Abstract
This study prospectively examined the relationships among cognitive factors and severity of Posttraumatic stress disorder (PTSD) symptoms in female victims of sexual violence. Thirty-eight victims of sexual violence recruited from Center for Women Victims of Sexual and Domestic Violence at Ajou University Hospital. Cognitive factors and PTSD symptom were assessed within 4 months of sexual violence and 25 victims were followed-up 1 month after initial assessment. Repeated-measured ANOVA revealed that PTSD incidence and severity decreased over the month (F [1, 21]=6.61). Particularly, avoidant symptoms might decrease earlier than other PTSD symptoms (F [1, 21]=5.92). This study also showed the significant relationship between early negative trauma-related thoughts and subsequent PTSD severity. Shame and guilt proneness had significant cross-sectional correlations with PTSD severity, but did not show associations when depression severity is controlled. Our results suggest that avoidant symptoms might decrease earlier than other PTSD symptoms during the acute phase and that cognitive appraisals concerning the dangerousness of the world seem to play an important role in the maintenance of PTSD (r=0.499, P<0.05).
Graphical Abstract
Keywords: Sex Offenses, Stress Disorders, Post-traumatic, Cognition, Prospective Studies
INTRODUCTION
Similar to other parts of the world, sexual violence is one of the most serious major crimes in Korea. The Korean Legal Research and Training Institute, a governmental institute, reported 11,105 sexual crimes in 2007. Compared to the report of 6,174 sexual crimes in 1997, the rate of sexual crimes has increased by about 80% during this 10-yr period, which indicates the seriousness of sexual violence (1). Given the pervasiveness of sexual violence in our society, it is imperative to investigate the effects of traumatization by sexual violence on victims' psychological and social functioning. Numerous cross-sectional and retrospective studies have examined factors that may mediate or moderate the relationship between sexual abuse and later psychological maladjustment (2, 3, 4). However, few studies have examined victimization and the resulting adverse psychological effects longitudinally. Posttraumatic Stress Disorder (PTSD) is a common aftermath of sexual assault. A considerable proportion of victims suffer PTSD symptoms, though a significant number of those presenting PTSD symptoms recover in ensuing months without treatment (5). In a national study in the United States, raped women had a 6.2 times higher rate of lifetime PTSD than those who had never been victims of crime (31% vs 5%), and about one-third of raped women meet the diagnostic criteria (6). Therefore, knowledge of the factors involved in the maintenance of PTSD and its initial development is needed to provide effective treatment for victims of sexual crimes.
Many trauma theorists have proposed that maladaptive thoughts and beliefs of victims play an important role in the persistence of PTSD. For example, Foa and Riggs (7) and Foa and Rothbaum (8) proposed that negative thoughts about the world and one's incompetence mediate the development of PTSD after sexual assault. Similarly, some researchers have argued that thoughts about one's perceived weakness and the dangerousness of the world play an important role in the development of PTSD (9, 10). Ehlers and Clark (11) also proposed that negative appraisals of a traumatic event increase the sense of threat, which makes PTSD symptoms and anxiety persist. Preliminary studies conducted by Foa's and Ehlers-Clark's groups have provided support for the importance of cognitive variables related to persistent PTSD (5, 7, 8, 11).
Shame and guilt have common core features. First, they are "moral" emotions associated with a negative evaluation because one has failed to meet standards and norms of others or self (12). Second, they are "self-conscious" emotions that require the concept of self and ability to be evaluated objectively (13). However, many researchers have distinguished between shame and guilt. Some researchers argue that shame is experienced when people attribute their transgressions to their global and stable self, whereas guilt is experienced when people attribute their transgressions to transient actions or states (13). Other scholars have distinguished between shame and guilt in other ways. While shame typically involves being negatively evaluated by others, guilt usually involves being negatively evaluated by oneself (14). Higher levels of guilt and shame are associated with more severe PTSD symptoms in survivors of various traumatic events, including domestic violence, child sexual abuse, and adult sexual assault (15). Feiring et al. (16) established a theoretical model in which sexual abuse leads to shame through the mediation of cognitive attributions and shame has a negative effect on adjustment of sexual abuse victims. A Japanese study also showed the explaining power of shame on PTSD symptoms in university women with negative sexual experiences (17). Furthermore, trauma-related guilt was related to increased PTSD symptomatology both directly and indirectly in a study of women experiencing both physical and psychological abuse from their romantic partners (15).
