Abstract
Objectives:
DiabCare India 2011 was a cross-sectional study in patients with diabetes mellitus, undertaken to investigate the relationship between diabetes control, management and complications in a subset of urban Indian diabetes patients treated at referral diabetes care centres in India.
Materials and Methods:
This was a cross-sectional, multicentre (330 centres) survey in 6168 diabetes patients treated at general hospitals, diabetes clinics and referral clinics across India. Patient data, including medical and clinical examination reports during the past year were collected during their routine visit. The patients’ and physicians’ perceptions about diabetes management were recorded using a questionnaire.
Results:
A total of 6168 subjects with diabetes (95.8% type 2), mean age 51.9 ± 12.4 years and mean duration of diabetes, 6.9 ± 6.4 years were included. Mean HbA1c was 8.9 ± 2.1% and the mean fasting (FPG), post prandial (PPG) and random (RBG) plasma glucose levels were 148 ± 50 mg/dl 205 ± 66 mg/dl and 193 ± 68mg/dl respectively. Neuropathy was the most common complication (41.4%); other complications were: Foot (32.7%), eye (19.7%), cardiovascular (6.8%) and nephropathy (6.2%). The number of diabetic complications increased with mean duration of diabetes. Most (93.2%) of the patients were on oral anti-diabetic drugs (OADs) and 35.2% were on insulin (±OADs). More than 15% physicians felt that the greatest barrier to insulin therapy from patient's perspective were pain and fear of using injectable modality; 5.2% felt that the greatest barrier to insulin therapy from physician's perspective was the treatment cost; 4.8% felt that the major barriers to achieve optimum diabetic care in practice was loss to follow-up followed by lack of counselling (3.9%) and treatment compliance (3.6%).
Conclusion:
DiabCare India 2011 has shown that type 2 diabetes sets in early in Indians and glycaemic control is often sub-optimal in these patients. These results indicate a need for more structured intervention at an early stage of the disease and need for increased awareness on benefits of good glycaemic control. It cannot be overemphasized that the status of diabetes care in India needs to be further improved. (ClinTrials.gov identifier: NCT01351922)
Keywords: Control and complications, current status of diabetes care, DiabCare India
INTRODUCTION
Diabetes mellitus is recognized as the fourth most commonly diagnosed chronic condition after hypertension, arthritis and dyslipidemia.[1] It is the most common cause of macrovascular and microvascular complications, posing a huge international health burden. According to the International Diabetes Federation (IDF) Diabetes Atlas 2011, the number of people living with diabetes is expected to rise from 366 million in 2011 to 552 million by 2030 if preventive programmes are not put in place.[2] This dramatic rise in the prevalence of diabetes has been associated with fast population growth, ageing and urbanization leading to altered lifestyle. Apart from age, multiple risk factors like family history of diabetes, obesity, hypertension, are also significantly associated with diabetes.[3] A high proportion of people with diabetes in the age group of 45-64 years has been reported from the developing countries and by the year 2025,[4] it is expected that 75% of all people with diabetes would reside in the developing countries like India, which already has the second highest number of people with diabetes in the world. The Indian Council of Medical Research-India Diabetes (ICMR-INDIAB) study estimates the number of people with diabetes in India as approximately 62.4 million.[3] A decrease in the prevalence of diabetes has been observed after 65 years of age which may be due to deaths at early age due to diabetes complications.[3] Therefore, surveillance of diabetes and its risk factors is the first step towards its management, which includes prevention and control of diabetes.
“DiabCare” is a generalized clinical database which gathers information from thousands of diabetes patients and monitors their improvement and potentially involves participation of many physicians. The details of this model have been described elsewhere.[5] The DiabCare project was initially started in Europe in 1990s and after the success of this project, the DiabCare Asia and DiabCare India projects were designed similar to the Europe DiabCare project in collaboration with Novo Nordisk (NN) and the participating Asian countries and regions, mostly working through their national diabetes associations.[6] The objective was to provide large-scale, yet simple, standardized information about patient characteristics and care received from multiple centres across the country. This project was initiated in 1997 in 6 countries and subsequently extended to 11 countries in 1998.[7] In 2001, DiabCare India was first published which involved patients from primary health care sectors,[8] and in 2003, DiabCare Asia collected information of patients managed by specialist's care.[9] DiabCare India 2011 was initiated with the aim to evaluate the current Status of diabetes management, its control and complication ten years after the completion of the last DiabCare study in India. In the present survey, both physician and patient perceptions of diabetes management were also explored using specific questionnaires. We expect that the DiabCare India 2011 findings will act as an incentive to initiate and improve local diabetes monitoring, prevention and management strategies.
