Abstract
Objective
To explore the underlying causation of unexplained multimorbidity with sensitivities and to discuss the management of patients who present with this perplexing condition.
Sources of information
Medical and scientific literature was used from MEDLINE (PubMed), several books, toxicology and allergy journals, conference proceedings, government publications, and environmental health periodicals.
Main message
Multimorbidity with sensitivities has become an increasingly common and confusing primary care dilemma. Escalating numbers of debilitated individuals are now presenting to family physicians and specialists with multisystem health complaints, including sensitivities and fatigue, with no obvious causation, a paucity of laboratory findings, and a lack of straightforward solutions. In the recent scientific literature, there is discussion of sensitivity-related illness, an immune-mediated disorder that frequently manifests with multisystem symptoms, commonly including sensitivities and fatigue. This condition appears to be originally caused by adverse environmental exposures and toxicant bioaccumulation—an increasingly prevalent and well-documented problem in contemporary culture.
Conclusion
Various toxic exposures and their bioaccumulation within the body frequently manifest as sensitivity-related illness. In clinical settings, patients with this disorder often present with otherwise unexplained multimorbidity and sensitivities. The health status of patients with this condition can be ameliorated by removing triggers (eg, scented products), optimizing biochemistry, removing further sources of toxicant exposures, and eliminating the internal dose of persistent toxicants.
Résumé
Objectif
Explorer les causes sous-jacentes d’une multimorbidité inexpliquée avec sensibilités et discuter de la prise en charge des patients qui se présentent avec ce problème singulier.
Sources des données
La documentation médicale et scientifique est tirée de MEDLINE (PubMed), de divers manuels, de revues spécialisées en toxicologie et en allergies, de comptes rendus de conférences, de publications gouvernementales et de périodiques sur la santé environnementale.
Message principal
La multimorbidité accompagnée de sensibilités est devenue un dilemme de plus en plus fréquent et déroutant en soins primaires. Un nombre grandissant de personnes affaiblies se présentent maintenant chez des médecins de famille et d’autres spécialistes en raison de problèmes de santé multisystémiques, y compris des sensibilités et de la fatigue, sans cause évidente, avec des résultats de laboratoires peu concluants, sans qu’il y ait de solutions simples. Dans la documentation scientifique récente, on traite des maladies reliées aux sensibilités, un trouble à médiation immunitaire qui se manifeste fréquemment par des symptômes multisystémiques, incluant habituellement des sensibilités et de la fatigue. Ce problème semble être causé à l’origine par des expositions environnementales néfastes et une bioaccumulation de substances toxiques, un phénomène de plus en plus prévalent et bien documenté dans la culture contemporaine.
Conclusion
Diverses expositions à des substances toxiques et leur bioaccumulation dans le corps se manifestent souvent sous forme de maladies reliées à des sensibilités. Dans les milieux cliniques, des patients souffrant d’un tel trouble se présentent avec une multimorbidité et des sensibilités inexplicables autrement. L’état de santé des patients qui ont ce problème peut être amélioré en supprimant les déclencheurs (p. ex. produits parfumés), en optimisant la condition biochimique, en enlevant les autres sources d’exposition à des substances toxiques et en éliminant la dose interne de substances toxiques persistantes.
To prevent disease, to relieve suffering, and to heal the sick—this is our work.
Sir William Osler
As discussed in a commentary in this month’s issue of Canadian Family Physician (page 511),1 escalating numbers of exasperated individuals suffering from chronic multisystem conditions, often including chemical sensitivities or food intolerances, are repeatedly presenting to primary care physicians and specialists, as their symptoms remain unresponsive to standard medical treatments and conventional pharmaceuticals. Recent evidence suggests that about three-quarters of patients in general practice now present with multiple ongoing conditions,2 with management of chronic disorders accounting for about 80% of primary care in Canada. As clinical practice guidelines are generally focused on single and distinct disorders, practitioners are often not effectively trained to modify care to manage multimorbidity states.3 The repercussions of this reality are profound, as multimorbidity is associated with increased disability, declining functional status, diminished quality of life, higher mortality, and greater consumption of health care services.4
In this clinical review, we describe the clinical state and progressive recovery of a man presenting with chronic multisystem complaints.
Case description
A 59-year-old rabbi experienced episodic headache, dizziness, and muscle discomfort beginning in adolescence. Into adulthood, these symptoms became more frequent and manifestations expanded to include episodic vision and hearing loss, inexplicable rashes, memory impairment, ataxia, profound agitation, and eventual blackouts. He also complained of intractable fatigue, insomnia, recurrent wheezing, musculoskeletal discomfort, and cognitive dysfunction.
The patient saw multiple physicians, but no physiologic cause for his multimorbidity was identified. Various diagnoses were given, but a subsequent psychiatric assessment conferred a diagnosis of “narcissistic, borderline personality disorder with extreme anxiety” to explain the totality of his presentation. As analgesic, asthma, and allergy medications provided minimal sustained benefit, psychotropic medication was employed but to no avail.