The purpose of this study was to investigate the relationships among cognitive/emotional factors, including trauma-related thoughts, belief, shame, and guilt proneness and severity of PTSD symptoms.
MATERIALS AND METHODS
Participants
Forty-one participants who had been sexually assaulted within the previous 4 months were included in this study. They were recruited from the Center for Women Victims of Sexual and Domestic Violence at Ajou University Hospital, which provides victims with help and support at the same site in areas of medical care, social service, and criminal investigative service. Three participants who were mentally retarded or had personality problems were excluded based on a clinical interview and assessment. Twenty-nine (76.3%) participants were assessed during the first month after being assaulted, seven (18.4%) were assessed during the second month, one (2.6%) during the third month, and one (2.6%) during the forth month. Among these participants, 25 (65.8%) participated in the second assessment conducted 1 month after the initial assessment. The retention rate was 65.8%, and the dropout analysis showed no significant differences in age, education, marital status, time since trauma, or type of sexual trauma.
The Post-traumatic Cognitions Inventory (PTCI)
The PTCI consists of 36 items and uses a seven-point Likert scale to assess negative trauma-related thoughts and beliefs. The PTCI produces a total score and three subscores based on the means of items for each subscale: Negative Cognitions about Self (21 items), Negative Cognitions about the World (7 items), and Self-Blame (5 items). The PTCI subscales have good test-retest reliability (0.75-0.89), good internal consistency (Cronbach's α, 0.86-0.97), and moderate-to-high correlations with PTSD symptom severity (18). The PTCI items were translated into Korean by the first author, then reviewed by a fluent bilingual psychiatrist. The Cronbach's α of PTCI in the present study was 0.95.
Clinician Administered PTSD Scale (CAPS)
The CAPS is a 30-item semi-structured clinical interview that assesses severity of each of the 17 PTSD symptoms defined by the DSM-IV (19). Clinicians rate both the frequency and intensity of each symptom on a five-point Likert-type scale. The CAPS has well established psychometric properties and is widely regarded as the gold standard measure for assessing PTSD. The Korean version of CAPS has a high internal consistency value of 0.95 (20).
PTSD Symptoms Scale: Self-reported Version (PSS-SR)
This 17 item scale corresponds to the PTSD symptoms listed in the DSM-IV. The PSS-SR has been demonstrated to have acceptable to good levels of reliability and validity and provides a measure of symptom severity (21). The PTSD symptoms scale used in this study was composed of items derived from the PTSD diagnostic criteria in the Korean version of the Structured Clinical Interview for the DSM-IV (22).
Harder's Personal Feelings Questionnaire-2 (PFQ-2)
The PFQ-2 consists of 16 items and use a five-point Likert scale to measure proneness to shame and guilt. Subjects are asked how frequently they experience a feeling, followed by 10 shame-items and six guilt-items. The PFQ-2 has good test-retest reliability of 0.91 (shame-proneness) and 0.85 (guilt-proneness), and satisfactory internal consistency of 0.78 (shame-proneness) and 0.72 (guilt-proneness) (23). The PFQ-2 items were translated into Korean by the first author, then reviewed by a bilingual psychiatrist. The Cronbach's α of the PFQ-2 in this present study was 0.94.
Beck Depression Inventory (BDI)
The BDI is a well-performing, 21-item self-report scale designed to assess and evaluate the severity of depressive symptoms. We administered a Korean version of the BDI, which has demonstrated good psychometric properties. The internal consistency of the BDI is 0.92 (24).
Mini International Neuropsychiatric Interview-Plus Version 5.0.0 (MINI-Plus 5.0.0)
MINI-Plus is a comprehensive diagnostic semi-structured interview that was developed as a short diagnostic instrument for generating DSM-IV criteria diagnoses. The Korean version of the MINI was validated and demonstrates good psychometric properties. The range of Kappa values is 0.62-0.81 for anxiety disorders and that for major depressive disorder is 0.71 (26).
