Abstract
Background:
Prevalence of diabetes is on an increase in India, currently there is limited nation-wide data regarding the prevalence of chronic complications in diabetic patients at diagnosis. This information will help health-care professionals approach management more aggressively to prevent complications.
Objective:
To determine the prevalence of chronic complications in newly-diagnosed Type 2 diabetic (T2D) patients in India.
Design and Methods:
This was a cross-sectional survey of T2D patients, diagnosed within 3 months of their first visit to the centers doing the survey. Each patient was screened for diabetic complications, hypertension, dyslipidemia, and body mass index. Family history was recorded. Standard protocols were used to make the diagnosis of retinopathy, neuropathy and nephropathy. Data analysis was carried out using the standard statistical techniques.
Results:
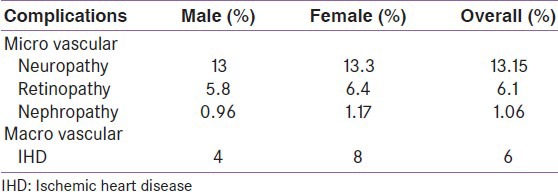
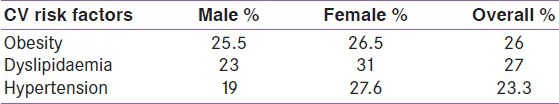
Of the total 4,600 (males 67%, females 33%) newly diagnosed patients with T2D, majority were from the age group 41-50 years (40%). 13.15% of newly detected India T2D had neuropathy 6.1% had retinopathy and 1.06% had nephropathy. Risk factors of macro vascular complication such as hypertension, obesity, and dyslipidemia were observed in 23.3%, 26%, and 27% of patients respectively. Ischemic heart disease was noticed in 6%.
Conclusion:
High prevalence of micro vascular complications was present at diagnosis along with association of CV cardiovascular risk factors among Indian T2D. In view of this, screening must be instituted for all diabetics for complications at the time of diagnosis itself.
Keywords: Complications, dyslipidemia, hypertension, neuropathy, prevalence, retinopathy, type 2 diabetes mellitus
INTRODUCTION
Type 2 diabetes mellitus (T2DM) is the most common form of diabetes constituting 90% of the diabetic population. The number of patients with diabetes in India is currently around 40.9 million and is expected to rise to 101 million by 2030.[1]
The so-called “Asian Indian Phenotype” refers to certain unique clinical and biochemical abnormalities in Indians which include increased insulin resistance, higher waist circumference despite lower body mass index (BMI), lower adiponectin and higher levels of highly sensitive
C-reactive protein levels. This phenotype makes Asians more prone to diabetes and premature coronary artery disease.[2]
The course leading to complications related to diabetes starts with lingering dysglycemia. Chronic complications of diabetes, the major cause of morbidity and mortality, are often present at the time of diagnosis. The problem is further worsened as the diagnosis of diabetes is often delayed from months to years due to lack of symptoms, lack of awareness and the fear of unknown in spite of awareness.
A very high prevalence of complications at diagnosis has been reported from various studies across the globe and from parts of India. However, a nationwide Indian data for the same is not available. A high prevalence of such complications, if documented, will help to convince the physicians of the importance of screening for these complications in all Type 2 diabetics (T2D) at presentation, for appropriate implementation of treatment without delay.
The present study was designed to determine the prevalence of complications in newly-diagnosed T2D patients across various regions of India.
DESIGN AND METHODS
The present study was a cross-sectional survey done across 14 centers representing north, west, south and east region of India. In this study, adult patients aged 18 years and above, newly-diagnosed with T2DM for less than 3 months based on the American Diabetes Association criteria were included.[3] Patients who have been diagnosed with diabetes for more than 3 months, patients on any drug therapy, gestational diabetics, and steroid-induced diabetics or those with co-morbid conditions that require prolonged steroid therapy were excluded. Cut-off of < 3 months duration was selected mainly because of the fact that some earlier studies had used the same criteria. The diagnostic criteria comprising standard methods were agreed upon by all investigators from 14 Indian centers; they were senior endocrinologists and physicians who had particular research interest in diabetes.
