Abstract
Introduction. The use of videolaryngoscopes is recommended for morbidly obese patients. The aim of the study was to evaluate the Levitan FPS optical stylet (Levitan) vs Lafy-Flex videolaryngoscope (Lary-Flex) in a group of MO patients. Methods. Seventy-nine MO (BMI > 40 kg m−2) patients scheduled for bariatric surgery were included in the study and randomly allocated to the Levitan FPS or Lary-Flex group. The primary endpoint was time to intubation and evaluation laryngoscopic of glottic view. Anesthesiologists were asked to evaluate the glottic view first under direct laryngoscopy using the videolaryngoscope as a standard laryngoscope (monitor display was excluded from use) and then using devices. The secondary endpoint was the cardiovascular response to intubation and the participant's evaluation of such devices. Results. The time to intubation was 8.572.66 sec. versus 5.790.2 sec. for Levitan and Lary-Flex, respectively (P < 0.05). In all cases of CL grade >1 under direct laryngoscopy, the study devices improved CL grade to 1. The Levitan FPS produced a greater cardiovascular response than the Lary-Flex videolaryngoscope. Conclusion. The Lary-Flex videolaryngoscope and the Levitan FPS optical stylet improve the laryngeal visualization in morbidly obese patients, allowing for fast endotracheal intubation, but Lary-Flex produces less cardiovascular response to intubation attempt.
1. Introduction
Obesity is a rising problem amongst population health worldwide. The percentage of obese individuals in the Poland's population is about 12% but in western countries nears 60% [1]. Increased BMI is associated with an increased probability of difficult intubation [2]. This probability is 1.24 times higher with BMI 25–35 kg m−2 and 1.42 times higher with BMI ≥ 35 kg m−2 when compared to nonobese patients [2]. Other research suggests that the probability of difficult intubation is three times [3] or even six times [4] higher in obese patients compared to nonobese patients.
Laryngoscopy may be difficult in obese patients because of elevated chest diameter giving limited space for the laryngoscope positioning, limited neck mobility, and increased amount of fat tissue in the upper airway, including a larger tongue [5, 6]. Because of these challenges, it is recommended to properly position obese patients for intubation [7].
The use of videolaryngoscopes should improve laryngeal view in morbidly obese patients [8, 9]. Although obesity alone is not a risk factor for difficult intubation [10], it is recommended to use videolaryngoscopes as a part of routine practice in anesthesia for morbidly obese patients [11]. The Levitan FPS optical stylet (Clarus Medical, Minneapolis, USA) and Lary-Flex videolaryngoscope (Acutronic, Switzerland) are portable devices for airway management (Figures 1 and 2). A limited number of scientific papers describe clinical experience with these devices in morbidly obese patients. To our knowledge, this is the first prospective randomized study comparing the use of Lary-Flex videolaryngoscope and Levitan FPS in morbidly obese patients.
Figure 1.

Lary-Flex videolaryngoscope (source: manufacturer marketing materials).
Figure 2.

Levitan FPS optical stylet (source: manufacturer marketing materials).
2. Materials and Methods
The study protocol was approved by the Medical University of Lodz Ethics Committee (Protocol number: RNN/752/10/KB, Chairperson: Professor P. Polakowski, December 14, 2010). Eighty morbidly obese (BMI > 40 kg m−2) patients scheduled for bariatric surgery were included into study after receiving written consent. Patients with predicted difficult intubation were excluded from the study: limited mouth opening < 3 cm, Mallampati grade > 3, neck circumflex > 50 cm, and thyromental distance < 6 cm [12]. Patients were randomly allocated to intubate with the Levitan optical stylet or Lary-Flex videolaryngoscope (Figure 3).
Figure 3.
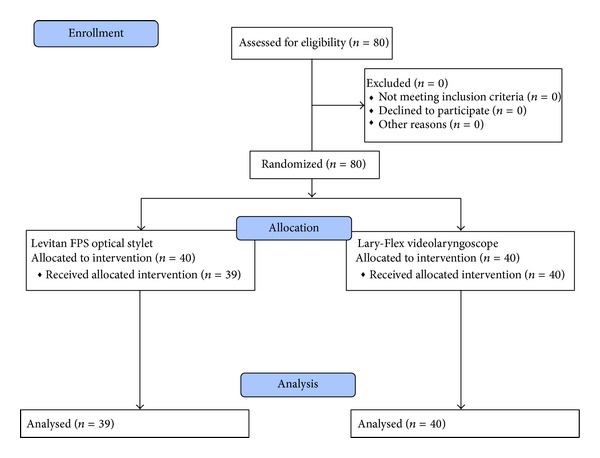
Flow diagram for the study.
