Abstract
Aims:
To compare waist circumference (WC), body mass index (BMI), waist hip ratio (WHR), and waist-to-height ratio (WHtR) and define an appropriate cut-off, which is most closely predictive of the non-adipose components of the IDF metabolic syndrome (MetS) definition.
Methods and Results:
A total of 3,042 adults (1,693 in rural area and 1,349 in urban area) were screened for the presence of MetS according to the IDF definition. Among 3,042 adults selected as subjects, 1,518 were male and 1,524 were female. The receiver operating curve (ROC) analysis was done to determine the optimal cut-off value and the best discriminatory value of each of these anthropometric parameters to predict two or more non-obese components of metabolic syndrome. The area under ROC (AURC) for WC was superior to that for other anthropometric variables. The optimal cut-off value of WC in urban and rural males was >89 cm, which is higher than that in urban and rural females at 83 cm and 79 cm, respectively; the optimal cut-off for WHtR was >0.51 in rural females, 0.52 in rural males, and 0.53 in both urban males and females. Both parameters were found to be better than BMI and WHR. ROC and AURC values for WC were better than those for WHtR in men and women in both urban and rural areas (P = 0.0054); however, when the entire study cohort was analyzed together, irrespective of gender and place of residence, then at a value of 0.52, WHtR scored over WC as a predictor of metabolic syndrome (P = 0.001).
Conclusion:
Although the predictive value of different gender-specific WC values is clearly superior to other anthropometric measures for predicting two or more non-adipose components of MetS, a single value of WHtR irrespective of gender and the area of residence can be used as a universal screening tool for the identification of individuals at high risk of development of metabolic complications.
Keywords: Anthropometric variables, metabolic syndrome, waist-height ratio
INTRODUCTION
The metabolic syndrome (MetS) is a clustering of metabolic and cardiovascular risk factors that have been widely discussed for at least 20 years. Although some have questioned the clinical utility of metabolic syndrome, there are many reasons to believe that this entity is useful. Identification of metabolic syndrome is a simple measure of finding people with a clustering of risk factors that put them at increased risk of diabetes and cardiovascular disease (CVD). Furthermore, such individuals need more intensive lifestyle interventions at an early stage to delay the disease progression to a still higher-risk category. Also, the identification of metabolic syndrome will attract attention to various other related conditions such as fatty liver, polycystic ovary syndrome, and obstructive sleep apnea. Since the first official definition of the metabolic syndrome put forward by a working group of the World Health Organization (WHO)[1] in 1998, a number of different definitions have been proposed. The latest definition given by International Diabetes Federation (IDF)[2] takes into account the evidence that abdominal obesity is an important component of the metabolic syndrome and proposes gender- and race-specific cut-offs for waist circumference (WC). Although the need for different WC is attributed to ethnic variation, it was observed that even within the same population, people with identical WC but different heights have different risks for metabolic syndrome. Several studies from Asia indicate that waist-to-height ratio (WHtR) is more strongly associated with CVD risk factors than other anthropometric measures such as WC, body mass index (BMI), and waist hip ratio (WHR).[3,4,5,6] The aim of our study was to perform a comparative validation of WC, BMI, WHR, and WHtR for defining the metabolic syndrome in Indian population living in the urban and rural areas of Rohtak district, Haryana, India. We used the IDF definition of metabolic syndrome, excluding the measure of obesity, to determine which obesity measure among WC, BMI, WHR, and WHtR, and what appropriate cut-off value are most closely predictive of the non-adipose components of the IDF's definition of metabolic syndrome.
