The pathogenesis of encephalitis associated with the respiratory pathogen Mycoplasma pneumoniae is not well understood. A direct infection of the central nervous system (CNS) and an immune-mediated process have been discussed [1]. Recent observations suggest that intrathecally detectable antibodies against the bacterium, which can serve to establish the etiology of encephalitis, may indeed mediate the disease.
Mycoplasma pneumoniae is a major cause of upper and lower respiratory tract infections in humans worldwide, particularly in children [2], [3]. Up to 40% of community-acquired pneumonia in children admitted to the hospital are attributed to M. pneumoniae infection [4]–[7]. Although the infection is rarely fatal, patients of every age can develop severe and fulminant disease. Apart from the respiratory tract infection, M. pneumoniae can cause extrapulmonary manifestations. They occur in up to 25% of manifest M. pneumoniae infections and may affect almost every organ, including the skin as well as the hematologic, cardiovascular, musculoskeletal, and nervous system [8]. Encephalitis is one of the most common and severe complications [1]. M. pneumoniae infection is established in 5%–10% of pediatric encephalitis patients [9], [10], and up to 60% of them show neurologic sequelae [10], [11].
It is important to establish the cause of encephalitis at an early stage in order to specifically treat what can be treated and to avoid unnecessary treatment. The diagnosis of M. pneumoniae encephalitis is challenging. The current diagnostic algorithm of the “Consensus Statement of the International Encephalitis Consortium” [12] recommends for the diagnosis of M. pneumoniae infection in children with encephalitis (1) serology and polymerase chain reaction (PCR) from throat samples (routine studies), and if positive test results and/or respiratory symptoms are present, then (2) additionally PCR in cerebrospinal fluid (CSF) (conditional studies).
However, M. pneumoniae serology and PCR in the respiratory tract cannot discern between colonization and infection in a clinically relevant time frame [13]. The main reason for this is the relatively high prevalence of M. pneumoniae in the upper respiratory tract of healthy children (up to 56%) [13], [14]. The demonstrated positive serological results in such asymptomatic PCR-positive children (positive immunoglobulin (Ig) M in 17%, IgG in 24%, and IgA in 6% of 66 cases) [13] may simply reflect one or more previous encounters with M. pneumoniae and are not necessarily related to the presence of M. pneumoniae in the respiratory tract. It is clear that this may give rise to an overestimation of the M. pneumoniae-related disease burden. A more reliable diagnosis of M. pneumoniae infection may be achieved by using paired patient sera in order to detect seroconversion and/or a 4-fold increase in antibody titers in addition to PCR (Table 1; table references: [13], [15]–[24]). However, such procedures are time-consuming and are therefore neither practicable nor useful in an acutely ill patient.
Table 1. Overview of diagnostic tests for M. pneumoniae.
| Method | Test | Target/Antigen | Antibodies | Specimen | Performance1 | Value | Comments |
| Direct identification of M. pneumoniae | PCR | Different target genes (e.g., P1 gene, 16S rDNA, 16S rRNA, RepMP elements, etc.) | - | Respiratory specimen (nasopharyngeal secretion, pharyngeal swab, sputum, bronchoalveolar lavage), CSF, and other bodily fluids or tissues | High sensitivity, high specificity | RD2 | NAATs provide fast results (in less than a day) and may be earlier than serology (because antibody production requires several days); validation and standardization required for routine diagnostic |
| Culture | - | - | Respiratory specimen (see above) | Low sensitivity, high specificity | AD | Special enriched broth or agar media; isolation takes up to 21 days | |
| Nonspecific serological tests for M. pneumoniae | Cold-agglutinin test (“bedside test”) | Erythrocytes (I antigen) | Cold agglutinins (IgM) | Serum | Low sensitivity, low specificity | -3 | Cold agglutinins target the I antigen of erythrocytes (alternative theory: cold agglutinins target directly M. pneumoniae adhered to erythrocytes); positive in only about 50% and in the first week of symptoms; less well studied in children; cross-reactivity with other pathogens and noninfectious diseases |
| Specific serological tests for M. pneumoniae | CFT | Crude antigen extract with glycolipids and/or proteins | Igs (no discrimination between isotypes) | Serum | Sensitivity and specificity comparable to EIA | -3 | Positive criteria: 4-fold titer increase between acute and convalescent sera or single titer ≥1∶32; cross-reactivity with other pathogens and noninfectious diseases |
| PA | IgM and IgG simultaneously | -3 | See above | ||||
| EIA | Proteins (e.g., adhesion protein P1) and/or glycolipids | IgM, IgG,4 , 5 (IgA)6 | Serum4, CSF5 , 7, other bodily fluids7 | Moderate-high sensitivity, moderate-high specificity | RD | The sensitivity depends on the time point of the first serum and on the availability of paired sera (for seroconversion and/or rise in titer); “gold standard”: 4-fold titer increase as measured in paired sera | |
| Immunoblotting | High sensitivity, high specificity8 | AD | Confirmatory assay | ||||
| IFA | Less sensitive and less specific than EIA | AD | Subjective interpretation |
Abbreviations: AD, advanced diagnostic test; CFT, complement fixation test; CNS, central nervous system; CSF, cerebrospinal fluid; EIA, enzyme immunoassay; IFA, immunofluorescent assay; Ig, immunoglobulin; NAATs, nucleic acid amplification tests; PA, particle agglutination assay; PCR, polymerase chain reaction; RD, routine diagnostic test; RepMP, repeated M. pneumoniae DNA. References: [13], [15]–[24].
