Abstract
Cases of metastases to the thyroid gland seem to be increasing in recent years. The clinical and ultrasonographic findings of diffuse metastases have been sparsely reported. Thirteen cases of diffuse metastases to the thyroid gland were documented by thyroid ultrasonography-guided fine needle aspiration cytology between 2004 and 2013. We retrospectively reviewed the patients with diffuse thyroid metastases. The most common primary site was the lung (n=9), followed by unknown origin cancers (n=2), cholangiocarcinoma (n=1), and penile cancer (n=1). Eleven patients were incidentally found to have thyroid metastases via surveillance or staging FDG-PET. Other 2 patients were diagnosed during work-up for hypothyroidism and palpable cervical lymph nodes. On ultrasonography, the echogenicity of the enlarged thyroid gland was heterogeneously hypoechoic or isoechoic, and reticular pattern internal hypoechoic lines were observed without increased vascularity found by power Doppler ultrasonography (3 right lobe, 2 left lobe, and 8 both lobes). In the 8 patients who had involvement of both lobes, 3 had hypothyroidism. In conclusion, ultrasonographic finding of diffuse metastasis is a diffusely enlarged heterogeneous thyroid with reticular pattern internal hypoechoic lines. Thyroid function testing should be performed in all patients with diffuse thyroid metastases, especially those with bilateral lobe involvement.
Graphical Abstract
Keywords: Thyroid, Diffuse, Metastasis, Ultrasonography, Fine Needle Aspiration Cytology
INTRODUCTION
The thyroid gland has an abundant arterial supply. Despite this, metastases to the thyroid gland have been reported in only 1.4%-3% of all patients who have surgery for thyroid malignancy (1, 2, 3). This low incidence is possibly due to a fast arterial flow through the thyroid; and high oxygen and iodine content of the thyroid gland may inhibit the settling and growth of metastatic cells (4). In addition, the relatively short life expectancy of patients with advanced non-thyroid malignancies discourages the evaluation of newly detected thyroid lesions. However, the incidence in autopsy studies has been variable, with rates from 0.5% in an unselected autopsy study to 24% in autopsies of patients with non-thyroid malignancies (5,6, 7, 8). The incidence in clinical studies has been gradually increasing because of the use of high-resolution ultrasonography (US) and frequent use of fine-needle aspiration cytology (FNAC) in suspected lesions (1, 4, 9, 10, 11). The typical US findings of metastases to the thyroid gland consist of hypoechoic nodules with ill-defined margins and intranodular vascularization; however, diffuse metastases have been sparsely reported. The aim of this study was to determine ultrasonographic findings and clinical characteristics of diffuse metastases to the thyroid gland.
MATERIALS AND METHODS
Patients
Patients who were diagnosed with thyroid metastases from non-thyroid malignancies from April 2004 to February 2013 at the Chonnam National University Hwasun Hospital were examined retrospectively. Among them, patients who had abnormal thyroid lesions on 18F-FDG PET (fluoro-deoxyglucose positron emission tomography) or had evidence of thyroid dysfunction on laboratory evaluation during the initial or follow-up evaluations for the primary malignancy were included. Thyroid ultrasonographic examination and fine needle aspiration were performed for these patients.
Thyroid ultrasonography and fine needle aspiration cytology
We used high-resolution ultrasonography using a 5-13 MHz linear transducer (Logiq9, GE Medical system, Milwaukee, WI, USA or ACUSON Antares, Siemens Medical Solutions, Malvern, PA, USA). Diffuse thyroid enlargement with a uniform or discretely irregular echo pattern was examined by FNAC with ultrasonographic guidance. Thyroid US and US-FNAC were performed by a single endocrinologist. FNAC was performed using a 25-27 G needle without local anesthesia, and specimens were obtained from multiple sites within enlarged lobe, because there was no discrete nodular lesion. A minimum of 3 specimens were aspirated and placed onto 3 slides. Specimens were fixed in ethanol immediately after smearing and were stained with Papanicolaou stain. Diagnosis of metastases to the thyroid gland was confirmed cytologically in all cases and reviewed by additional pathologist.