Procedure
Participants were initially asked to complete the PTCI, PSS-SR, PFQ-2, and K-BDI, and a study questionnaire including information on demographic data and types of sexual assault experiences. Clinicians examined detailed psychiatric histories and clinical diagnoses by means of the MINI-Plus Korean version 5.0.0. A second assessment was performed 1 month after the initial assessment. PTSD symptom severity was assessed using the CAPS and participants completed the PSS-SR, and K-BDI. Participants were defined as the PTSD group and non-PTSD group according to the diagnosis using the CAPS at the second assessment. All participants had received medications at the time of the initial assessment.
Statistical analysis
The 38 participants were assigned to the PTSD and non-PTSD groups according to the CAPS results 1 month after the initial assessment. Categorical variables were compared with the non-parametric Fisher's exact test, and continuous variables were compared with the non-parametric Mann-Whitney U analysis. Repeated-measures analyses of variance (ANOVAs) was used to determine changes across time points. Correlations between cognitive factors and PTSD severity at each time point were calculated using Pearson's statistic. Additionally partial correlations adjusted for depression severity were calculated. A P<0.05 was considered significant.
Ethics statement
The study protocol was approved by the institutional review board of Ajou University Medical Center (IRB No. 10-262). Written informed consent was obtained from all participants.
RESULTS
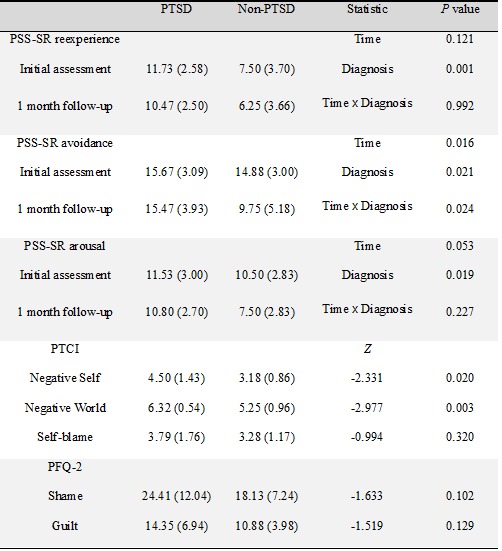
The background characteristics of the subjects are shown in Table 1. The mean age of the subjects was 29.05±11.35 yr, and the average educational level was 13.13±1.80 yr. Twenty-six (68.4%) participants experienced rape. Twenty-five of the 38 initial participants were followed up at the second assessment. Of them, 17 (68%) had PTSD and eight (32%) did not. It was revealed that PTCI-negative self (Z=-2.331, P=0.020), and PTCI-negative world (Z=-2.977, P=0.003) were significantly different between the PTSD and non-PTSD groups.
Table 1.
Background characteristics of the Post-Traumatic Stress Disorder (PTSD) and non-PTSD groups
SD, standard deviation; PTCI, post-traumatic cognitions inventory; PFQ-2, Harder's personal feelings questionnaire-2.