Qualitative statements included because of the wide range of test performances, which depend on the assay, the patient cohort (children and/or adults), the reference standard (PCR, culture, and/or serology), the respiratory specimen (for PCR), and the time point of the sample collection after disease onset (for EIA)—e.g., sensitivities and specificities for PCR [17], [18]: 79%–100% and 96%–99%; IgM EIA (in relation to PCR) [19]: 35%–77% and 49%–100%; and for IgG EIA [17], [19]: 37%–100% (no indication on specificity because of missing information on previous M. pneumoniae infections).
Epidemiological differentiation of clinical strains on the basis of differences in the P1 gene by PCR or in the number of repetitive sequences at a given genomic locus by multilocus variable-number tandem-repeat analysis (MLVA) [23].
Largely replaced by EIA.
Kinetics of antibody responses in blood. IgM: onset: within 1 week after the onset of symptoms; peak: 3–6 weeks; persistence: months (to years). IgG: onset and peak: 2 weeks after IgM; persistence: years (to lifelong); reinfection in adults may lead directly to an IgG response in the absence of an IgM response. IgA: onset, peak, and decrease earlier than IgM.
Antibody responses in the CNS differ from blood. There is no switch from an IgM to an IgG response, the pattern of IgM, IgG, and IgA synthesis remains rather constant and depends on the cause, and there is a long-lasting and slow decay of intrathecal antibody synthesis [22]. In M. pneumoniae encephalitis, a dominant IgM response has been observed [29].
The prevalence of serum IgA determined by EIA has been shown to be very low in PCR-positive children with symptomatic respiratory tract infection (2.0%) [13].
To our knowledge, no validated test is available.
Immunoblotting with a combination of at least five specific M. pneumoniae proteins showed sensitivities (in relation to PCR) of 83% (IgM), 51% (IgG), and 64% (IgA), and specificities of 94%–100% (IgM), 98%–100% (IgG), and 93%–97% (IgA) [24].
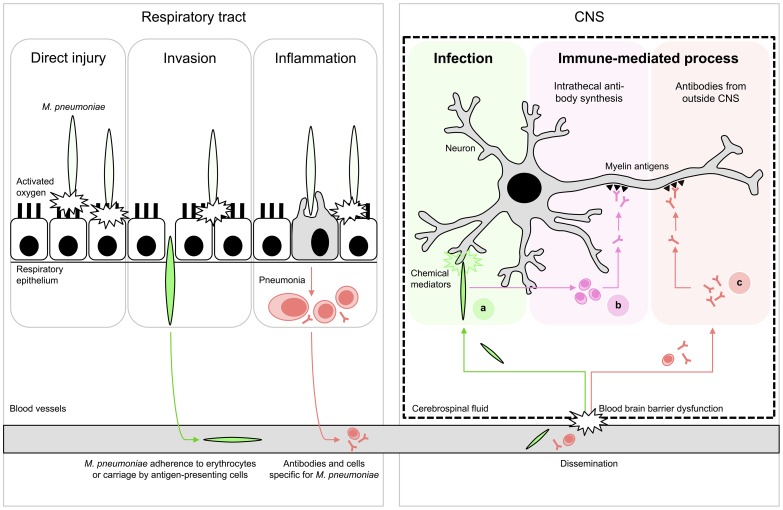
The detection rate of M. pneumoniae by PCR in the CSF of M. pneumoniae encephalitis patients is relatively low (0%–14%) [9], [10], [25], [26]. Moreover, various cases with M. pneumoniae encephalitis in which bacterial DNA could not be detected in the CSF had a more prolonged duration of respiratory symptoms before the onset of encephalitis (>5–7 days) [10], [25], [27]. These cases indicate that M. pneumoniae encephalitis may exemplify a postinfectious phenomenon that manifests after clearance of the bacteria from the CNS or respiratory tract by the immune system. The immune response to M. pneumoniae in the CNS or other sites may also contribute to the encephalitis (Figure 1; figure references: [1]).