On taking an environmental history, the patient described exposure to perfumes and other scents as precipitating and aggravating his varied symptoms. While fervently avoiding all scented locales, many environments were still not trigger free. With worsening hypersensitivity, he reduced social interaction and public activities, and eventually stopped working as a religious leader and teacher.
Marked psychological distress and hopelessness ensued. Contact with his children and grandchildren was greatly curtailed; social gatherings and public events were out of the question; and his health condition put considerable stress on his marriage. Every aspect of his life seemed to be crumbling, and the patient described his quality of life as being exceptionally low.
The patient was referred to a physician who was trained in environmental health sciences for evaluation of his multisystem complaints. History revealed considerable pesticide exposure and street-drug use as a young man. On examination, the patient was found to have nearly 20 amalgam dental fillings, with elevated serum levels of mercury on laboratory testing. Further biochemical and toxicologic assessment demonstrated high ochratoxin levels, with a subsequent home inspection confirming extensive hidden mold—a well-recognized potential source of myriad health problems.5–7 Considerable levels of lead were found in his urine on toxic metal provocation testing,8 but no clear history of lead exposure was identified. The patient was not able to afford laboratory testing for various persistent pesticides and pesticide metabolites; such laboratory analysis is expensive, not readily available, and typically is not covered by health care plans in Canada. Biochemical deficiencies that were identified included low serum levels of copper, manganese, coenzyme Q10, α-tocopherol, and beta-carotene.
Sources of information
This review was prepared by assessing medical and scientific literature from MEDLINE (PubMed), several books, toxicology and allergy journals, conference proceedings, government publications,9 and environmental health periodicals. References cited in identified publications were examined for additional relevant writings. Searching techniques included key word searches with terms related to chemical sensitivity, chronic disease co-occurrence, cluster comorbidity, comorbidity, concurrent comorbidity, food intolerance, environmental illness, multimorbidity, and multisystem disease. We found that there was limited scientific literature on the underlying cause of these disorders, the pathogenesis involved, and the management of multimorbidity with sensitivities (MWS). The first author’s (S.J.G.) professional observations as an environmental health physician were also incorporated into the discussion of management strategies. The format of an integrated clinical review was chosen, as such reviews play a pivotal role in scientific research and professional practice in emerging medical issues with limited primary study and uncharted clinical territory.10
Main message
Definition of terms
Multimorbidity: Multimorbidity is defined as the co-occurrence of 2 or more ongoing or chronic medical conditions that might or might not interact with each other within 1 person. However, there is ambiguity in the understanding of multimorbidity, as current definitions have been described as simplistic and inadequate11 because the term multimorbidity does not delineate between situations of apparently unrelated conditions or multisystem manifestations of a common source that causes illness. For example, while long-term tobacco toxicant exposure might be the single primary determinant for each condition in an individual with chronic obstructive pulmonary disease, bladder cancer, and intractable sinusitis, the patient is still considered to have multimorbidity.
Sensitivity: Sensitivity is a broad term referring to situations in which adverse reactions occur in association with exposure to low concentrations of antigenic stimuli such as foods, inhalants, or chemicals that are well tolerated by most people.12 It is important to note that direct questioning might be necessary to elicit sensitivities to foods or chemicals; patients often neglect to mention such intolerances because they might seem unimportant compared with other presenting complaints.