Physicians from all the 14 centers were contacted and informed about the protocol and criteria for making the diagnosis of diabetes and various complications. After discussing each of the criteria, a decision was taken to use what is normally followed in clinical practice, and the performa was approved. A standard performa for recording the complications was made and circulated to all the centers. Following criteria was followed to make the diagnosis of neuropathy, retinopathy, nephropathy, hypertension, dyslipidemia, ischemic heart disease (IHD) and obesity.
Retinopathy
Direct/indirect fundscopy was used to make the diagnosis and grading of retinopathy. Physician if trained or a Retinologist did the fundus examination after full dilatation of the pupil. All doubtful cases were referred for a second opinion before the performa was filled. Routine stereoscopic fundus photography was not done as it was not available across the country in all the centers.[4]
Nephropathy
Nephropathy was diagnosed based on 24 h urine collection for proteinuria (mg/24 h). A value of >300 mg/dl was taken as confirmed nephropathy. Twenty four hours collection was carried out by the treating physician taking care of the factors that interfere with proteinuria (like, uncontrolled hypertension, urinary infection etc.).[5]
Neuropathy
Diagnosis of neuropathy was made on clinical grounds for senses of touch, pain, vibration and jerks ruling out all other non-diabetic causes for neuropathy. 128 Hz tuning fork for vibration perception and 10-g monofilament pressure sensation at the distal plantar aspect of both great toes and metatarsal joints were carried out along with assessment of ankle reflexes. Michigan neuropathy screening score was used in all cases. Combination of more than one test has > 87% sensitivity in detecting diabetic poly neuropathy.[5,6]
Hypertension
Hypertension was defined as a value > 130/90 mm/Hg. BP was recorded twice, 10 min apart-both arms, standing and lying down. Known hypertensive patients were recorded separately. All baseline high values were retested over a period of 15 days for confirmation of hypertension (>130/90 mm/hg) to avoid the “White Coat Phenomenon.”[4]
Dyslipidemia
For diagnosing dyslipidemia, whole lipid profile of the patient was tested in the fasting blood sample. Value over and above the goal of therapy (low density lipoprotein (LDL) > 100 mg/dl and total cholesterol > 200 mg/dl) was considered abnormal.[4]
IHD
IHD diagnosis was made on the basis of treadmill test or coronary angiogram (if resting ECG showed changes) or chest pain relieved by nitrates in cases where patient complained of anginal pain.[4]
Obesity
For anthropometry, BMI cut-off of 25 kg/m2 for men and 23 kg/m2 for women was used for making a diagnosis of obesity as recommended by various studies as Indians are having Asian-Indian Phenotype.[7]
Data analysis
Data was collected from June 2006 till October 2011. Incomplete performas were excluded.
A total of 4600 completed performa's were included for analysis.
Quantitative variables were described as mean + 1SD unless otherwise indicated. Qualitative variables were described by percentages.
RESULTS
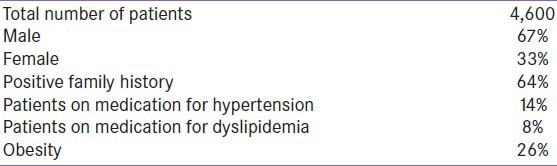
Our study is a specialized clinic-based survey rather than population based or epidemiological survey and reflects the prevalence of diabetic complications in the out-patient setting in the current health system of India. Doctors who contributed to this survey are Endocrinologist or Senior Diabetologists. The study recruited 4,600 patients with equal contribution from all the centers from June 2006 to October 2011. Of the total 4,600 newly diagnosed patients with T2D, majority were male (67%, N: 3,082) in comparison to female (33%, N: 1,518). The demographics are shown in Table 1.
Table 1.
Baseline characteristics in CINDI
The importance of age on the prevalence of newly diagnosed diabetes shows that the majority of the patients were from the age group 41-50 years (40%) as illustrated in Figure 1, which shows sex-specific estimates of diabetes prevalence by age.
Figure 1.
