Abstract
Background:
Papillary thyroid microcarcinoma (PTMC) describes a focus of papillary thyroid cancer that is less than 1 cm in size. These tumors are frequently found on histopathological examination of thyroid specimens, operated upon for an indication other than suspected malignancy.
Materials and Methods:
From 2005 to 2012, 94 of 1300 thyroidectomy specimens in our institution were found to have PTMC. Of these, 77 were isolated PTMC while the others were associated with other differentiated cancers. We studied their clinicopathologic features, treatment and long-term outcome.
Results:
There were 18 men and 59 women (the male: female ratio was 1:3), their mean age was 44 ± 10.5 years (range: 18-72 years). Multinodular goiter was the most common indication for surgery. Malignancy was suspected in only 31.4% cases. The mean tumor size was 4.1 ± 2.3 mm. Nearly 17% cases had slightly larger tumors measuring >6 but <10 mm. Multifocal tumor was found in 44.1% of cases and among these, multifocal disease restricted to a single lobe was found in 19.5%. Eleven patients (14.2%) had cervical lymph node metastasis, 3 (3.9%) had extra thyroid tumor extension and 2 (2.6%) had evidence of vascular invasion. One patient (1.3%) presented with bone metastasis. Majority of the patients (79.2%) underwent total thyroidectomy with or without lymph node dissection. Sixteen patients (20.7%) who had initially undergone hemithyroidectomy went on to have completion thyroidectomy. Twenty nine patients (36.8%) also received radioactive iodine. The mean duration of follow-up was 20.2 ± 13.5 months. On follow-up one patient developed cervical lymph node recurrence and one died due to a second malignancy.
Conclusions:
PTMC is often found as an incidental finding on the thyroidectomy specimen. Sometimes they present with regional lymph node metastasis and very rarely with distant metastasis. They have a good prognosis similar to papillary thyroid carcinoma.
Keywords: Micro papillary cancer, papillary thyroid micro cancer, thyroid micro cancer
INTRODUCTION
The World Health Organization describes papillary thyroid microcarcinoma (PTMC) as a focus of papillary thyroid cancer <1 cm in size.[1] These tumors are frequently found as a histological surprise following excision of benign thyroid tumors. Even though these tumors are small, a small proportion can behave aggressively and they can present with lymph node/distant metastasis. In low risk cases, the extent of surgery and the adjuvant therapy to be used is still being debated. In this study, we looked at the profile of these patients and their clinical outcome.
MATERIALS AND METHODS
This was a retrospective study of patients with PTMC diagnosed between January 2005 and June 2012. All details pertaining to their clinical presentation, surgery, adjuvant therapy and follow-up were obtained. The data was analyzed using the statistical package for social sciences (SPSS) 17.0 software (SPSS, Inc., Chicago, Illinois).
During this period, 94 cases of PTMC were detected among 1300 thyroidectomy specimens. Among these, there were 77 cases of isolated PTMC and only these were included in the final analysis. The others were excluded because the thyroidectomy specimen also harbored differentiated thyroid malignancies.
All patients had pre-operative assessment of thyroid function. Anti-thyroid antibodies were measured in select patients in whom autoimmune thyroiditis was suspected.
Ultrasonography and fine-needle aspiration biopsy
Ultrasound examination was performed using a 9-12 MHz linear probe. The size of each lobe of the thyroid was measured and the presence of nodules was noted. The features of malignancy included the presence of hypo echoic nodules with irregular margins, loss of peripheral halo, micro calcification, increased central vascularity, the nodule appearing taller than wide and the presence of cervical lymph node enlargement.
Ultrasound guided FNAC was performed when the nodule was <1 cm in diameter. For larger nodules direct FNAC was performed using the multiple aspiration technique. Based on cellularity, colloid consistency and nuclear features the FNAC reports were classified as follows: Inadequate/benign/follicular lesion/indeterminate/malignant.
Details of surgery and adjuvant therapy
Total thyroidectomy was performed when there was multifocal disease involving both lobes of thyroid or when the pre-operative ultrasound showed a nodule in the opposite lobe and the surgeon found nodules in the opposite lobe.
Hemithyroidectomy was performed when there was only a single nodule on one side. If the histopathology showed multifocal disease or the tumor was >6 mm in size, these patients then underwent completion thyroidectomy.
Following surgery all patients with high risk disease underwent whole body I-131 uptake scans.[2,3] Residual disease was treated with 50-100 mCi of I-131.
When there was no clinical recurrence and thyroglobulin levels were undetectable (done after stopping thyroxine for at least 30 days) these patients were declared cured. Patients with aggressive tumors were declared cured based on 3 negative I-131 whole body scans done during their annual follow-up visit.
RESULTS
There were 18 men and 59 women with a male: female ratio of 1:3. The mean age at presentation was 44.54 ± 10.5 years (range: 18-72 years).
Most patients presented with either thyroid enlargement (92.1%) or cervical lymph node enlargement (5.3%). One patient had an incidentally detected thyroid nodule.
The duration of symptoms ranged from <1 month to as long as 25 years.
