Abstract
Objectives. We combined a metabolic and an epidemiological model of obesity to estimate changes in calorie intake and physical activity necessary to achieve the Healthy People 2020 objective of reducing adult obesity prevalence from 33.9% to 30.5%.
Methods. We used the National Health and Nutrition Examination Survey (1999–2010) to construct and validate a microsimulation model of the US population aged 10 years and older, for 2010 to 2020.
Results. Obesity prevalence is expected to shift toward older adults, and disparities are expected to widen between White, higher-income groups and minority, lower-income groups if recent calorie consumption and expenditure trends continue into the future. Although a less than 10% reduction in daily calorie intake or increase in physical activity would in theory achieve the Healthy People 2020 objective, no single population-level intervention is likely to achieve the target alone, and individual weight-loss attempts are even more unlikely to achieve the target.
Conclusions. Changes in calorie intake and physical activity portend rising inequalities in obesity prevalence. These changes require multiple simultaneous population interventions.
The US federal government’s Healthy People 2020 objectives include reducing obesity prevalence among adults aged 20 years and older from 33.9% in 2005 to 2008 to 30.5%.1 It is unclear how much of a reduction in calorie intake or increase in physical activity would be necessary to achieve this objective, because of real metabolic constraints on people’s ability to lose weight. It is also unclear whether the reduction in calorie intake or increase in physical activity necessary to reach this objective is consistent across age, racial/ethnic, and income groups. The latter question has important implications for targeting interventions to population groups with greatest need.
In the past, mathematical models incorporating either epidemiological or metabolic data have been used to try to answer these questions. Epidemiological models forecast future trends in obesity by extending trends in body mass index (BMI) into the future; metabolic models project how individuals’ actions affect their body weight, taking into account the biochemistry of intake and expenditure.2–6 To understand what population-level changes in calorie intake and physical activity are necessary to achieve the Healthy People 2020 objectives, we created a combined epidemiological–metabolic model.
METHODS
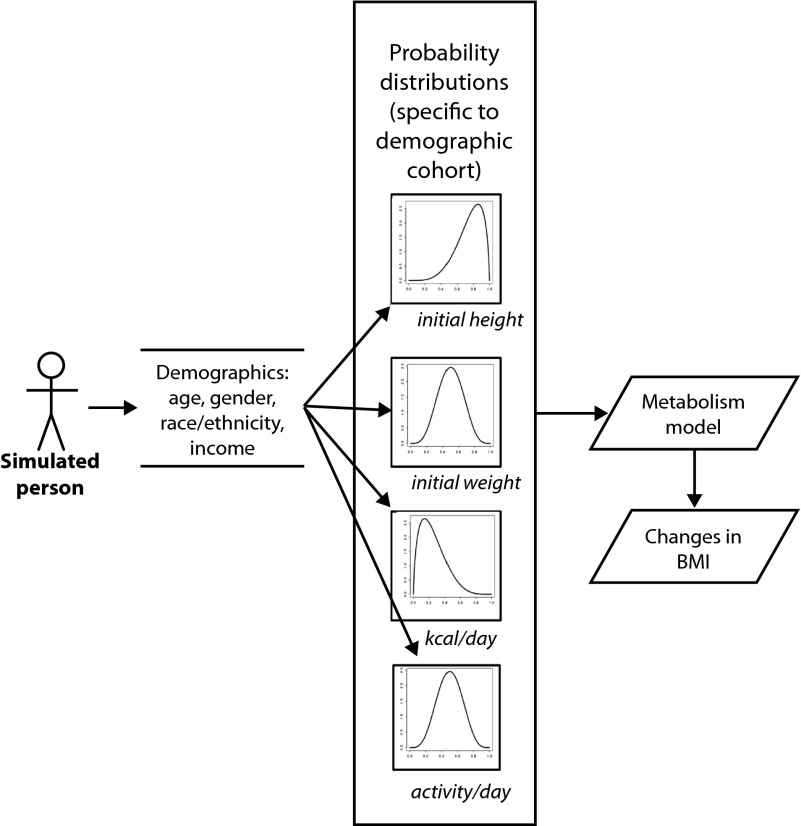
We developed a stochastic, discrete-time, individual-level microsimulation model (Figure 1) informed by data from the National Health and Nutrition Examination Survey (NHANES).9 In accordance with standard reporting guidelines,10 key parameters for the model are itemized with the model’s assumptions in Table 1, and the model’s equations are detailed in Appendix A (available as a supplement to the online version of this article at http://www.ajph.org).
FIGURE 1—
Metabolic–epidemiological simulation model to estimate the changes in energy intake and physical activity necessary to meet the Healthy People 2020 obesity objective.