Environmental health sciences
What is meant by the “environment” and “environmental health sciences”? In 2000, the Centers for Disease Control and Prevention stated that virtually all human disease represents the interaction between the genome and the environment.13 There are essentially 2 parts that make up the functional aspect of the environment in relation to health. In order to thrive, any fully functional system relies on 1) the presence of requisite components and 2) the absence of harmful influences; without these conditions, systems falter. As with any functional system, the human body adheres to this basic scientific principle.14
A 2010 article in Science confirms that most chronic disease results from environmental factors15; that is, most disease results from individuals missing what they need to thrive or being exposed to toxic factors such as pathogens or toxicants that induce harm. This is hopeful information, as the environment, unlike the genome, is modifiable. So, rather than assuming that chronic illness is solely genetic and masking signs and symptoms with assorted therapies, environmental medical practice endeavours to identify and rectify causal determinants that are the sources of the underlying illness.14 Dysfunctional systems have potential for remarkable restoration and improved function if the underlying detrimental state is rectified by providing necessary components and eradicating harmful ones.16
Toxicant damage
The ongoing accumulation of toxic pollutants within the body certainly qualifies as a source of escalating and pervasive harm.17,18 Although patients experiencing MWS are often given a psychiatric diagnosis, an expanding body of scientific literature suggests that harm from bioaccumulated toxicant loads from adverse chemical or biologic exposures (eg, mold exposure) might be causally involved in their illness.19–22
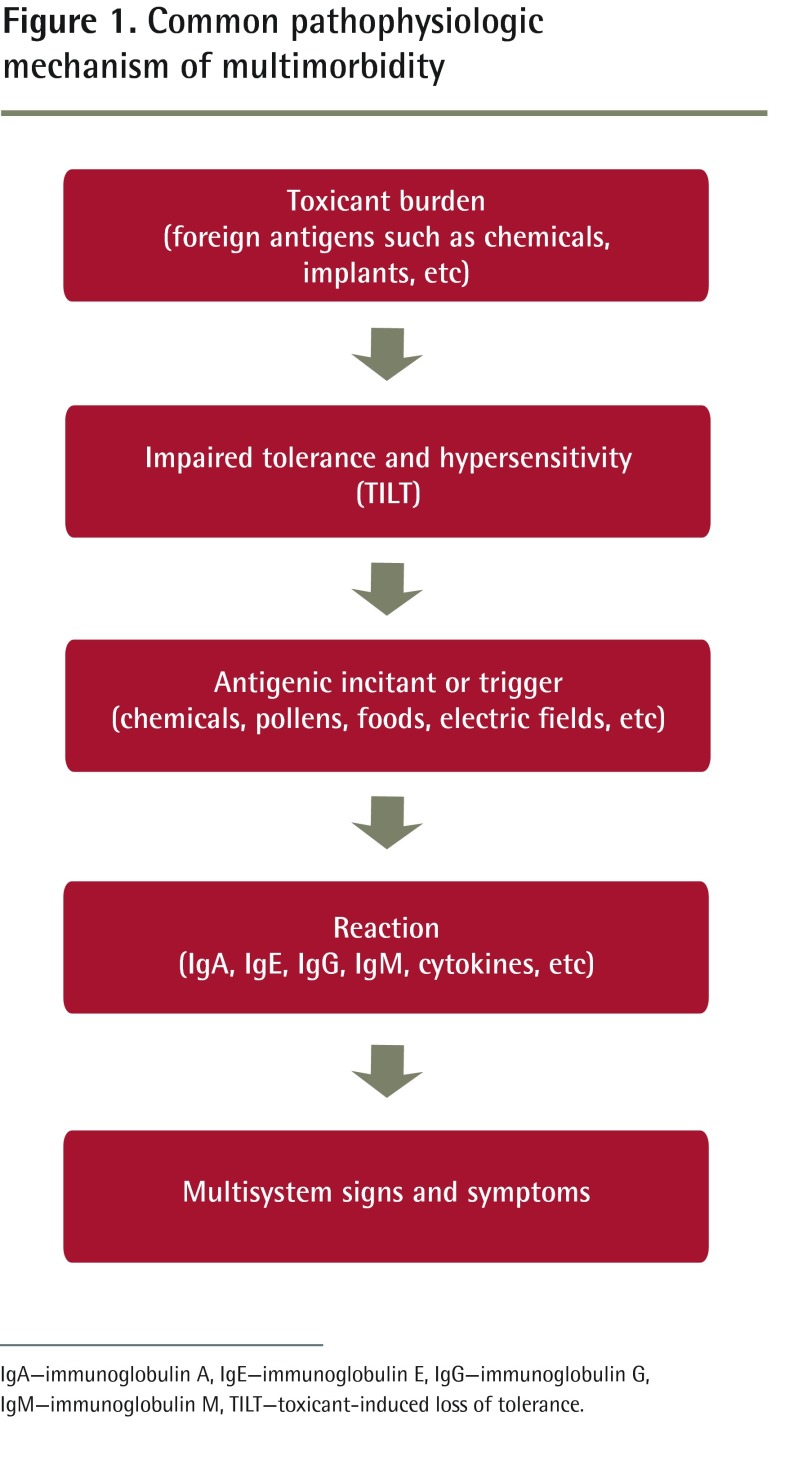
Approximately 85 000 synthetic chemicals have been manufactured over the past few decades, and although only about 2800 are used in high volumes (more than 1 million pounds produced per year), little toxicity information exists for most of these compounds, including many in common use today.23 It has been well established that some of these agents can cause serious damage at small doses24 and that myriad toxicants can bioaccumulate and persist within human tissues for many years or even decades.25 In the scientific literature of late, the underlying cause of several disease states and presentations is being linked to such adverse environmental exposures.17,24,26,27 Multiple mechanisms of harm have been elucidated, including cytotoxicity,28 endocrine disruption,29 enzyme inhibition,30 oxidative stress,31 genotoxicity,32 mitochondrial damage,33 microbiome disruption,34 autonomic nervous system impairment,35 and epigenetic alterations.36 However, there is emerging evidence that bioaccumulated toxicant burdens frequently induce a phenomenon of immune dysregulation37–39 with release of various proteins including pro-inflammatory cytokines frequently resulting in a varied constellation of signs and symptoms involving multiple organ systems.22
Figure 1 presents this common pathophysiologic mechanism of multimorbidity.