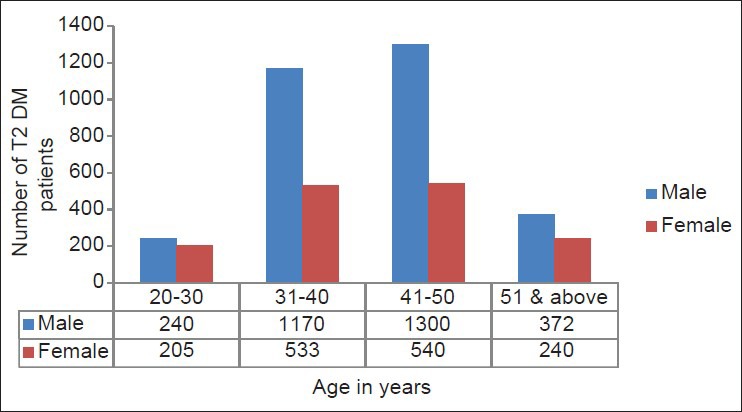
Age distribution in CINDI
The prevalence of diabetes specific micro vascular and IHD are shown in Table 2. In patients having diabetic retinopathy, majority (65.9%) were having non-proliferative diabetic retinopathy.
Table 2.
Prevalence of complications: CINDI
The prevalence of risk factors for macro vascular disease is shown below in Table 3.
Table 3.
Prevalence of CV risk factors: CINDI
DISCUSSION
T2D is an insidious illness with a long preclinical asymptomatic phase during which patients may be exposed to the ill-effects of asymptomatic hyperglycemia for many years before they are diagnosed. The present study reconfirms this and shows that a substantial proportion of patients with T2DM have evidence of diabetic tissue damage at the time of diagnosis of diabetes.
In our study Chronic complications in newly diagnosed patients with Type 2 Diabetes Mellitus in India
CINDI, many patients were from a younger age 31-40 years (35%) and almost equal (40%) population was from the age group 41-50 years, which confirms similar finding of other studies showing that in developing countries],[ the majority of patients with diabetes are in the age range of 45-64 years, whereas age group is higher (>65 years) in the developed countries.[1,8]
Younger age of onset implies that these subjects develop diabetes in the most productive years of their life and have a greater chance of developing complications. Both environmental and genetic factors might explain the younger onset of age along with high prevalence of diabetes in the Indian population.[2]
The Indian patients also had a more sedentary life-style and a higher prevalence of family history of known diabetes than the other groups. Ramachandran et al., observed similar findings in their study of parental influence on the spectrum of T2D in the offspring among Indians. Familial clustering of T2D is well-known and is high in Indians, which was also observed in our study with more than half of the patients (64%) having positive diabetes family history for first degree relatives.[9,10]
While the relatively low rate of diabetic retinopathy (6%) in CINDI is similar to some of the studies from South India (7.3%) and abroad that include Denmark (5%), where they suggested that the low prevalence is due to the Danish health system, which is free of charge and results in early diagnosis of diabetic patients. the results for diabetic retinopathy are in contrast to findings of other studies showing higher prevalence in Romania (14.37%) and Taiwan (25.5%).[11,12,13,14] the prevalence of diabetic retinopathy in newly diagnosed patients among various studies, Chennai Urban Rural Epidemiology Study (CURES) (5.1%) and United Kingdom Prospective Diabetes Study (UKPDS) (35%) is shown below in Figure 2.[15,16]
Figure 2.