Note. BMI = body mass index. Simulated persons were assigned an initial height, weight, and typical intake of kcal/d and expenditure of calories via minutes of moderate- or high-intensity physical activity each day. These assignments were made by sampling from probability distributions of each variable, specific to each demographic cohort, accounting for the correlation among these factors when conducting the sampling. Time trends in calorie intake and physical activity (and height for the 10–19-year-old cohort) shifted the distributions of calorie intake and activity to the right or left. A model of metabolism then translated changes in calorie intake and activity into changes in body weight and BMI.7,8
Source. National Health and Nutrition Examination Survey 2009–2010.9
TABLE 1—
Model Parameters, Assumptions, and Data Sources Simulating Changes Needed to Meet Healthy People 2020 Obesity Objective
| Parameter | Key Assumptions | Data Source |
| Baseline weight (kg) and height (m) | Used to calculate BMI among simulated persons | NHANES 2009–20109 |
| Calorie intake/person/d | Derived from 24-h dietary recalls | NHANES 2009–20109 |
| Physical activity/person/d | Reflected by minutes of moderate-intensity and greater activity (work and recreation) | NHANES 2009–20109 |
| Time trends in energy intake and expenditure | Baseline simulation: assumed to be linear change in calories/activity per person per y | NHANES 1999–20109 |
| Sensitivity analyses: varied among subpopulations from baseline levels | ||
| Metabolic parameters: synthesis efficiency and resting metabolic rate of fat and protein, energy content per unit change in body fat and lean tissue, and relative change in lean mass per change in fat mass | Derived from NIH model of in vivo energy metabolism | NIH body weight model7,8 |
Note. BMI = body mass index; NHANES = National Health and Nutrition Examination Survey; NIH = National Institutes of Health.
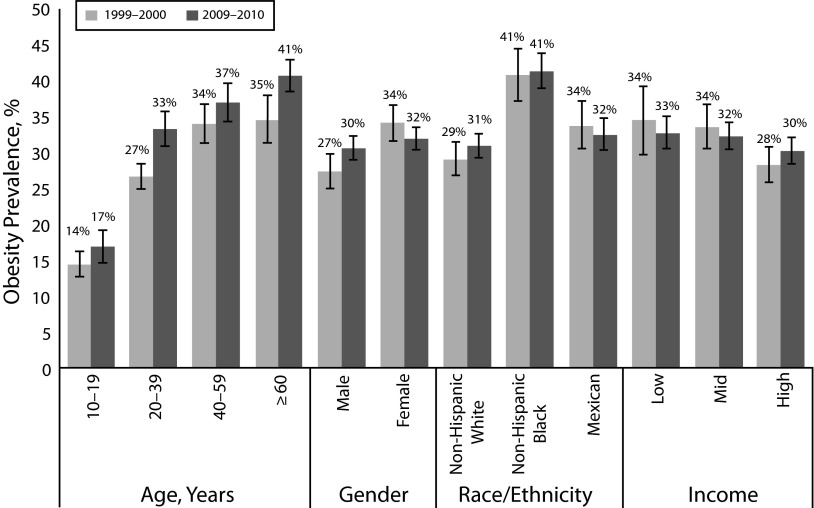
FIGURE 2—
Obesity prevalence (percentage of US population): National Health and Nutrition Examination Survey, 1999–2010.
Note. Obesity was defined as body mass index ≥ 30 kg/m2. The sample size was n = 7776. Survey sample weights were used to generate population-representative estimates. Race/ethnicity was defined by standard National Health and Nutrition Examination Survey categories of non-Hispanic White, non-Hispanic Black, and Mexican American. Income was categorized by poverty income ratio into those living in households with a poverty income ratio of ≤ 1 (low income, < 100% of federal poverty level), > 1–≤ 3 (middle income, 100%–300% of federal poverty level), and > 3 (high income, > 300% of federal poverty level). Error bars reflect 95% confidence intervals around the mean (circle).
Simulated Population
We simulated a nationally representative sample of 10 000 individuals in each of several cohorts defined by all combinations of age (10–19, 20–39, 40–59, and ≥ 60 years), gender, race/ethnicity (with the NHANES categories of non-Hispanic White, non-Hispanic Black, and Mexican American), and income (poverty income ratio ≤ 1, > 1–≤ 3, and > 3), for a total of 72 cohorts. We selected these clusters to ensure sufficient sample size to detect a 1% difference in obesity prevalence among cohorts in NHANES with more than 80% power (n = 46 872). We used POWER software version 3 (National Cancer Institute, Bethesda, MD).
The model incorporated estimates of how racial/ethnic composition and mortality rates differ across age and income groups according to the US Census to account for changing demographics from 2010 to 2020 (Appendix A).11 We simulated ages 10 years and older starting in 2010, so that by 2020 the simulated population would be aged 20 years and older to match the Healthy People target. We did not simulate younger groups because a validated model of metabolism was not available for them at the time of our study.
Simulated Energy Intake and Expenditure
Simulated individuals “ate food” by sampling from the probability distribution of calorie intake corresponding to their cohort (Figure 1). We obtained these probability distributions from NHANES 2009 to 2010 (the most recent data available at the time of our study).9 We estimated calorie intake from 24-hour dietary recall with macros and survey sample weights to account for within-person variation in consumption and differential probabilities of selection, nonresponse, and noncoverage in the population.12 The dietary recall technique used in NHANES is validated against gold standard measures of energy intake.13
Similarly, individuals “exercised” in the model simulation by sampling from their cohort’s NHANES distribution of minutes spent per day in moderate- or high-intensity physical activities (both work and leisure time). We used a correlation matrix to guide the sampling, to account for the correlation between calorie intake and physical activity observed in NHANES (Appendix A shows intake–expenditure distributions). As people age, their calorie intake and activity levels change as well, and we used data from NHANES to account for those changes over the course of the simulation (Table 2 and Appendix A).