Figure 1.
Common pathophysiologic mechanism of multimorbidity
IgA—immunoglobulin A, IgE—immunoglobulin E, IgG—immunoglobulin G, IgM—immunoglobulin M, TILT—toxicant-induced loss of tolerance.
Toxicant-induced loss of tolerance
By toxicant-induced loss of tolerance (TILT), an intriguing mechanism of illness described in the literature since 1997,19,22,37,40 accrued toxicant burdens in humans and animals41 seem to evoke immune dysregulation, leading to hypersensitivity and consequent adverse reactions to commonly encountered compounds in the environment.22,40 A resulting sensitivity-related illness (SRI) ensues with multisystem response to the release of proteins from immune sources, often including antibodies and cell-regulating pro-inflammatory cytokines.22,39
To further expound, the accrual of toxicant compounds foreign to the human body instigates a pathologic hypersensitivity state called TILT, with ensuing inflammation in response to antigenic stimulation.22,37 The toxicant burden might be caused by varying agents including stockpiled chemical compounds stored in tissues, implants, dental materials, chronic infections, and radioactive materials. The toxicant burden does not appear to be agent specific, but myriad types of toxicants alone or in combination have potential to induce SRI.22,42,43 The resulting immune dysregulation manifests as a profound hypersensitivity to commonly encountered substances such as specific foodstuffs, inhalants (eg, pollens), and various chemicals in the environment.44
Multimorbidity presentation
Upon exposure to such inciting triggers, individuals with SRI might experience reactions leading to many apparently unrelated signs and symptoms. These reactions might include allergiclike responses, respiratory compromise, neurologic dysfunction, gastrointestinal damage, fatigue, musculoskeletal impairment, psychiatric difficulties, and other signs and symptoms.19,22,45 The reactions might be immediate or delayed and usually abate after 3 to 5 days in the absence of further exposure. In clinical practice, symptoms often persist for much longer, likely owing to recurrent exposure with insufficient recovery time. If exposure to triggers occurs habitually, inflammation persists and manifests as chronic ongoing body system impairment. It is generally observed that the greater the total toxicant burden, the more severe the hypersensitivity state. Biochemistry is frequently compromised from gastrointestinal dysfunction and malabsorptive states associated with inflammation.
The ensuing multisystem morbidity frequently drives individuals to their primary health providers with apparently inexplicable multisystem health complaints. Most people with such multisystem complaints go from caregiver to caregiver over many years desperately trying to find answers for their various health struggles; these individuals certainly fall into the World Health Organization category of having chronic conditions, described as “health problems that require ongoing management over a period of years or decades.”46 A diagnosis of SRI should be considered whenever a presentation of plural diagnoses or multisystem complaints exists with associated food or chemical sensitivities.
Management
Resolution of multimorbidity follows appropriate assessment and intervention. Treatment is directed into 3 broad categories22,47: resolution of inflammation by incitant avoidance; remediation of biochemistry; and toxicant burden elimination to resolve immune dysregulation and the hypersensitivity state. With alleviation of the TILT state by diminution of the toxicant burden, intolerance of foods and chemicals gradually abates with resumption of normal functioning. Left unrecognized, individuals with SRI often flounder with ongoing symptoms. Detailed information regarding pathophysiologic mechanisms and management strategies can be found in recent scientific literature.19,21,22,25,38,48
Case resolution
The patient’s presentation was consistent with a diagnosis of SRI. Removal of inciting agents was meticulously carried out. In the early stages, the patient initially wore a filter mask designed to preclude particulate and volatile exposures both indoors and outdoors as required. The indoor air environment was initially addressed through a home inventory and associated high-efficiency particulate air filtration. Professional mold remediation was undertaken and follow-up mold testing was clear. Commercial scents, perfumes, and fresheners were eliminated. Common food triggers such as gluten, casein, refined fructose, nightshades, artificial sweeteners, and flavouring agents were temporarily eliminated from the diet.22
With these measures, the patient’s symptoms began to abate steadily and attention was directed to remediating his nutritional biochemistry.49 An organic, traditional whole food diet to minimize further toxicant and pesticide or herbicide exposure was implemented, along with directed supplementation to target specific biochemical deficiencies. With ongoing improvement, elimination of his total toxicant burden was commenced.
Amalgam removal employing exposure precautions and safe replacement materials was systemically done by a dental professional.50–52 A saline nasal rinse with sodium bicarbonate was used for 3 weeks to eliminate residual mold from the sinus area, and detoxification measures were used to facilitate removal of residual mycotoxin.53 General measures to facilitate toxicant elimination were undertaken, including exercise and regular transdermal depuration.25,54,55 High serum levels of trans fatty acid were addressed with dietary counseling.