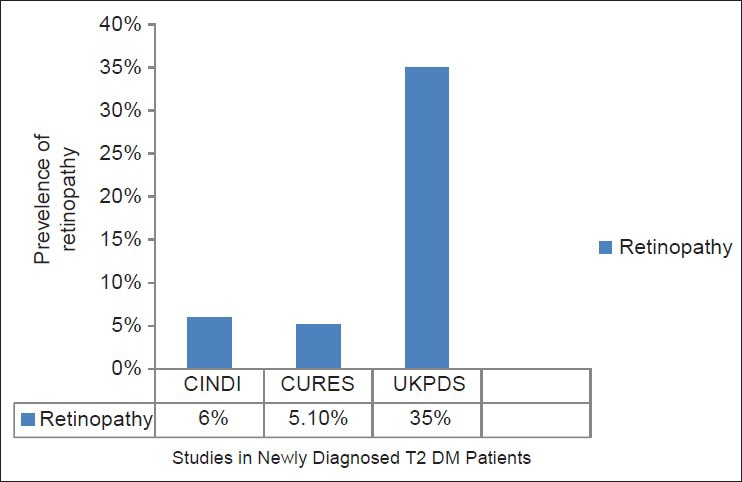
Prevalence of retinopathy in newly diagnosed Type 2 diabetes mellitus patients
Although, it is difficult to identify the reasons for such variation in prevalence rates among various populations, race, age, method of detecting diabetic retinopathy, health-care facilities, and other risk factors could have contributed to the differences. as mentioned in one of the study from India, inherent ethnic difference in the Indians in relation to the susceptibility to diabetic retinopathy may be one aspect and another reason may be the type of diet which although rich in carbohydrates includes more vegetables, less fat and perhaps more antioxidants and anti-inflammatory agents like curcumin.[17]
Overall prevalence of nephropathy in CINDI is only 1.02%, which is comparable to other studies from India CURES, which showed overt nephropathy in 0.8% but low in comparison to UKPDS which showed 7% as shown below in Figure 3.[18,19] Unlike CURES, CINDI did not include diabetic retinopathy in defining nephropathy. However, all patients with nephropathy had retinopathy including proliferative retinopathy. It is possible that micro-albuminuria may have been transient considering glycemic control may have modulated the albumin excretion. This question would be addressed in future longitudinal studies
Figure 3.
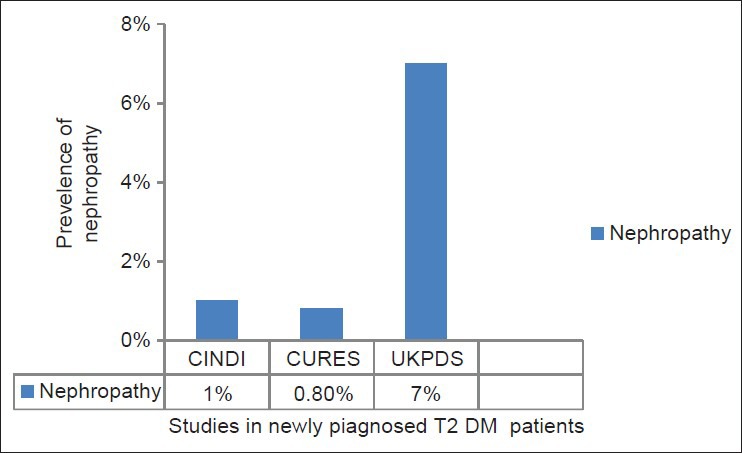
Prevalence of nephropathy in newly diagnosed Type 2 diabetes mellitus patients
In CINDI prevalence of peripheral neuropathy is 13.15%, which is again comparatively low in comparison to other studies from Sri Lanka (25.2%) and Amsterdam (48.3%).[20,21]
Literature search for articles on the prevalence of neuropathy in newly diagnosed T2DM in India (<3 months duration) for comparison are very few. Karmakar et al. have shown 9% prevalence at diagnosis and Rani et al. have also reported 13% in established cases of retinopathy having neuropathy.[22,23] Explanation for a lower rate of diabetic neuropathy among Indians may be due to better skin micro-vascularization compared to Europeans despite having similar risk factors.[24]
Whether this low rate for micro vascular complications found in CINDI and other studies from India in comparison to western studies like UKPDS is due to increased screening/earlier detection of diabetes, or a change in risk factors is unclear. Furthermore, the observed differences may be due to the difference in the study designs, methodologies and possibly ethnic differences among various populations.
Prevalence of hypertension was comparable to that found in the Asian population subset of UKPDS, but lower in comparison to other ethnic groups as shown below in Figure 4.[25]
Figure 4.