MATERIALS AND METHODS
This is an investigator initiated cross-sectional study. Informed consent was obtained after explaining the details of the procedure to all subjects. In rural population, two rural blocks out of total were selected randomly. Of these two rural blocks, 85 anganwadi centers (AWC) were selected by the random selection method. From the population survey register of AWC, male and female patients were randomly selected and called at the AWC on a specified date and time after an overnight fast. In urban areas, two out of total six urban health centers were selected randomly, and from the survey registers of these two health centers, male and female patients were selected randomly. A day before the study, all subjects were advised to observe overnight fasting (at least 8 hours) and called at the nearest health center/AWC in the morning. Initial evaluation included detailed history and clinical examination of the subjects to exclude any systemic diseases. Anthropometric indices including height (without shoes and socks), weight, WC, and hip circumference were recorded for the subjects. Height was measured to the nearest 0.1 cm using a portable stadiometer and weight measured to the nearest 0.1 kg using calibrated platform scales. Waist circumference was measured to the nearest 0.1 cm at the midpoint between the subcostal margin and the margin of the supracristal plane according to the IDF diagnostic criteria. Hip circumference was measured to the nearest 0.1 cm around the thighs, at the height of the greater trochanter, with the patients in the standing position. Blood pressure was recorded after patients were made to sit and rest for at least half an hour. Blood pressure was recorded thrice at 5-minute intervals in a sitting position in the non-dominant arm, with the value to the nearest 2 mm Hg, using a standard adult mercury sphygmomanometer. The mean of the three readings was taken as blood pressure. Patients suffering from chronic renal, pancreatic or other severe illness, pregnant women, and women who delivered 2 months or less preceding the study, patients on lipid lowering agents, steroids, nicotinic acid, or other medications likely to cause dysglycemia, were excluded from the study.
In the morning after an overnight fasting period, blood samples were obtained from the antecubital vein and transfused into vacuum tubes containing EDTA. All patients were allowed to sit and rest for at least half an hour before the blood samples were taken. Plasma glucose, total cholesterol, triglycerides, and HDL-cholesterol were measured.
Criteria for metabolic syndrome
According to the IDF definition for the Indian population,[2] for an individual to be defined as having the metabolic syndrome, he/she must be diagnosed as having central obesity defined as waist circumference ≥90 cm in males or ≥80 cm in females plus any two of the following four factors: (1) triglycerides ≥150 mg/dl or specific treatment for this lipid abnormality; (2) HDL-cholesterol <40 mg/dl in males or <50 mg/dl in females or specific treatment for this lipid abnormality; (3) SBP ≥130 mmHg, or DBP ≥85 mmHg or treatment for previously diagnosed hypertension; (4) fasting plasma glucose ≥100 mg/dl or previously diagnosed type 2 diabetes.
All analyses were done separately for men and women and according to their place of residence. Continuous data were expressed as mean ± SD. The optimal cut-off points for BMI, WC, WHR, and WHtR were obtained by selecting a point on the ROC curve, which represented the largest sum of sensitivity and specificity. The area under the ROC curve (AURC) was used as a measure of discrimination of a predictor. The level of statistical significance was set at 0.05. The Youden Index is a frequently used summary measure of the ROC curve. It measures the effectiveness of a diagnostic marker and enables the selection of an optimal threshold value (cut-off point) for the marker. The statistical program for social sciences, version 17.0 (SPSS Inc., Chicago IL), was used for all statistical analyses.