With incitant avoidance, biochemical remediation, and toxicant elimination, the patient continued to steadily improve. His sensitivities continued to decrease, with diminished frequency and intensity of reactions, and there was dramatic improvement in overall physical and psychological functioning. His multisystem problems including chronic pain and asthma subsided, and all medication was discontinued. The patient recommenced work as a teacher and religious instructor, and he resumed his ability to enjoy daily activities without constant fear of debilitating reactions.
Conclusion
It has been said that “chronic disease is the great epidemic of our time.”56 Most patients with chronic illness now present with multimorbidity and many of these individuals experience associated sensitivities. Multimorbidity with sensitivities generally results in much frustration for both physicians and patients, as no cause is usually found and results of routine laboratory testing are unremarkable.57,58 Psychiatric attribution is commonplace; outcomes are generally poor; and associated health care costs are enormous.
Over the past 4 decades, a plethora of potentially adverse anthropogenic agents have been inadvertently unleashed into the environment for reasons of convenience, beauty, financial gain, safety, and other perceived needs within our culture.17 Increasing evidence indicates that some of these agents, as well as certain biotoxins and toxic elements, might bioaccumulate within the human organism and, after surpassing a certain accrued threshold, disrupted physiology ensues.19,21,22,48 Many adverse effects of toxicant accrual have been recognized, one of which is TILT,37,59 a pathognomonic feature of SRI and the disordered pathway to a clinical presentation of MWS.22
The case we presented illustrates how various toxic exposures and their bioaccumulation within the body can manifest as SRI with associated MWS. Many primary care practitioners and specialists are not yet familiar with this common mechanism of illness or the required interventions to address this affliction. The protocol of removing triggers, optimizing biochemistry, removing future sources of exposure, and eliminating the stockpile of existing toxicants25,60 can be successfully employed to ameliorate the health status of countless patients with previously inexplicable multimorbidity.
EDITOR’S KEY POINTS
Multimorbidity with sensitivities is frustrating for both physicians and patients. Investigations typically reveal no objective abnormality, and clinical management with psychiatric intervention is usually unsuccessful.
The pathophysiologic mechanism toxicant-induced loss of tolerance or TILT is the pathognomonic feature of sensitivity-related illness and the disordered pathway to a clinical presentation of multimorbidity with sensitivities.
Resolution of multimorbidity follows appropriate assessment and intervention. Treatment is directed into 3 broad categories: resolution of inflammation by incitant avoidance; remediation of biochemistry; and toxicant burden elimination to resolve immune dysregulation and the hypersensitivity state (toxicant-induced loss of tolerance).
POINTS DE REPÈRE DU RÉDACTEUR
La multimorbidité avec sensibilités est un problème frustrant à la fois pour les médecins et les patients. Les investigations ne révèlent habituellement aucune anomalie objective et la prise en charge clinique au moyen d’interventions psychiatriques échouent la plupart du temps.
Le mécanisme pathophysiologique de la perte de tolérance induite par des substances toxiques, ou «TILT» en anglais, est la caractéristique pathognomonique de la maladie liée aux sensibilités et la voie désordonnée menant à une présentation clinique de multimorbidité avec sensibilités.
Le règlement de la multimorbidité fait suite à une évaluation et à une intervention appropriées. Le traitement se divise en 3 grandes catégories: l’élimination de l’inflammation par l’évitement des déclencheurs, la restauration de l’état biochimique et l’élimination du fardeau toxique pour remédier à la dysrégulation immunitaire et à l’hypersensibilité (perte de tolérance induite par des substances toxiques).
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
Both authors contributed to the literature search and to preparing the article for submission.
