Abstract
Controversy remains regarding the effect of obesity on the survival of patients with ovarian cancer in Asia. This study examined the impact of obesity on the survival outcomes in advanced epithelial ovarian cancer (EOC) using Asian body mass index (BMI) criteria. The medical records of patients undergoing surgery for advanced (stage III and IV) EOC were reviewed. Statistical analyses included ANOVA, chi-square test, Kaplan-Meier survival and Cox regression analysis. Among all 236 patients, there were no differences in overall survival according to BMI except in underweight patients. In a multivariate Cox analysis, surgical optimality and underweight status were independent and significant prognostic factors for survival (HR, 2.302; 95% CI, 1.326-3.995; P=0.003 and HR, 8.622; 95% CI, 1.871-39.737; P = 0.006, respectively). In the subgroup of serous histology and optimal surgery, overweight and obese I patients showed better survival than normal weight patients (P = 0.012). We found that underweight BMI and surgical optimality are independent risk factors for the survival of patients with advanced ovarian cancer. High BMI groups (overweight, obese I and II) are not associated with the survival of advanced EOC patient. However, in the subgroup of EOC patients with serous histology and after optimal operation, overweight and obese I group patients show better survival than the normal weight group patients.
Graphical Abstract
Keywords: Ovarian Neoplasms, Survival, Body Mass Index, Obesity
INTRODUCTION
Ovarian cancer is a highly fatal gynecologic cancer and the fifth leading cause of cancer mortality in women, with 14,030 deaths occurring in the United States per year (1). In Korea, ovarian cancer is the ninth leading cause of death with an age-standardized cancer mortality rate of 2.3 per 100,000 women during 2010 (2). Most cases of ovarian cancer are discovered at an advanced stage and quickly progress, resulting in a poor outcome. The National Cancer Institute's Surveillance, Epidemiology, End Results Program (SEER) reported that 68% of ovarian cancer cases diagnosed during 2002-2008 presented at the late distant stage with very low 5-yr survival rates (< 26%) (3). Due to the rapid progression and low survival rate, there is usually only a short window of time to evaluate the environmental factors affecting the course of the disease.
Obesity is a health problem with increasing prevalence and is directly related to various morbidities. Among gynecologic cancers, hormone-related cancers such as endometrial cancer and breast cancer are associated with obesity (4). Recently, there have been some epidemiologic and experimental studies indicating that abdominal adiposity and weight gain increase ovarian cancer risk. They may also increase tumor invasiveness and tumor cell migration in various cancer types (5, 6). However, there have been only a few clinical studies determining the role of obesity in ovarian cancer outcomes.
Advanced ovarian cancer patients are frequently found in a cachectic state with ascites which may contribute significantly to body weight, but do not counted as real body mass. Most patients with ovarian cancer are operative candidates who then receive adjuvant chemotherapy, which can jeopardize their health status. In Asian populations, the categorizing standard of obesity is different from that applied to people of Western populations, and the incidence of comorbidities is different (7, 8). Therefore, there is still some question regarding whether obesity truly has an adverse effect on the outcome of ovarian cancer among Asian patients.
The aim of this study was to analyze the relationship between obesity and the survival of patients with advanced epithelial ovarian cancer in Korean population.
MATERIALS AND METHODS
A total of 236 patients who underwent staging laparotomy for advanced (stage III and IV) EOC between January 2000 and February 2009 were included. Medical records of 320 patients were retrieved from Korea University Anam Hospital (86 patients), Korea University Guro Hospital (44 patients), Gachon University Gil Medical Center (120 patients), Kyung Hee Medical center at Gangdong (22 patients) and CHA University Hospital (48 patients), Korea. All cases were reviewed for height, weight, age, comorbidities and treatment-specific details. Patients with a non-epithelial tumor histology, synchronous or metachronous tumors, borderline tumors and early stage (stage I and II) ovarian cancer were excluded. Other patients with a different chemotherapy regimen or with missing data were also excluded. Patients who did not complete at least six cycles of chemotherapy were excluded.
The patients' primary surgery was performed at the gynecological department of one of the five different hospitals, and the staging procedure was done at the time of surgery. Cytoreductive surgery was considered to have achieved optimal debulking when the residual disease was <1 cm. Postoperatively, all patients received at least six cycles of taxane-platin based chemotherapy. Four patients had three or fewer cycles of neoadjuvant chemotherapy before staging operation and no patient had intraperitoneal chemotherapy.
