. Journal of Medicinal Plants Research. 2012;6:4113–4127. [Google Scholar]
- 28.Murad W, Ahmad A, Gilani SA, Khan MA. Indigenous knowledge and folk use of medicinal plants by the tribal communities of Hazar Nao Forest, Malakand District, North Pakistan. Journal of Medicinal Plant Research. 2011;5(7):1072–1086. [Google Scholar]
- 29.Tolossa K, Debela E, Athanasiadou S, Tolera A, Ganga G. Ethno-medicinal study of plants used for treatment of human and livestock ailments by traditional healers in South Omo, Southern Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2013;9, article 32 doi: 10.1186/1746-4269-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Azizullah A, Khattak MNK, Richter P, Häder D-P. Water pollution in Pakistan and its impact on public health—a review. Environment International. 2011;37(2):479–497. doi: 10.1016/j.envint.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 31.Alamgeer, Ahmad T, Rashid M, et al. Ethnomedicinal Survey of plants of Valley Alladand Dehri, Tehsil Batkhela, District Malakand, Pakistan. International Journal of Basic Medical Sciences and Pharmacy. 2013;3(1):23–32. [Google Scholar]
- 32.Bhattacharya SK, Bhattacharya D, Sairam K, Ghosal S. Effect of Withania somnifera glycowithanolides on a rat model of tardive dyskinesia. Phytomedicine. 2002;9(2):167–170. doi: 10.1078/0944-7113-00089. [DOI] [PubMed] [Google Scholar]
- 33.Rauf A, Jan MR, Rehman WU, Muhammad N. Phytochemical, phytotoxic and antioxidant profile of Caralluma tuberculata N. E. Brown. Wudpecker Journal of Pharmacy and Pharmacology. 2013;2(2):21–25. [Google Scholar]
- 34.Bekalo TH, Woodmatas SD, Woldemariam ZA. An ethnobotanical study of medicinal plants used by local people in the lowlands of Konta Special Woreda, southern nations, nationalities and peoples regional state, Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2009;5, article 26 doi: 10.1186/1746-4269-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lulekal E, Asfaw Z, Kelbessa E, Damme VP. Ethnomedicinal study of plants used for human ailments in Ankober District, North Shewa Zone, Amhara Region, Ethiopia. Journal of Ethnobiology and Ethnomedicine. 2013;9, article 63 doi: 10.1186/1746-4269-9-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kala CP. Ethnomedicinal botany of the Apatani in the Eastern Himalayan region of India. Journal of Ethnobiology and Ethnomedicine. 2005;1, article 11 doi: 10.1186/1746-4269-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bhat JA, Kumar M, Bussmann RW. Ecological status and traditional knowledge of medicinal plants in Kedarnath Wildlife Sanctuary of Garhwal Himalaya India. Journal of Ethnobiology Ethnomedicine. 2013;9, article 1 doi: 10.1186/1746-4269-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deeba F. Documentation of ethnoveterinary practices in urban and peri-urban areas of Faisalabad, Pakistan [Ph.D. thesis] Faisalabad, Pakistan: University of Agriculture; 2009. [Google Scholar]
- 39.Zonyane S, van Vuuren SF, Makunga NP. Pharmacological and phyto-chemical analysis of a medicinal plant mixture that is used as traditional medicine in Western Cape. Proceedings of the 38th Annual Conference of the South African Association of Botanist; January 2012; Pretoria, South Africa. University of Pretoria; p. p. 124. [Google Scholar]
- 40.Ignacimuthu S, Ayyanar M, Sivaraman K. Ethnobotanical investigations among Tribes in Madurai District of Tamil Nadu (India) Journal of Ethnobiology and Ethnomedicine. 2006;2, article 25 doi: 10.1186/1746-4269-2-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bussmann RW, Sharon D. Traditional medicinal plant use in Loja Province, Southern Ecuador. Journal of Ethnobiology and Ethnomedicine. 2006;2, article 44 doi: 10.1186/1746-4269-2-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jabbar A, Raza MA, Iqbal Z, Khan MN. An inventory of the ethnobotanicals used as anthelmintics in the southern Punjab (Pakistan) Journal of Ethnopharmacology. 2006;108(1):152–154. doi: 10.1016/j.jep.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 43.Sher Z, Khan DZ, Hussain F. Ethnobotanical studies of some plants of Chagharzai Valley, District Buner, Pakistan. Pakistan Journal of Botany. 2011;43(3):1445–1452. [Google Scholar]
- 44.Yineger H, Kelbessa E, Bekele T, Lulekal E. Ethnoveterinary medicinal plants at Bale Mountains National Park, Ethiopia. Journal of Ethnopharmacology. 2007;112(1):55–70. doi: 10.1016/j.jep.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 45.Gedif T, Hahn H. The use of medicinal plants in self-care in rural central Ethiopia. Journal of Ethnopharmacology. 2003;87(2-3):155–161. doi: 10.1016/s0378-8741(03)00109-0. [DOI] [PubMed] [Google Scholar]
- 46.Bastien JW. Exchange between Andean and Western medicine. Social Science and Medicine. 1982;16(7):795–803. doi: 10.1016/0277-9536(82)90232-5. [DOI] [PubMed] [Google Scholar]