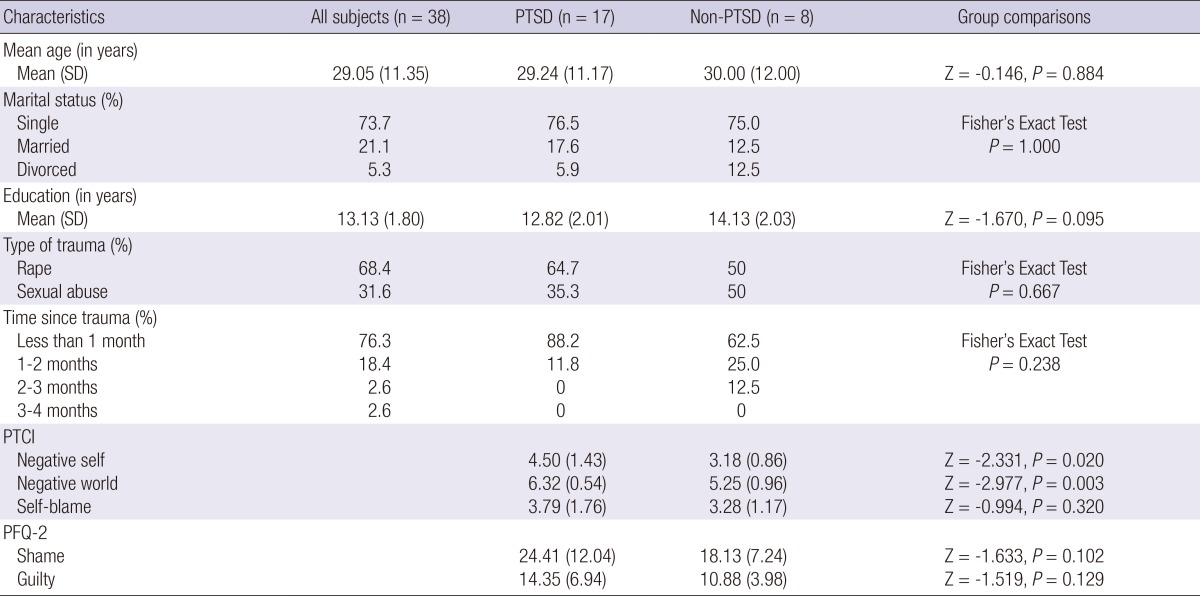
The mean PSS-SR and BDI scores at each time point are presented in Table 2. Repeated-measures ANOVAs were conducted with time (initial vs second assessment) as the within-group factor and diagnostic group (PTSD vs non-PTSD) as the between-group factor. A main effect for time was observed with the PSS-SR total (F [1, 21]=6.61, P=0.018), and avoidance scores (F [1, 21] =6.92, P=0.016) declined significantly. A significant main effect was observed for diagnosis with PSS-SR total (F [1, 21]= 16.11, P=0.001), re-experience (F [1, 21]=16.51, P=0.001), avoidance (F [1, 21]=6.19, P=0.021), and arousal cores (F [1, 21]=6.48, P=0.019), but only avoidance scores had a significant interaction between time and diagnosis (F [1, 21]=5.92, P=0.024). A significant main effect was observed for diagnosis in the BDI, and the PTSD group scored higher than that of the non-PTSD group (F [1, 22]=15.10, P=0.001), but no significant main effect was observed for time or the interaction between time and diagnosis.
Table 2.
Severity of Post-Traumatic Stress Disorder (PTSD) and depression at each time point
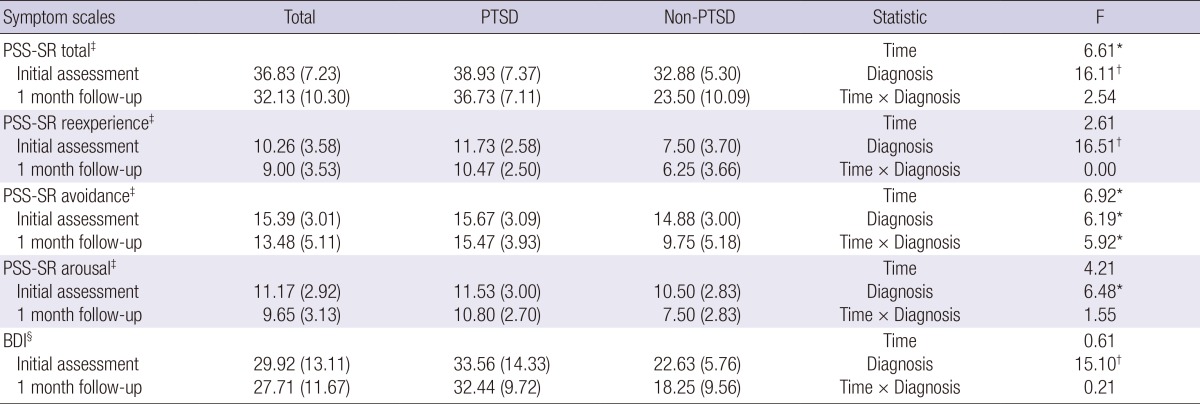
*P<0.05; †P<0.01; ‡n=23, PTSD=15, non-PTSD=8; §n=24, PTSD=16, non-PTSD=8. PSS-SR, PTSD symptoms scale: self-reported version; BDI, Beck depression inventory.