Competing interests
None declared
References
- 1.Genuis SJ. Pandemic of idiopathic multimorbidity. Can Fam Physician. 2014;60:511–4. (Eng), e290–3 (Fr). [PMC free article] [PubMed] [Google Scholar]
- 2.Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L. Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med. 2005;3(3):223–8. doi: 10.1370/afm.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schäfer I, von Leitner EC, Schön G, Koller D, Hansen H, Kolonko T, et al. Multimorbidity patterns in the elderly: a new approach of disease clustering identifies complex interrelations between chronic conditions. PLoS One. 2010;5(12):e15941. doi: 10.1371/journal.pone.0015941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, van den Bos GA. Causes and consequences of comorbidity: a review. J Clin Epidemiol. 2001;54(7):661–74. doi: 10.1016/s0895-4356(00)00363-2. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics, Committee on Environmental Health Toxic effects of indoor molds. Pediatrics. 1998;101(4 Pt 1):712–4. [PubMed] [Google Scholar]
- 6.Curtis L, Lieberman A, Stark M, Rea W, Vetter M. Adverse health effects of indoor molds. J Nutr Environ Med. 2004;14(3):261–74. [Google Scholar]
- 7.Genuis SJ. Clinical medicine and the budding science of mold exposure. Eur J Intern Med. 2007;18(7):516–23. doi: 10.1016/j.ejim.2007.05.005. Epub 2007 Jul 25. [DOI] [PubMed] [Google Scholar]
- 8.Miller NJ, Howard MA. Dimercaptosuccinic acid loading test for assessing mercury burden in healthy individuals. Ann Clin Biochem. 2004;41(Pt 5):421–2. doi: 10.1258/0004563041731664. [DOI] [PubMed] [Google Scholar]
- 9.Sears ME. The medical perspective on environmental sensitivities. Ottawa, ON: Canadian Human Rights Commission; 2007. Available from: www.chrc-ccdp.gc.ca/sites/default/files/envsensitivity_en.pdf. Accessed 2014 Apr 15. [Google Scholar]
- 10.Dijkers MP, Task Force on Systematic Reviews and Guidelines The value of traditional reviews in the era of systematic reviewing. Am J Phys Med Rehabil. 2009;88(5):423–30. doi: 10.1097/phm.0b013e31819c59c6. [DOI] [PubMed] [Google Scholar]
- 11.Mercer SW, Smith SM, Wyke S, O’Dowd T, Watt GC. Multimorbidity in primary care: developing the research agenda. Fam Pract. 2009;26(2):79–80. doi: 10.1093/fampra/cmp020. [DOI] [PubMed] [Google Scholar]
- 12.Cullen MR. The worker with multiple chemical sensitivities: an overview. Occup Med. 1987;2(4):655–61. [PubMed] [Google Scholar]
- 13.Office of Genetics and Disease Prevention, Centers for Disease Control and Prevention . Gene-environment interaction fact sheet. Atlanta, GA: Centers for Disease Control and Prevention; 2000. Available from: www.ashg.org/pdf/CDC%20Gene-Environment%20Interaction%20Fact%20Sheet.pdf. Accessed 2014 Apr 25. [Google Scholar]
- 14.Genuis SJ. What’s out there making us sick? J Environ Public Health. 2012;2012:605137. doi: 10.1155/2012/605137. Epub 2011 Oct 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rappaport SM, Smith MT. Epidemiology. Environment and disease risks. Science. 2010;330(6003):460–1. doi: 10.1126/science.1192603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Genuis SJ. Medical practice and community health care in the 21st century: a time of change. Public Health. 2008;122(7):671–80. doi: 10.1016/j.puhe.2008.04.002. Epub 2008 Jun 4. [DOI] [PubMed] [Google Scholar]
- 17.Genuis SJ. The chemical erosion of human health: adverse environmental exposure and in-utero pollution—determinants of congenital disorders and chronic disease. J Perinat Med. 2006;34(3):185–95. doi: 10.1515/JPM.2006.033. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention, Department of Health and Human Services . Fourth national report on human exposure to environmental chemicals. Atlanta, GA: Centers for Disease Control and Prevention; 2009. Available from: www.cdc.gov/exposurereport/pdf/FourthReport.pdf. Accessed 2009 Jan 18. [Google Scholar]
- 19.Ashford N, Miller C. Chemical exposures. Low levels and high stakes. 2nd ed. New York, NY: John Wiley & Sons; 1998. [Google Scholar]
- 20.Genuis SJ. Chemical sensitivity: pathophysiology or pathopsychology? Clin Ther. 2013;35(5):572–7. doi: 10.1016/j.clinthera.2013.04.003. Epub 2013 May 1. [DOI] [PubMed] [Google Scholar]
- 21.Pall ML. Multiple chemical sensitivity: toxicological questions and mechanisms. In: Ballantyne B, Marrs TC, Syversen T, editors. General and applied toxicology. 3rd ed. London, UK: John Wiley & Sons; 2009. [Google Scholar]
- 22.Genuis SJ. Sensitivity-related illness: the escalating pandemic of allergy, food intolerance and chemical sensitivity. Sci Total Environ. 2010;408(24):6047–61. doi: 10.1016/j.scitotenv.2010.08.047. [DOI] [PubMed] [Google Scholar]