Thyroid hormone test
Thyroid hormone (free T4, FT4) and thyroid stimulating hormone (TSH) were measured by electrochemical luminescence immunoassay (ECLIA; Roche Diagnostics, Mannheim, Germany) and Elecsys and Cobase analyzer kits (Roche Diagnostics, GmbH, Mannheim, Germany), respectively. The laboratory reference range of FT4 and TSH were 0.80-1.71 ng/dL and 0.4-4.48 mIU/L, respectively.
Ethics statement
This study was reviewed and approved by the institutional review board of the Chonnam National University Hwasun Hospital, Hwasun, Korea (IRB No. 2013-004). The exemption of informed consent was allowed by the board because this study was based on a retrospective review and the patient IDs were removed in the data provided by the hospital records office.
RESULTS
Primary sites of metastases to the thyroid gland and screening methods
A total of 13 patients (12 men, 1 woman) was diagnosed with diffuse metastases to the thyroid gland without definite nodules; and their mean age (±SD) was 64.8±8.1 yr. The primary malignancies were lung cancer (n=9), cholangiocarcinoma (n=1), penile cancer (n=1), and cancer of unknown primary site (n=2).
Eleven patients were incidentally found to have thyroid metastases via surveillance or staging 18F-FDG-PET; and two patients underwent ultrasonography for work-up of hypothyroidism (Case 5) and palpable cervical lymph nodes (Case 13) (Tables 1, 2).
Table 1.
Cancer origin and screening methods
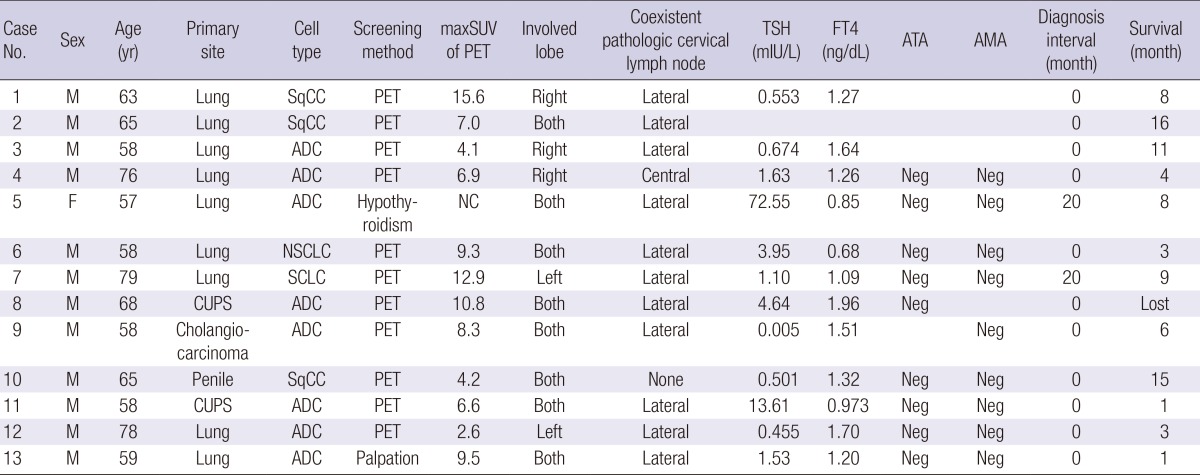
SqCC, squamous cell carcinoma; ADC, adenocarcinoma; NSCLC, non-small cell lung carcinoma; SCLC, small cell lung carcinoma; CUPS, carcinoma of unknown primary site; PET, positron emission tomography; SUV, standardized uptake value; NC, not checked; ATA, anti-thyroglobulin antibody; AMA, anti-microsome antibody; Neg, negative.
Table 2.