Correlations between cognitive factors and PTSD and depression severity at each time point are presented in Table 3. At the initial assessment, the majority of cognitive variables were significantly associated with PTSD severity. At the second assessment, the "Negative World" subscale of the PTCI was significantly associated with CAPS (r= 0.621, P<0.01), and with PSS-SR avoidance scale (r= 0.513, P<0.05). The "Negative Self" subscale of the PTCI was significantly correlated only with CAPS score (r= 0.403, P<0.05). Partial correlation coefficients adjusted for depression severity are also presented in Table 3. At the initial assessment, "Negative Self" subscale of the PTCI was significantly associated with PSS-SR avoidance scale (r= 0.408, P<0.05), and "Negative World" was significantly associated with total score (r= 0.416, P<0.05) and arousal scale of PSS-SR (r= 0.341, P<0.05). At the second assessment, only "Negative World" subscale of the PTCI was significantly correlated with CAPS score (r= 0.499, P<0.05).
Table 3.
Correlations between cognitive variables and severity of Post-Traumatic Stress Disorder (PTSD), and partial correlations with depression severity controlled at the initial assessment and at the 1 month follow-up
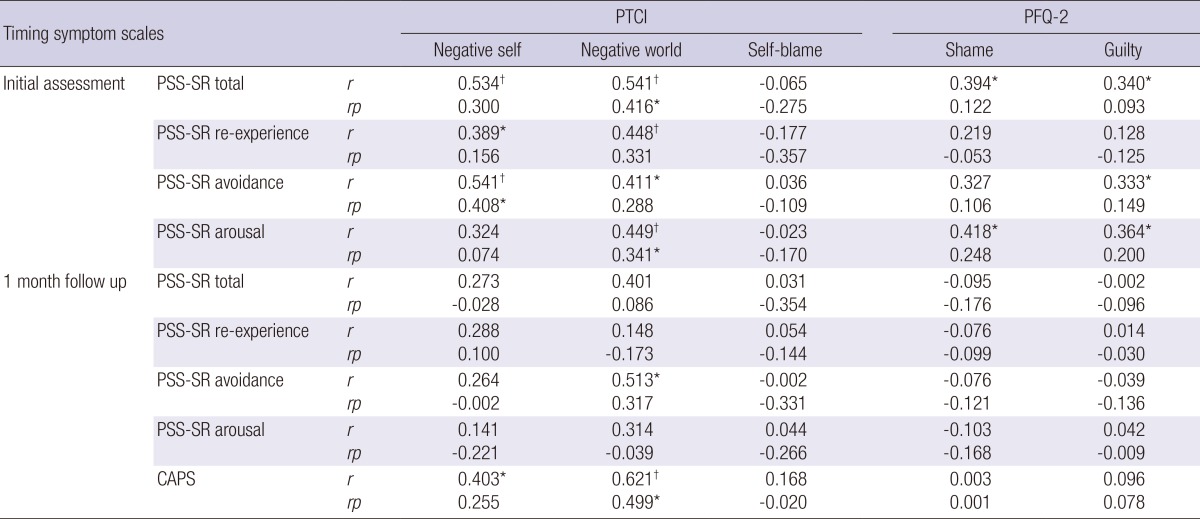
*P<0.05; †P<0.01. r, correlation coefficient; rp, partial correlation coefficient; PTCI, post-traumatic cognitions inventory; PFQ-2, Harder's personal feelings questionnaire-2; PSS-SR, PTSD symptoms scale: self-reported version; CAPS, clinician administered PTSD scale.