RESULTS
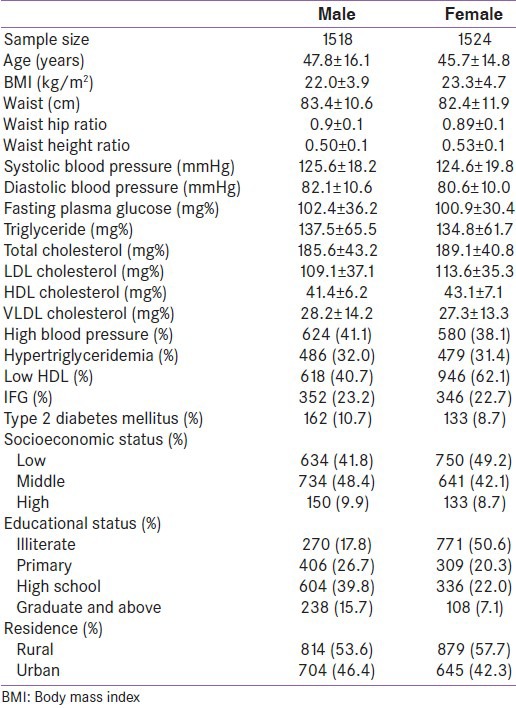
In the present study, 3,042 individuals were screened for the prevalence of metabolic syndrome and their baseline characteristics, as shown in Table 1. Out of the 3,042 individuals selected, 1,693 were from rural areas (male, 814; and female, 879) and 1,349 from urban areas (male, 704; and female, 645). In our study participants, the prevalence of metabolic syndrome according to the IDF criteria was 23.8% and 42.6% in urban men and women, respectively, while it was 14.9% and 36.3% in rural men and women, respectively. In males, high blood pressure was the most common abnormality, followed by low HDL and hypertriglyceridemia. In females, low HDL was the most common abnormality, followed by hypertension and hypertriglyceridemia. Impaired fasting glucose and diabetes mellitus were seen in 23.2% and 10.7% of the men, respectively, while these were seen in 22.7% and 8.7% of the women, respectively.
Table 1.
Baseline characteristics of study subjects stratified by gender
The ROC curve analysis was performed to find out optimal cut-off points for BMI, WC, WHR, and WHtR. The point on the ROC, which represented the largest sum of sensitivity and specificity, was chosen to obtain the optimal cut-off point for each of these four measurements in predicting metabolic syndrome. Figure 1 shows the ROC curves of BMI, WC, WHR, and WHtR for predicting the presence of two or more non-adipose components of metabolic syndrome as defined for both men and women. The optimal cut-off value of WC in urban and rural males was >89 cm, which was higher than that in urban and rural females, i.e. 83 cm and 79 cm, respectively, while the optimal cut-off for WHtR was >0.51 in rural females, 0.52 in rural males, and 0.53 in both urban males and females. Both parameters were found to be better than BMI and WHR. WHR cut-off for the prediction of metabolic syndrome was 0.87 and 0.93, respectively, in rural females and males and 0.92 and 0.95, respectively, in urban females and males. The best cut-off value for BMI was >23 kg/m2 in both urban and rural males as well as urban females, while it was >21 kg/m2 in rural females. Table 2 shows AURC, optimal cut-off values, and the associated measure of each cut-off value. In both men and women, irrespective of their place of residence, WC was found to be a better predictor of metabolic syndrome than WHtR [Table 2].
Figure 1.
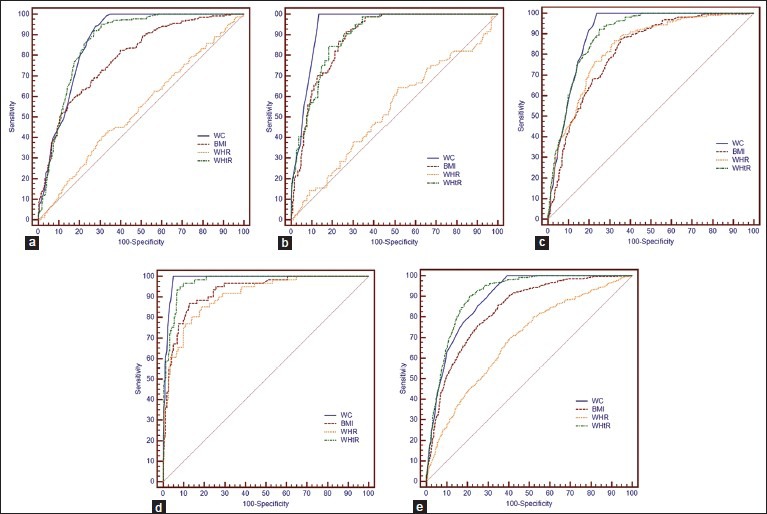
(a) ROC curves of BMI, WC, WHR, and WHtR to predict the presence of two or more non-adipose components of metabolic syndrome in urban females. (b) ROC curves of BMI, WC, WHR, and WHtR to predict the presence of two or more non-adipose components of metabolic syndrome in urban males. (c) ROC curves of BMI, WC, WHR, and WHtR to predict the presence of two or more non-adipose components of metabolic syndrome in rural females. (d) ROC curves of BMI, WC, WHR, and WHtR to predict the presence of two or more non-adipose components of metabolic syndrome in rural males. (e) ROC curves of BMI, WC, WHR, and WHtR to predict the presence of two or more non-adipose components of metabolic syndrome in the entire study population irrespective of gender and place of living
Table 2.