Clinical characteristics of 13 cases with diffuse metastatic lesions
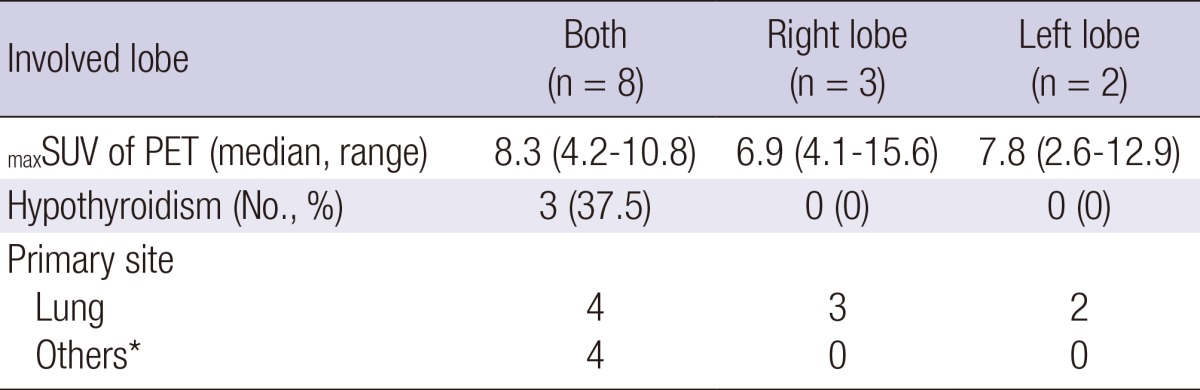
*Others include cholangiocarcinoma, penile squamous cell carcinoma, and two CUPS.
Ultrasonographic findings
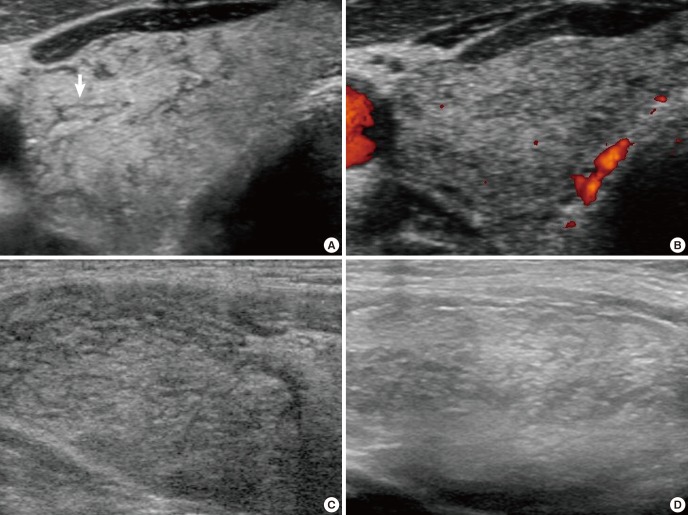
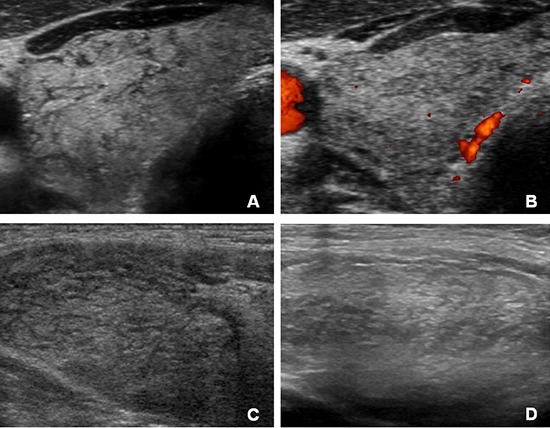
In 8 of 13 patients, diffuse thyroid enlargement involved both lobes. The other 5 patients had involvement of a single lobe (right lobe in 3, left lobe in 2). The echogenicity of the enlarged thyroid gland was heterogeneously hypoechoic or isoechoic. Internal hypoechoic lines were observed without increased vascularity on power Doppler ultrasonography in all cases (Fig. 1). These findings are unique features of diffuse metastases to the thyroid, regardless of the primary malignancy. All patients except 1 (Case 10) had coexistent pathologic cervical lymphadenopathies. Eight cases were confirmed to have metastatic lymph nodes by excisional biopsy or FNAC. Remaining 4 cases did not undergo histological or cytologic confirmation.
Fig. 1.
Ultrasonographic findings of diffuse metastases to the thyroid. (A, B) 65-yr-old man with thyroid metastasis arising from penile squamous cell carcinoma. Transverse sonogram (A) shows diffuse thyroid enlargement with irregular hypoechoic striae (white arrow). Power Doppler study (B) documents no vascularity in the enlarged thyroid and hypoechoic lines. Longitudinal sonograms of 65-yr-old man with metastatic lung squamous cell carcinoma (C) and 68-yr-old man with unknown origin adenocarcinoma (D) show similar imaging features.