Figure 1. Proposed schematic pathomechanisms in M. pneumoniae encephalitis.
(Left) Respiratory tract infection. M. pneumoniae resides mostly extracellularly on epithelial surfaces. Its close association allows the production of direct injury by a variety of local cytotoxic effects. Furthermore, it can induce inflammatory responses, elicited by both adhesion proteins and glycolipid epitopes that result in pneumonia. (Right) Encephalitis. Extrapulmonary disease of the CNS is characterized by systemic dissemination with resultant direct infection and local tissue injury (A) or immune-mediated injury (B,C). The latter may occur as a result of cross-reactive antibodies against myelin components, e.g., gangliosides and galactocerebroside C. These antibodies could theoretically have originated from intrathecal synthesis (B) or from outside the CNS (C). Figure adapted from [1]; see references in the text.
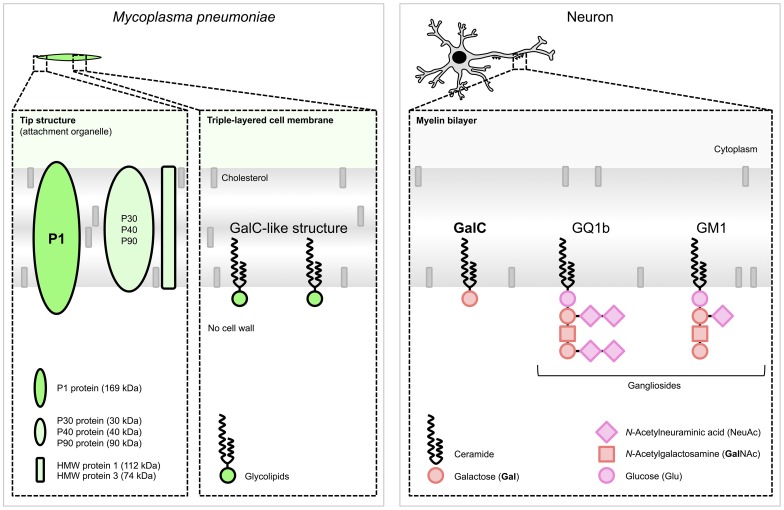
Interestingly, a promising diagnostic marker for M. pneumoniae encephalitis has recently emerged from a few case studies. In one study, intrathecal synthesis of antibodies to M. pneumoniae was reported in 14 cases of M. pneumoniae encephalitis (74%) [28]. The intrathecal production of antibodies is generally considered a highly specific marker for infection of the CNS [22]. All cases that underwent PCR testing (93%) indeed had a positive PCR targeting M. pneumoniae in the CSF [28] even though it has been recently demonstrated that intrathecal antibody responses to M. pneumoniae but not bacterial DNA can be present at the onset of clinical encephalitis [29]. In another study, it was reported that intrathecal antibodies to M. pneumoniae were found to cross-react with galactocerebroside C (GalC) in eight out of 21 (38%) of M. pneumoniae encephalitis cases [30]. All eight cases showed a negative PCR targeting M. pneumoniae in CSF. The cross-reactivity in these cases is likely induced by molecular mimicry between bacterial glycolipids and host myelin glycolipids, including GalC and gangliosides (Figure 2; figure references: [31]–[34]). Cross-reactive, anti-GalC antibodies have previously been detected in patients with Guillain-Barré syndrome (GBS) who suffered from a preceding M. pneumoniae infection [32], [35]–[38]. GBS is a typical postinfectious immune-mediated peripheral neuropathy [39]. In GBS, cross-reactive antibodies cause complement activation and formation of a membrane attack complex at the peripheral nerves, resulting in neuromuscular paralysis. Anti-GalC antibodies have been associated with demyelination in patients with GBS [35], [38]. Moreover, these anti-GalC antibodies cause neuropathy in rabbits that are immunized with GalC [40]. Such antibodies may also be involved in demyelination of central nerve cells in M. pneumoniae encephalitis, as a significant correlation was found between the presence of anti-GalC antibodies in the CSF and demyelination (p = 0.026) [30].