Areas under the ROC curve, cut offs, sensitivity, specificity of WC, BMI, WHR and WHtR
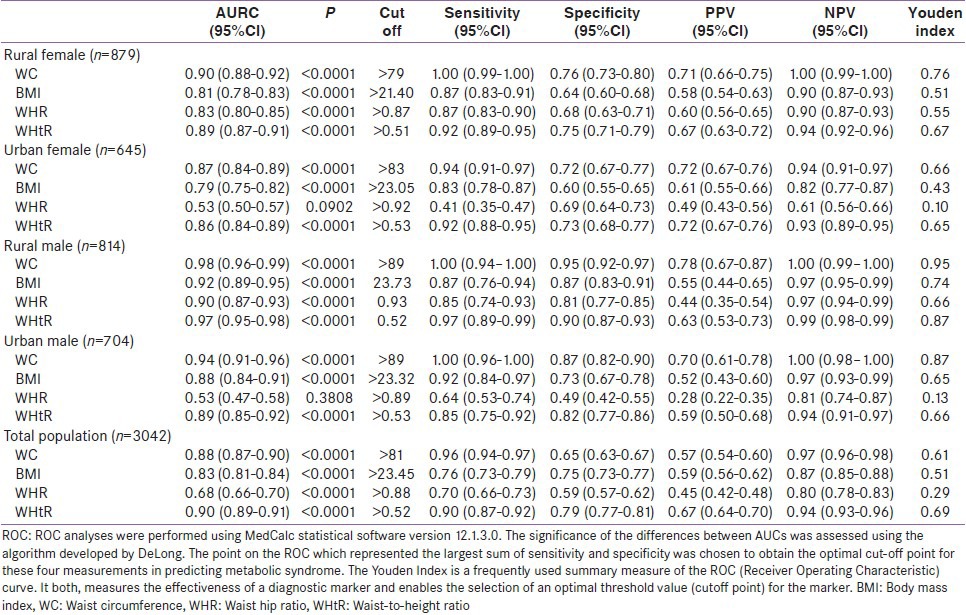
When we compared these anthropometric variables as a predictor of metabolic syndrome irrespective of the place of living and gender, WHtR was found to have the best AURC as a predictor of metabolic syndrome at a cut-off value of 0.52 [Table 2], and it scored over WC as a predictor of metabolic syndrome (P = 0.001).