TABLE 2—
Time Trends in Calorie Consumption and Physical Activity Among US Subpopulations: National Health and Nutrition Examination Survey 1999–2010
| Variable | Annual Change in Daily kcal Consumption per Person,a Mean (95% CI) | Annual Change in Daily Minutes of Moderate- or High-Intensity Physical Activity per Person, Mean (95% CI) |
| Age, y | ||
| 10–19 | −17.3*** (−26.1, −8.4) | −34.0 (−97.8, 29.9) |
| 20–39 | −13.6*** (−21.6, −5.6) | −21.5 (−62.8, 19.8) |
| 40–59 | 2.9 (−4.5, 10.3) | −53.2 (−115.7, 9.4) |
| ≥ 60 | 4.3 (−1.0, 9.6) | −79.5 (−173.1, 14.1) |
| Gender | ||
| Male | −9.4*** (−14.8, −4.0) | −40.3* (−74.0, −6.7) |
| Female | −6.9*** (−10.4, −3.3) | −22.4 (−75.7, 30.9) |
| Race/ethnicity | ||
| Non-Hispanic White | −8.0*** (−12.7, −3.4) | −41.3* (−76.9, −5.8) |
| Non-Hispanic Black | −5.9 (−12.5, 0.7) | 2.5 (−60.8, 65.9) |
| Mexican American | −3.6 (−9.6, 2.4) | 27.6 (−85.3, 140.5) |
| Incomeb | ||
| Low | −1.8 (−9.7, 6.0) | −55.5 (−141.2, 30.2) |
| Middle | −11.3*** (−17.2, −5.4) | −18.9 (−73.9, 36.1) |
| High | −8.0** (−12.9, −3.0) | −41.0* (−77.6, −4.4) |
| All persons aged ≥ 10 y | −7.5*** (−11.3, −3.6) | −35.7* (−64.7, −6.8) |
Note. CI = confidence interval; NHANES = National Health and Nutrition Examination Survey. Only statistically significant trends at the P < .05 level (2-sided) were incorporated in the model. Values are summary statistics for each demographic category; the model itself sampled directly from NHANES probability distribution functions specific to each individual (i.e., combining all 4 demographic characteristics). The sample size was n = 46 872.
Survey sample weights were used to generate population-representative estimates.
Categorized by poverty income ratio into those living in households with a poverty income ratio of ≤ 1 (low income, > 1–≤ 3 (middle income), and > 3 (high income).
P < .05; **P < .01; ***P < .001.
Estimation of Body Mass Index Changes
We assigned all simulated individuals a starting body weight (in kilograms) and height (in meters) by sampling from their cohort’s distribution of weight and height in NHANES 2009 to 2010; we used a covariance algorithm to account for correlations among weight, height, calorie intake, and physical activity.14 To estimate how changes in calorie consumption and physical activity would be expected to change BMI (defined as weight in kilograms divided by the square of height in meters), we used a previously published, validated model of in vivo energy metabolism constructed by the National Institutes of Health.5 This metabolism submodel used age, gender, height, weight, calorie intake, and activity data to estimate changes in fat, protein, and glycogen storage and shifts between extracellular and intracellular compartments, according to parameters defining the metabolism of body fat, fat-free mass, and adaptive thermogenesis (Appendix A). We chose this model because it has been validated against experimental controlled-feeding studies among humans in the age groups relevant to this simulation, and it more accurately predicted changes in body weight resulting from measured changes in energy intake and physical activity than did alternative models in head-to-head comparisons.7
The key assumptions in the metabolism submodel were that energy must be conserved and that changes in body composition and body weight result from imbalances between the intake and utilization rates of calories along with shifts between intracellular and extracellular compartments.
Simulations
In our baseline simulation, we forecast BMI changes assuming that time trends in calorie intake and physical activity were linear; that is, we estimated the distribution of calories and physical activity in each cohort for each year of the simulation with the assumption that secular trends in consumption and activity would continue linearly over time. For example, as shown in Table 2, persons aged 20 to 29 years reduced their intake by 13.6 kilocalories per person in each year of the simulation. We also accounted for age-related changes in growth along a standard trajectory for the youngest (10–19 years) cohort to ensure accurate calculation of BMI, because this group aged according to a previous model (Appendix A).8 We applied revised international child cutoffs for obesity for individuals younger than 18 years, because BMI cutpoints for adults (BMI ≥ 30 kg/m2) do not apply to this group.15
Our baseline simulation estimated how much of a sustained reduction in calorie intake or increase in physical activity would be required to achieve the Healthy People 2020 obesity prevalence target. Prevalence projections were age adjusted (via the direct method) to produce overall prevalence rates.16 We also estimated what level of population intervention would be needed at the national level to achieve the targeted outcome. We reviewed all 36 Cochrane systematic reviews on obesity, selecting 4 that were relevant to population interventions (as opposed to purely clinical–pharmacological therapies),17–20 and supplemented these systematic reviews with the Institute of Medicine review on population obesity interventions.21
The results of this synthesis are summarized in Table 3; we extracted data on changes in energy intake or expenditure for only those interventions where statistically significant differences in energy intake or physical activity were reported (at the P < .05 level, 2-tailed), with low risk of study bias according to Cochrane metrics and at least 12 months of follow-up or evaluation. We simulated each intervention meeting these criteria by estimating the impact of the change in energy intake–expenditure from the intervention on overall obesity prevalence, assuming optimistically that the intervention had 100% coverage nationwide at the start of 2015.