MATERIALS AND METHODS
The DiabCare India 2011 was a cross-sectional survey in patients with type 1 and type 2 diabetes mellitus being treated at general hospitals, diabetes clinics and referral clinics in India. Centres across the country were identified to participate in the study. The investigators from these centres were trained by an advisory board, an expert panel and Novo Nordisk representatives. The primary objective of the study was to evaluate the disease pattern, its management, control status and complication profiles in Indian patients with diabetes. The secondary objectives of the study were to evaluate: (1) the association between the physician and patient perceptions and current treatment practices; (2) the relationship between duration of diabetes and diabetes complications; (3) the relationship between duration of diabetes and quality of life of a patient; (4) psychosocial aspects of diabetes; and (5) areas for possible improvement. Only those patients with diabetes who visited the study centre at least once in the last 3-6 months apart from first visit (to the clinic) and were willing to sign the informed consent form were eligible to participate in this study. All patients, >18 years of age, men or women and willing to participate and comply with the study requirements were enrolled in the study. The patients were allowed to withdraw at will at any point of time during the study. The survey was conducted over a period of eight months and for an individual patient, duration of the study was one day. There were no study specific visit and the data was recorded during their routine visit to the clinic. The study was conducted in accordance with good pharmaco-epidemiological practices and the Declaration of Helsinki.
Data collection
The data was collected by reviewing patient's medical records and clinical examination reports for the past one year and by personal interviews for further information. Patient data included demographic parameters like age, sex, educational status, marital status and ethnicity; baseline medical history included information regarding previous and current treatment; glycaemic parameters (fasting plasma glucose [FPG], postprandial plasma glucose [PPG], random blood glucose [RBG] glycosylated haemoglobin [HbA1c]) and other parameters including (blood pressure [BP], total cholesterol, high density lipoprotein [HDL]-cholesterol, low density lipoprotein [LDL]-cholesterol and serum triglycerides); status of having type 1 and type 2 diabetes mellitus, duration of diabetes, concomitant diseases, risk factors, self-monitoring data, diabetes education, complications, including eye and foot examinations and diabetes management. These parameters were accessed from patients’ records and interviews at the participating physicians’ clinics. The HbA1c assessment was done in a central lab as per National Glycosylated Standardisation Programme (www.ngsp.org/docs/Protocol). Data obtained from these patients were systematically recorded into a case report form designed for the study.
Patient questionnaire
The patient questionnaire was adapted from the Diabetes Attitude, Wishes and Needs (DAWN) survey to evaluate quality of life and compliance to the therapy recommended during the last one year.[10] The questionnaire consisted of 3 parts: (1) WHO-5 Well Being Index; (2) Psychosocial questionnaire; and (3) Compliance questionnaire. At each study centre, the study investigator/physician or his designee interviewed the patient and ensured that all the information was complete and accurately transcribed. Translations and back translations in regional languages were performed as required.
Physician questionnaire
At each centre, the physician/investigator completed a questionnaire designed to capture their perceptions about various aspects of diabetes management. This physician questionnaire was developed after a review of a variety of diabetes-related instruments and finalized by an advisory board.
Statistical analysis
Sample size calculation was based upon prevalence of various microvascular and macrovascular complications in the country which project a broad picture of diabetic control and care prevalent in the country. For calculation of sample size, country specific rates of neuropathy, nephropathy, retinopathy and cardiovascular complications were considered. The complication most specific to diabetes, i.e. diabetic retinopathy was chosen for sample size calculation. The prevalence of diabetic retinopathy in the population with diabetes mellitus has been reported to be 18.0% (95% CI, 16.0-20.1) in a recent study.[11] Sample Size Software nMaster 2.0, was used for sample size calculation with 5% level of significance, 90% power and 15 to 20% margin of error (estimation of single proportions using relative precision). A sample size of 6843 was calculated for this study.
All statistical analyses were performed using SAS® Software version 9.1.3. Continuous variables were summarized with descriptive statistics like N (%), mean, median, standard deviation, range (min: max) and number of missing values (%). Estimates are expressed as mean ± standard deviation or proportions. Pearson's correlation was performed for calculating the correlation between the mean duration of diabetes and the number of diabetic complications.
RESULTS
Demographic characteristics
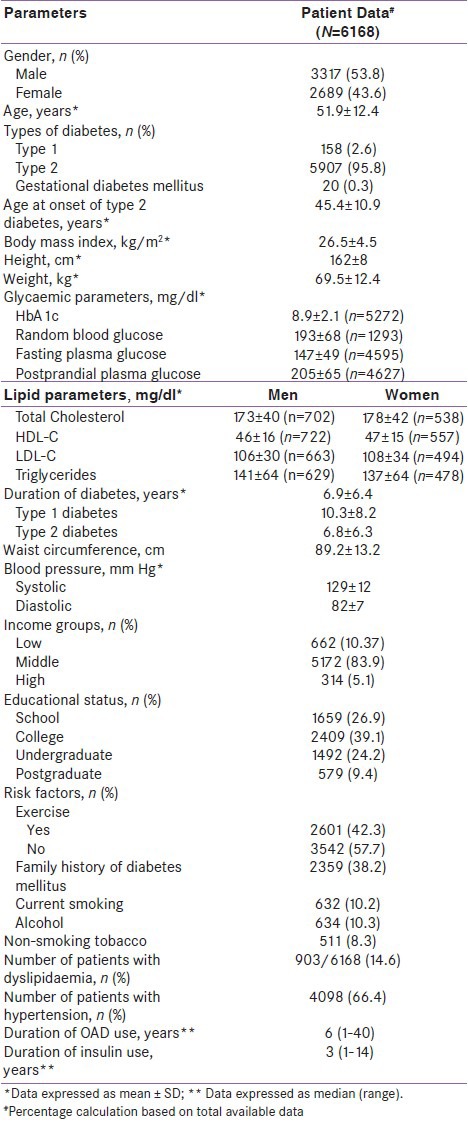
Patient demographics and metabolic characteristics are presented in Table 1. A total of 6168 patients were included in the study and the male/female ratio was 53.8/43.6%. The mean age was 51.9 ± 12.4 years and mean duration of diabetes 6.9 ± 6.4 years. The majority (n = 5907, 95.8 %) of the patients had type 2 diabetes. The mean age at onset of type 2 diabetes was 45.4 ± 10.9 years and the mean duration of treatment of type 2 diabetes, was 6.6 ± 6.1 years. Approximately 84% of the patients belonged to the middle income group; 39% had completed college and only 9.4% were post-graduates. Among the patients enrolled for the study 42.2% (2601/6168) reported regular exercise.