For intubation, patients were situated in the head-elevated position [13]. All patients were anesthetized following our institution protocols: induction of anesthesia with propofol 2.0 mg kg−1 of corrected body weight; for muscle relaxation rocuronium 0.6 mg kg−1 of ideal body weight (IBW); fentanyl 0.05 mg kg−1 of IBW. After achieving 100% neuromuscular suppression confirmed by TOF-Watch monitoring, laryngoscopy was performed by various anesthesiologists with ranging degrees of videolaryngoscope experience. All have been working at least few years in the University Hospital Bariatric Centre. Intubation in each patient, allocated to the Levitan group, was facilitated with the use of a laryngoscope and Macintosh-shaped blade. In the Lary-Flex group, intubation was facilitated using videolaryngoscopes as a standard laryngoscope (the monitor display was excluded from use) while also evaluating the glottic view under direct laryngoscopy (C/L 1). Afterwards they were asked to look at the monitor of the videolaryngoscope and facilitate patient intubation (C/L 2). The laryngoscopic conditions were evaluated using the Cormack-Lehane scale. In the Levitan group, anesthesiologists were asked to evaluate the laryngoscopic view using a standard Macintosh blade laryngoscope (C/L 1) and then intubate patient using Levitan FPS optical stylet (C/L 2). Intubation conditions were evaluated using the Krieg scale (Table 1): K1 in the Levitan group using only laryngoscope and in Lary-Flex group using videolaryngoscope as standard laryngoscope and K2 using Levitan FPS and using the whole videolaryngoscope set.
Table 1.
Krieg scale.
| Score | 1 | 2 | 3 | 4 |
|
| ||||
| Laryngoscopy | Easy | Good | Difficult | Impossible |
|
| ||||
| Vocal cords | Open | Move | Closing | Closed |
|
| ||||
| Coughing reflex | Absent | Diaphragm move | Weak | Strong |
Evaluation of intubation conditions: 3-4: ideal; 5-6: good; 8–10: poor; 10–12: difficult.
The time from placing the laryngoscope in the hand to insertion of the endotracheal tube was recorded using the same stopwatch in every case and the number of attempts was recorded. Failed intubation was defined as esophageal intubation or intubation attempt taking longer than 30 seconds. Cardiovascular parameters were recorded before intubation (T1) and during intubation (T2) based on the cardiovascular response to intubation. Subsequent to intubation, participants evaluated whether the devices studied aided intubation conditions or not.
3. Data Analysis
Our primary endpoint was the time required for successful intubation for each device. The secondary endpoints are evaluation of the efficacy of the study devices in improving glottic visualization and the cardiovascular response to intubations.
Statistical analysis was performed with Statistica 10.0 software (Statsoft, Tulsa, OK, USA). For evaluation of data distribution, the Shapiro-Wilk test was used. The Mann-Whitney U test was used for nonpaired categorical and continuous data analysis (time of intubation). For evaluation of numerical scales a Spearman correlation ratio of rang was used. The Chi square test for independent pairs was used with the Yates correction as required (analysis of failed intubation). Post hoc testing was performed with the Fisher LSD test. Kaplan-Meier curves were drawn and a Log-rank test was performed for group comparison. P values lower than 0.05 were considered statistically significant.
4. Results
Complete data was collected in 40 patients in the Levitan group and 39 patients in the Lary-Flex group. Demographic data are presented in Table 2. Results of evaluation of preintubation conditions are presented in Table 3. There were no statistical differences in the demographic profiles of groups or in the preintubation tests. For evaluation of intubation conditions, there were no statistically significant differences (Table 4). In the Levitan group, the intubation time was significantly longer but still within acceptable clinical limits—Table 4, Figure 4. Evaluations of the intubation conditions are presented in Figures 5, 6, and 7. In all cases of CL grade > 1 in direct laryngoscopy the study devices improved CL grade to 1. No complications of intubation were observed.
Table 2.
Demographic data of studied groups.
| Group | Parameter | N | Mean | 95% CI | Median | Minimum | Maximum | Q1 | Q3 | SD | SE | P group Levitan versus Lary-Flex | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Levitan | Age (yrs) | 40 | 40.10 | 36.57 | 43.63 | 39.00 | 19.00 | 60.00 | 32.50 | 48.50 | 11.05 | 1.75 | 0.307822 |
| Weight (kg) | 40 | 126.03 | 119.43 | 132.62 | 123.00 | 100.00 | 200.00 | 109.50 | 139.00 | 20.63 | 3.26 | 0.968712 | |
| Height (cm) | 40 | 168.03 | 165.21 | 170.84 | 165.50 | 154.00 | 190.00 | 163.00 | 172.00 | 8.80 | 1.39 | 0.606690 | |
| BMI (kg/m2) | 40 | 44.58 | 42.73 | 46.42 | 44.14 | 35.15 | 57.75 | 40.28 | 49.06 | 5.77 | 0.91 | 0.821564 | |
|
| |||||||||||||
| Lary-Flex | Age (yrs) | 39 | 38.05 | 34.35 | 41.75 | 35.00 | 20.00 | 64.00 | 30.00 | 47.00 | 11.42 | 1.83 | |
| Weight (kg) | 39 | 124.90 | 119.78 | 130.02 | 125.00 | 95.00 | 160.00 | 115.00 | 132.00 | 15.79 | 2.53 | ||
| Height (cm) | 39 | 167.31 | 164.47 | 170.15 | 165.00 | 152.00 | 190.00 | 162.00 | 170.00 | 8.76 | 1.40 | ||
| BMI (kg/m2) | 39 | 44.99 | 43.28 | 46.70 | 43.82 | 38.75 | 60.97 | 40.77 | 49.08 | 5.28 | 0.85 | ||
95% CI: confidence interval; Q1: quartile 1; Q3: quartile 3; SD: standard deviation; SE: standard error.