DISCUSSION
We prospectively investigated the relationship between post-traumatic cognitive factors and PTSD and depressive symptoms among female victims of sexual violence. At the initial assessment, 30 (78.9%) of the victims met diagnostic criteria for PTSD and Acute Stress Disorder. By the second assessment, the incidence of PTSD dropped to 68%. This was comparable to the results of a prospective study on rape victims reporting that the PTSD incidence rate decreased from 94% to 65% in about 1 month (27). Our study also showed that PTSD incidence and severity decreased over the month. However, further analyses revealed that only avoidance symptoms declined significantly over that month and showed a significant interaction between time and diagnostic group. This result suggested that the non-PTSD group had more prominently recovered avoidance symptoms than those in the PTSD group. This was consistent with a previous study suggesting that avoidance symptoms might be associated with the course of PTSD (28). In contrast, our results suggest that symptoms of re-experience, hyperarousal, and depression did not change significantly after 1 month. In the repeated-measures ANOVA, a significant main effect was observed for diagnosis with all PTSD and depressive symptoms, suggesting that victims of persistent PTSD had a greater severity of overall PTSD and depressive symptoms at the initial assessment than those who recovered. This result agreed with that of a previous study on acute stress reactions or Acute Stress Disorder that emphasized the associations between the immediate response after a traumatic event and the longitudinal course of PTSD (29).
The Self and World subscales of the PTCI showed associations with self-report measures of PTSD and depressive symptoms at the initial assessment but were not correlated with the Blame subscale or PTSD severity. Some studies have noted similar findings about the PTCI Blame subscale (30, 31). Startup et al. (31) suggested that the Blame subscale is indefinite for discriminating character vs behavioral self-blame, because it may hold protective and harmful effects on self. They proposed that the Blame subscale be revised to specifically assess behavioral self-blame.
The Self and World subscales of the PTCI, which were evaluated at the initial assessment, were significantly correlated with PTSD severity measured by the CAPS at the second assessment. Furthermore, the World subscale correlated significantly with CAPS score adjusted for depression severity at the second assessment. This result is consistent with that of previous studies suggesting that dysfunctional cognition regarding a traumatic event seem to strongly affect the maintenance and severity of PTSD symptoms (5, 32). In the present study, cognitive appraisals concerning the dangerousness of the world seemed to play an important role in the maintenance of PTSD symptoms.
Shame and guilt proneness had significant cross-sectional correlations with PTSD severity, but did not show associations when controlled depression severity. Several researchers have cited shame and guilt feelings as the major emotional aspects of negative self-evaluations associated with the most psychopathological conditions. Additionally, shame and guilt proneness have been theorized to play an essential role in symptom formation and the maintenance of psychiatric symptoms, particularly affective disorders (33, 34). In our study, shame and guilt proneness seemed to be related to formation of depression rather than PTSD symptoms.
Our findings should be interpreted with some caveats. First, the current sample is not representative of general rape victims because of the small sample size. It has been well established that only a small proportion of sexual crimes are reported to law-enforcing agencies such as police (35). Moreover, the participants in the present study were victims of sexual violence who sought psychiatric help and evaluation. In reality, a larger proportion of victims do not want psychiatric services. Thus, a selection bias may have been present. However, the present findings are consistent with the results from previous longitudinal studies that examined the impact of cognitive factors on the maintenance of PTSD. Second, it must be noted that this study did not attempt to comprehensively examine the cognitive factors implicated in previous studies including appraisal of reactions during assault and control strategies.
Despite these limitations, strength of this study is that we longitudinally investigated the relationship between PTSD symptoms and trauma-associated cognitive factors in female victims of sexual violence. In conclusion, our results suggest that avoidance symptoms might decrease earlier than other PTSD symptoms during the acute phase and that cognitive appraisals concerning the dangerousness of the world seem to play an important role in the maintenance of PTSD. Further studies with a larger sample size, various trauma-related cognitive factors, and longer follow-up periods are needed.
Footnotes
This study is partially supported by the fund generously donated by Sanofi-Aventis Inc. in Korea (M-2010-C0980-12060).
The authors have no conflicts of interest to disclose.
References
- 1.Kim HK, Kang EY. Sentencing of sexual violence crime and management of sexual offenders. [accessed on 19 August 2013]. Available at http://www.prism.go.kr/homepage/researchCommon/retrieveResearchDetailPopup.do?research_id=1270000-200600011.