Recurrence was defined as the earliest date when abnormal findings were detected on a follow-up CT scan. Time of survival was defined as the time from diagnosis to recurrence for progression free survival (PFS), and from diagnosis to death irrespective of cause for overall survival (OS). For censored cases survival was calculated from the last clinical visit.
Patients were evaluated for complications, rates of optimal debulking (residual disease<1 cm), PFS, OS and platinum sensitivity, i.e. recurrence more than 6 months from completion of platinum-based chemotherapy.
Body weight and height were checked at diagnosis which means within three months before operation. Body mass index (BMI) was calculated using the Quetelet's index expressed in kg/m2 and categorized into five groups: underweight (BMI<18.5), normal (18.5≤BMI<23), overweight (23≤BMI<25), obese I (25≤BMI<30) and obese II (30.0≤BMI). The BMI cut-off points followed those proposed by the regional office for Western Pacific Region of World Health Organization (WHO) (WPRO criteria, 2000) (9).
Survival was analyzed using the Kaplan-Meier method and compared using a log-rank test. Cox-regression was used to reveal risk factors related to survival. Statistical analysis was performed using the chi-square test, Fisher's exact test and ANOVA, where appropriate.
Ethics statement
This study was approved by institutional review board of Korea University Anam Hospital (ED10313) and 4 other hospitals. The subjects' informed consent was waived by the boards due to the observation design of this study.
RESULTS
Five (2.1%), 85 (36.0%), 69 (29.2%), 64 (27.2%), and 13 (5.5%) patients were underweight, normal weight, overweight, obese I and obese II, respectively. Age at diagnosis significantly differed across the five BMI groups (P = 0.003). Overweight and obese I patients were older than the other BMI groups. The initial Hb of underweight patients (10.4±1.8 g/dL) was significantly lower compared to the other BMI groups (P = 0.049). No significant differences were seen in parity, medical history, surgery optimality, stage, CA 125, CA 19-9 and follow-up time among the five BMI categories. Histologic characteristics showed an even distribution across the five BMI groups, and the serous type comprised majority for each BMI group (Table 1).
Table 1.
General characteristics of patients (N=236)
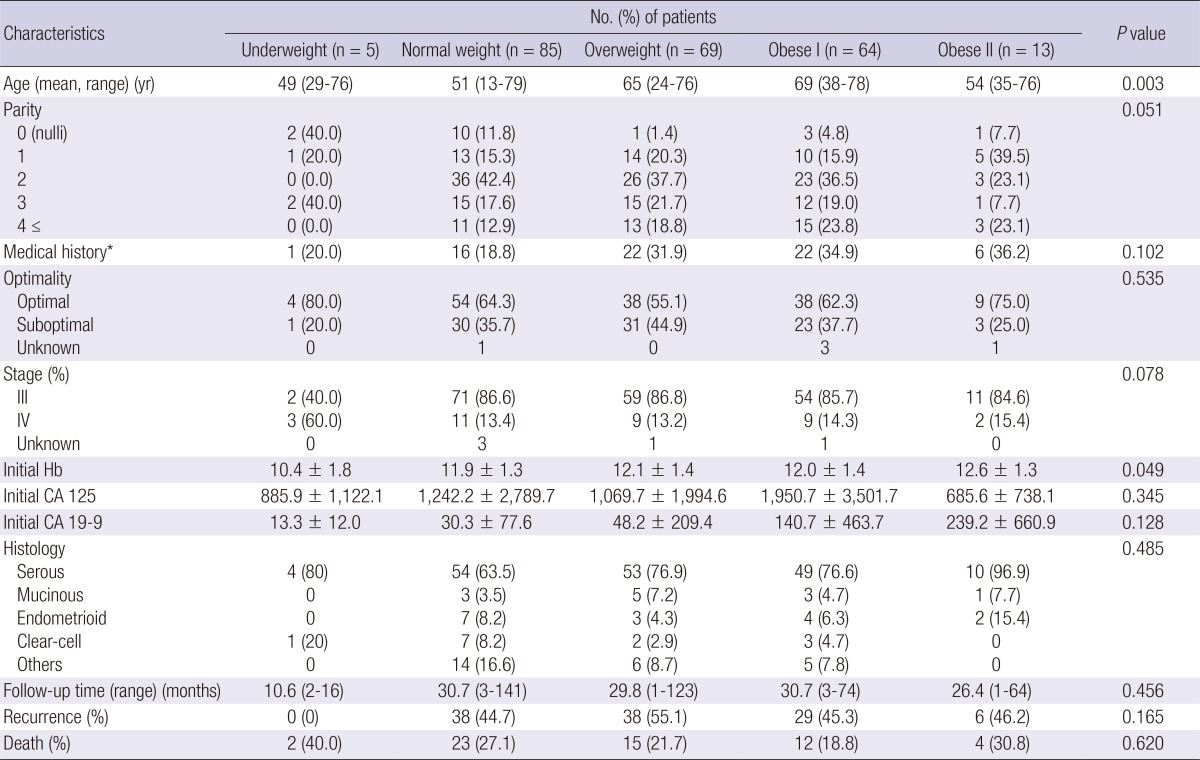
*Medical disease history includes diabetes mellitus, hypertension, thyroid disease, etc. Hb, hemoglobin.