Figure 2. Schematic structures responsible for molecular mimicry between M. pneumoniae and neuronal cells.
(Left) M. pneumoniae adhesion proteins and glycolipids. The immunogenic and major cytadherence proteins P1 and P30 are densely clustered at the tip structure. The P1 protein [31] and glycolipids, e.g., those forming a GalC-like structure [32], elicit cross-reactive antibodies induced by molecular mimicry. (Right) Host myelin glycolipids, to which antibodies were found in patients with M. pneumoniae encephalitis. Glycolipids are organized in specialized functional microdomains called “lipid rafts” and play a part in the maintenance of the cell membrane structure. Abbreviations: GalC, galactocerebroside C; GQ1b, ganglioside quadrosialo 1b; GM1, ganglioside monosialo 1 (the numbers stand for the order of migration on thin-layer chromatography, and the lower-case letters stand for variations within basic structures); HMW, high-molecular-weight. Structures of M. pneumoniae adhesion proteins and host glycolipids are adapted from [33] and [34], respectively.
Anti-GalC antibodies have not only been detected in CSF but also in the serum of M. pneumoniae encephalitis patients [30], [36], [41]–[43], including rates from 13% (2/15) [30] to 100% (3/3) [41], respectively. It is possible that during inflammation the blood-brain barrier (BBB) can become permeable, which would thereby enable antibodies to cross the BBB and cause disease. As a consequence, the cross-reactive antibodies in the CSF of M. pneumoniae encephalitis patients do not necessarily have to be produced intrathecally (Figure 1).
M. pneumoniae infections may also be followed by the production of antibodies to gangliosides, both in patients with GBS and in those with encephalitis. In M. pneumoniae encephalitis, such antibodies were directed against GQ1b [44], [45] or GM1 [46] (Figure 2). Interestingly, anti-GQ1b antibodies are associated with a distinct and severe encephalitis variant, referred to as Bickerstaff brain stem encephalitis [47].
In conclusion, while PCR and serology may be of limited value in the diagnosis of M. pneumoniae encephalitis, the detection of intrathecal antibodies to M. pneumoniae, including cross-reactive antibodies against GalC and gangliosides, may be regarded as a promising new diagnostic tool.
The routine diagnostic workup of M. pneumoniae encephalitis should therefore aim for the detection of M. pneumoniae antibodies in both CSF and serum, in addition to M. pneumoniae PCR in CSF. Intrathecal antibodies can be detected by widely accessible enzyme immunoassays (EIAs) or immunoblotting (Table 1), while intrathecal antibody synthesis can be established either by calculation of an antibody index [22] or through parallel immunoblotting of simultaneously collected CSF and serum samples [48], [49]. Antiganglioside antibodies can be detected routinely by some specialized laboratories, but their detection together with cross-reactive antibodies against GalC primarily serve scientific purposes and may help to clarify M. pneumoniae antibodies' immune target(s). Furthermore, their hypothesized role in the pathogenesis might provide a basis for immunomodulatory treatment in M. pneumoniae encephalitis.