TABLE 3—
Simulation of Population Interventions to Decrease Obesity
| Intervention | Change in kcal/person/d, % (range) | Change in Physical Activity min/d, % (range) |
| Community-based moderate- or high-intensity exercise programs | 0 (0 to 0.5) | 1.6 (1.1 to 2.4) |
| Community-based moderate- or high-intensity exercise programs + dietary counseling | −1.2 (−2.2 to –0.3) | 1.6 (1.1 to 2.4) |
| Sugar-sweetened beverage tax (20% excise tax, including impact of substitution) | −1.7 (−1.8 to –0.7) | NA |
| Restaurant menu labeling | −1.0 (−2.3 to 0) | NA |
| School-based (youngest cohort 10–19 y) curriculum on physical activity and nutrition with dedicated activity time | −0.1 (−0.2 to 0) | 0.1 (0 to 0.2) |
Note. NA = not available. We identified interventions in studies with ≥ 12-mo duration of follow-up or evaluation, with low risk of study bias, and statistically significant changes in energy intake or expenditure at a significance level of P < .05. Many interventions, such as front-of-package food labels, and several types of other interventions, did not meet the inclusion criteria for sustained significant long-term data.
Sensitivity and Uncertainty Analyses
We performed 3 kinds of sensitivity analysis. First, we modeled the time trends in calorie intake and physical activity with logistic and polynomial regressions (instead of the linear regressions we used in the baseline scenario) for each cohort to examine how different time trend curves affected future obesity prevalence rates.
Second, although we did not simulate a differential mortality rate among overweight and obese individuals in the baseline analysis, in a sensitivity analysis we simulated an additional mortality risk among the obese: average life expectancy was approximately 3 years less on average for persons with BMIs of 30 to 40 (95% confidence interval [CI] = 2, 7) and 9 years for persons with BMIs higher than 40 (95% CI = 8, 10) than for normal-weight individuals, according to pooled prospective cohort data.22,23
Third, it is well known that most individuals who attempt weight loss regain much of their lost weight. In the baseline analysis, we looked at what population-level changes in calorie intake or expenditure would be needed to achieve the Healthy People 2020 objective, but in further sensitivity analyses we estimated what individual-level number of attempts at weight loss would be required, accounting for realistic relapse rates associated with weight-loss attempts. We used a meta-analysis of longitudinal studies to simulate a typical number of 4 weight-loss attempts per year of 1-month duration each among overweight and obese individuals, with an average net reduction of 47 kilocalories per person per day (95% CI = 33, 55), net increase of 11 minutes of moderate- or high-intensity activity per day (95% CI = 8, 13) during attempts, and an average 17% (95% CI = 13%, 22%) probability of long-term maintenance of these changes from each attempt.24
To generate mean and 95% CI estimates for model results, we conducted 100 000 repeated replications of the model by Monte Carlo sampling from the probability distributions of all the input parameters. We regenerated 10 000 individuals per cohort by repeatedly sampling from the input parameters to estimate the uncertainty for the modeled results. We observed that the 100 000 value produced stable estimates of BMI to the nearest 0.1 kilogram per squared meter upon repeated replication. We performed simulations in MATLAB version R2012a (MathWorks, Natick, MA).
RESULTS
The NHANES 1999 to 2010 data set indicates statistically significant time trends in calorie consumption among most US subpopulations (Table 2). Among Americans aged 10 years and older, daily calorie consumption changed by approximately −7.5 kilocalories per person each year from 1999 to 2010 (95% CI = −3.6,−11.3), from a mean intake of 2098 kilocalories per person per day in the 1999 to 2000 survey wave. However, most of this decline was driven by lower consumption among younger groups (10–39 years); older adults increased their calorie consumption on average (Table 2). Calorie consumption declined significantly among both genders, among non-Hispanic Whites, and among middle- and higher-income groups, but not among non-Hispanic Blacks, Mexican Americans, and lower-income populations. Nearly all cohorts also exhibited decreasing physical activity over time; however, most of the secular trends were not statistically significant at the P < .05 level (Table 2).
When we input the 2009 to 2010 levels of weight, height, calorie intake, and physical activity into the simulation model, the model forecast a decline in obesity prevalence from 36% in 2010 (95% CI = 34%, 39%), matching the NHANES 2009 to 2010 estimate, to 34% in 2020 among adults aged 20 years and older (95% CI = 32%, 36%), if statistically significant time trends in energy intake and expenditure continued linearly into the future. Predictions were similar when we examined logistic or polynomial trends rather than linear ones (Table A, available as a supplement to the online version of this article at http://www.ajph.org).
Disparity Trends
We observed widening disparities in obesity prevalence among age, racial/ethnic, and income groups over time (Table 4). Among age groups, obesity prevalence ranged from 33% (20–39 years) to 41% (≥ 60 years) in 2010, but following secular trends, age disparities widened by 2020. For example, the cohort aged 20 to 39 years lowered its obesity prevalence rate from 33% to 27% (95% CI = 25%, 29%), but obesity prevalence increased in the 40- to 59-year age group from 37% to 39% (95% CI = 36%, 41%) and more substantially in the oldest group, aged 60 years and older, from 41% to 44% (95% CI = 42%, 46%) between 2010 and 2020.