Cytology findings
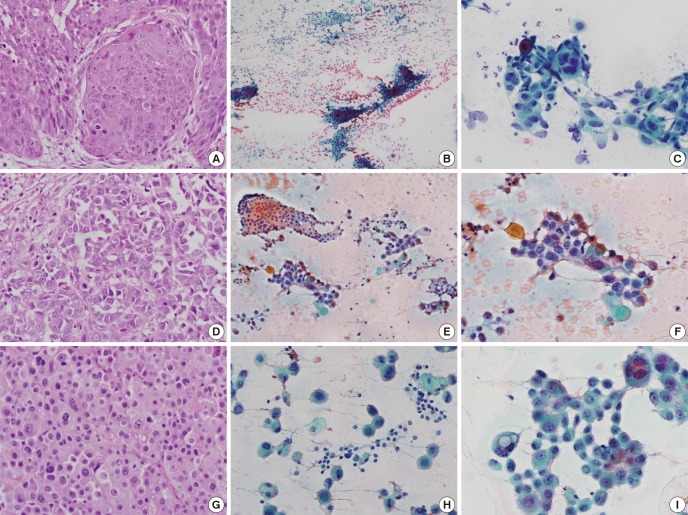
All cases were diagnosed based on the cytology of the thyroid and histological sections of the primary foci (Fig. 2). The most common cytological type was adenocarcinoma (n=8), followed by squamous cell carcinoma (n=3). The majority of aspirates from the thyroid exhibited high cellularity, cohesive clusters, and a clean or minimal inflammatory background. A paucicellular smear was observed in Case 10 and a colloid background was seen in Case 11. Although relatively loose epithelial clusters were observed in Cases 7 and 12, these samples lacked marked pleomorphism and displayed cytomorphology that was typical of small cell carcinoma and adenocarcinoma, respectively. Neither a necrotic background nor cytological evidence of differentiated thyroid carcinoma was noted. Seven cases had heterogeneous populations (Cases 2-4, 6, 7, 11, and 13) that were composed of unremarkable follicular epithelial cells and large hyperchromatic malignant epithelial cells. Because the majority of aspirates exhibited cohesive epithelial clusters with definite glandular or squamous differentiation, other thyroid malignancies such as medullary or anaplastic carcinoma could be excluded. There was no evidence of lymphocytic thyroiditis or Hashimoto's thyroiditis in any case.
Fig. 2.
The histology shows the primary foci and cytological features of matched thyroid lesions (A-C, Case 2; D-F, Case 11; G-I, Case 13). (A) Tumor nests of a well-differentiated squamous cell carcinoma are observed in a specimen of right bronchus. (B, C) Thyroid cytology of Case 2 reveals a slight inflammatory background, and two populations of epithelial cells: follicular epithelial cells and tumor cells. Dyskeratotic cells are also observed in the tumor clusters. (D) A moderately differentiated adenocarcinoma is seen, with frequent mitotic figures. (E, F) The cytology of Case 11 shows a colloid background and heterogeneous population. (G) A poorly differentiated adenocarcinoma is seen. (H, I) Smear of the thyroid aspirate shows large hyperchromatic atypical cells with occasional intracytoplasmic vacuoles. (A, D, G, hematoxylin and eosin, ×400; B, C, E, F, H, I, Papanicolaou stain, ×400).
Clinical characteristics of 13 cases of diffuse thyroid metastases
Thyroid function testing was performed in 12 patients. Two patients were hypothyroid, which was reflected in increased TSH (Case 5 and 11). One patient had early asymptomatic thyrotoxicosis (Case 9), but TSH level had increased to reflect hypothyroidism approximately 2 months later in the absence of any medications (TSH 82.34 mIU/L). These 3 patients with hypothyroidism had metastatic lesions involving both lobes. Their thyroid autoantibodies were negative, and they had no history of irradiation to the head or neck. Patients with unilateral lobe involvement all had normal thyroid function.
In 11 patients, thyroid metastases were found during the initial work-up for the primary tumor. In the other 2 cases, the time interval between diagnosis of primary tumor and metastases to the thyroid was 20 months. None of the patients underwent thyroid surgery for treatment of metastases. All patients had extensive metastases in other organs at the time of thyroid metastases diagnosis. One patient (Case 8) was lost to follow-up after the diagnosis of metastases; and 12 patients with multiple metastases died 1 months to 16 months after the diagnosis of thyroid metastasis (Table 1).