Nearly 22% of the cases had only isolated thyroid stimulating hormone (TSH) suppression and 6.5% had elevated free thyroxin levels and suppressed TSH. Thyroid antibodies were performed in 30 patients and only 1 was positive.
Of the 77 patients included in the study 60 (77.9%) underwent neck ultrasonography and among them 36.4% had single nodules and 41.6% had multiple nodules. FNAC was performed in 59 (76.6%) patients, 40.3% of them were reported as benign. Overt malignancy or suspicious lesions on FNAC were found only in 26% of the cases [Table 1].
Table 1.
Fine-needle aspiration biopsy
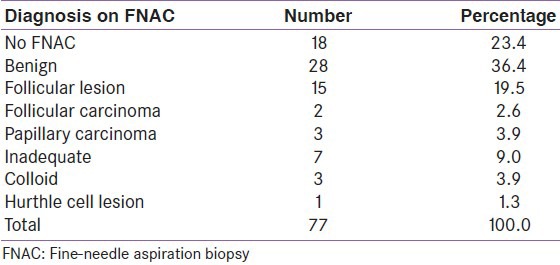
Based on the ultrasound findings and FNAC, 31.4% of the cases were suspected to have an underlying malignancy. The main indication for surgery in the other cases was the presence of large multinodular goiter. Sometimes patients with smaller goiters opted for surgery for cosmetic reasons.
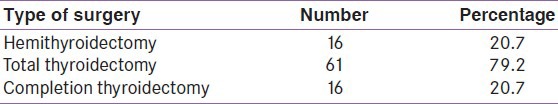
Most of the patients (79.2%) underwent total thyroidectomy [Table 2]. Eleven patients (14.3%) with cervical lymph node metastasis underwent modified radical neck dissection. Following surgery 29 patients (36.8%) received I-131 ablation.
Table 2.
Details of surgery
The mean tumor size was 4.11 mm (range: 0.2-9 mm). Thirteen patients (17%) had tumors >6 mm in size. Multifocal disease was noted in 34 patients (44.1%) and among them 15 (19.5%) had multifocal disease restricted to one lobe. Three patients had extra thyroid extension of the tumor and two had only evidence of vascular invasion on their biopsy.
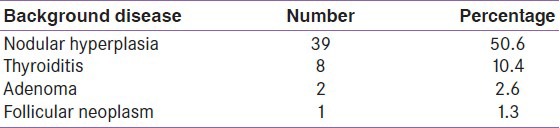
In addition to PTMC, the pathologist noted additional disease in 65% of the thyroidectomy cases. Nodular hyperplasia (50.6%) was the most common condition noted [Table 3].
Table 3.
Background disease
Follow-up
Around 63% of our patients are on regular follow-up. The mean duration of follow-up was 20 months and the maximum duration of follow-up was 57 months.
One patient had metastasis to bone (sacrum). She underwent completion thyroidectomy, which was followed by 3 doses of I-131; she finally succumbed to metastatic disease arising from the pancreas. One patient developed lymph node metastasis 2 years following surgery and I-131 ablation.
On follow-up, 14.5% of patients with aggressive tumors were declared cured of the disease.
DISCUSSION
This study gives an overview of the clinical profile of patients with papillary microcarcinoma treated in our institution over the past 7 years. The male: female ratio of 1:3 is lower compared with the larger female preponderance seen among the Japanese people.[2] This could be because of a much larger load of thyroid cancers observed among the Japanese.
The mean age of our patients was 44 ± 10.52 years (range: 18-72 years) and this was similar to that described in earlier studies. There was a wide range in the duration of symptoms. It is well- known that long standing goiters can turn malignant. Papillary carcinomas as well as micro carcinomas are the most common malignancy seen in autopsy specimens with multinodular goiter.[4] In some studies underlying Graves’ disease was found to be a risk factor for thyroid malignancy.[5,6] This was not the case in our study as no case of Graves’ disease was noted among our patients. The deranged thyroid function tests in our patients was due overtreatment with thyroxin as most patients with thyroid nodules are routinely treated with Thyroxin by their local physicians.
With the advent of ultrasonography, smaller nodules and bilateral disease are recognized very early. The most common indication for surgery in our patients was a multinodular goiter (36.8%). A composite clinical diagnosis based on radiology and guided FNAC will ensure accurate diagnosis of these tumors.
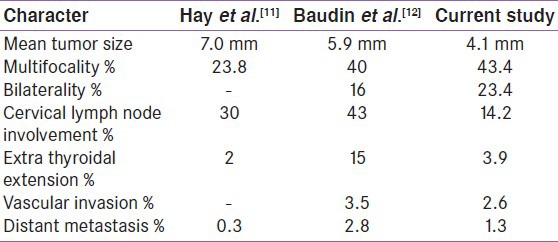
The mean tumor size (4.1 ± 2.3 mm) was comparable with that of other studies. Only 17% patients had tumors >6 mm in size. Noguchi et al.[2] reported that >40% of their patients had tumors >6 mm in size.