Table 3.
Evaluation of preintubation conditions data of studied groups.
| Group | Parameter | N | Mean | 95% CI | Median | Minimum | Maximum | Q1 | Q3 | SD | SE | P value Levitan versus Lary-Flex | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Levitan | Mallampati scale | 40 | 1.28 | 1.11 | 1.44 | 1.00 | 1.00 | 3.00 | 1.00 | 1.50 | 0.51 | 0.08 | 0.960896 |
| Thyromental distance | 40 | 6.78 | 6.57 | 7.00 | 6.70 | 6.0 | 8.10 | 6.25 | 7.30 | 0.67 | 0.11 | 0.705785 | |
|
| |||||||||||||
| Lary-Flex | Mallampati scale | 39 | 1.28 | 1.12 | 1.45 | 1.00 | 1.00 | 3.00 | 1.00 | 2.00 | 0.51 | 0.08 | |
| Thyromental distance | 39 | 6.84 | 6.64 | 7.04 | 6.90 | 6.0 | 8.00 | 6.30 | 7.30 | 0.61 | 0.10 | ||
95% CI: confidence interval; Q1: quartile 1; Q3: quartile 3; SD: standard deviation; SE: standard error.
Table 4.
Evaluation of intubation conditions data of studied groups.
| Group | Parameter | N | Mean | 95% CI | Median | Minimum | Maximum | Q1 | Q3 | SD | SE | P value Levitan versus Lary-Flex | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Levitan | Intubation time | 40 | 8.57 | 7.72 | 9.43 | 8.00 | 5.00 | 18.00 | 7.00 | 9.50 | 2.66 | 0.42 | 0.000000 |
| Number of attempts | 40 | 1.08 | 0.99 | 1.16 | 1.00 | 1.00 | 2.00 | 1.00 | 1.00 | 0.27 | 0.04 | 0.705785 | |
| C/L 1 | 40 | 1.75 | 1.43 | 2.07 | 1.00 | 1.00 | 4.00 | 1.00 | 2.00 | 1.01 | 0.16 | 0.898564 | |
| C/L 2 | 40 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.00 | 0.00 | 1.000000 | |||
| K1 | 40 | 5.15 | 4.39 | 5.91 | 3.50 | 3.00 | 9.00 | 3.00 | 7.00 | 2.38 | 0.38 | 0.848359 | |
| K2 | 40 | 3.60 | 3.25 | 3.95 | 3.00 | 3.00 | 7.00 | 3.00 | 4.00 | 1.08 | 0.17 | 0.651942 | |
|
| |||||||||||||
| Lary-Flex | Intubation time | 39 | 5.79 | 5.40 | 6.19 | 6.00 | 3.00 | 8.00 | 5.00 | 7.00 | 1.22 | 0.20 | |
| Number of attempts | 39 | 1.03 | 0.97 | 1.08 | 1.00 | 1.00 | 2.00 | 1.00 | 1.00 | 0.16 | 0.03 | ||
| C/L I | 39 | 1.72 | 1.44 | 2.00 | 1.00 | 1.00 | 4.00 | 1.00 | 2.00 | 0.86 | 0.14 | ||
| C/L II | 39 | 1.00 | — | — | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.00 | 0.00 | ||
| K1 | 39 | 4.90 | 4.19 | 5.60 | 4.00 | 3.00 | 9.00 | 3.00 | 7.00 | 2.17 | 0.35 | ||
| K2 | 39 | 3.41 | 3.16 | 3.66 | 3.00 | 3.00 | 6.00 | 3.00 | 4.00 | 0.79 | 0.13 | ||
95% CI: confidence interval; Q1: quartile 1; Q3: quartile 3; SD: standard deviation; SE: standard error; C/L 1: evaluation of laryngoscopic view in Cormack-Lehane scale at beginning of intubation: for Levitan group using only laryngoscope, for Lary-Flex group using videolaryngoscope as standard laryngoscope; C/L 2: evaluation of laryngoscopic view using Levitan FPS or looping on monitor of Lary-Flex videolaryngoscope. Intubation conditions were evaluated using Krieg scale K1 in Levitan group using only laryngoscope, in Lary-Flex group using videolaryngoscope as standard laryngoscope and K2 using Levitan FPS and using whole videolaryngoscope set.
Figure 4.

Time for intubation with studied devices (s).
Figure 5.