DISCUSSION
To our knowledge, the present report represents the first study to describe the ultrasonographic findings of diffuse metastases to the thyroid. The ultrasonographic finding of diffuse metastasis to the thyroid is a diffusely enlarged and heterogeneously hypoechoic or isoechoic echogenicity of entire thyroid gland without nodular lesions. And diffuse thyroid metastases have unique findings such as internal hypoechoic lines, appearing in a "reticular pattern." In the cases of which thyroid enlargement involved both lobes, 37.5% of the patients showed evidence of hypothyroidism.
Previous reports of ultrasonographic findings of thyroid metastases demonstrated single or multiple hypoechoic nodules with ill-defined margins and intranodular vascularization without evidence of microcalcification (6, 12). Although there have been a few reports of diffuse thyroid metastasis in which patients had abnormal thyroid function (13, 14, 15), the ultrasonographic findings of diffuse metastases were not established in these cases. Miyakawa et al. (15) reported diffuse thyroid metastasis from lung cancer, which showed diffuse thyroid enlargement with inhomogeneous and hypoechoic internal architecture; the sonographic appearance in their case report was similar to our findings in our series of patients. Diffuse thyroid involvement is commonly observed in inflammatory thyroid diseases, such as chronic autoimmune thyroiditis (Hashimoto's thyroiditis) and Graves' disease. In Hashimoto's thyroiditis, the ultrasonography shows a heterogeneously hypoechoic thyroid with lobular margins and multiple hypoechoic micronodules, not hypoechoic lines. In Graves' disease, there is increased vascular blood flow on power Doppler (16). These inflammatory thyroid diseases are characterized by a female predominance; presence of antibodies to thyroglobulin, thyroid peroxidase or TSH receptors; and with infiltration of lymphocytes and plasma cells on cytological examination (17). In our study, diffuse thyroid metastasis showed a smooth margined thyroid without micronodules, and atypical hypoechoic lines were commonly observed without increased blood flow on power Doppler ultrasonography. These signs are unique findings of metastasis to the thyroid gland. There have been controversies about sex predominance for metastasis to the thyroid (1, 7). Men were predominant in our study. Thyroid autoantibody was measured in 10 cases, including cases with hypothyroidism, and all were negative.
In our study, the most prevalent primary cancer was lung cancer (n=9); this result is different from previously reported prevalent cancers including renal cell cancer (RCC) and breast cancer (18). The first reason for this difference is that we confirmed the diagnosis by cytology. FNAC was highly accurate in diagnosing thyroid metastases from lung cancer (90.1%), but did not make the correct diagnosis in 28.7% of patients with RCC (18). Second, most cases were detected by screening or surveillance imaging studies. Clinical symptoms such as newly detected palpable neck mass, increased neck mass, neck edema, dysphagia, hoarseness or cough, were reported in more than half of the patients with thyroid metastases in a recent report by Chung et al. (18). In particular, the clinical diagnosis of thyroid metastases from lung cancer was uncommon because local symptoms were rare. However, autopsy results showed that lung cancer commonly metastasizes to the thyroid (5, 18, 19, 20). Lung cancer is known for its aggressiveness; the interval between diagnosis of primary cancer to thyroid metastasis is the shortest in lung cancer (4). Therefore, aggressive evaluation for abnormal thyroid imaging findings would increase the likelihood of detecting thyroid metastasis from primary lung cancer. Third, compared to aggressive imaging studies for lung cancer including 18F-FDG-PET at diagnosis and follow-up, 18F-FDG-PET or physical examination of the thyroid gland was not routinely performed for known common primary cancers such as RCC. In our study, metastasis from lung cancer was diagnosed earlier, but metastasis from renal cell carcinoma was clinically not acted upon due to advanced disease. Finally, the difference in findings between our study and other studies is caused by epidemiological prevalence of the primary cancers. A report from Italy, where lung cancer is the most prevalent primary cancer, showed that 25% of metastases to the thyroid originated from lung cancer (6). In our study, there were 599 RCC patients during the study period in our hospital but 6,217 lung cancer patients. The prevalence of the primary cancer affected the results for metastasis to the thyroid in this study.