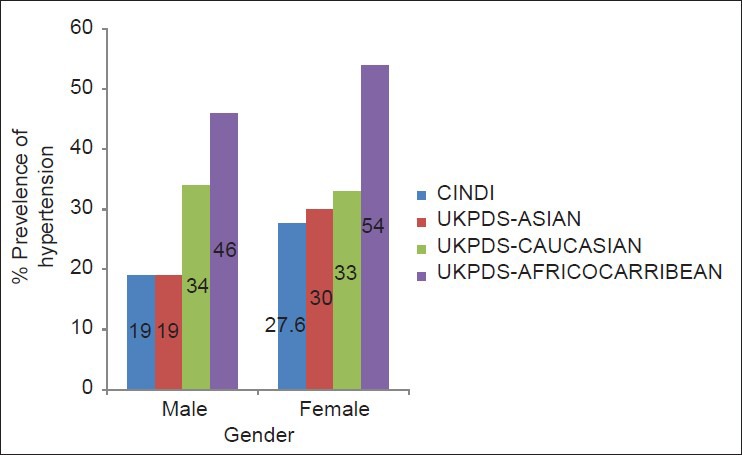
Prevalence of hypertension in newly diagnosed Type 2 diabetics
This is an interesting finding when compared to the known high-risk for cardiovascular disease of the Asian population.
Another important finding emerging is that the prevalence of hypertension is higher for female in comparison to male across all the studies including CINDI and UKPDS subgroups as shown in Figure 4. This combined with higher prevalence of diabetic dyslipidemia in female (31%) in comparison to male (23%) seen in CINDI might account for high-risk of coronary artery disease in female in line with latest International diabetes federation data, which shows higher all-cause mortality in female than a male who were having diabetes. To add more to cardiovascular burden, in CINDI, all lipid parameters were more disturbed in female as compared to male [Table 3].[26]
CINDI data has not compared glycemic parameters with chronic complications as the glycosylated hemoglobin estimations were not carried out in a centralized lab, the values may not all be comparable, although each individual center followed good laboratory practice methods.
Limitations of the study
CINDI data was collected from specialized diabetes centers across the country where Endocrinologists or Diabetologists see the cases. This is a clinic based survey and not an epidemiological study. Prevalence of complications may change in a population based epidemiological study.
Methodology used to diagnose various complications was based on ‘practice pattern’ rather than methods used as ‘gold standards.’ Specificity and sensitivity for diagnosing Neuropathy may slightly change based on methods used.
Mismatch between the number of patients (male vs. female) is just a coincidence as more number of male patients attended the specialized clinics with duration of diabetes < 3 months when the data was being collected. Being an office and hospital based study the gender difference of subjects who presented did not match the population prevalence of diabetes.
CONCLUSION
CINDI reconfirms that screening for both micro vascular and macro vascular complications along with assessment of CV Cardiovascular risk factors must be done at diagnosis in all patients with T2DM. Prevalence of complications may appear low compared to the available western data but is quite high considering the population at risk at the time of diagnosis of T2D in India. This is probably because of the insidious onset of diabetes and asymptomatic nature of the disease before symptoms develop. Lack of awareness can also be a contributing factor in a developing country like India. Futhermore, once complications develop, treating hyperglycemia alone usually does not suffice and complications from diabetes can be prevented only up to a certain point, beyond, which these will progress.
Although in CINDI, the prevalence of micro vascular complications appears to be low, if one were to extrapolate these results to all of India, the number would still be quite staggering. Furthermore, the number of subjects with diabetes is expected to increase to > 100 million by 2030, which could translate into a heavy economic burden and compromise the quality of life.
This underlines for the high importance of screening of all newly diagnosed T2D patients not only for early detection of micro vascular and macro vascular complications, but also to prevent or retard the progression of complications by aggressive management.
Beyond screening, education of our high risk population regarding diabetes related complications must be started to encourage earlier medical consultation. Medical stakeholders must be encouraged to formulate new guidelines as to how aggressive physicians should be in diagnosing and managing diabetes in Indian population.