The median PFS was 9.5 months (1-132 months) and the 5-yr OS was 47%, considering all stages for the whole series (data not shown). During the median follow-up period of 21.4 months (range, 1-141 months), a total of 56 deaths were recorded (23.7%) with an even distribution across the BMI strata (Table 1).
Table 2 shows the univariate and multivariate hazard ratios (HRs) and 95% confidence intervals (CIs) for ovarian cancer mortality associated with BMI and surgical optimality. Underweight patients (BMI<18.5) had a significantly higher mortality compared to patients in the reference group (18.5≤BMI<23) (HR, 8.622; 95% CI, 1.871-39.737; P=0.006). Other BMI groups (23≤BMI) were not associated with ovarian cancer mortality.
Table 2.
Risk factors for mortality in stage III and IV ovarian cancer patients
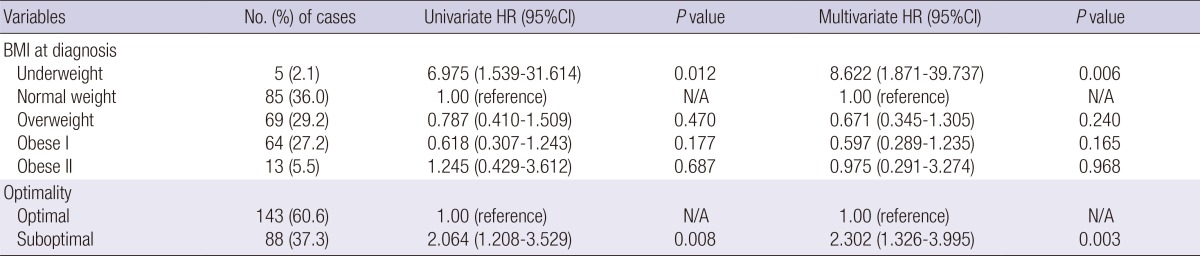
Adjusted for age at diagnosis, parity, medical history, stage, histologic subtype and initial lab findings (Hb, CA 125, CA 19-9). N/A, not applicable.
The HR and 95% CI comparing women who had non-optimal surgery versus patients with optimal surgery was 2.302 (95% CI, 1.326-3.995; P=0.003). Our analysis did not find any other factors affecting the survival of stage III and IV ovarian cancer (data not shown).
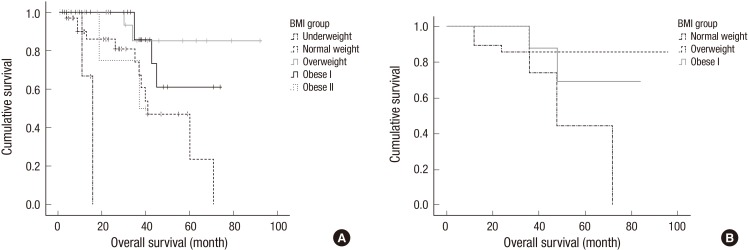
In the subcohort analysis, within 97 patients with serous ovarian cancers after optimal surgery, underweight patients had significantly poorer survival than other BMI groups (P=0.031) and obese II patients showed no significant difference in survival compared to normal weight, overweight and obese I patients (P=0.097) (Fig. 1A). However, among the three mid-range BMI groups overweight and obese I patients had a higher rate of survival than normal weight patients (P=0.012) (Fig. 1B).
Fig. 1.
Survival of patients with serous ovarian cancer after optimal surgery (n = 97). (A) Underweight patients have significantly poorer survival than other BMI groups (P = 0.031) and obese II patients showed no significant difference in survival compared to normal weight, overweight and obese I patients (P = 0.097). (B) However, among three mid-range BMI groups, overweight and obese I patients have a higher rate of survival than normal weight patients (P = 0.012).