Table 1.
Summary of demographic and metabolic profiles of diabetic population
Glycaemic control
HbA1c was measured in 1745 (28.3%) patients at least once in the previous year. The mean HbA1c was 8.9 ± 2.1% in the overall study population (n = 5272) [type 1 diabetes: mean HbA1c = 9.3 ± 2.3, 16.3 < 7% (n = 145); type 2 diabetes: mean HbA1c = 8.9 ± 2.1, 19.7 < 7%]. The mean values (mg/dl) of FPG, PPG and RBG were, 147 ± 50 mg/dl (n = 4595), 205 ± 66mg/dl (n = 4627) and 193 ± 68 mg/dl (n = 1293) respectively.
Lipid and blood pressure status
The mean (mg/dl) fasting total serum cholesterol, HDL-C, LDL-C and triglycerides were 175 ± 41 mg/dl (n = 1260), 46 ± 15mg/dl (n = 1299), 107 ± 32mg/dl (n = 1177) and 139 ± 64mg/dl (n = 1126), respectively. In patients who received lipid lowering treatment for dyslipidaemia, 82.1 % (682/831) were on statins, 9.6% on fibrates (80/831) and 4% on ezetimibe (33/831). Out of 6168 patients, 4098 (66.4%) were found to have hypertension but only1931 (47.1%) were on anti-hypertensive medications like angiotensin converting enzyme (ACE) inhibitors (794/1931, 41.1%), β-blockers (533/1931, 27.6 %), angiotensin II receptor blockers (313/1931, 16.2%) and calcium channel antagonists (247/1931, 12.8%). Other medications, including diuretics, α-2-agonist, α blockers were used by <10 % patients.
Diabetes complication status
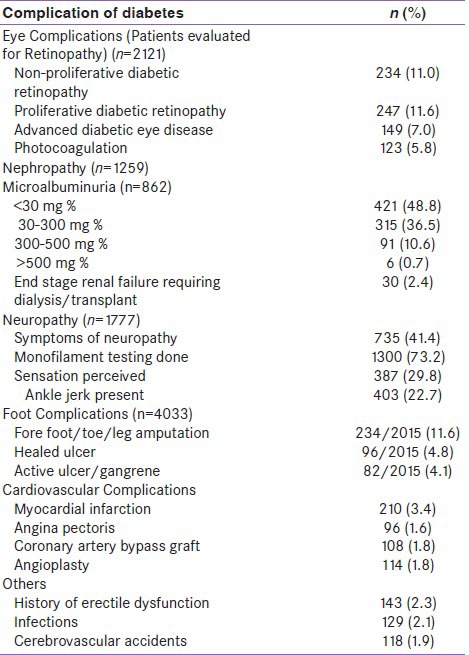
Of 6168 patients, proportion of patients evaluated for complications was as follows: Retinopathy, 2121/6168 (34.4 %); nephropathy, 1259/6168 (20.4%); neuropathy, 1777/6168 (28.8%); peripheral vascular disease, 4033/6168 (65.4%) and cardiovascular diseases 6168/6168 (100%). Prevalence of diabetic complications is presented in Table 2.
Table 2.
Diabetic complications
Microvascular complications
Eye
In all, 1216 (19.7%) patients had at least one diabetic eye complication. Out of 6168 patients with diabetes, 2121 patients were evaluated for retinopathy. Non-proliferative diabetic retinopathy was found in 234 (11%) patients, proliferative diabetic retinopathy in 247 (11.6%) and photocoagulation had been done in 123 (5.8 %).
Nephropathy
Three hundred and eighty (6.2%) patients had diabetic nephropathy. The microalbuminuria test was performed in 862/1259 (68.5%) patients with 36.5% (315/862) testing positive for microalbuminuria (30-300 mg %), while 11.3% (97/862) patients tested positive for macroalbuminuria (>300 mg %). A total of 976 (77.5%) patients were tested for serum creatinine which is the most common modality for assessing renal function. The mean serum creatinine was 0.9 ± 0.4mg/dL. The end stage renal failure requiring dialysis/transplant was present in 2.4% (30/1259) of the patients.