- 23.Goldman LR, Koduru S. Chemicals in the environment and developmental toxicity to children: a public health and policy perspective. Environ Health Perspect. 2000;108(Suppl 3):443–8. doi: 10.1289/ehp.00108s3443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Welshons WV, Thayer KA, Judy BM, Taylor JA, Curran EM, vom Saal FS. Large effects from small exposures. I. Mechanisms for endocrine-disrupting chemicals with estrogenic activity. Environ Health Perspect. 2003;111(8):994–1006. doi: 10.1289/ehp.5494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Genuis SJ. Elimination of persistent toxicants from the human body. Hum Exp Toxicol. 2011;30(1):3–18. doi: 10.1177/0960327110368417. Epub 2010 Apr 16. [DOI] [PubMed] [Google Scholar]
- 26.Crews D, McLachlan JA. Epigenetics, evolution, endocrine disruption, health, and disease. Endocrinology. 2006;147(6 Suppl):S4–10. doi: 10.1210/en.2005-1122. Epub 2006 May 11. [DOI] [PubMed] [Google Scholar]
- 27.Kripke ML. Reducing death from cancer: what will it take? Tumour Biol. 2012;33(5):1275–8. doi: 10.1007/s13277-012-0425-0. Epub 2012 Jun 5. [DOI] [PubMed] [Google Scholar]
- 28.Boyd JM, Huang L, Xie L, Moe B, Gabos S, Li XF. A cell-microelectronic sensing technique for profiling cytotoxicity of chemicals. Anal Chim Acta. 2008;615(1):80–7. doi: 10.1016/j.aca.2008.03.047. Epub 2008 Apr 1. [DOI] [PubMed] [Google Scholar]
- 29.Vandenberg LN, Maffini MV, Sonnenschein C, Rubin BS, Soto AM. Bisphenol-A and the great divide: a review of controversies in the field of endocrine disruption. Endocr Rev. 2009;30(1):75–95. doi: 10.1210/er.2008-0021. Epub 2008 Dec 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vahidnia A, van der Straaten RJ, Romijn F, van Pelt J, van der Voet GB, de Wolff FA. Mechanism of arsenic-induced neurotoxicity may be explained through cleavage of p35 to p25 by calpain. Toxicol In Vitro. 2008;22(3):682–7. doi: 10.1016/j.tiv.2007.12.010. Epub 2007 Dec 31. [DOI] [PubMed] [Google Scholar]
- 31.Bhatti P, Stewart PA, Hutchinson A, Rothman N, Linet MS, Inskip PD, et al. Lead exposure, polymorphisms in genes related to oxidative stress, and risk of adult brain tumors. Cancer Epidemiol Biomarkers Prev. 2009;18(6):1841–8. doi: 10.1158/1055-9965.EPI-09-0197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garry VF. Biomarkers of thyroid function, genotoxicity and agricultural fungicide use. J Biochem Mol Toxicol. 2005;19(3):175. doi: 10.1002/jbt.20073. [DOI] [PubMed] [Google Scholar]
- 33.Mena S, Ortega A, Estrela JM. Oxidative stress in environmental-induced carcinogenesis. Mutat Res. 2009;674(1–2):36–44. doi: 10.1016/j.mrgentox.2008.09.017. Epub 2008 Oct 11. [DOI] [PubMed] [Google Scholar]
- 34.Snedeker SM, Hay AG. Do interactions between gut ecology and environmental chemicals contribute to obesity and diabetes? Environ Health Perspect. 2012;120(3):332–9. doi: 10.1289/ehp.1104204. Epub 2011 Oct 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liao D, Duan Y, Whitsel EA, Zheng ZJ, Heiss G, Chinchilli VM, et al. Association of higher levels of ambient criteria pollutants with impaired cardiac autonomic control: a population-based study. Am J Epidemiol. 2004;159(8):768–77. doi: 10.1093/aje/kwh109. [DOI] [PubMed] [Google Scholar]
- 36.Hou L, Zhang X, Wang D, Baccarelli A. Environmental chemical exposures and human epigenetics. Int J Epidemiol. 2012;41(1):79–105. doi: 10.1093/ije/dyr154. Epub 2011 Dec 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Miller CS. Are we on the threshold of a new theory of disease? Toxicant-induced loss of tolerance and its relationship to addiction and abdiction. Toxicol Ind Health. 1999;15(3–4):284–94. doi: 10.1177/074823379901500302. [DOI] [PubMed] [Google Scholar]
- 38.Pall ML. Explaining “unexplained illness.” Disease paradigm for chronic fatigue syndrome, multiple chemical sensitivity, fibromyalgia, post-traumatic stress disorder, Gulf War syndrome and others. New York, NY: Harrington Park Press; 2007. [Google Scholar]
- 39.De Luca C, Scordo MG, Cesareo E, Pastore S, Mariani S, Maiani G, et al. Biological definition of multiple chemical sensitivity from redox state and cytokine profiling and not from polymorphisms of xenobiotic-metabolizing enzymes. Toxicol Appl Pharmacol. 2010;248(3):285–92. doi: 10.1016/j.taap.2010.04.017. Epub 2010 Apr 27. [DOI] [PubMed] [Google Scholar]
- 40.Miller CS. Toxicant-induced loss of tolerance—an emerging theory of disease? Environ Health Perspect. 1997;105(Suppl 2):445–53. doi: 10.1289/ehp.97105s2445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Overstreet DH, Miller CS, Janowsky DS, Russell RW. Potential animal model of multiple chemical sensitivity with cholinergic supersensitivity. Toxicology. 1996;111(1–3):119–34. doi: 10.1016/0300-483x(96)03370-7. [DOI] [PubMed] [Google Scholar]