DISCUSSION
Ovarian cancer is one of the most lethal cancers in women; however, there is little data available on the precise nature of the relationship between obesity and ovarian cancer mortality. Furthermore, there is lack of study about the effect of obesity to the ovarian cancer survival in Asian population. This study examined whether BMI group following Asian criteria has an association with the ovarian cancer survival. We found that an underweight BMI and surgical optimality are independent risk factors for the survival of patients with advanced ovarian cancer. However, there was no significant relationship between ovarian cancer survival and the other four BMI groups. Only in the subgroup analysis with a serous histology and with optimal surgery, patients in the overweight and obese I groups had better survival than normal weight patients.
The median PFS and 5-yr OS of our data (15 months and 47%, respectively) are pretty better than the PFS and OS expected in advanced ovarian cancer patients. It seems because only patients who completed over six cycles of chemotherapy were included in this study.
These results are notable because to date obesity has been shown to have only two effects on ovarian cancer survival, either a worse prognosis or no effect. Pavelka et al. (10) reported that obesity was independently associated with both shorter time to recurrence and shorter overall survival for patients with advanced ovarian cancer. Our study is both of a different ethnic population and a large sample size. According to study by Yang et al. (11), obesity did not influence EOC survival. However, BMI was measured one year before the diagnosis of ovarian cancer, and the BMI definition used were different from those in our study. The pathophysiology of both obesity and cancer biology is complicated, and therefore, the approach to reveal the association between them should be carefully considered.
Despite the technical challenge that may be present during surgery, our patients had consistent optimal cytoreduction rates across the BMI groups. This important factor in the rate of survival was emphasized in the study of Matthews et al. who suggested that maximal effort should be directed towards debulking tumor mass in obese patients with EOC (12). They reported that survival rates are similar between obese and non-obese patients when optimal debulking status is the same.
Underweight patients in our study showed a significantly poor survival rate than other BMI groups. Although elevated BMI is associated with an increased prevalence of comorbidities, the survival rate of obese II patients was not different from normal weight patients. These findings are similar to a study done by Skírnisdóttir and Sorbe (13). However, the study population in underweight and obese II groups was very small (five and thirteen, respectively) so, we obtained the reliability of our results through subgroup analysis with normal, overweight and obese I patients.
Serous carcinoma is the most common type of ovarian cancer with a frequency of over 90% (14). Nearly all comprehensively staged patients present in advanced stage with tumor disseminated throughout the abdominal and pelvic cavities. Some characteristics of serous carcinoma, including early metastasis and dissemination, can be key targets for improving the prognosis of overweight and obese I patients. It is possible that overweight status in Asians with advanced ovarian cancer is a protective factor since Asian obesity appears to be associated with a better prognosis than Western obesity. Overweight and obese I patients may be resistant to the toxicity of chemotherapy due to better initial nutritional status. One potential confounder in advanced serous ovarian cancer is that there is a discrepancy between real body mass and BMI due to the burden of ascites and multi-organ metastasis.
The International Obesity Task Force of the WHO proposed a system of classification based on BMI, and selected a BMI of 30.0 as the cutoff point for obesity based on mortality and morbidity outcomes (15). In recent years, accumulating evidence has suggested that the WHO criteria for classifying obesity in adult Caucasians may not be appropriate for Asian populations. Asian populations have a high level of abdominal fat at a lower BMI relative to Caucasians, and show an increasing trend toward obesity. Therefore, the Regional Office for the Western Pacific Region of the WHO, the International Association for the Study of Obesity and the International Obesity Task Force proposed a separate classification of obesity for Asian population in 2000. This led to the proposal that overweight adults be designed as such in Asia with a BMI≥23.0, and that obesity be defined by a BMI≥25.0 (WPRO criteria) (9). To the best of our knowledge, this is the first study analyzing ovarian cancer survival using the Asian BMI criteria. However, there are still many unanswered questions about the association between Asian BMI criteria and ovarian cancer survival.
Some strengths and limitations of the present study should be considered when interpreting these findings. Strengths include appropriate BMI criteria for Asian patients, subgroup analysis excluding the effects of important variables, directly measured anthropometric variables and a study population consisting of advanced epithelial ovarian cancer. To the best of our knowledge, this is the first epidemiologic evidence showing that overweight and obese status is associated with a better prognosis.