Neuropathy
A total of 1777 (28.8%) were evaluated by the treating physician for signs and symptoms of neuropathy and 14.7% (905/6168) were confirmed to have neuropathy by monofilament testing. Out of 1777 patients who were evaluated for diabetic neuropathy, 41.4% (735/1777) had symptoms of neuropathy. Ankle jerk was absent in 22.7% (403/1777) of the patients in whom the test was performed.
Macrovascular complications
Foot infections
A total of 4033 (out of 6168) patients were screened for foot complications out of which 1.3% had active ulcers/gangrene and 1.6% had healed ulcers or gangrene. Fore foot/toe/leg amputation was observed in 3.8% of the patients.
Cardiovascular complications
Four hundred and eighteen (6.8%) patients had cardiovascular complications. Majority (3.4 %, 210/6168) of the patients had myocardial infarction followed by coronary artery bypass (1.75%, 108/6168) and angioplasty (1.85%, 114/6168).
Other complications
Amongst other complications, history of erectile dysfunction was reported in 2.3% (143/6168) patients followed by infections in 2.1% (129/6168) and cerebral stroke in 1.9% (118/6168) patients.
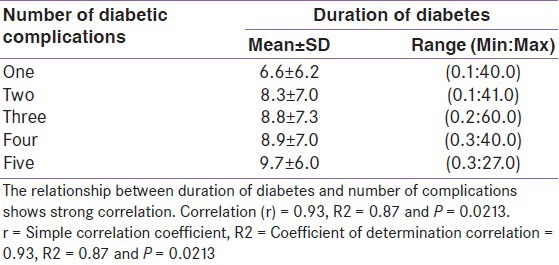
Relationship between duration of diabetes and diabetic complications
The relationship between duration of diabetes with number of diabetic complications is shown in Table 3. The number of diabetic complications increased with mean duration of diabetes; maximum number of diabetic complications was observed with a greater duration of diabetes.
Table 3.
Relationship between duration of diabetes with number of diabetic complications (N=6168)
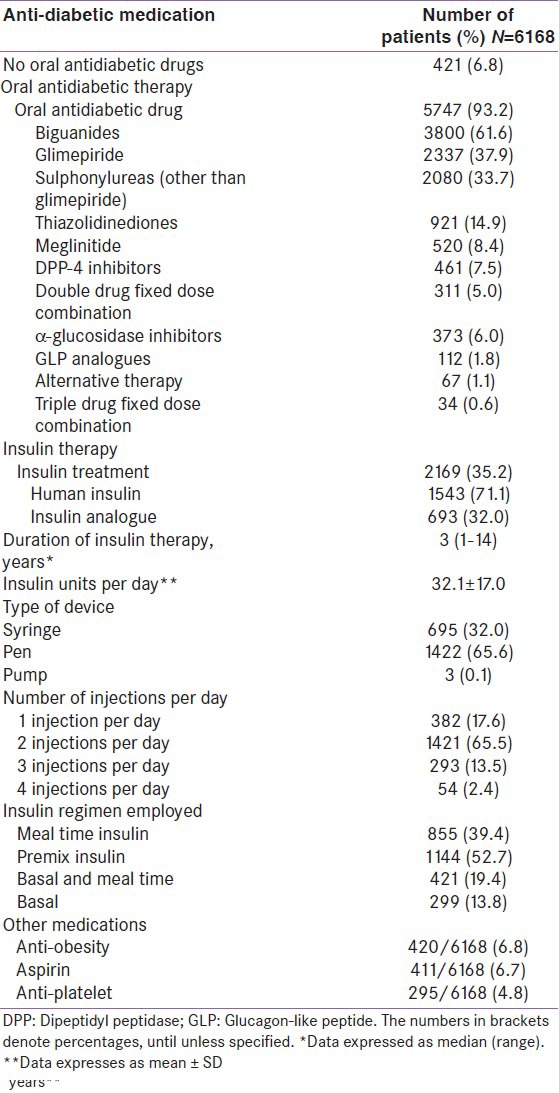
Diabetes management
Of 6168 patients, 5747 (93.2%) were on oral antidiabetic drug (OAD) (± insulin) and 2169 (35.2%) were on insulin (± OADs). Amongst OAD users, majority (61.6 %) of the patients were on biguanides followed by glimepiride (37.9%) and other sulphonylureas (33.7%). Among the insulin users, the majority (71.1%) were taking human insulin and 32% patients were on insulin analogues. Some of the patients (3.1%) were using combination using both analogues and human insulin preparations. The premix insulin (52.7%) was the most common type of insulin used followed by meal time insulin (39.4%) and basal-meal time insulin (19.4%). The median (range; min: max) duration of insulin treatment was 2.00 (0.1: 35) years; mean dose of insulin was 32.1 ± 17units/day; overall 382, 1421, 293 and 54 patients took insulin injections once, twice, thrice and four times per day respectively. In 1422 (65.6%) patients, insulin was administered by a pen device followed by a syringe in 695 (32%) patients and pump in 3 (0.13%) patients out of 2169 patients. Anti-obesity medication was used by 6.8% patients and aspirin treatment in 6.7 % patients. The details on status of diabetes management are given in Table 4.