ACKNOWLEDGMENTS
Dr. Siddharth Das for the conceptual idea of naming this project as “regeneration” and for helping in the performa design. Dr. Kuljinder Singh for review of the manuscript. Dr Sadashiva Rao, Dr. C Munichoodappa, Dr. SS Murthy, Dr. Shobha Aravind, Dr. Sai Subba Rao, Dr. Mala Dharmalingam, Dr. Mayur Patel, Dr. Sharad Pendsay, Dr. Trivedi, Dr. Kabir, Dr. Anil Kumar reddy and Dr. Makkar for contributing cases to CINDI. Dr. Shobha Aravind, Dr. N P Rashmi and Dr. Jayalaksmi for helping in Data tabulation.
Footnotes
Source of Support: UGC, Sri Lanka
Conflict of Interest: None declared
REFERENCES
- 1.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–53. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 2.Mohan V, Deepa R. Adipocytokines and the expanding ‘Asian Indian Phenotype’. J Assoc Physicians India. 2006;54:685–6. [PubMed] [Google Scholar]
- 3.Diabetes Care’ January 2010 Vol. 33 No. supplement 1 S62-S69 Positional statement. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–9. [Google Scholar]
- 4.‘Diabetes Care’January, 2006 Supplement 2 Page Nos S5-S42 Position Statement: Standards of Medical Care in Diabetes-2006 [Google Scholar]
- 5.Marshal SM, Flyvbjerg A. Chapter on “Diabetic nephropathy” Page 599-614, Dan Ziegler, chapter on “Diabetic peripheral neuropathy, page 615-634. In: Holt RI, Cockram CS, Flyvbjerg A, Goldstein BJ, editors. Textbook of Diabetes. 4th ed. Blackwell Publishing Limited; 2010. pp. 599–636. [Google Scholar]
- 6.Mythili A, Kumar KD, Subrahmanyam KA, Venkateswarlu K, Butchi RG. A Comparative study of examination scores and quantitative sensory testing in diagnosis of diabetic polyneuropathy. Int J Diabetes Dev Ctries. 2010;30:43–8. doi: 10.4103/0973-3930.60007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009;57:163–70. [PubMed] [Google Scholar]
- 8.Ramachandran A. Socio-economic burden of diabetes in India. J Assoc Physicians India. 2007;55(Suppl):9–12. [PubMed] [Google Scholar]
- 9.Ramachandran A, Snehalatha C, Sivasankari S, Hitman GA, Vijay V. Parental influence on the spectrum of type 2 diabetes in the offspring among Indians. J Assoc Physicians India. 2007;55:560–2. [PubMed] [Google Scholar]
- 10.McCarthy MI, Hitman GA, Shields DC, Morton NE, Snehalatha C, Mohan V, et al. Family studies of non-insulin-dependent diabetes mellitus in South Indians. Diabetologia. 1994;37:1221–30. doi: 10.1007/BF00399796. [DOI] [PubMed] [Google Scholar]
- 11.Rema M, Ponnaiya M, Mohan V. Prevalence of retinopathy in non insulin dependent diabetes mellitus at a diabetes centre in southern India. Diabetes Res Clin Pract. 1996;34:29–36. doi: 10.1016/s0168-8227(96)01327-7. [DOI] [PubMed] [Google Scholar]
- 12.De Fine Olivarius N, Nielsen NV, Andreasen AH. Diabetic retinopathy in newly diagnosed middle-aged and elderly diabetic patients. Prevalence and interrelationship with microalbuminuria and triglycerides. Graefes Arch Clin Exp Ophthalmol. 2001;239:664–72. doi: 10.1007/s004170100324. [DOI] [PubMed] [Google Scholar]
- 13.Tălu S, Kaucsar E, Soreanu A. Diabetic retinopathy in newly diagnosed patients with type II diabetes mellitus. Oftalmologia. 2002;54:27–30. [PubMed] [Google Scholar]
- 14.Tzeng TF, Hsiao PJ, Hsieh MC, Shin SJ. Association of nephropathy and retinopathy, blood pressure, age in newly diagnosed type 2 diabetes mellitus. Kaohsiung J Med Sci. 2001;17:294–301. [PubMed] [Google Scholar]