With regard to limitations, a history of medical disease was not detailed for patients enrolled in the study. Nevertheless, overweight and obese I patients had better outcomes despite being older and potentially being at higher risk for cardiovascular disease. All patients were Korean. Further large scale studies including other Asian countries will be needed to confirm the observed associations in this study.
In conclusion, underweight and surgical optimality are independent risk factors for advanced ovarian cancer survival in Korean patients. BMI does not influence the survival of advanced EOC patients except in underweight patients. In the subgroup of serous histology and optimal debulking surgery, patients of the overweight and obese I groups have higher rates of survival than normal-weight patients. These results provide a useful reference for planning further studies and for predicting the prognosis of Asian patients with ovarian cancer.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30. doi: 10.3322/caac.21166. [DOI] [PubMed] [Google Scholar]
- 2.Jung KW, Won YJ, Kong HJ, Oh CM, Seo HG, Lee JS. Cancer statistics in Korea: incidence, mortality, survival and prevalence in 2010. Cancer Res Treat. 2013;45:1–14. doi: 10.4143/crt.2013.45.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, Altekruse SF, Kosary CL, Ruhl J, Tatalovich Z, et al. Previous version: SEER Cancer Statistics review, 1975-2009 (vintage 2009 populations) [accessed on 1 March 2013]. Available at http://seer.cancer.gov/archive/csr/1975_2009_pops09.
- 4.Ballard-Barbash R, Swanson CA. Body weight: estimation of risk for breast and endometrial cancers. Am J Clin Nutr. 1996;63:437S–441S. doi: 10.1093/ajcn/63.3.437. [DOI] [PubMed] [Google Scholar]
- 5.Canchola AJ, Chang ET, Bernstein L, Largent JA, Reynolds P, Deapen D, Henderson KD, Ursin G, Horn-Ross PL. Body size and the risk of ovarian cancer by hormone therapy use in the California Teachers Study cohort. Cancer Causes Control. 2010;21:2241–2248. doi: 10.1007/s10552-010-9647-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma D, Wang J, Fu PP, Sharma S, Nagalingam A, Mells J, Handy J, Page AJ, Cohen C, Anania FA, et al. Adiponectin antagonizes the oncogenic actions of leptin in hepatocellular carcinogenesis. Hepatology. 2010;52:1713–1722. doi: 10.1002/hep.23892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, Joshi SR, Sadikot S, Gupta R, Gulati S, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009;57:163–170. [PubMed] [Google Scholar]
- 8.Shiwaku K, Anuurad E, Enkhmaa B, Nogi A, Kitajima K, Shimono K, Yamane Y, Oyunsuren T. Overweight Japanese with body mass indexes of 23.0-24.9 have higher risks for obesity-associated disorders: a comparison of Japanese and Mongolians. Int J Obes Relat Metab Disord. 2004;28:152–158. doi: 10.1038/sj.ijo.0802486. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization; International Association for the Study of Obesity; International Obesity Task Force. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia; 2000. [Google Scholar]
- 10.Pavelka JC, Brown RS, Karlan BY, Cass I, Leuchter RS, Lagasse LD, Li AJ. Effect of obesity on survival in epithelial ovarian cancer. Cancer. 2006;107:1520–1524. doi: 10.1002/cncr.22194. [DOI] [PubMed] [Google Scholar]
- 11.Yang L, Klint A, Lambe M, Bellocco R, Riman T, Bergfeldt K, Persson I, Weiderpass E. Predictors of ovarian cancer survival: a population-based prospective study in Sweden. Int J Cancer. 2008;123:672–679. doi: 10.1002/ijc.23429. [DOI] [PubMed] [Google Scholar]
- 12.Matthews KS, Straughn JM, Jr, Kemper MK, Hoskins KE, Wang W, Rocconi RP. The effect of obesity on survival in patients with ovarian cancer. Gynecol Oncol. 2009;112:389–393. doi: 10.1016/j.ygyno.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 13.Skírnisdóttir I, Sorbe B. Body mass index as a prognostic factor in epithelial ovarian cancer and correlation with clinico-pathological factors. Acta Obstet Gynecol Scand. 2010;89:101–107. doi: 10.3109/00016340903322735. [DOI] [PubMed] [Google Scholar]
- 14.Barakat RR, Berchuck A, Markman M, Randall ME. Principles and practice of gynecologic oncology. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2013. [Google Scholar]
- 15.World Health Organization. Obesity: preventing and managing the global epidemic. Geneva: World Health Organization; 2000. [PubMed] [Google Scholar]