TABLE 4—
Simulation Model Projections of Adult Obesity Prevalence in 2020 by Subgroup and Changes in Energy Intake and Physical Activity
| 2020 Obesity Prevalence |
||||||
| Variable | 2010 Obesity Prevalence, Mean % (95% CI) | No Change in Calorie Intake or Physical Activity, Mean % (95% CI) | Cut Daily Calorie Consumption by 8.5%,a Mean (95% CI) % | Increase Daily Physical Activity by 7.5%,b Mean % (95% CI) | Cut Daily Consumption by 50 kcal, Mean % (95% CI) | Add 15 min Daily Exercise, Mean % (95% CI) |
| Age, y | ||||||
| 20–39 | 33.2 (30.8, 35.5) | 26.9 (25.1, 28.7) | 18.8 (17.4, 20.3) | 17.7 (16.3, 19.1) | 24.6 (22.9, 26.3) | 22.6 (21.0, 24.2) |
| 40–59 | 36.8 (34.2, 39.4) | 38.5 (36.1, 40.9) | 25.9 (24.1, 27.8) | 24.6 (22.8, 26.4) | 35.4 (33.1, 37.7) | 31.5 (29.4, 33.7) |
| ≥ 60 | 40.5 (37.8, 43.2) | 43.8 (41.6, 46.0) | 32.2 (30.4, 33.9) | 29.3 (27.7, 30.9) | 39.7 (37.6, 41.7) | 35.6 (33.7, 37.5) |
| Gender | ||||||
| Male | 36.0 (33.8, 38.2) | 34.4 (27.9, 40.8) | 31.1 (24.7, 37.6) | 30.8 (24.5, 37.1) | 33.6 (27.1, 40.1) | 32.9 (26.5, 39.4) |
| Female | 36.7 (34.7, 38.7) | 34.3 (28.5, 40.0) | 30.0 (24.4, 35.5) | 30.2 (24.7, 35.8) | 33.0 (27.3, 38.7) | 31.9 (26.3, 37.5) |
| Race/ethnicity | ||||||
| Non-Hispanic White | 35.4 (33.4, 37.4) | 33.3 (27.5, 39.1) | 29.3 (23.7, 34.8) | 29.0 (23.5, 34.5) | 32.2 (26.4, 37.9) | 31.4 (25.7, 37.0) |
| Non-Hispanic Black | 50.2 (47.1, 53.3) | 49.1 (42.8, 55.4) | 46.4 (40.2, 52.6) | 45.2 (39.2, 51.2) | 48.7 (42.3, 55.0) | 47.8 (41.6, 54.0) |
| Mexican American | 40.1 (36.9, 43.3) | 39.3 (33.1, 45.5) | 36.6 (30.6, 42.6) | 35.8 (29.9, 41.8) | 38.4 (32.3, 44.6) | 38.0 (31.9, 44.0) |
| Incomec | ||||||
| Low | 38.5 (35.3, 41.7) | 38.2 (31.6, 44.8) | 35.5 (29.2, 41.8) | 34.6 (28.2, 41.0) | 37.2 (30.6, 43.7) | 36.6 (30.0, 43.1) |
| Middle | 38.4 (36.0, 40.9) | 35.9 (30.0, 41.9) | 33.1 (27.2, 39.0) | 32.3 (26.4, 38.1) | 35.2 (29.1, 41.2) | 34.4 (28.5, 40.3) |
| High | 34.6 (32.4, 36.8) | 32.5 (26.9, 38.1) | 28.7 (23.3, 34.1) | 28.1 (22.8, 33.5) | 31.4 (25.9, 36.8) | 30.3 (24.9, 35.7) |
| All adults aged ≥ 20 y | 36.4 (34.2, 38.5) | 34.3 (32.3, 36.3) | 30.5 (28.8, 32.3) | 30.5 (28.7, 32.3) | 33.3 (31.4, 35.2) | 32.4 (30.6, 34.3) |
Note. CI = confidence interval. Only statistically significant trends at the P < .05 level (2 sided) were incorporated into the model.
Average of −166 kcal/person.
Average of 29 min/person.
Categorized by poverty income ratio into those living in households with a poverty income ratio of ≤ 1 (low income, > 1–≤ 3 (middle income), and > 3 (high income).
Disparities among racial/ethnic groups increased as well, widening a gap between Whites and both Blacks and Mexican Americans by more than 1%. We observed a larger differential change among income groups: a 4% prevalence difference among high- and low-income groups expanded to a 6% difference because of larger reductions in obesity among high-income than low-income populations (Table 4). Trends in nonobese overweight (BMI 25–< 30 kg/m2) and morbid obesity (BMI ≥ 40 kg/m2) prevalence followed the same patterns.
Reaching Healthy People 2020
Overall, the changes required to reach the Healthy People 2020 target were less than 10%, especially for physical activity. We found that an 8.5% (95% CI = 8.0%, 9.0%) decrease from current daily calorie consumption among each cohort (a 166-kcal drop from 1958 kcal/d to 1792 kcal/d, on average) would be necessary to achieve the overall adult obesity prevalence target, if physical activity levels and trends did not change. However, if all subpopulations reduced calorie consumption by the same 8.5%, we would observe widening disparities among groups, because the obesity prevalence decline would primarily be driven by reductions in BMI among persons aged 20 to 39 years, Whites, and high-income populations (Table 4). Similarly, a 7.5% increase (95% CI = 7.1%, 7.9%) in daily exercise (an additional 29 minutes/person/day on average) would be needed to reach the Healthy People 2020 target, if existing levels and trends in calorie intake remained stable. We found the 2 changes—reducing intake and increasing expenditure—to be physiologically synergistic, such that altering both by about 4% (reducing kcal/d by 4% and increasing minutes of daily activity by 4% from current rates simultaneously; 95% CI = 3.8%, 4.2%) would be sufficient to achieve the Healthy People 2020 target. This amounts to reducing calorie intake by approximately one-half can of sugar-sweetened soda per day and exercising an additional 15 minutes per day.