DISCUSSION
Varying degree of prevalence of metabolic syndrome is reported from various regions of the world and the Indian subcontinent, but very few data is available regarding the prevalence of metabolic syndrome separately in the urban and rural population of Haryana and also regarding which anthropometric parameter of adiposity is best suited for urban and rural population. We found a prevalence of 23.8% (168/704), 14.9% (122/814), 42.6% (275/645), and 36.3% (319/879) in urban men, rural men, urban women, and rural women, respectively, using the IDF diagnostic criteria. Moreover, the prevalence is more common in urban population than in rural population, which is likely due to the higher educational status and sedentary lifestyle of urban population. These results are in accordance with the other studies.[7,8,9]
In the present study, we evaluated and compared the extent to which four different anthropometric variables of adiposity (BMI, WC, WHR, and WHtR) are able to predict two or more non-adipose components of metabolic syndrome using the IDF criteria. It was observed that in both urban and rural men and women, WC is a better predictor of metabolic syndrome than the other three anthropometric variables (BMI, WHR, and WHtR). However, when the entire population was clubbed together and analyzed irrespective of their place of residence and gender, it was found that WHtR scored over WC as a predictor of metabolic syndrome. The optimal cut-off of WHtR for this prediction was 0.52, which is in accordance with several reports from other Asian countries where a cut-off value of WHtR >0.5 appears to offer a simple and reliable index of identifying individuals who face increased future risk of metabolic complications.[3,4,5,6,10]
Traditionally, BMI is a widely popular index of obesity used. Wang et al.,[11] in their study of Chinese population, found that BMI and WC are more useful than WHR for predicting two or more non-adipose components of metabolic syndrome. However, the majority of Asian population is obese and at risk of developing metabolic complications even at BMI cut-off level of ≤25 kg/m2, which is not in accordance with the WHO BMI cut-off level used to define obesity. This has prompted experts across the globe to redefine BMI standards for Asian population, and which is now set at 23 kg/m2 or above for Asian population. In the present study, the BMI cut-off of >23 kg/m2 was also predictive of metabolic syndrome, except in rural females where optimal cut-off for BMI was >21 kg/m2. Despite this change in BMI criteria, its use does not always indicate the degree of obesity. A large number of studies clearly suggest that the degree of central fat distribution is more clearly related to metabolic risk than BMI. In the present study, the comparison of ROC of BMI with that of WC showed that BMI is inferior to WC in predicting metabolic syndrome (P = 0.0001).
WC and WHR have been used as measures of central adiposity and evidences suggest a greater association of these anthropometric variables with a future metabolic risk than BMI, which is a measure of general obesity. Between WC and WHR, several studies have shown that that WC is a better predictor of metabolic syndrome because of variations in the level of hip measurements, differences in cut-off values between men and women and among different ethnic groups, and the possibility of embarrassment to both examiner and examinee when measuring hip circumference.[10,12,13] However, the ability of WC to be used as a universal predictor of central adiposity is limited by the use of different methods for the measurement of WC and different cut-offs used for men and women and for different ethnic groups. In the present study, the optimal cut-off value of WC is >89 cm each in urban and rural males and >83 cm and >79 cm in urban and rural females, respectively, and is clearly superior to WHR in the prediction of metabolic syndrome (P = 0.0001).