Funding Statement
PMMS is supported by a Swiss National Science Foundation (SNSF) grant (PBZHP3_147290). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Narita M (2009) Pathogenesis of neurologic manifestations of Mycoplasma pneumoniae infection. Pediatr Neurol 41: 159–166. [DOI] [PubMed] [Google Scholar]
- 2. Foy HM (1993) Infections caused by Mycoplasma pneumoniae and possible carrier state in different populations of patients. Clin Infect Dis 17 Suppl 1 S37–S46. [DOI] [PubMed] [Google Scholar]
- 3. Lind K, Benzon MW, Jensen JS, Clyde WA Jr (1997) A seroepidemiological study of Mycoplasma pneumoniae infections in Denmark over the 50-year period 1946–1995. Eur J Epidemiol 13: 581–586. [DOI] [PubMed] [Google Scholar]
- 4. Michelow IC, Olsen K, Lozano J, Rollins NK, Duffy LB, et al. (2004) Epidemiology and clinical characteristics of community-acquired pneumonia in hospitalized children. Pediatrics 113: 701–707. [DOI] [PubMed] [Google Scholar]
- 5. Baer G, Engelcke G, Abele-Horn M, Schaad UB, Heininger U (2003) Role of Chlamydia pneumoniae and Mycoplasma pneumoniae as causative agents of community-acquired pneumonia in hospitalised children and adolescents. Eur J Clin Microbiol Infect Dis 22: 742–745. [DOI] [PubMed] [Google Scholar]
- 6. Principi N, Esposito S, Blasi F, Allegra L (2001) Mowgli study group (2001) Role of Mycoplasma pneumoniae and Chlamydia pneumoniae in children with community-acquired lower respiratory tract infections. Clin Infect Dis 32: 1281–1289. [DOI] [PubMed] [Google Scholar]
- 7. Juven T, Mertsola J, Waris M, Leinonen M, Meurman O, et al. (2000) Etiology of community-acquired pneumonia in 254 hospitalized children. Pediatr Infect Dis J 19: 293–298. [DOI] [PubMed] [Google Scholar]
- 8. Narita M (2010) Pathogenesis of extrapulmonary manifestations of Mycoplasma pneumoniae infection with special reference to pneumonia. J Infect Chemother 16: 162–169. [DOI] [PubMed] [Google Scholar]
- 9. Christie LJ, Honarmand S, Talkington DF, Gavali SS, Preas C, et al. (2007) Pediatric encephalitis: what is the role of Mycoplasma pneumoniae? Pediatrics 120: 305–313. [DOI] [PubMed] [Google Scholar]
- 10. Bitnun A, Ford-Jones EL, Petric M, MacGregor D, Heurter H, et al. (2001) Acute childhood encephalitis and Mycoplasma pneumoniae . Clin Infect Dis 32: 1674–1684. [DOI] [PubMed] [Google Scholar]
- 11. Bitnun A, Ford-Jones E, Blaser S, Richardson S (2003) Mycoplasma pneumoniae encephalitis. Semin Pediatr Infect Dis 14: 96–107. [DOI] [PubMed] [Google Scholar]
- 12. Venkatesan A, Tunkel AR, Bloch KC, Lauring AS, Sejvar J, et al. (2013) Case Definitions, Diagnostic Algorithms, and Priorities in Encephalitis: Consensus Statement of the International Encephalitis Consortium. Clin Infect Dis 57: 1114–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Spuesens EB, Fraaij PL, Visser EG, Hoogenboezem T, Hop WC, et al. (2013) Carriage of Mycoplasma pneumoniae in the upper respiratory tract of symptomatic and asymptomatic children: an observational study. PLoS Med 10: e1001444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wood PR, Hill VL, Burks ML, Peters JI, Singh H, et al. (2013) Mycoplasma pneumoniae in children with acute and refractory asthma. Ann Allergy Asthma Immunol 110: 328–334.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jacobs E (1993) Serological diagnosis of Mycoplasma pneumoniae infections: a critical review of current procedures. Clin Infect Dis 17 Suppl 1 S79–S82. [DOI] [PubMed] [Google Scholar]