- 2.Classen C, Field NP, Koopman C, Nevill-Manning K, Spiegel D. Interpersonal problems and their relationship to sexual revictimization among women sexually abused in childhood. J Interpers Violence. 2001;16:495–509. [Google Scholar]
- 3.Deblinger E, Steer R, Lippmann J. Maternal factors associated with sexually abused children's psychosocial adjustment. Child Maltreat. 1999;4:13–20. [Google Scholar]
- 4.Noll JG, Horowitz LA, Bonanno GA, Trickett PK, Putnam FW. Revictimization and self-harm in females who experienced childhood sexual abuse: results from a prospective study. J Interpers Violence. 2003;18:1452–1471. doi: 10.1177/0886260503258035. [DOI] [PubMed] [Google Scholar]
- 5.Dunmore E, Clark DM, Ehlers A. A prospective investigation of the role of cognitive factors in persistent posttraumatic stress disorder (PTSD) after physical or sexual assault. Behav Res Ther. 2001;39:1063–1084. doi: 10.1016/s0005-7967(00)00088-7. [DOI] [PubMed] [Google Scholar]
- 6.Kilpatrick DG, Edmunds CN, Seymour AK. Rape in America: a report to the nation. Arlington: National Victim Center and Medical University of South Carolina; 1992. [Google Scholar]
- 7.Foa EB, Riggs DS. Post-traumatic stress disorder in rape victims. In: Oldham J, Riba MB, Tasman A, editors. American Psythiatric Press review of psychiatry. Vol. 12. Washington, D.C.: American Psychiatry Press; 1993. pp. 272–303. [Google Scholar]
- 8.Foa EB, Rothbaum BO. Treating the trauma of rape: cognitive-behavioral therapy for PTSD. New York: Guilford Press; 1998. [Google Scholar]
- 9.McCann IL, Pearlman LA. Psychological trauma and the adult survivor: theory, therapy, and transformation. New York: Brunner/Mazel; 1990. [Google Scholar]
- 10.Resick PA, Schnicke MK. Cognitive processing therapy for rape victims: a treatment manual. Newbury Park: Sage Publications; 1993. [Google Scholar]
- 11.Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther. 2000;38:319–345. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- 12.Tangney JP, Stuewig J. A moral-emotional perspective on evil persons and evil deeds. In: Miller AG, editor. The social psychology of good and evil. New York: Guilford Press; 2004. pp. 327–355. [Google Scholar]
- 13.Tracy JL, Robins RW. Putting the self into self-conscious emotions: a theoretical model. Psychol Inq. 2004;15:103–125. [Google Scholar]
- 14.Smith RH, Webster JM, Parrott WG, Eyre HL. The role of public exposure in moral and nonmoral shame and guilt. J Pers Soc Psychol. 2002;83:138–159. [PubMed] [Google Scholar]
- 15.Street AE, Gibson LE, Holohan DR. Impact of childhood traumatic events, trauma-related guilt, and avoidant coping strategies on PTSD symptoms in female survivors of domestic violence. J Trauma Stress. 2005;18:245–252. doi: 10.1002/jts.20026. [DOI] [PubMed] [Google Scholar]
- 16.Feiring C, Taska L, Lewis M. A process model for understanding adaptation to sexual abuse: the role of shame in defining stigmatization. Child Abuse Negl. 1996;20:767–782. doi: 10.1016/0145-2134(96)00064-6. [DOI] [PubMed] [Google Scholar]
- 17.Uji M, Shikai N, Shono M, Kitamura T. Contribution of shame and attribution style in developing PTSD among Japanese University women with negative sexual experiences. Arch Womens Ment Health. 2007;10:111–120. doi: 10.1007/s00737-007-0177-9. [DOI] [PubMed] [Google Scholar]
- 18.Foa EB, Ehlers A, Clark DM, Tolin DF, Orsillo SM. The Posttraumatic Cognitions Inventory (PTCI): development and validation. Psychol Assess. 1999;11:303–314. [Google Scholar]