WHtR is another anthropometric variable that has been used and found to be a better predictor of metabolic complications in various studies. This is because the height of an individual influences the distribution of body fat, and this factor should be taken into consideration before adopting any anthropometric variable as a measure of adiposity. On average, men are taller than women and have larger waist circumferences. This means that average WHtR values are closer for men and women than average WC values because of adjustments for height, and the same value can be used for both genders to indicate increased risk.[14] Parikh et al.[15] earlier reported that WHtR is a better parameter of central obesity and obviates the need for numerous WC cut-offs; it may be useful in children where existing parameters are not useful. They also reported that using the average height in various countries and their respective WC cut-offs as defined by the IDF consensus definition, the range of WHtR varies from 0.51 to 0.58 among males and from 0.47 to 0.54 among females. In the present study, we also observed that a single value of WHtR at more than 0.52 is a better predictor of metabolic syndrome in both genders. Moreover, for the first time in the present study, we compared both urban and rural population and found that irrespective of the place of living, a single value of WHtR can be used as a marker to identify individuals with a high likelihood of contracting central adiposity and metabolic syndrome. A study conducted on adult females from Singapore demonstrated that WHtR can act as the best screening tool for cardiovascular risk.[16] In Japanese men and women, WHtR was found to be a better predictor of metabolic risk compared to other anthropometric indices.[17] Other studies also reported that the WHtR is a simple and effective screening tool for cardiovascular risk factors in both men and women.[18] In contrast, a Dutch study revealed that height did not significantly influence the differences in measures of adiposity or intra-abdominal fat volume in women, or intra-abdominal fat areas in both genders.[19] Nakamura et al.[20] reported that WHtR did not confer an improved discriminatory performance compared to WC. Kato et al.[21] concluded that the predictive power of WC was not inferior to WHtR, and WC is practically the most convenient measure for predicting metabolic syndrome because of its simplicity. In the present study, the ROC and AURC values for WC are better than that for WHtR in case of men and women in both urban and rural areas (P = 0.0054), but if one has to use a single value for the ease and simplicity of prediction of metabolic syndrome, irrespective of gender and place of residence, then at a value of 0.52, WHtR is a good predictor of metabolic syndrome in comparison to WC where one has to use different values for different gender and place of residence. Also, for disease with a high prevalence in population, such as metabolic syndrome, there is the need for a test with high specificity to ensure all true negative cases are picked up and the test will have a high positive predictive value. The same is true for WHtR, when used irrespective of gender and place of residence, which has high specificity as well as Youden's index.
CONCLUSION
To conclude, although the predictive value of different gender-specific WC values is clearly superior to other anthropometric measures for the diagnosis of metabolic syndrome in both urban and rural population of both genders, a single value of WHtR >0.52 irrespective of gender and area of residence can be used as a universal screening tool for the identification of individuals at high risk to the development of metabolic complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part I: Diagnosis and classification of diabetes mellitus provisional report of WHO consultation. Diabet Med. 1998;15:539–53. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 2.Alberti KG, Zimmet PZ, Shaw J. The metabolic syndrome-a new world-wide definition. A consensus statement from International diabetic federation. Diabet Med. 2006;23:469–80. doi: 10.1111/j.1464-5491.2006.01858.x. [DOI] [PubMed] [Google Scholar]
- 3.Hsieh SD, Yoshinaga H. Abdominal fat distribution and coronary heart disease risk factors in men-waist/height ratio as a simple and useful predictor. Int J Obes Relat Metab Disord. 1995;19:585–9. [PubMed] [Google Scholar]
- 4.Lee JS, Aoki K, Kawakubo K, Gunji A. A study on indices of body fat distribution for screening for obesity. J Occup Health. 1995;37:9–18. doi: 10.1539/sangyoeisei.37.9. [DOI] [PubMed] [Google Scholar]