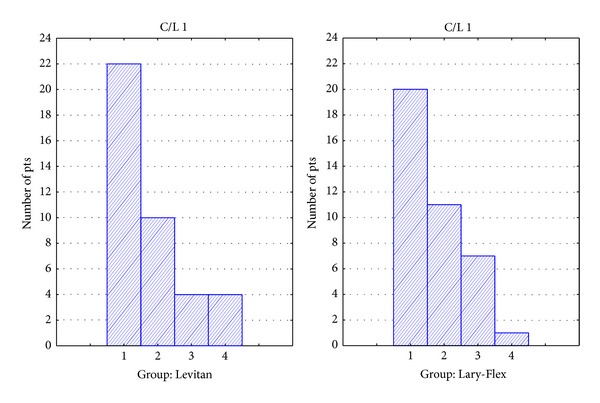
Histogram of evaluation of laryngeal view: Macintosh blade laryngoscope (Levitan group) or Lary-Flex as standard laryngoscope (Lary-Flex group).
Figure 6.
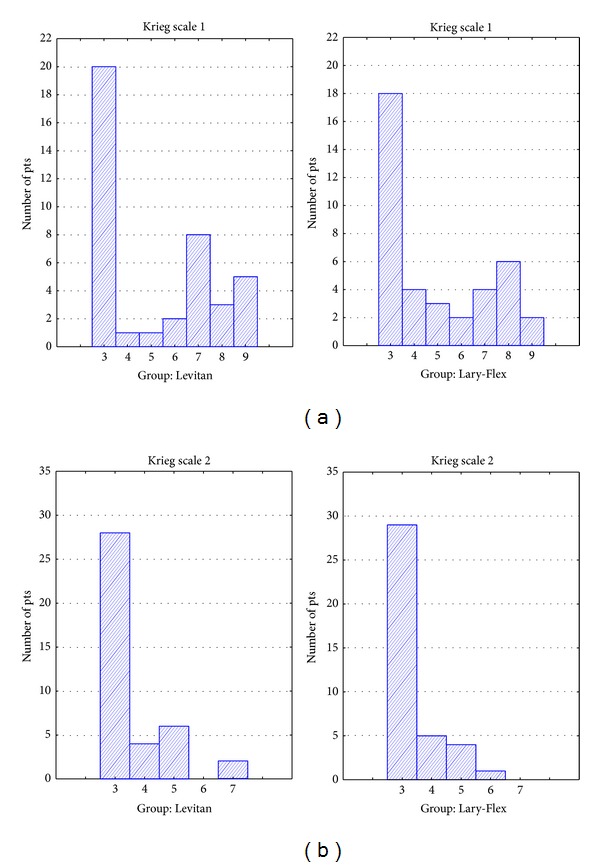
Histograms of evaluation of intubation conditions: Krieg scale 1, conditions using Macintosh blade laryngoscope (Levitan group) or Lary-Flex as standard laryngoscope (Lary-Flex group), Krieg scale 2, conditions using devices.
Figure 7.
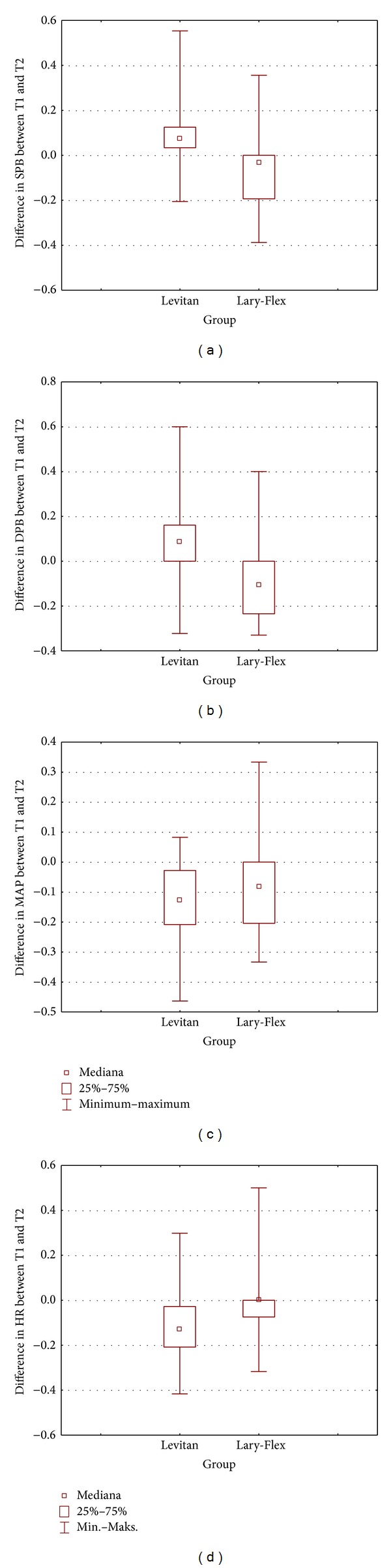
Differences in cardiovascular parameters between time points [%]. T1: preintubation (postinduction), T2: postintubation.
Most of anesthesiologists felt the study devices improved intubation conditions (Table 5). When using the Levitan FPS, the cardiovascular response was significantly larger in comparison to the Lary-Flex videolaryngoscope (Table 6).
Table 5.
Evaluation of participants opinion of potential improvement of intubation conditions.
| Group | Improvement of intubation conditions | |
|---|---|---|
| No | Yes | |
| Levitan | 45.00% | 55.00% |
| Lary-Flex | 48.72% | 51.28% |
Table 6.