Abnormal thyroid function can be observed in metastatic thyroid cancer (13, 14, 21, 22). Diffuse infiltration of cancer cells induces hypothyroidism (8) and, in rare cases, temporary thyrotoxicosis when destruction of the thyroid gland occurs with leakage of stored thyroid hormone into the peripheral blood (6, 21, 22). In this study, 37.5% (3/8) of patients with diffuse thyroid involvement including both lobes had hypothyroidism without thyroid autoantibody. These results support the known phenomenon that hypothyroidism is caused by massive infiltration of the thyroid gland by tumor cells (8).
The prognosis of thyroid metastases is controversial (5). However, the clinical course of patients is commonly associated with the type of primary cancer and its stage, and not with the presence of thyroid metastases. When the thyroid is the only metastatic site, prognosis is much better than with multiple metastases (6, 23). Surgical resection such as lobectomy or total thyroidectomy can induce complete remission of the primary cancer (1, 23, 24, 25, 26). If the primary cancer is lung cancer, the prognosis is poor, with an average survival of 2 months (16). Saito et al. (27) classified thyroid metastases into two categories based on the US findings: diffuse type represents diffuse hypoechoic lesions occupying the entire thyroid gland and nodular type represents hypoechoic nodular lesion in the thyroid with ill-defined margins. They reported that diffuse thyroid metastases showed poor outcome compared nodular metastases, in which 3-yr-survaval rates were 0% and 35%, respectively. In our study, all patients had extensive metastases in other organs at the time of thyroid metastasis diagnosis, and the survival was as much as 16 months. Therefore, the clinical significance of thyroid metastases was considered with the final course of malignancy. Patients who developed hypothyroidism could have experienced altered tumor growth and aggressiveness; however, the effects on progression and survival are controversial (28, 29). There was no significant difference in the survival of the patients who did and did not develop hypothyroidism (mean survival 5.0±3.6 vs 7.6 ±4.5 months, P=0.414) in our study. A larger study is needed to determine the prognosis with altered thyroid function in patients with metastases to the thyroid.
There are some limitations in this study. Diagnosis was based on cytologic results in all cases; however, cytologic results alone are usually not sufficient to make a definite diagnosis. The reason for our limited diagnosis is that all patients had multiple metastases; therefore, aggressive studies like thyroidectomy or core needle biopsy could not be performed. It can be difficult to discriminate between thyroid metastases and anaplastic thyroid cancer using cytopathology. However, cytopathological observations can identify morphological indicators of anaplastic thyroid cancer such as severe pleomorphism and dyscohesive smear patterns (31). In the present study, cytological data from 11 cases revealed cohesive cluster patterns and typical glandular or squamous differentiation, which allowed for the exclusion of anaplastic thyroid cancer. However, the two remaining cases displayed dyscohesive smear patterns with either typical neuroendocrine cell features (Case 7) or features compatible with adenocarcinoma, including round contoured cells and intracellular vacuoles (Case 12). Another limitation of the study is that we did not histologically confirm the unique finding of reticular pattern hypoechoic lines. We hypothesize that the hypoechoic lines might be intra-thyroidal lymphatics engorged with malignant cells. No Doppler signal on such hypoechoic lines, coexistent cervical lymph nodes metastases, and somewhat different arborizing pattern of the lines may serve as a plausible background of our hypothesis. More studies are needed to correlate the unique features to histologic findings and to investigate whether those features represent lymphatic infiltrations of metastatic cells.
In conclusion, the diffuse thyroid metastases revealed a diffuse goiter with heterogeneously hypoechoic or isoechoic echogenicity and internal hypoechoic lines in a "reticular pattern" on ultrasonography. Although it can be misdiagnosed as autoimmune thyroiditis, diffuse metastasis will be diagnosed more frequently with meticulous ultrasonography and routine use of FNAC in patients with known cancer. Thyroid function testing should be performed in all patients with diffuse thyroid metastases, especially those with involvement of both lobes, because 37.5% of the patients have functional abnormalities.
Footnotes
This study was supported by a grant (CRI 12044-1) from Chonnam National University Hospital Biomedical Research Institute.
The authors declare that there is no conflict of interests regarding the publication of this article.