- 19.Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a Clinician-Administered PTSD Scale. J Trauma Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- 20.Lee BY, Kim Y, Yi SM, Eun HJ, Kim DI, Kim JY. A reliability and validity study of a clinician-administered PTSD scale. J Korean Neuropsychiatr Assoc. 1999;38:514–522. [Google Scholar]
- 21.Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress. 1993;6:459–473. [Google Scholar]
- 22.Han OS. In: Korean version of the Structured Clinical Interview for DSM-IV. Hong JP, editor. Seoul: Hana Medical Publishing Co.; 2000. [Google Scholar]
- 23.Harder DH, Zalma A. Two promising shame and guilt scales: a construct validity comparison. J Pers Assess. 1990;55:729–745. doi: 10.1080/00223891.1990.9674108. [DOI] [PubMed] [Google Scholar]
- 24.Lee YS, Song JY. Study of reliability and validity of the BDI, the SDS, and the MMPI Depression scale. Korean J Clin Psychol. 1991;10:98–113. [Google Scholar]
- 25.Kwon SM. Differential roles of dysfunctional attitudes and automatic thoughts in depression: an integrated model of depression. Queensland: University of Queensland; 1992. [Google Scholar]
- 26.Yoo SW, Kim YS, Noh JS, Oh KS, Kim CH, Namkoong K, Chae JH, Lee GC, Jeon SI, Min KJ, et al. Validity of Korean version of the Mini-International Neuropsychiatric Interview. Anxiety Mood. 2006;2:50–55. [Google Scholar]
- 27.Rothbaum BO, Foa EB, Riggs DS, Murdock T, Walsh W. A prospective examination of post-traumatic stress disorder in rape victims. J Trauma Stress. 1992;5:455–475. [Google Scholar]
- 28.Perkonigg A, Pfister H, Stein MB, Höfler M, Lieb R, Maercker A, Wittchen HU. Longitudinal course of posttraumatic stress disorder and posttraumatic stress disorder symptoms in a community sample of adolescents and young adults. Am J Psychiatry. 2005;162:1320–1327. doi: 10.1176/appi.ajp.162.7.1320. [DOI] [PubMed] [Google Scholar]
- 29.Harvey AG, Bryant RA. Two-year prospective evaluation of the relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry. 2000;157:626–628. doi: 10.1176/appi.ajp.157.4.626. [DOI] [PubMed] [Google Scholar]
- 30.Beck JG, Coffey SF, Palyo SA, Gudmundsdottir B, Miller LM, Colder CR. Psychometric Properties of the Posttraumatic Cognitions Inventory (PTCI): a replication with motor vehicle accident survivors. Psychol Assess. 2004;16:289–298. doi: 10.1037/1040-3590.16.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Startup M, Makgekgenene L, Webster R. The role of self-blame for trauma as assessed by the Posttraumatic Cognitions Inventory (PTCI): a self-protective cognition? Behav Res Ther. 2007;45:395–403. doi: 10.1016/j.brat.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 32.Bennett SA, Beck JG, Clapp JD. Understanding the relationship between posttraumatic stress disorder and trauma cognitions: the impact of thought control strategies. Behav Res Ther. 2009;47:1018–1023. doi: 10.1016/j.brat.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 33.Harder DW, Rockart L, Cutler L. Additional validity evidence for the Harder Personal Feelings Questionnaire-2 (PFQ2): a measure of shame and guilt proneness. J Clin Psychol. 1993;49:345–348. doi: 10.1002/1097-4679(199305)49:3<345::aid-jclp2270490307>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 34.Tangney JP, Wagner P, Fletcher C, Gramzow R. Shamed into anger? the relation of shame and guilt to anger and self-reported aggression. J Pers Soc Psychol. 1992;62:669–675. doi: 10.1037//0022-3514.62.4.669. [DOI] [PubMed] [Google Scholar]
- 35.Koss MP, Gidycz CA, Wisniewski N. The scope of rape: incidence and prevalence of sexual aggression and victimization in a national sample of higher education students. J Consult Clin Psychol. 1987;55:162–170. doi: 10.1037//0022-006x.55.2.162. [DOI] [PubMed] [Google Scholar]