Cardiovascular response to intubation attempts.
| Group | Parameter | N | Mean | 95% CI | Median | Minimum | Maximum | Q1 | Q3 | SD | SE | P value Levitan versus Lary-Flex | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Levitan | SPB | T1 | 40 | 119.03 | 114.14 | 123.91 | 119.00 | 94.00 | 143.00 | 105.50 | 130.50 | 15.29 | 2.42 | 0.197238 |
| T2 | 40 | 129.07 | 124.23 | 133.92 | 126.00 | 108.00 | 160.00 | 114.00 | 143.00 | 15.15 | 2.40 | 0.000000 | ||
| DBP | T1 | 40 | 74.25 | 70.81 | 77.69 | 72.50 | 50.00 | 94.00 | 66.50 | 80.50 | 10.76 | 1.70 | 0.007321 | |
| T2 | 40 | 81.03 | 78.07 | 83.98 | 80.00 | 63.00 | 96.00 | 74.00 | 90.00 | 9.24 | 1.46 | 0.000000 | ||
| MAP | T1 | 40 | 102.88 | 97.86 | 107.89 | 101.00 | 71.00 | 132.00 | 94.00 | 110.00 | 15.69 | 2.48 | 0.000004 | |
| T2 | 40 | 88.50 | 85.05 | 91.95 | 88.00 | 66.00 | 110.00 | 81.00 | 97.00 | 10.78 | 1.70 | 0.000000 | ||
| HR | T1 | 40 | 88.53 | 83.42 | 93.63 | 85.00 | 54.00 | 122.00 | 77.50 | 96.00 | 15.95 | 2.52 | 0.000000 | |
| T2 | 40 | 75.88 | 71.89 | 79.86 | 77.50 | 54.00 | 105.00 | 65.00 | 85.00 | 12.46 | 1.97 | 0.000029 | ||
|
| ||||||||||||||
| Lary-Flex | SBP | T1 | 39 | 113.97 | 106.40 | 121.55 | 119.00 | 73.00 | 165.00 | 94.00 | 130.00 | 23.38 | 3.74 | |
| T2 | 39 | 102.51 | 97.31 | 107.71 | 101.00 | 71.00 | 143.00 | 94.00 | 118.00 | 16.04 | 2.57 | |||
| DBP | T1 | 39 | 66.05 | 60.48 | 71.62 | 61.00 | 40.00 | 98.00 | 52.00 | 83.00 | 17.19 | 2.75 | ||
| T2 | 39 | 58.69 | 54.68 | 62.70 | 58.00 | 42.00 | 98.00 | 50.00 | 64.00 | 12.37 | 1.98 | |||
| MAP | T1 | 39 | 81.18 | 75.51 | 86.85 | 78.00 | 54.00 | 112.00 | 66.00 | 98.00 | 17.48 | 2.80 | ||
| T2 | 39 | 73.13 | 68.83 | 77.42 | 73.00 | 52.00 | 112.00 | 64.00 | 78.00 | 13.25 | 2.12 | |||
| HR | T1 | 39 | 64.41 | 61.17 | 67.65 | 66.00 | 48.00 | 82.00 | 53.00 | 72.00 | 9.98 | 1.60 | ||
| T2 | 39 | 63.92 | 61.26 | 66.58 | 66.00 | 51.00 | 77.00 | 55.00 | 70.00 | 8.20 | 1.31 | |||
T1: preintubation (postinduction); T2: postintubation.
5. Discussion
There is a wide range of videolaryngoscopes and other airway devices currently available. Videolaryngoscopes can be divided into subgroups: Macintosh-like blades (e.g., C-Mac, McGrath MAC) and modified blades (e.g., McGrath Series 5, Glidescope). The TruView PCD, which we have used, is a laryngoscope with a modified blade. The glottic view is obtained through the optical view tube incorporated into the blade; a video system can be additionally connected. There are also devices with a special channel for the endotracheal tube, for example, AirTraq, Pentax AWS, and King Vision. Nasotracheal AirTraq intubation, which we used, is modified: it has no channel for the tube. A separate group of airway devices are optical stylets. They combine features of fibroscopes and intubation stylets. The intubation tube should be placed over the optical stylet before using. The operator may use them as intubation stylets together with the laryngoscope. When using rigid optical stylets, the operator can look through the ocular (Bonfils, Levitan FPS) like in a fiberscope and observe the entrance to larynx. This allows for location of entrance to larynx in difficult cases and increases the safety of the procedure. The optical stylets are rigid. Only one of the optical stylets, SensaScope, is a rigid optical stylet with a moving tip similar to fiberscopes.
Each device has its advantages and disadvantages. Videolaryngoscopes are advantageous in that they function very similar to that of standard laryngoscopes. As a result, anesthesiologists can quickly master the skill to effectively employ this device. A possible disadvantage to its use is fogging, which may be resolved in a variety of ways. For example, in the case of the C-Mac, applying antifog solution or for AirTraq the device should be turned on 30 seconds prior to use, to warm up the lens. In the case of the TruView PCD, constant oxygen flow to the lens area prevents fogging and removes secretions from the view. Optical stylets have disadvantages similar to fiberscopes: limited view, possible fogging, and further limitation of view by secretions. The advantage to using optical stylets is that they are similar in use to standard intubation introducers; they are easy to use and requiring minimal training.