- 42.Savage JH, Matsui EC, Wood RA, Keet CA. Urinary levels of triclosan and parabens are associated with aeroallergen and food sensitization. J Allergy Clin Immunol. 2012;130(2):453–60. e7. doi: 10.1016/j.jaci.2012.05.006. Epub 2012 Jun 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nemery B. Late consequences of accidental exposure to inhaled irritants: RADS and the Bhopal disaster. Eur Respir J. 1996;9(10):1973–6. doi: 10.1183/09031936.96.09101973. [DOI] [PubMed] [Google Scholar]
- 44.Katerndahl DA, Bell IR, Palmer RF, Miller CS. Chemical intolerance in primary care settings: prevalence, comorbidity, and outcomes. Ann Fam Med. 2012;10(4):357–65. doi: 10.1370/afm.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Miller CS, Ashford NA. Multiple chemical intolerance and indoor air quality. In: Spengler JD, Samet JM, McCarthy JF, editors. Indoor air quality handbook. New York, NY: McGraw Hill; 2000. [Google Scholar]
- 46.World Health Organization . Innovative care for chronic conditions: building blocks for action. Geneva, Switz: World Health Organization; 2002. [Google Scholar]
- 47.Sears ME, Genuis SJ. Environmental determinants of chronic disease and medical approaches: recognition, avoidance, supportive therapy, and detoxification. J Environ Public Health. 2012;2012:356798. doi: 10.1155/2012/356798. Epub 2012 Jan 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Genuis SJ, Lipp CT. Electromagnetic hypersensitivity: fact or fiction? Sci Total Environ. 2012;414:103–12. doi: 10.1016/j.scitotenv.2011.11.008. Epub 2011 Dec 5. [DOI] [PubMed] [Google Scholar]
- 49.Bralley JA, Lord RS. Laboratory evaluations in molecular medicine. Nutrients, toxicants, and cell regulators. Norcross, GA: The Institute for Advances in Molecular Medicine; 2005. [Google Scholar]
- 50.Colson DG. A safe protocol for amalgam removal. J Environ Public Health. 2012;2012:517391. doi: 10.1155/2012/517391. Epub 2012 Jan 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lindh U, Hudecek R, Danersund A, Eriksson S, Lindvall A. Removal of dental amalgam and other metal alloys supported by antioxidant therapy alleviates symptoms and improves quality of life in patients with amalgam-associated ill health. Neuro Endocrinol Lett. 2002;23(5–6):459–82. [PubMed] [Google Scholar]
- 52.Wojcik DP, Godfrey ME, Christie D, Haley BE. Mercury toxicity presenting as chronic fatigue, memory impairment and depression: diagnosis, treatment, susceptibility, and outcomes in a New Zealand general practice setting (1994–2006) Neuroendocrinol Lett. 2006;27(4):415–23. [PubMed] [Google Scholar]
- 53.Hope J. A review of the mechanism of injury and treatment approaches for illness resulting from exposure to water-damaged buildings, mold and mycotoxins. ScientificWorldJournal. 2013;2013:767482. doi: 10.1155/2013/767482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sears ME, Kerr KJ, Bray RI. Arsenic, cadmium, lead, and mercury in sweat: a systematic review. J Environ Public Health. 2012;2012:184745. doi: 10.1155/2012/184745. Epub 2012 Feb 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Genuis SJ, Birkholz D, Rodushkin I, Beesoon S. Blood, Urine, and Sweat (BUS) Study: monitoring and elimination of bioaccumulated toxic elements. Arch Environ Contam Toxicol. 2011;61(2):344–57. doi: 10.1007/s00244-010-9611-5. Epub 2010 Nov 6. [DOI] [PubMed] [Google Scholar]
- 56.McClusky J. Minimally disruptive medicine. “Epidemic” of chronic disease? BMJ. 2009;339:b3753. doi: 10.1136/bmj.b3753. [DOI] [PubMed] [Google Scholar]
- 57.Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380(9836):37–43. doi: 10.1016/S0140-6736(12)60240-2. Epub 2012 May 10. [DOI] [PubMed] [Google Scholar]
- 58.Hawkes N. Better training is needed to deal with increasing multimorbidity. BMJ. 2012;344:e3336. doi: 10.1136/bmj.e3336. [DOI] [PubMed] [Google Scholar]
- 59.Miller C, Ashford N, Doty R, Lamielle M, Otto D, Rahill A, et al. Empirical approaches for the investigation of toxicant-induced loss of tolerance. Environ Health Perspect. 1997;105(Suppl 2):515–9. doi: 10.1289/ehp.97105s2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jandacek RJ, Genuis SJ. An assessment of the intestinal lumen as a site for intervention in reducing body burdens of organochlorine compounds. Scientific World Journal. 2013;2013:205621. doi: 10.1155/2013/205621. Epub 2013 Feb 7. [DOI] [PMC free article] [PubMed] [Google Scholar]