Table 4.
Diabètes management (DiabCare India 2011)
Patient perceptions
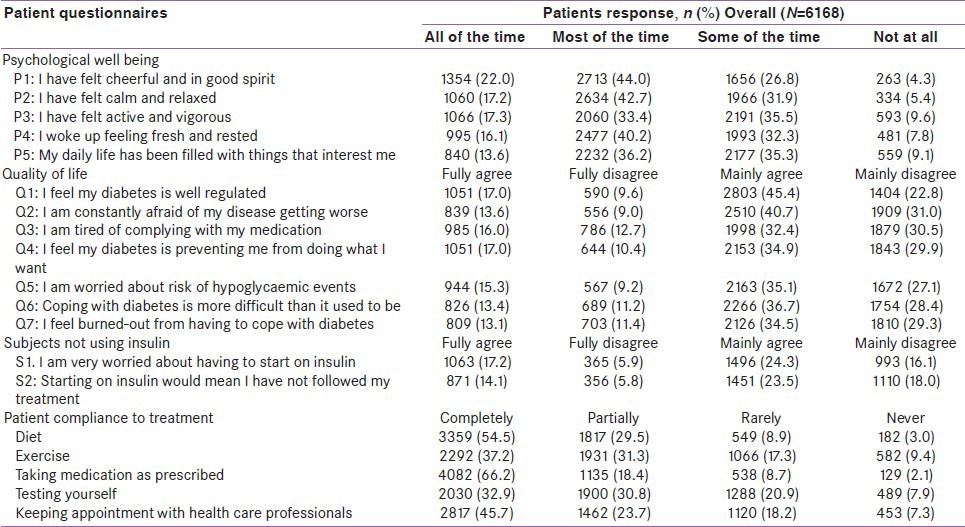
Psychological well-being
Responses to questions on psychological wellbeing fell largely in the positive territory with maximum number of patients indicating that most of the time, they felt “cheerful and were in good spirits” (44%) and 22% felt the same all the time. The percentage of patients who felt “calm and relaxed” most of the time was 42.7% and 17.2% felt the same all the time. Patients who felt that they “woke up feeling fresh and rested” most of the time were 40.2% and 16.1% all the time; 36.2% patients felt their “daily lives had been filled with things that interested them”. 35.5% patients felt “active and vigorous” some of the time and 33.4% felt this most of the time. In addition, majority of the patients who were not using insulin mainly agreed on the question “I am worried about having to start on insulin” (24.3%) and “starting on insulin would mean I have not followed my treatment” (23.5%).
Quality of life
Many patients (45.4%) said yes to the question that their “diabetes is well regulated”, “I am constantly afraid of my disease getting worse” (40.7%), “I am tired of complying with my medications” (32.4%), “I feel my diabetes is preventing me from doing what I want to do”, (34.9%), “I am worried about the risk of hypoglycaemic events” (35.1%), “coping with diabetes is more difficult at present than it used to be” (36.7%) and “I feel burntout from having to cope with diabetes” (34.5%).
Compliance to treatment
Majority of the patients were compliant to their “dietary recommendations” (54.5%), “exercise regimen” (37.2%), “took medications as prescribed” (66.2%), “tested themselves” (32.9%) and in “kept appointment with health care professionals” (45.7%).
Patient perceptions through patient questionnaire are summarized in Table 5.
Table 5.
Summary of patient perceptions through patient questionnaire
Physicians’ perceptions
Majority (89.4%) of the physicians said they advised HbA1c estimation to every patient. If patient's HbA1c was >7% during the course of treatment, 33.6% of the participating physicians preferred HbA1c estimation twice a year followed by 30.3% physicians who preferred to estimate HbA1c four times a year. Physicians around 47.3% of them felt that 20-40% of their patients were under HbA1c target of 7% and 28.8% physicians felt that 40-60% of their patients had HbA1c target of 7-50.9% physicians believed that the dose of OADs must be titrated monthly if the patient's blood sugar was not on target (for those on OADs); 43.9% physicians preferred the dose of insulin to be titrated every 7 days if the patient's blood sugar was not on target (for those on insulin therapy + OADs). 72.7 % physicians advocated the self-monitoring of blood sugar by patients. The majority (92.7%) of physicians felt combination of two OADs and 74.2% use of three OADs was justified in type 2 diabetes patients compared to initiation of insulin therapy. Fifty one per cent of the physicians reported that 25-50% of the patients were on combination of three OADs. Majority (81.8 %) of the physicians recommended initiating insulin therapy in type 2 diabetics when there was OAD failure (HbA1c levels remained >7 even after maximal doses of 2-3 OADs) while 76.1% physicians believed the presence of complications to be a criterion to initiate insulin therapy in these patients.