- 15.Rema M, Premkumar S, Anitha B, Deepa R, Pradeepa R, Mohan V. Prevalence of diabetic retinopathy in urban India: The Chennai Urban Rural Epidemiology Study (CURES) eye study, I. Invest Ophthalmol Vis Sci. 2005;46:2328–33. doi: 10.1167/iovs.05-0019. [DOI] [PubMed] [Google Scholar]
- 16.Kohner EM, Aldington SJ, Stratton IM, Manley SE, Holman RR, Matthews DR, et al. United Kingdom Prospective Diabetes Study, 30: Diabetic retinopathy at diagnosis of non-insulin-dependent diabetes mellitus and associated risk factors. Arch Ophthalmol. 1998;116:297–303. doi: 10.1001/archopht.116.3.297. [DOI] [PubMed] [Google Scholar]
- 17.Rema M, Pradeepa R. Diabetic retinopathy: An Indian perspective. Indian J Med Res. 2007;125:297–310. [PubMed] [Google Scholar]
- 18.Unnikrishnan RI, Rema M, Pradeepa R, Deepa M, Shanthirani CS, Deepa R, et al. Prevalence and risk factors of diabetic nephropathy in an urban South Indian population: The Chennai Urban Rural Epidemiology Study (CURES 45) Diabetes Care. 2007;30:2019–24. doi: 10.2337/dc06-2554. [DOI] [PubMed] [Google Scholar]
- 19.Adler AI, Stevens RJ, Manley SE, Bilous RW, Cull CA, Holman RR, et al. Development and progression of nephropathy in type 2 diabetes: The United Kingdom Prospective Diabetes Study (UKPDS 64) Kidney Int. 2003;63:225–32. doi: 10.1046/j.1523-1755.2003.00712.x. [DOI] [PubMed] [Google Scholar]
- 20.Weerasuriya N, Siribaddana S, Dissanayake A, Subasinghe Z, Wariyapola D, Fernando DJ. Long-term complications in newly diagnosed Sri Lankan patients with type 2 diabetes mellitus. QJM. 1998;91:439–43. doi: 10.1093/qjmed/91.6.439. [DOI] [PubMed] [Google Scholar]
- 21.Spijkerman AM, Dekker JM, Nijpels G, Adriaanse MC, Kostense PJ, Ruwaard D, et al. Microvascular complications at time of diagnosis of type 2 diabetes are similar among diabetic patients detected by targeted screening and patients newly diagnosed in general practice: The hoorn screening study. Diabetes Care. 2003;26:2604–8. doi: 10.2337/diacare.26.9.2604. [DOI] [PubMed] [Google Scholar]
- 22.Karmakar RN, Khandakar MR, Gangopadhyay PK, Ghosh K, Babu AS. Albuminuria and neuropathy in newly detected diabetics: Profile and correlation. J Indian Med Assoc. 2011;109:396–9. [PubMed] [Google Scholar]
- 23.Rani PK, Raman R, Rachapalli SR, Pal SS, Kulothungan V, Sharma T. Prevalence and risk factors for severity of diabetic neuropathy in type 2 diabetes mellitus. Indian J Med Sci. 2010;64:51–7. [PubMed] [Google Scholar]
- 24.Abbott CA, Chaturvedi N, Malik RA, Salgami E, Yates AP, Pemberton PW, et al. Explanations for the lower rates of diabetic neuropathy in Indian Asians versus Europeans. Diabetes Care. 2010;33:1325–30. doi: 10.2337/dc09-2067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.UKPDS study group. UK Prospective Diabetes Study. XII: Differences between Asian, Afro-Caribbean and white Caucasian type 2 diabetic patients at diagnosis of diabetes. UK Prospective Diabetes Study Group. Diabet Med. 1994;11:670–7. [PubMed] [Google Scholar]
- 26.Unwin N, Gan D, Whiting D. The IDF Diabetes Atlas: Providing evidence, raising awareness and promoting action. Diabetes Res Clin Pract. 2010;87:2–3. doi: 10.1016/j.diabres.2009.11.006. [DOI] [PubMed] [Google Scholar]