Rarely, PTMC can behave aggressively leading to early metastasis. However, the vast majority remain quiescent, causing no symptoms or threat to life. All patients in this study with metastatic disease had multifocal cancer, indicating that, multifocality would mean a more aggressive tumor.[7]
In a recent study from Italy by Malandrino et al.,[8] tumor size, lymph nodes, extra thyroidal extension and multifocality were considered as risk factors for recurrence. In our study, recurrence was not associated with large tumor size. Patients who had recurrence had tumors 2-3 mm in size. Buffet et al.[9] reported that, lymph node metastasis at presentation, multifocality and the male sex is associated with recurrence.
An interesting finding of multifocal disease restricted to a single lobe was observed in our study. This could mean that multifocality restricted to a single lobe likely formed from a single clone, rather than from intra thyroidal hematological spread of tumor.[10] This would probably make hemithyroidectomy a sufficient choice in low risk disease.
Comparing our data with other studies, extra thyroidal extension and cervical lymph node metastases were less common in our patients[11,12] [Table 4].
Table 4.
Comparison of data
Limitations
This study is limited by the short duration of follow-up and small numbers. We also have not looked into the pathological subtypes of PTMC (e.g., Tall cell and insular variants), which are more aggressive.
CONCLUSIONS
This study will provide baseline data about PTMC's from India. PTMC was most often diagnosed incidentally following surgery for multinodular goiters. It is important to stratify risk and treat these patients accordingly. Even the rare aggressive tumors respond well to treatment. Multifocality is an important risk factor for tumor recurrence.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Sugitani I, Kasai N, Fujimoto Y, Yanagisawa A. A novel classification system for patients with PTC: Addition of the new variables of large (3 cm or greater) nodal metastases and reclassification during the follow-up period. Surgery. 2004;135:139–48. doi: 10.1016/s0039-6060(03)00384-2. [DOI] [PubMed] [Google Scholar]
- 2.Noguchi S, Yamashita H, Uchino S, Watanabe S. Papillary microcarcinoma. World J Surg. 2008;32:747–53. doi: 10.1007/s00268-007-9453-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yamashita H, Noguchi S, Murakami N, Toda M, Uchino S, Watanabe S, et al. Extracapsular invasion of lymph node metastasis. A good indicator of disease recurrence and poor prognosis in patients with thyroid microcarcinoma. Cancer. 1999;86:842–9. doi: 10.1002/(sici)1097-0142(19990901)86:5<842::aid-cncr21>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 4.Lang W, Borrusch H, Bauer L. Occult carcinomas of the thyroid. Evaluation of 1,020 sequential autopsies. Am J Clin Pathol. 1988;90:72–6. doi: 10.1093/ajcp/90.1.72. [DOI] [PubMed] [Google Scholar]
- 5.Pearce EN, Braverman LE. Papillary thyroid microcarcinoma outcomes and implications for treatment. J Clin Endocrinol Metab. 2004;89:3710–2. doi: 10.1210/jc.2004-1189. [DOI] [PubMed] [Google Scholar]
- 6.Pellegriti G, Belfiore A, Giuffrida D, Lupo L, Vigneri R. Outcome of differentiated thyroid cancer in Graves› patients. J Clin Endocrinol Metab. 1998;83:2805–9. doi: 10.1210/jcem.83.8.4997. [DOI] [PubMed] [Google Scholar]
- 7.Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Revised American Thyroid Association Management Guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009;19:1167–214. doi: 10.1089/thy.2009.0110. [DOI] [PubMed] [Google Scholar]
- 8.Malandrino P, Pellegriti G, Attard M, Violi MA, Giordano C, Sciacca L, et al. Papillary thyroid microcarcinomas: A comparative study of the characteristics and risk factors at presentation in two cancer registries. J Clin Endocrinol Metab. 2013;98:1427–34. doi: 10.1210/jc.2012-3728. [DOI] [PubMed] [Google Scholar]
- 9.Buffet C, Golmard JL, Hoang C, Trésallet C, Du Pasquier Fédiaevsky L, Fierrard H, et al. Scoring system for predicting recurrences in patients with papillary thyroid microcarcinoma. Eur J Endocrinol. 2012;167:267–75. doi: 10.1530/EJE-12-0105. [DOI] [PubMed] [Google Scholar]
- 10.Shattuck TM, Westra WH, Ladenson PW, Arnold A. Independent clonal origins of distinct tumor foci in multifocal papillary thyroid carcinoma. N Engl J Med. 2005;352:2406–12. doi: 10.1056/NEJMoa044190. [DOI] [PubMed] [Google Scholar]
- 11.Hay ID, Grant CS, van Heerden JA, Goellner JR, Ebersold JR, Bergstralh EJ. Papillary thyroid microcarcinoma: A study of 535 cases observed in a 50-year period. Surgery. 1992;112:1139–46. [PubMed] [Google Scholar]
- 12.Baudin E, Travagli JP, Ropers J, Mancusi F, Bruno-Bossio G, Caillou B, et al. Microcarcinoma of the thyroid gland: The Gustave-Roussy Institute experience. Cancer. 1998;83:553–9. doi: 10.1002/(sici)1097-0142(19980801)83:3<553::aid-cncr25>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]