The general indications for all devices mentioned above are in situations of both predicted and unexpected difficult intubation. Such devices are becoming more frequently employed in cases of standard patients because they provide optimal prevention of possible intubation injuries in comparison to standard laryngoscopes. In the case of predicted intubation difficulties (like in the case of morbidly obese patients) the fiberscope is preferred; however, the modern airway devices can be a good alternative. For the anesthesiologists who are using the new devices during every day practice they create new opportunities to manage difficult patients in an effective way, including morbidly obese patients [1].
The primary goal was to improve the time required for intubation. As evidenced with use of the Lary-Flex videolaryngoscope, intubation times were slightly improved. Though intubation conditions were comparable, the cardiovascular response to intubation attempts was smaller while employing the Lary-Flex videolaryngoscope. However, the majority of participants stated that both devices seemed to improve intubation conditions.
The use of videolaryngoscopes in morbidly obese patients not only improves glottic view but also makes intubation efforts easier and less traumatic [14, 15]. Therefore, although obesity is not associated with a higher probability of difficult intubation, endotracheal intubation in morbidly obese patients success requires skill and usually more strength. In our study we confirmed previous reports results that standard Mallampati evaluation cannot predict an increased Cormack-Lehane score in morbidly obese patients [16], and in this group of patients it is justified to use videolaryngoscopes as a standard practice. The Lary-Flex videolaryngoscope and Levitan FPS optical stylet proved to be very good, effective, and easy to use even for anesthesiologists with limited experience using videolaryngoscopes. There is no other study evaluating the Lary-Flex or Levitan FPS in morbidly obese patients. In the study describing the use of V-Mac videolaryngoscope (previous version of C-Mac) in morbidly obese patients, Maassen et al. demonstrate similar results to ours: intubation time of 17 sec. but more intubation efforts (average 1.4) [17]. We evaluated the C-MAC videolaryngoscope (Storz, Germany) in morbidly obese patients and we found that it improved the laryngeal view [9]. In this study and the presented study, all cases of the intubation were successful within the recommended time for intubation attempts, which is especially important in morbidly obese patients, in whom desaturation is faster than that in nonobese patients [18]. Maassen et al. compared three videolaryngoscopes: Storz V-MAC, Glidescope Ranger, and McGrath in MO patients [17]. They concluded that the Storz V-MAC was better than the other devices evaluated for intubation of MO patients. Dhonneur et al. proved that the use of the X-Lite Videolaryngoscope improved intubation conditions in MO [15]. Ndoko et al. evaluated the AirTraq in MO and demonstrated similar results to those concluded within our study; AirTraq is a useful device in this group of patients [19]. We evaluated the AirTraq in morbidly obese patients and found that it improves intubation conditions in such patients [20]. Dhonneur et al. also validate similar results [15, 21]. Andersen et al. compared the Glidescope videolaryngoscope and the standard laryngoscope [22]. Slightly longer intubation times were attained; however, significantly better intubation difficulty scale scores were also achieved with use of the Glidescope. The use of a videolaryngoscope is justified in patients in whom the probability of difficult intubation is increased because of coexisting diabetes mellitus, a common comorbidity in morbidly obese patients [23]. Videolaryngoscopes may be used instead of fibroscopes for awake intubation [24, 25].
The cardiovascular response to videolaryngoscopy is smaller when compared to the use of standard Macintosh laryngoscopes in morbidly obese patients [17]. The cardiovascular response while using the Levitan FPS was not previously evaluated in such patient population. As noted in other studies, Levitan FPS should provoke less of a cardiovascular response comparing to standard laryngoscopy [26]. Some authors compared fiberoptic intubation with the use of Bonfils optical stylets. They concluded that both devices require a similar time for successful orotracheal intubation and cause a similar magnitude of hemodynamic response [27]. As evidenced in our study, the response to intubation using the Levitan FPS device was greater than that of the Lary-Flex videolaryngoscope. This may be justified as the Macintosh laryngoscope was employed while using the Levitan FPS device.
The cardiovascular response to the videolaryngoscopy may be similar to insertion of supraglottic devices in morbidly obese patients [28]. By reducing the stress response, videolaryngoscopes may prove advantageous to the standard laryngoscope in obese patients. Although transitory hypertension and tachycardia are probably of little clinical consequence in healthy individuals, they may be a matter of concern in patients with known, or at risk of, cardiovascular disease such as obese patients [28]. Smaller release of stress hormones may influence the postoperative outcome [28]. The response from the cardiovascular system is smaller for videolaryngoscopes than that with standard laryngoscopy [29]. Although fiberoptic intubation in morbidly obese is still recommended, there is no evidence that this technique is superior to videolaryngoscopy [30]. On the contrary, some studies demonstrate that videolaryngoscopy is good alternative to fiberoptic intubation in morbidly obese patients [30].