Majority (90.3%) of physicians had their patients on OADs and/or insulin; 87.6% believed insulin analogues offer distinct advantages in improving glycaemic control and the main advantages were better glycaemic control and less risk of hypoglycaemia. Over 5% of physicians felt that the greatest barrier to insulin therapy from patient's perspective were pain and fear of using an injectable modality (15.5%) and cost and the fear of injections (7%). More than 5% of physicians felt that the greatest barrier to insulin therapy from physician's perspective was the treatment cost followed by lack of awareness (3.9%). As per physicians, the major barriers to achieve optimum diabetic care in practice were loss to follow-up (4.8%), lack of counselling (3.9%), compliance (3.6%), cost of the treatment (2.7%), education (2.7%) and irregular follow-up (2.7%).
DISCUSSION
The DiabCare-Asia-India 1998 had investigated the relationship between diabetes control, management and late complications in a subset of urban Indian diabetes population at 26 tertiary diabetes care centres.[8] The study highlighted poor glycaemic control in over 50% of the study population (n = 2269). More than a decade after the first DiabCare India survey, we continue to report a mean HbA1c (8.9 ± 2.8%) that is almost 2% higher than the ADA recommended target. Type 2 diabetes patients constituted 95.8% of the patients in this study as against 90.6% type 2 diabetes patients in DiabCare Asia 1998, implying that the disease has not been treated optimally.[6] It has been hypothesized that if, before initiation of insulin therapy, a patient's treatment was done in a stepwise manner, (from non-pharmacologic therapy through oral agent monotherapy to a combination oral agent therapy), as mostly done in majority of practice, he or she would accumulate nearly 5 HbA1c-years of total burden >8.0% and about 10 HbA1c-years of total burden >7.0%.[12] It is well accepted that glycaemic control reduces the risk of blindness, renal failure, neuropathy and other microvascular complications in type 2 diabetes.[13] Additionally, good glycaemic control is an important component of cardiovascular disease prevention and treatment.[14] An early intensive glycaemic control reduces the risk of diabetic complications and has long-term influence of early metabolic control on clinical outcomes. This phenomenon has been defined as ‘metabolic memory’.[15] The emergence of the metabolic memory suggests the need for early aggressive treatment aiming to ‘normalize’ metabolic control and reduce cellular reactive species and glycation in order to minimize long-term diabetic complications.
In the present study at time of diagnosis of diabetes, the mean age was 45.4 (±10.9) years which is younger than seen in Europeans. Of significance is the fact that even with state of art referral diabetes clinics in India, patients seek treatment only when complications have started to set in. It can be stated that there appears to be an association between number of complications and duration of diabetes.
Unmet needs in the management of diabetes combined with progressive β-cell failure and persistent insulin resistance attribute to long-term complications of diabetes eventually leading to disability or death. In the present study, 11.6% of the patients had proliferative diabetic retinopathy and another 11% had non-proliferative diabetic retinopathy. The prevalence of diabetic retinopathy has been reported as 18% in an urban population with diabetes mellitus in India. Similarly, the Chennai Urban Rural Epidemiology Study (CURES) reported the prevalence of DR in urban Chennai to be 17.6% in diabetic population,[16] while the Aravind Comprehensive Eye Study reported the prevalence of DR (in self-reported subjects with diabetes) in rural South India to be 10.5%.[17]
In addition, the prevalence of other microvascular complications like nephropathy and neuropathy (confirmed by diagnosis) were 6.2% and 14.7% respectively. It may be worthwhile to note that the overall prevalence of complications tends to be higher in clinic based studies due to referral bias. In other epidemiological studies reported from India, the prevalence of overt nephropathy was 2.2% and that of neuropathy was 26.1%.[18,19] Due to referral patterns in clinics, DiabCare India 2011 study is not meant to be representative of the Indian population as a whole. However, it is remarkable for its focus on the status of diabetes care at referral centres and the current management practices at urban referral centres in India.
Patients with diabetes are known to have a two to four times increased risk for developing cardiovascular disease and CVD has been reported to occur two to three decades earlier in these patients as compared to the non-diabetic population.[20] The identified risk factors for CVD include aging, smoking and a family history of coronary artery disease. Type 2 diabetes is a part of the insulin resistance cluster or metabolic syndrome, which is a consortium of hyperglycaemia, obesity, dyslipidaemia and hypertension. Each of these can contribute independently to the CAD risk or may cluster to increase the risk. In the present study, among 6.8% patients who had cardiovascular complications, myocardial infarction was most commonly reported. The recent years have seen a surge in the prevalence of both diabetes and hypertension. In the recent SITE study it has been reported that 21% suffer from both diabetes and hypertension (leading to a possible twin epidemic). Of the diabetic population already aware of their condition, almost 70% had ‘uncontrolled’ diabetes (HbA1c levels >7%) and of the known hypertensive population 79% were uncontrolled.[21] The DiabCare India study adds that less than half of the patients who have hypertension with diabetes are treated with anti-hypertensive drugs.
Of 22.4% diabetics who underwent lipid measurements, 65.3% (903/1383) of them were found to have dyslipidaemia. A higher number (92%) of patients were receiving lipid lowering agents showing an overall improvement in the management of dyslipidaemia [patients were prescribed statins (82.1), a first line medication for lipid management, followed by fibrates (9.6%)].