References
- 1.Nakhjavani MK, Gharib H, Goellner JR, van Heerden JA. Metastasis to the thyroid gland: a report of 43 cases. Cancer. 1997;79:574–578. doi: 10.1002/(sici)1097-0142(19970201)79:3<574::aid-cncr21>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 2.Calzolari F, Sartori PV, Talarico C, Parmeggiani D, Beretta E, Pezzullo L, Bovo G, Sperlongano P, Monacelli M, Lucchini R, et al. Surgical treatment of intrathyroid metastases: preliminary results of a multicentric study. Anticancer Res. 2008;28:2885–2888. [PubMed] [Google Scholar]
- 3.Cichoń S, Anielski R, Konturek A, Barczyński M, Cichoń W. Metastases to the thyroid gland: seventeen cases operated on in a single clinical center. Langenbecks Arch Surg. 2006;391:581–587. doi: 10.1007/s00423-006-0081-1. [DOI] [PubMed] [Google Scholar]
- 4.Wychulis AR, Beahrs OH, Woolner LB. Metastasis of carcinoma to the thyroid gland. Ann Surg. 1964;160:169–177. doi: 10.1097/00000658-196408000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lam KY, Lo CY. Metastatic tumors of the thyroid gland: a study of 79 cases in Chinese patients. Arch Pathol Lab Med. 1998;122:37–41. [PubMed] [Google Scholar]
- 6.Papi G, Fadda G, Corsello SM, Corrado S, Rossi ED, Radighieri E, Miraglia A, Carani C, Pontecorvi A. Metastases to the thyroid gland: prevalence, clinicopathological aspects and prognosis: a 10-year experience. Clin Endocrinol (Oxf) 2007;66:565–571. doi: 10.1111/j.1365-2265.2007.02773.x. [DOI] [PubMed] [Google Scholar]
- 7.Wood K, Vini L, Harmer C. Metastases to the thyroid gland: the Royal Marsden experience. Eur J Surg Oncol. 2004;30:583–588. doi: 10.1016/j.ejso.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 8.Shimaoka K, Sokal JE, Pickren JW. Metastatic neoplasms in the thyroid gland: pathological and clinical findings. Cancer. 1962;15:557–565. doi: 10.1002/1097-0142(196205/06)15:3<557::aid-cncr2820150315>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 9.Czech JM, Lichtor TR, Carney JA, van Heerden JA. Neoplasms metastatic to the thyroid gland. Surg Gynecol Obstet. 1982;155:503–505. [PubMed] [Google Scholar]
- 10.Smith SA, Gharib H, Goellner JR. Fine-needle aspiration. Usefulness for diagnosis and management of metastatic carcinoma to the thyroid. Arch Intern Med. 1987;147:311–312. doi: 10.1001/archinte.147.2.311. [DOI] [PubMed] [Google Scholar]
- 11.Watts NB. Carcinoma metastatic to the thyroid: prevalence and diagnosis by fine-needle aspiration cytology. Am J Med Sci. 1987;293:13–17. doi: 10.1097/00000441-198701000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Chung SY, Kim EK, Kim JH, Oh KK, Kim DJ, Lee YH, An HJ, Kim JS. Sonographic findings of metastatic disease to the thyroid. Yonsei Med J. 2001;42:411–417. doi: 10.3349/ymj.2001.42.4.411. [DOI] [PubMed] [Google Scholar]
- 13.Gkountouvas A, Chatjimarkou F, Sevastiadou M, Ntoula E, Georgiadis P, Kaldrimidis P. Diffuse goiter and severe hypothyroidism due to metastasis to the thyroid. Case Rep Oncol. 2010;3:439–444. doi: 10.1159/000322725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Youn JC, Rhee Y, Park SY, Kim WH, Kim SJ, Chung HC, Hong SW, Lim SK. Severe hypothyroidism induced by thyroid metastasis of colon adenocarcinoma: a case report and review of the literature. Endocr J. 2006;53:339–343. doi: 10.1507/endocrj.k05-115. [DOI] [PubMed] [Google Scholar]