Both the Lary-Flex videolaryngoscope and the Levitan FPS optical stylet proved to be very effective for intubation of morbidly obese patients. Therefore, we suggest that videolaryngoscopes and optical stylets should be recommended for routine practice in anesthesia for morbidly obese patients.
6. Conclusion
Both devices, the Lary-Flex videolaryngoscope and the Levitan FPS optical stylet, improve the laryngeal view in morbidly obese patients and allowed for efficient endotracheal intubation. However, the Lary-Flex videolaryngoscope produced less cardiovascular response to endotracheal intubation attempt.
Acknowledgment
The authors would like to thank Ms. Corrine Fiddick MD for language correction of the paper.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Leykin Y, Pellis T, del Mestro E, Marzano B, Fanti G, Brodsky JB. Anesthetic management of morbidly obese and super-morbidly obese patients undergoing bariatric operations: hospital course and outcomes. Obesity Surgery. 2006;16(12):1563–1569. doi: 10.1381/096089206779319491. [DOI] [PubMed] [Google Scholar]
- 2.Lundstrøm LH, Møller AM, Rosenstock C, Astrup G, Wetterslev J. High body mass index is a weak predictor for difficult and failed tracheal intubation: a cohort study of 91,332 consecutive patients scheduled for direct laryngoscopy registered in the Danish anesthesia database. Anesthesiology. 2009;110(2):266–274. doi: 10.1097/ALN.0b013e318194cac8. [DOI] [PubMed] [Google Scholar]
- 3.Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance. Anesthesiology. 2005;103(2):429–437. doi: 10.1097/00000542-200508000-00027. [DOI] [PubMed] [Google Scholar]
- 4.Brodsky JB, Lemmens HJM, Brock-Utne JG, Vierra M, Saidman LJ. Morbid obesity and tracheal intubation. Anesthesia and Analgesia. 2002;94(3):732–736. doi: 10.1097/00000539-200203000-00047. [DOI] [PubMed] [Google Scholar]
- 5.Jakubiak J, Gaszynski T, Gaszynski W. Neuromuscular block reversal with sugammadex in a morbidly obese patient with myasthenia gravis. Anaesthesiology Intensive Therapy. 2012;44(1):28–30. [PubMed] [Google Scholar]
- 6.Juvin P, Lavaut E, Dupont H, et al. Difficult tracheal intubation is more common in obese than in lean patients. Anesthesia and Analgesia. 2003;97(2):595–600. doi: 10.1213/01.ANE.0000072547.75928.B0. [DOI] [PubMed] [Google Scholar]
- 7.Brodsky JB, Lemmens HJM, Brock-Utne JG, et al. Anesthetic considerations for bariatric surgery: proper positioning is important for laryngoscopy. Anesthesia and Analgesia. 2003;96(6):1841–1842. doi: 10.1213/01.ANE.0000063165.15467.1B. [DOI] [PubMed] [Google Scholar]
- 8.Marrel J, Blanc C, Frascarolo P, Magnusson L. Videolaryngoscopy improves intubation condition in morbidly obese patients. European Journal of Anaesthesiology. 2007;24(12):1045–1049. doi: 10.1017/S0265021507000889. [DOI] [PubMed] [Google Scholar]
- 9.Gaszynski T. Clinical experience with the C-Mac videolaryngoscope in morbidly obese patients. Anaesthesiology Intensive Therapy. 2014;46(1):14–16. doi: 10.5603/AIT.2014.0003. [DOI] [PubMed] [Google Scholar]
- 10.Ezri T, Medalion B, Weisenberg M, Szmuk P, Warters RD, Charuzi I. Increased body mass index per se is not a predictor of difficult laryngoscopy. Canadian Journal of Anesthesia. 2003;50(2):179–183. doi: 10.1007/BF03017853. [DOI] [PubMed] [Google Scholar]
- 11.Pelosi P, Gregoretti C. Perioperative management of obese patients. Best Practice & Research: Clinical Anaesthesiology. 2010;24(2):211–225. doi: 10.1016/j.bpa.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Gonzalez H, Minville V, Delanoue K, Mazerolles M, Concina D, Fourcade O. The importance of increased neck circumference to intubation difficulties in obese patients. Anesthesia and Analgesia. 2008;106(4):1132–1136. doi: 10.1213/ane.0b013e3181679659. [DOI] [PubMed] [Google Scholar]
- 13.Collins JS, Lemmens HJM, Brodsky JB, Brock-Utne JG, Levitan RM. Laryngoscopy and morbid obesity: a comparison of the “sniff” and “ramped” positions. Obesity Surgery. 2004;14(9):1171–1175. doi: 10.1381/0960892042386869. [DOI] [PubMed] [Google Scholar]
- 14.Maassen R, Lee R, van Zundert A, Cooper R. The videolaryngoscope is less traumatic than the classic laryngoscope for a difficult airway in an obese patient. Journal of Anesthesia. 2009;23(3):445–448. doi: 10.1007/s00540-009-0780-1. [DOI] [PubMed] [Google Scholar]