It is well known that obesity is an important cause of increasing insulin resistance and prevalence of diabetes in the Indian population as evident from the higher BMI (26.5 ± 4.5kg/m2) observed in this study.[22] Furthermore, waist circumference (WC), which is a better predictor of diabetes and obesity-related cardiovascular risk factors than BMI, was also high (than the cut-off proposed for the Indian population).[22]
There are significant barriers not only to initiating treatment with insulin but also to optimising the dose and intensifying the regimen, all of which are necessary steps to tailor treatment to individual needs and maintain glycaemic control. These barriers arise from the concerns of both physicians and patients.[23] Insulin initiation is becoming more frequent in primary care, but there is still a widespread perception that intensification is the preserve of specialists. Barriers to appropriate insulin therapy increase the likelihood that effective treatment will be delayed and may increase the patient's risk of complications.
Subjective well-being has been described as an important dimension of overall perceived quality of life and in entirety, an important outcome of diabetes care. In people with diabetes emotional well-being may be compromised by the burden of living with diabetes and/or life stresses. Depression has been observed among diabetic subjects, affecting 10-20% of the patient population. Unfortunately the diagnosis of depression is often ignored by health care professionals.[24]
In the present study, patient responses to the WHO-5 well-being index largely fell in the positive territory in agreement with other DiabCare 2008 studies. Our results corroborated with DiabCare Asia and Bangladesh 2008 studies where the majority of the physicians preferred to measure HbA1c, advocated self-monitoring of blood glucose by patients, insulin analogues better to human insulin and recommended the use of insulin delivery devices.[9,25,26] The DiabCare India study also focussed on urban referral centres which cater to the needs of patients from their catchment rural areas as well. The study encompassed the entire geographical spread of India. The present study also draws its strength from the fact that it was an adaptation of the DAWN study. The assessments made were based on questionnaires drawn from the landmark DAWN study. It may be noted that based on key findings from the DAWN study, several goals and strategies were put forth and proved pivotal in improving diabetes care across the globe.[10]
DiabCare India was a cross-sectional study and although it offers several advantages, such as the ease of assessing the prevalence of diseases, a cross-sectional study has limitations. The snapshot nature of cross-sectional studies, while convenient, has the disadvantage that it does not provide a good basis for establishing causality.
Despite these methodological limitations, DiabCare India 2011 has demonstrated that a vast majority of patients with diabetes in India remain sub-optimally controlled. In conclusion, the results indicate a need for more structured intervention at an early stage of the disease and need for increased awareness on benefits of good glycaemic control. It cannot be overemphasized that the status of diabetes care in India needs to be further improved.
ACKNOWLEDGEMENT
The authors thank Max Neeman India (MNI) for statistical analysis and data management; and Dr. Nirupam Sharma (MNI) for project management services.
Footnotes
Source of Support: DiabCare India 2011 Study was sponsored by Novo Nordisk India
Conflict of Interest: Shahid Akhtar and Raman V Shetty are employees of Novo Nordisk. Other authors declare no conflict of interest pertaining to this publication
REFERENCES
- 1.Hsiao CJ, Cherry DK, Beatty PC, Rechtsteiner EA. National Ambulatory Medical Care Survey: 2007 Summary. Natl Health Stat Report. 2010;3:1–32. [PubMed] [Google Scholar]
- 2.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–21. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 3.Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–7. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 4.King H, Aubert RE, Herman WH. Global Burden of Diabetes, 1995-2025 Prevalence, Numerical Estimates and Projections. Diabetes Care. 1998;21:1414–31. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 5.Piwernetz K. DIABCARE Quality Network in Europe--A model for quality management in chronic diseases. Int Clin Psychopharmacol. 2001;16:S5–13. doi: 10.1097/00004850-200104003-00002. [DOI] [PubMed] [Google Scholar]
- 6.Chuang LM, Tsai ST, Huang BY, Tai TY Diabcare-Asia 1998 Study Group. The status of diabetes control in Asia--a cross-sectional survey of 24 317 patients with diabetes mellitus in 1998. Diabet Med. 2002;19:978–85. doi: 10.1046/j.1464-5491.2002.00833.x. [DOI] [PubMed] [Google Scholar]