- 16.Waites KB, Talkington DF (2004) Mycoplasma pneumoniae and its role as a human pathogen. Clin Microbiol Rev 17: : 697–728, table of contents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Loens K, Goossens H, Ieven M (2010) Acute respiratory infection due to Mycoplasma pneumoniae: current status of diagnostic methods. Eur J Clin Microbiol Infect Dis 29: 1055–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nadal D, Bossart W, Zucol F, Steiner F, Berger C, et al. (2001) Community-acquired pneumonia in children due to Mycoplasma pneumoniae: diagnostic performance of a seminested 16S rDNA-PCR. Diagn Microbiol Infect Dis 39: 15–19. [DOI] [PubMed] [Google Scholar]
- 19. Beersma MF, Dirven K, van Dam AP, Templeton KE, Claas EC, et al. (2005) Evaluation of 12 commercial tests and the complement fixation test for Mycoplasma pneumoniae-specific immunoglobulin G (IgG) and IgM antibodies, with PCR used as the "gold standard". J Clin Microbiol 43: 2277–2285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ozaki T, Nishimura N, Ahn J, Watanabe N, Muto T, et al. (2007) Utility of a rapid diagnosis kit for Mycoplasma pneumoniae pneumonia in children, and the antimicrobial susceptibility of the isolates. J Infect Chemother 13: 204–207. [DOI] [PubMed] [Google Scholar]
- 21. Gavranich JB, Chang AB (2005) Antibiotics for community acquired lower respiratory tract infections (LRTI) secondary to Mycoplasma pneumoniae in children. Cochrane Database Syst Rev 2005: CD004875. [DOI] [PubMed] [Google Scholar]
- 22. Reiber H (1994) Flow rate of cerebrospinal fluid (CSF)— a concept common to normal blood-CSF barrier function and to dysfunction in neurological diseases. J Neurol Sci 122: 189–203. [DOI] [PubMed] [Google Scholar]
- 23. Jacobs E (2012) Mycoplasma pneumoniae: now in the focus of clinicians and epidemiologists. Euro Surveill 17: 1–3. [PubMed] [Google Scholar]
- 24. Dumke R, Strubel A, Cyncynatus C, Nuyttens H, Herrmann R, et al. (2012) Optimized serodiagnosis of Mycoplasma pneumoniae infections. Diagn Microbiol Infect Dis 73: 200–203. [DOI] [PubMed] [Google Scholar]
- 25. Daxboeck F, Blacky A, Seidl R, Krause R, Assadian O (2004) Diagnosis, treatment, and prognosis of Mycoplasma pneumoniae childhood encephalitis: systematic review of 58 cases. J Child Neurol 19: 865–871. [DOI] [PubMed] [Google Scholar]
- 26. Domenech C, Leveque N, Lina B, Najioullah F, Floret D (2009) Role of Mycoplasma pneumoniae in pediatric encephalitis. Eur J Clin Microbiol Infect Dis 28: 91–94. [DOI] [PubMed] [Google Scholar]
- 27. Narita M, Yamada S (2001) Two distinct patterns of central nervous system complications due to Mycoplasma pneumoniae infection. Clin Infect Dis 33: 916–917. [DOI] [PubMed] [Google Scholar]
- 28. Bencina D, Dovc P, Mueller-Premru M, Avsic-Zupanc T, Socan M, et al. (2000) Intrathecal synthesis of specific antibodies in patients with invasion of the central nervous system by Mycoplasma pneumoniae . Eur J Clin Microbiol Infect Dis 19: 521–530. [DOI] [PubMed] [Google Scholar]
- 29. Meyer Sauteur PM, Relly C, Hackenberg A, Stahr N, Berger C, et al. (2014) Mycoplasma pneumoniae Intrathecal Antibody Responses in Bickerstaff Brain Stem Encephalitis. Neuropediatrics 45: 61–63. [DOI] [PubMed] [Google Scholar]
- 30. Christie LJ, Honarmand S, Yagi S, Ruiz S, Glaser CA (2007) Anti-galactocerebroside testing in Mycoplasma pneumoniae-associated encephalitis. J Neuroimmunol 189: 129–131. [DOI] [PubMed] [Google Scholar]
- 31. Jacobs E, Bartl A, Oberle K, Schiltz E (1995) Molecular mimicry by Mycoplasma pneumoniae to evade the induction of adherence inhibiting antibodies. J Med Microbiol 43: 422–429. [DOI] [PubMed] [Google Scholar]
- 32. Kusunoki S, Shiina M, Kanazawa I (2001) Anti-Gal-C antibodies in GBS subsequent to mycoplasma infection: evidence of molecular mimicry. Neurology 57: 736–738. [DOI] [PubMed] [Google Scholar]
- 33. Rottem S (2003) Interaction of mycoplasmas with host cells. Physiol Rev 83: 417–432. [DOI] [PubMed] [Google Scholar]