If all groups responded with similar reductions in calories or increased exercise, rather than as a percentage of their current calorie intake or activity, then disparities would remain relatively stable or slightly decline (Table 4). Reaching the Healthy People 2020 target through equal changes in all groups would require either a reduction of 173 kilocalories per person per day (−8.8%, if physical activity levels and trends did not change) or 30 minutes per day of additional exercise (+6.9%, if calorie intake levels and trends did not change), or roughly half of these levels if calorie intake declined and expenditure increased. Table 4 also displays the change in obesity prevalence for each change of 50 kilocalories per person per day or each additional 15 minutes of exercise per person per day. For example, persons aged 20 to 39 years would be expected to experience a decline in obesity prevalence from 33% to 27% according to current trends in calorie intake, but an additional 50 kilocalories per person per day decline in intake would be expected to reduce prevalence to 25%, and 15 minutes per day of additional exercise would reduce prevalence to 23%.
To allow the obesity prevalence rate among older adults (≥ 60 years) to match that among younger adults (20–39 years) would require a 222-kilocalorie drop from current daily consumption (95% CI = −209, −235; −13.7%) or 35 minutes per day (95% CI = 33, 37; +10.7%) of additional exercise. We found that it is not likely that the obesity prevalence rate among Black populations will match that of White populations during the 10-year period from 2010 to 2020: through calorie reduction alone, even a more than 500-kilocalorie drop in calorie consumption from current daily per capita levels would not allow for a closure of the disparity, because of metabolic time constraints that limit how quickly BMI can decline. Similarly, more than 90 minutes per day of additional exercise would still leave obesity prevalence above 40% among Blacks in 2020 (and only 33% among Whites). Among Mexican Americans, lowering calorie intake by 375 kilocalories from current daily intake (95% CI = −353, −397 kcal/d; −22.0%) or 75 minutes per day of additional exercise (95% CI = 71, 79; +19.7%) would be needed to match the 33% prevalence of Whites. The lowest-income group would need to reduce intake by 72 kilocalories from current daily calorie consumption (95% CI = −67, −76; −4.3%) or increase exercise by 14 minutes per day (95% CI = 13, 15; +3.5%) to match the middle-income population’s obesity prevalence rate of 34%.
No single population-level intervention that appeared in our review (Table 3) would achieve the Healthy People 2020 objective if implemented alone. We modeled interventions as overall cohort-level declines in calorie intake or increases in physical activity, not individual weight-loss attempts. As displayed in Table 3, only a few interventions had sufficient long-term data on sustained energy intake or expenditure changes, and among these interventions, all achieved intake or expenditure changes of less than 2%, well short of the 8% to 9% change required for achieving the objective. We had insufficient data, however, on how much overall population-level energy intake and expenditure may change when interventions are combined.
These simulations assumed sustained changes in calorie intake and expenditure across entire cohorts. For comparison with population-level interventions, we also estimated what individual-level weight loss attempts would be needed to achieve the objective. Even if all overweight and obese US adults aged 20 years and older actively attempted weight loss 4 times each year through both calorie reduction and increased exercise, the national obesity prevalence would only decline to 33.8% (95% CI = 31.8%, 35.8%) because of the high current rates of relapse from weight loss. In further sensitivity analyses, simulating an increased mortality risk among the obese reduced prevalence by less than 0.6% among each cohort, but did not systematically change our forecasts or requirements for target achievement.
DISCUSSION
If current trends in calorie intake continue over the next several years, we expect the prevalence of obesity to decline among younger groups while rising among older adults. This has important implications for resource demand, allocation, and disability expenditures, especially among the large number of baby boomers who will likely account for much of the obesity-related morbidity and associated health care cost. This finding is analogous to the cohort effect in smoking in the 1980s and 1990s, which produced a generation of tobacco-related morbidity and mortality before subsequent declines.
The changes in calorie intake and expenditure required to meet the Healthy People 2020 targets, according to our model, may be difficult to achieve through population-level interventions or through individual-level weight-loss attempts. Our review of population interventions to reduce obesity revealed no single intervention with sufficient long-term data to suggest that 1 population intervention alone could achieve the target, and it is even less likely that individual weight-loss attempts will achieve the objective. This suggests the need for more long-term population intervention trials that combine interventions, especially targeting older groups, among whom few interventions have been studied for long-term efficacy. The current high levels of relapse following weight loss also reveal that changes must be sustained to effect population-level improvements. This finding highlights the need to focus on weight-loss strategies that provide maintenance of consumption and activity change.25
We observed that because of preexisting differences in calorie intake and expenditure, the same percentage improvement in intake and expenditure would likely exacerbate existing disparities in obesity prevalence among age, racial/ethnic, and income groups. Older, minority, and low-income populations would be expected to lag behind younger, White, higher-income groups in reducing obesity prevalence, with age-related disparities declining as less obese younger groups age. It will likely take longer than a decade for disparities in obesity prevalence between non-Hispanic Whites and non-Hispanic Blacks to be eliminated, because of real constraints in metabolism and current disparities and trends in BMI, calorie intake, and physical activity.