- 15.Dhonneur G, Abdi W, Ndoko SK, et al. Video-assisted versus conventional tracheal intubation in morbidly obese patients. Obesity Surgery. 2009;19(8):1096–1101. doi: 10.1007/s11695-008-9719-0. [DOI] [PubMed] [Google Scholar]
- 16.Gaszynski T. Standard clinical tests for predicting difficult intubation are not useful among morbidly obese patients. Anesthesia and Analgesia. 2004;99(3, article 956) doi: 10.1213/01.ANE.0000131702.14060.DD. [DOI] [PubMed] [Google Scholar]
- 17.Maassen R, Lee R, Hermans B, Marcus M, van Zundert A. A comparison of three videolaryngoscopes: the macintosh laryngoscope blade reduces, but does not replace, routine stylet use for intubation in morbidly obese patients. Anesthesia and Analgesia. 2009;109(5):1560–1565. doi: 10.1213/ANE.0b013e3181b7303a. [DOI] [PubMed] [Google Scholar]
- 18.Gaszynski T. The effect of pneumoperitoneum on hemodynamic parameters in morbidly obese patients anaesthetized with Sevoflurane or Propofol: a randomized comparison study. Anaesthesiology Intensive Therapy. 2011;43:148–152. [Google Scholar]
- 19.Ndoko SK, Amathieu R, Tual L, et al. Tracheal intubation of morbidly obese patients: a randomized trial comparing performance of Macintosh and Airtraq laryngoscopes. British Journal of Anaesthesia. 2008;100(2):263–268. doi: 10.1093/bja/aem346. [DOI] [PubMed] [Google Scholar]
- 20.Gaszyński T, Gaszyński W. A comparison of the optical AirTraq and the standard Macintosh laryngoscope for endotracheal intubation in obese patients. Anestezjologia Intensywna Terapia. 2009;41(3):145–148. [PubMed] [Google Scholar]
- 21.Dhonneur G, Ndoko S, Amathieu R, Housseini LE, Poncelet C, Tual L. Tracheal intubation using the Airtraq in morbid obese patients undergoing emergency cesarean delivery. Anesthesiology. 2007;106(3):629–630. doi: 10.1097/00000542-200703000-00027. [DOI] [PubMed] [Google Scholar]
- 22.Andersen LH, Rovsing L, Olsen KS. GlideScope videolaryngoscope versus Macintosh direct laryngoscope for intubation of morbidly obese patients: a randomized trial. Acta Anaesthesiologica Scandinavica. 2011;55(9):1090–1097. doi: 10.1111/j.1399-6576.2011.02498.x. [DOI] [PubMed] [Google Scholar]
- 23.Mashour GA, Kheterpal S, Vanaharam V, et al. The extended mallampati score and a diagnosis of diabetes mellitus are predictors of difficult laryngoscopy in the morbidly obese. Anesthesia and Analgesia. 2008;107(6):1919–1923. doi: 10.1213/ane.0b013e31818a9946. [DOI] [PubMed] [Google Scholar]
- 24.Wujtewicz M, Maciejewski D, Misiolek H, et al. Use of dexmedetomidine in adult intensive care unit. Anaesthesiology Intensive Therapy. 2013;45(4):253–260. doi: 10.5603/AIT.2013.0045. [DOI] [PubMed] [Google Scholar]
- 25.Wender R, Goldman AJ. Awake insertion of the fibreoptic intubating LMA CTrach in three morbidly obese patients with potentially difficult airways. Anaesthesia. 2007;62(9):948–951. doi: 10.1111/j.1365-2044.2007.05127.x. [DOI] [PubMed] [Google Scholar]
- 26.Park SY, Kim ST, Shin YD. The effect of tracheal intubation with the Levitan FPS scope or Macintosh laryngoscope on the arterial pressure and heart rate. Anesthesiology and Pain Medicine. 2010;5(2):125–129. [Google Scholar]
- 27.Gupta K, Girdhar KK, Anand R, Majgi SM, Gupta SP, Gupta PB. Comparison of haemodynamic responses to intubation: flexible fibreoptic bronchoscope versus bonfils rigid intubation endoscope. Indian Journal of Anaesthesia. 2012;56(4):353–358. doi: 10.4103/0019-5049.100816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carron M, Veronese S, Gomiero W, et al. Hemodynamic and hormonal stress responses to endotracheal tube and ProSeal Laryngeal Mask airway for Laparoscopic gastric banding. Anesthesiology. 2012;117(2):309–320. doi: 10.1097/ALN.0b013ef31825b6a80. [DOI] [PubMed] [Google Scholar]
- 29.Maassen RLJG, Pieters BMA, Maathuis B, et al. Endotracheal intubation using videolaryngoscopy causes less cardiovascular response compared to classic direct laryngoscopy, in cardiac patients according a standard hospital protocol. Acta Anaesthesiologica Belgica. 2012;63:181–186. [PubMed] [Google Scholar]
- 30.Nicholson A, Smith AF, Lewis SR, Cook TM. Tracheal intubation with a flexible intubation scope versus other intubation techniques for obese patients requiring general anaesthesia. Cochrane Database of Systematic Reviews. 2014;1 doi: 10.1002/14651858.CD010320.pub2.CD010320 [DOI] [PMC free article] [PubMed] [Google Scholar]