- 7.Nitiyanant W, Tandhanand S, Mahtab H, Zhu XX, Pan CY, Raheja BS, et al. The DiabCare Asia 1998 study - Outcomes on control and complications in type 1 and type 2 Diabetic Patients. Curr Med Res Opin. 2002;18:317–27. doi: 10.1185/030079902125000822. [DOI] [PubMed] [Google Scholar]
- 8.Raheja BS, Kapur A, Bhoraskar A, Sathe SR, Jorgensen LN, Moorthi SR, et al. DiabCare Asia--India Study: diabetes care in India--current status. J Assoc Physicians India. 2001;49:717–22. [PubMed] [Google Scholar]
- 9.Latif ZA, Jain A, Rahman MM. Evaluation of management, control, complications and psychosocial aspects of diabetics in Bangladesh: DiabCare Bangladesh 2008. Bangladesh Med Res Counc Bull. 2011;37:11–6. doi: 10.3329/bmrcb.v37i1.7793. [DOI] [PubMed] [Google Scholar]
- 10.Rubin RR, Peyrot M, Siminerio LM. Health care and patient-reported outcomes: results of the cross-national Diabetes Attitudes, Wishes and Needs (DAWN) study. Diabetes Care. 2006;29:1249–55. doi: 10.2337/dc05-2494. [DOI] [PubMed] [Google Scholar]
- 11.Raman R, Rani PK, Reddi Rachepalle S, Gnanamoorthy P, Uthra S, Kumaramanickavel G, et al. Prevalence of diabetic retinopathy in India: Sankara Nethralaya Diabetic Retinopathy Epidemiology and Molecular Genetics Study report 2. Ophthalmology. 2009;116:311–8. doi: 10.1016/j.ophtha.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 12.Brown JB, Nichols GA, Perry A. The burden of treatment failure in type 2 diabetes. Diabetes Care. 2004;27:1535–40. doi: 10.2337/diacare.27.7.1535. [DOI] [PubMed] [Google Scholar]
- 13.The Diabetes Control and Complications Trial Research Group (DCCT). The effect of intensive treatment of diabetes on the development and progression of long term complications in IDDM. N Engl J Med. 1993;329:977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 14.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–89. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 15.Ceriello A. Hypothesis: The “metabolic memory”, the new challenge of diabetes. Diabetes Res Clin Pract. 2009;86(Suppl 1):S2–6. doi: 10.1016/S0168-8227(09)70002-6. [DOI] [PubMed] [Google Scholar]
- 16.Rema M, Premkumar S, Anitha B, Deepa R, Pradeepa R, Mohan V. Prevalence of Diabetic Retinopathy in Urban India: The Chennai Urban Rural Epidemiological Study (CURES) Eye Study-1. Invest Ophthalmol Vis Sci. 2005;46:2328–33. doi: 10.1167/iovs.05-0019. [DOI] [PubMed] [Google Scholar]
- 17.Nirmalan PK, Tielsch JM, Katz J, Thulasiraj RD, Krishnadas R, Ramakrishnan R, et al. Relationship between vision impairment and eye disease to vision-specific quality of life and function in rural India: the Aravind Comprehensive Eye Survey. Invest Ophthalmol Vis Sci. 2005;46:2308–12. doi: 10.1167/iovs.04-0830. [DOI] [PubMed] [Google Scholar]
- 18.Unnikrishnan RI, Rema M, Pradeepa R, Deepa M, Shanthirani CS, Deepa R, et al. Prevalence and risk factors of diabetic nephropathy in an urban South Indian population: the Chennai Urban Rural Epidemiology Study (CURES 45) Diabetes Care. 2007;30:2019–24. doi: 10.2337/dc06-2554. [DOI] [PubMed] [Google Scholar]
- 19.Pradeepa R, Rema M, Vignesh J, Deepa M, Deepa R, Mohan V. Prevalence and risk factors for diabetic neuropathy in an urban south Indian population: The Chennai Urban Rural Epidemiology Study (CURES-55) Diabet Med. 2008;25:407–12. doi: 10.1111/j.1464-5491.2008.02397.x. [DOI] [PubMed] [Google Scholar]
- 20.Mohan V, Venkatraman JV, Pradeepa R. Epidemiology of cardiovascular disease in type 2 diabetes: The Indian scenario. J Diabetes Sci Technol. 2010;4:158–70. doi: 10.1177/193229681000400121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joshi SR, Saboo B, Vadivale M, Dani SI, Mithal A, Kaul U, et al. Prevalence of diagnosed and undiagnosed diabetes and hypertension in India--results from the Screening India's Twin Epidemic (SITE) study. Diabetes Technol Ther. 2012;14:8–15. doi: 10.1089/dia.2011.0243. [DOI] [PubMed] [Google Scholar]
- 22.Misra A, Chowbey P, Makkar BM, Vikram NK, Wasir JS, Chadha D, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009;57:163–70. [PubMed] [Google Scholar]
- 23.Peyrot M, Rubin RR, Lauritzen T, Skovlund SE, Snoek FJ, Matthews DR, et al. Resistance to insulin therapy among patients and providers: Results of the cross-national Diabetes Attitudes, Wishes and Needs (DAWN) study. Diabetes Care. 2005;28:2673–9. doi: 10.2337/diacare.28.11.2673. [DOI] [PubMed] [Google Scholar]
- 24.Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE. Psychosocial problems and barriers to improved diabetes management: Results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diabet Med. 2005;22:1379–85. doi: 10.1111/j.1464-5491.2005.01644.x. [DOI] [PubMed] [Google Scholar]
- 25.Soewondo P, Soegondo S, Suastika K, Pranoto A, Soeatmadji DW, Tjokroprawiro A. The DiabCare Asia 2008 study – Outcomes on control and complications of type 2 diabetic patients in Indonesia. Med J Indones. 2010;19:235–44. [Google Scholar]
- 26.Mafauzy M, Hussein Z, Chan SP. The status of diabetes control in Malaysia: Results of DiabCare 2008. Med J Malaysia. 2011;66:175–81. [PubMed] [Google Scholar]