Our data offer significant new contributions to the literature on obesity prevalence. Previous obesity projections predicted continuing increases in obesity prevalence over time, achieving steady-state high levels of obesity (> 33% of adults) before any potential declines.2,4 Our model results agree with those findings, but also incorporate new trends in calorie intake that suggest obesity prevalence may decrease among younger age groups. Investigating how these improvements were achieved may provide further insights into sustaining obesity decline in future generations. Also, because we explicitly incorporated calorie intake and expenditure into our population-level model, it did not simply project BMI trends into the future, but also accounted for how changes in food consumption and physical activity might manifest in population-level changes, as recommended in recent literature.5,6,26,27 This provided an estimate of how differences in behavior among US subpopulations relate to population-level disparities, consistent with findings in previous research of significant differences in behavior among demographic groups.28–31
The secular trends in intake and expenditure were also similar to previous assessments,32–34 but their robustness over future survey waves should be monitored to assess the persistence of reported trends in behavior. Our results further suggest that obesity rates will continue to decline among some cohorts, extending the prevalence changes observed in recent epidemiological studies,35 and that the modest effects of currently available population interventions may prevent any one such intervention from achieving the overall Health People 2020 target.17–20
Limitations
As with any mathematical model, ours had several important assumptions and limitations. We used data from NHANES, which are subject to the limitations of survey studies, including recall biases, acceptability biases, and underreporting.36 NHANES also does not have a sufficient sample size to estimate calorie intake or expenditure among many minority groups, such as Asian Americans, and excludes institutionalized members of the US population. Second, the model uses only moderate- and high-intensity physical activity as a metric of energy expenditure. Studies to date have not directly compared weight-loss models with alternative metrics of physical activity, but this metric does not fully capture all of the metabolic effects of different physical activities. The model also does not automatically simulate any compensatory effects associated with changes in behavior, such as increased energy intake at the start of an exercise program, for which insufficient information is available for modeling to date.5
Third, like all available body weight models, our model assumed that “a calorie is a calorie,” because further information was not yet available regarding how to best model the differential impact of different types of calories on obesity-related comorbidities.37 Finally, it is impossible to predict future trends in calorie intake or expenditure; hence we relied on existing trends and produced sensitivity analyses to understand how changes in those trends may alter future obesity trajectories.
Conclusions
The Healthy People 2020 obesity reduction goal is potentially attainable if relatively modest but sustained calorie reduction and increased physical activity can be achieved in the United States. However, cohort effects may increasingly lead to an older-adult obese population. Disparities in obesity prevalence are also likely to differentially burden ethnic minority populations and the poor if current trends in calorie consumption and physical activity continue.
Acknowledgments
The study was funded by the Department of Medicine, Stanford University.
Human Participant Protection
No protocol approval was needed because only publicly available data were used.
References
- 1.Healthy People 2020: Improving the Health of Americans. Washington, DC: Department of Health and Human Services; 2010. [Google Scholar]
- 2.Bibbins-Domingo K, Coxson P, Pletcher MJ, Lightwood J, Goldman L. Adolescent overweight and future adult coronary heart disease. N Engl J Med. 2007;357(23):2371–2379. doi: 10.1056/NEJMsa073166. [DOI] [PubMed] [Google Scholar]
- 3.Lightwood J, Bibbins-Domingo K, Coxson P, Wang YC, Williams L, Goldman L. Forecasting the future economic burden of current adolescent overweight: an estimate of the coronary heart disease policy model. Am J Public Health. 2009;99(12):2230–2237. doi: 10.2105/AJPH.2008.152595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basu A. Forecasting distribution of body mass index in the United States: is there more room for growth? Med Decis Making. 2010;30(3):E1–E11. doi: 10.1177/0272989X09351749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall KD, Sacks G, Chandramohan D et al. Quantification of the effect of energy imbalance on bodyweight. Lancet. 2011;378(9793):826–837. doi: 10.1016/S0140-6736(11)60812-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levy DT, Mabry PL, Wang YC et al. Simulation models of obesity: a review of the literature and implications for research and policy. Obes Rev. 2011;12(5):378–394. doi: 10.1111/j.1467-789X.2010.00804.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. US Centers for Disease Control and Prevention. NHANES—National Health and Nutrition Examination Survey. 2012. Available at: http://www.cdc.gov/nchs/nhanes.htm. Accessed December 29, 2012.