- 34. Willison HJ, Yuki N (2002) Peripheral neuropathies and anti-glycolipid antibodies. Brain 125: 2591–2625. [DOI] [PubMed] [Google Scholar]
- 35. Ang CW, Tio-Gillen AP, Groen J, Herbrink P, Jacobs BC, et al. (2002) Cross-reactive anti-galactocerebroside antibodies and Mycoplasma pneumoniae infections in Guillain-Barré syndrome. J Neuroimmunol 130: 179–183. [DOI] [PubMed] [Google Scholar]
- 36. Susuki K, Odaka M, Mori M, Hirata K, Yuki N (2004) Acute motor axonal neuropathy after Mycoplasma infection: Evidence of molecular mimicry. Neurology 62: 949–956. [DOI] [PubMed] [Google Scholar]
- 37. Arakawa H, Yuhara Y, Todokoro M, Kato M, Mochizuki H, et al. (2005) Immunoadsorption therapy for a child with Guillain-Barré syndrome subsequent to Mycoplasma infection: a case study. Brain Dev 27: 431–433. [DOI] [PubMed] [Google Scholar]
- 38. Samukawa M, Hamada Y, Kuwahara M, Takada K, Hirano M, et al. (2013) Clinical features in Guillain-Barré syndrome with anti-Gal-C antibody. J Neurol Sci 337: 55–60. [DOI] [PubMed] [Google Scholar]
- 39. van Doorn PA, Ruts L, Jacobs BC (2008) Clinical features, pathogenesis, and treatment of Guillain-Barré syndrome. Lancet Neurol 7: 939–950. [DOI] [PubMed] [Google Scholar]
- 40. Saida T, Saida K, Dorfman SH, Silberberg DH, Sumner AJ, et al. (1979) Experimental allergic neuritis induced by sensitization with galactocerebroside. Science 204: 1103–1106. [DOI] [PubMed] [Google Scholar]
- 41. Nishimura M, Saida T, Kuroki S, Kawabata T, Obayashi H, et al. (1996) Post-infectious encephalitis with anti-galactocerebroside antibody subsequent to Mycoplasma pneumoniae infection. J Neurol Sci 140: 91–95. [DOI] [PubMed] [Google Scholar]
- 42. Kumada S, Kusaka H, Okaniwa M, Kobayashi O, Kusunoki S (1997) Encephalomyelitis subsequent to mycoplasma infection with elevated serum anti-Gal C antibody. Pediatr Neurol 16: 241–244. [DOI] [PubMed] [Google Scholar]
- 43. Sugeno N, Kawaguchi N, Hasegawa T, Kuroda T, Nakashima I, et al. (2012) A case with anti-galactocerebroside antibody-positive Mycoplasma pneumoniae meningoencephalitis presenting secondary hypersomnia. Neurol Sci 33: 1473–1476. [DOI] [PubMed] [Google Scholar]
- 44. Kikuchi M, Tagawa Y, Iwamoto H, Hoshino H, Yuki N (1997) Bickerstaff's brainstem encephalitis associated with IgG anti-GQ1b antibody subsequent to Mycoplasma pneumoniae infection: favorable response to immunoadsorption therapy. J Child Neurol 12: 403–405. [DOI] [PubMed] [Google Scholar]
- 45. Steer AC, Starr M, Kornberg AJ (2006) Bickerstaff brainstem encephalitis associated with Mycoplasma pneumoniae infection. J Child Neurol 21: 533–534. [DOI] [PubMed] [Google Scholar]
- 46. Fusco C, Bonini E, Soncini G, Frattini D, Giovannini S, et al. (2010) Transient basal ganglia and thalamic involvement following Mycoplasma pneumoniae infection associated with antiganglioside antibodies. J Child Neurol 25: 1029–1033. [DOI] [PubMed] [Google Scholar]
- 47. Odaka M, Yuki N, Yamada M, Koga M, Takemi T, et al. (2003) Bickerstaff's brainstem encephalitis: clinical features of 62 cases and a subgroup associated with Guillain-Barré syndrome. Brain 126: 2279–2290. [DOI] [PubMed] [Google Scholar]
- 48. Monteyne P, Albert F, Weissbrich B, Zardini E, Ciardi M, et al. (1997) The detection of intrathecal synthesis of anti-herpes simplex IgG antibodies: comparison between an antigen-mediated immunoblotting technique and antibody index calculations. European Union Concerted Action on Virus Meningitis and Encephalitis. J Med Virol 53: 324–331. [DOI] [PubMed] [Google Scholar]
- 49. Granerod J, Cunningham R, Zuckerman M, Mutton K, Davies NW, et al. (2010) Causality in acute encephalitis: defining aetiologies. Epidemiol Infect 138: 783–800. [DOI] [PubMed] [Google Scholar]