- 5.Hsieh SD, Yoshinaga H, Muto T, Sakurai Y, Kosaka K. Health risks among Japanese men with moderate body mass index. Int J Obes Relat Metab Disord. 2000;24:358–62. doi: 10.1038/sj.ijo.0801157. [DOI] [PubMed] [Google Scholar]
- 6.Hsieh SD, Yoshinaga H, Muto T. Waist to ratio height, a simple and practical index for assessing central fat distribution and metabolic risk in Japanese men and women. Int J Obes Metab Disord. 2003;27:610–6. doi: 10.1038/sj.ijo.0802259. [DOI] [PubMed] [Google Scholar]
- 7.Gupta A, Deedwania PC, Gupta R, Rastogi S, Pawan RB, Kothari K. Prevalence of metabolic syndrome in an Indian urban population. Int J Cardiol. 2004;97:257–61. doi: 10.1016/j.ijcard.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Misra A, Wasir JS, Pandey RM. An evaluation of candidate definitions of the metabolic syndrome in adult Asian Indians. Diabetes Care. 2005;28:398–403. doi: 10.2337/diacare.28.2.398. [DOI] [PubMed] [Google Scholar]
- 9.Deepa M, Farooq S, Datta M, Deepa R, Mohan V. Prevalence of metabolic syndrome using WHO, ATP III and IDF definitions in Asian Indians: The Chennai urban rural epidemiological study (CURES-34) Diabetes Metab Res Rev. 2007;23:127–34. doi: 10.1002/dmrr.658. [DOI] [PubMed] [Google Scholar]
- 10.Brudavani V, Murthy SR, Kurpad AV. Estimation of deep abdominal adipose tissue (DAAT) accumulation from simple anthropometric measurements in Indian men and women. Eur J Clin Nutr. 2006;60:658–66. doi: 10.1038/sj.ejcn.1602366. [DOI] [PubMed] [Google Scholar]
- 11.Wang F, Wu S, Song Y, Tang X, Marshall R, Liang M, et al. Waist circumference, body mass index and waist to hip ratio for prediction of the metabolic syndrome in Chinese. Nutr Metab Cardiovasc Dis. 2009;19:542–7. doi: 10.1016/j.numecd.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 12.Pauliot MC, Despre JP, Lemieux S, Moorjani S, Bouchard C, Tremblay A, et al. Waist cirfumference and abdominal sagittal diameter: Best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risks in men and women. Am J Cardiol. 1994;73:460–8. doi: 10.1016/0002-9149(94)90676-9. [DOI] [PubMed] [Google Scholar]
- 13.Dalton M, Cameron AJ, Zimmet PZ, Shaw JE, Jolley D, Dunstan DW, et al. Waist circumference, waist hip ratio and body mass index and their correlation with cardiovascular risk factors in Australian adults. J Intern Med. 2003;254:555–63. doi: 10.1111/j.1365-2796.2003.01229.x. [DOI] [PubMed] [Google Scholar]
- 14.Ashwell M. The Ashwell shape chart- A public health approach to the metabolic risks of obesity. Int J Obes Relat Metab Disord. 1998;22(Suppl 3):S213. [Google Scholar]
- 15.Parikh RM, Joshi SR, Menon PS, Shah NS. Index of central obesity-A novel parameter. Med Hypotheses. 2007;68:1272–5. doi: 10.1016/j.mehy.2006.10.038. [DOI] [PubMed] [Google Scholar]
- 16.Pua YH, Ong PH. Anthropometric indices as screening tools for cardiovascular risk factors in Singaporean women. Asia Pac J Clin Nutr. 2005;14:74–9. [PubMed] [Google Scholar]
- 17.Heish SD, Muto T, Yoshinga H, Tsuji H, Arimoto S, Miyagawa M, et al. Waist to height ratio, a simple and effective predictor for metabolic risk in Japanese men and women. Int Congr Ser. 2006;1294:186–9. [Google Scholar]
- 18.Ashwell M, Gibson S. Waist to height ratio is a simple and effective obesity screening tool for cardiovascular risk factors: Analysis of data from the British national diet and nutrition survey of adults 19-64 years. Obes Facts. 2009;2:97–103. doi: 10.1159/000203363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Han TS, McNeill G, Seidell JC, Lean ME. Predicting intraabdominal fatness from anthropometric measures: The influence of stature. Int J Obes Relat Metab Disord. 1997;21:587–93. doi: 10.1038/sj.ijo.0800446. [DOI] [PubMed] [Google Scholar]
- 20.Nakamura K, Nanri H, Hara M, Higaki Y, Imaizumi T, Taguchi N, et al. Optimal cut off values of waist circumference and the discriminatory performance of other anthropometric indices to detect the clustering of cardiovascular risk factors for metabolic syndrome in Japanese men and women. Environ Health Prev Med. 2011;16:52–60. doi: 10.1007/s12199-010-0165-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kato M, Takahashi Y, Inoue M, Tsugane S, Kadowaki T, Noda M JPHC Study Group. Comparison between anthropometric indices for predicting the metabolic syndrome in Japanese. Asia Pac J Clin Nutr. 2008;17:223–8. [PubMed] [Google Scholar]