- 15.Miyakawa M, Sato K, Hasegawa M, Nagai A, Sawada T, Tsushima T, Takano K. Severe thyrotoxicosis induced by thyroid metastasis of lung adenocarcinoma: a case report and review of the literature. Thyroid. 2001;11:883–888. doi: 10.1089/105072501316973154. [DOI] [PubMed] [Google Scholar]
- 16.Hayashi N, Tamaki N, Konishi J, Yonekura Y, Senda M, Kasagi K, Yamamoto K, Iida Y, Misaki T, Endo K, et al. Sonography of Hashimoto's thyroiditis. J Clin Ultrasound. 1986;14:123–126. doi: 10.1002/jcu.1870140208. [DOI] [PubMed] [Google Scholar]
- 17.Yeh HC, Futterweit W, Gilbert P. Micronodulation: ultrasonographic sign of Hashimoto thyroiditis. J Ultrasound Med. 1996;15:813–819. doi: 10.7863/jum.1996.15.12.813. [DOI] [PubMed] [Google Scholar]
- 18.Chung AY, Tran TB, Brumund KT, Weisman RA, Bouvet M. Metastases to the thyroid: a review of the literature from the last decade. Thyroid. 2012;22:258–268. doi: 10.1089/thy.2010.0154. [DOI] [PubMed] [Google Scholar]
- 19.Berge T, Lundberg S. Cancer in Malmö 1958-1969. An autopsy study. Acta Pathol Microbiol Scand Suppl. 1977;(260):1–235. [PubMed] [Google Scholar]
- 20.De Ridder M, Sermeus AB, Urbain D, Storme GA. Metastases to the thyroid gland-a report of six cases. Eur J Intern Med. 2003;14:377–379. doi: 10.1016/s0953-6205(03)90005-7. [DOI] [PubMed] [Google Scholar]
- 21.Papi G, Corrado S, Scaltriti L, Carapezzi C, Ezzat S. Metastasis of urothelial sarcomatoid carcinoma to a toxic multinodular goiter. Endocr Pathol. 2005;16:153–156. doi: 10.1385/ep:16:2:153. [DOI] [PubMed] [Google Scholar]
- 22.Eriksson M, Ajmani SK, Mallette LE. Hyperthyroidism from thyroid metastasis of pancreatic adenocarcinoma. JAMA. 1977;238:1276–1278. [PubMed] [Google Scholar]
- 23.Chen H, Nicol TL, Udelsman R. Clinically significant, isolated metastatic disease to the thyroid gland. World J Surg. 1999;23:177–181. doi: 10.1007/pl00013162. [DOI] [PubMed] [Google Scholar]
- 24.Rosen IB, Walfish PG, Bain J, Bedard YC. Secondary malignancy of the thyroid gland and its management. Ann Surg Oncol. 1995;2:252–256. doi: 10.1007/BF02307032. [DOI] [PubMed] [Google Scholar]
- 25.Gault EW, Leung TH, Thomas DP. Clear cell renal carcinoma masquerading as thyroid enlargement. J Pathol. 1974;113:21–25. doi: 10.1002/path.1711130103. [DOI] [PubMed] [Google Scholar]
- 26.Madore P, Lan S. Solitary thyroid metastasis from clear-cell renal carcinoma. Can Med Assoc J. 1975;112:719, 721. [PMC free article] [PubMed] [Google Scholar]
- 27.Saito Y, Sugitani I, Toda K, Yamada K, Fujimoto Y. Metastatic thyroid tumors: ultrasonographic features, prognostic factors and outcomes in 29 cases. Surg Today. 2014;44:55–61. doi: 10.1007/s00595-013-0492-x. [DOI] [PubMed] [Google Scholar]
- 28.Yokoe T, Iino Y, Takei H, Horiguchi J, Koibuchi Y, Maemura M, Ohwada S, Morishita Y. Relationship between thyroid-pituitary function and response to therapy in patients with recurrent breast cancer. Anticancer Res. 1996;16:2069–2072. [PubMed] [Google Scholar]
- 29.Cristofanilli M, Yamamura Y, Kau SW, Bevers T, Strom S, Patangan M, Hsu L, Krishnamurthy S, Theriault RL, Hortobagyi GN. Thyroid hormone and breast carcinoma: primary hypothyroidism is associated with a reduced incidence of primary breast carcinoma. Cancer. 2005;103:1122–1128. doi: 10.1002/cncr.20881. [DOI] [PubMed] [Google Scholar]
- 30.Carcangiu ML, Steeper T, Zampi G, Rosai J. Anaplastic thyroid carcinoma: a study of 70 cases. Am J Clin Pathol. 1985;83:135–158. doi: 10.1093/ajcp/83.2.135. [DOI] [PubMed] [Google Scholar]