- 8.Hall KD, Jordan PN. Modeling weight-loss maintenance to help prevent body weight regain. Am J Clin Nutr. 2008;88(6):1495–1503. doi: 10.3945/ajcn.2008.26333. [DOI] [PubMed] [Google Scholar]
- 9.Hall KD, Butte NF, Swinburn BA, Chow CC. Dynamics of childhood growth and obesity: development and validation of a quantitative mathematical model. Lancet Diabetes Endocrinol. 2013;1(2):97–105. doi: 10.1016/s2213-8587(13)70051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rahmandad H, Sterman JD. Reporting guidelines for simulation-based research in social sciences. Syst Dyn Rev. 2012;28(4):396–411. [Google Scholar]
- 11.2010 to 2050 Supplemental Population Projections Based on Census 2000. Washington, DC: US Census Bureau; 2009. [Google Scholar]
- 12.The National Health and Nutrition Examination Survey (NHANES) Analytic and Reporting Guidelines. Hyattsville, MD: National Center for Health Statistics; 2005. [Google Scholar]
- 13.Moshfegh AJ, Rhodes DG, Baer DJ et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88(2):324–332. doi: 10.1093/ajcn/88.2.324. [DOI] [PubMed] [Google Scholar]
- 14.Simulating Dependent Random Variables Using Copulas. Natick, MA: MathWorks; 2013. [Google Scholar]
- 15.Extended International (IOTF) Body Mass Index Cut-Offs for Thinness, Overweight and Obesity in Children. London, UK: International Association for the Study of Obesity; 2012. [DOI] [PubMed] [Google Scholar]
- 16.Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. Age Standardization of Rates: A New WHO Standard. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 17.Tuah NA, Amiel C, Qureshi S, Car J, Kaur B, Majeed A. Transtheoretical model for dietary and physical exercise modification in weight loss management for overweight and obese adults. Cochrane Database Syst Rev. (10):CD008066. doi: 10.1002/14651858.CD008066.pub2. 2011. [DOI] [PubMed] [Google Scholar]
- 18.Shaw K, O’Rourke P, Del Mar C, Kenardy J. Psychological interventions for overweight or obesity. Cochrane Database Syst Rev. (2):CD003818. doi: 10.1002/14651858.CD003818.pub2. 2005. [DOI] [PubMed] [Google Scholar]
- 19.Waters E, de Silva Sanigorski A, Hall BJ et al. Interventions for preventing obesity in children (review) Cochrane Collaboration. (12):1–212. doi: 10.1002/14651858.CD001871.pub3. 2011. [DOI] [PubMed] [Google Scholar]
- 20.Thomas DE, Elliott EJ, Baur L. Low glycaemic index or low glycaemic load diets for overweight and obesity. Cochrane Database Syst Rev. (3):CD005105. doi: 10.1002/14651858.CD005105.pub2. 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Glickman D. Institute of Medicine, Committee on Accelerating Progress in Obesity Prevention. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, DC: National Academies Press; 2012. [PubMed] [Google Scholar]
- 22.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309(1):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prospective Studies Collaboration. Whitlock G, Lewington S et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anderson JW, Konz EC, Frederich RC, Wood CL. Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr. 2001;74(5):579–584. doi: 10.1093/ajcn/74.5.579. [DOI] [PubMed] [Google Scholar]
- 25.Kiernan M, Brown SD, Schoffman DE et al. Promoting healthy weight with “stability skills first”: a randomized trial. J Consult Clin Psychol. 2012;81(2):336–346. doi: 10.1037/a0030544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Swinburn BA, Sacks G, Hall KD et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378(9793):804–814. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- 27.Chow CC, Hall KD. The dynamics of human body weight change. PLOS Comput Biol. 2008;4(3):e1000045. doi: 10.1371/journal.pcbi.1000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29(1):6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 29.Crespo CJ, Smit E, Andersen RE, Carter-Pokras O, Ainsworth BE. Race/ethnicity, social class and their relation to physical inactivity during leisure time: results from the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Prev Med. 2000;18(1):46–53. doi: 10.1016/s0749-3797(99)00105-1. [DOI] [PubMed] [Google Scholar]
- 30.Gordon-Larsen P, Nelson MC, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117(2):417–424. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 31.Miech RA, Kumanyika SK, Stettler N, Link BG, Phelan JC, Chang VW. Trends in the association of poverty with overweight among US adolescents, 1971–2004. JAMA. 2006;295(20):2385–2393. doi: 10.1001/jama.295.20.2385. [DOI] [PubMed] [Google Scholar]
- 32.Norris J, Harnack L, Carmichael S, Pouane T, Wakimoto P, Block G. US trends in nutrient intake: the 1987 and 1992 National Health Interview Surveys. Am J Public Health. 1997;87(5):740–746. doi: 10.2105/ajph.87.5.740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borrud L, Enns CW, Mickle S. What we eat in America: USDA surveys food consumption changes. FoodReview. 1996. Available at: http://agris.fao.org/agris-search/search/display.do?f=2012/OV/OV201207846007846.xml;US19970112867. Accessed July 31, 2013.
- 34.Brownson RC, Boehmer TK, Luke DA. Declining rates of physical activity in the United States: what are the contributors? Annu Rev Public Health. 2005;26:421–443. doi: 10.1146/annurev.publhealth.26.021304.144437. [DOI] [PubMed] [Google Scholar]
- 35.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among us adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 36.Freedman LS, Schatzkin A, Midthune D, Kipnis V. Dealing with dietary measurement error in nutritional cohort studies. J Natl Cancer Inst. 2011;103(14):1086–1092. doi: 10.1093/jnci/djr189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Basu S, Yoffe P, Hills N, Lustig RH. The relationship of sugar to population-level diabetes prevalence: an econometric analysis of repeated cross-sectional data. PLoS ONE. 2013;8(2):e57873. doi: 10.1371/journal.pone.0057873. [DOI] [PMC free article] [PubMed] [Google Scholar]