Abstract
Objectives. Most state Medicaid programs reimburse nondental primary care providers (PCPs) for providing preventive oral health services to young children. We examined the association between who (PCP, dentist, or both) provides these services to Medicaid enrollees before age 3 years and oral health at age 5 years.
Methods. We linked North Carolina Medicaid claims (1999–2006) to oral health surveillance data (2005–2006). Regression models estimated oral health status (number of decayed, missing, and filled primary teeth) and untreated disease (proportion of untreated decayed teeth), with adjustment for relevant characteristics and by using inverse-probability-of-treatment weights to address confounding.
Results. We analyzed data for 5235 children with 2 or more oral health visits from a PCP, dentist, or both. Children with multiple PCP or dentist visits had a similar number of overall mean decayed, missing, and filled primary teeth in kindergarten, whereas children with only PCP visits had a higher proportion of untreated decayed teeth.
Conclusions. The setting and provider type did not influence the effectiveness of preventive oral health services on children’s overall oral health. However, children having only PCP visits may encounter barriers to obtaining dental treatment.
Guidelines from the American Dental Association, American Academy of Pediatric Dentistry, and the American Academy of Pediatrics recommend that children visit a dentist by their first birthday.1–3 Early dentist visits provide an opportunity to establish and promote good oral health practices, evaluate caries risk factors, and deliver caries prevention strategies, such as application of topical fluoride.2 Despite recommendations, few Medicaid-enrolled children visit dentists. During 2007, only 4 states (Iowa, North Carolina, Texas, and Washington) reported that 20% or more of its Medicaid-enrolled children younger than 3 years visited dentists.4
Recognizing that primary care providers (PCPs) see young children frequently and can provide many of these services, most state Medicaid programs now reimburse PCPs for delivery of preventive oral health services in medical offices.5 Since 2000, a North Carolina Medicaid program, known as Into the Mouths of Babes (IMB), has trained PCPs (e.g., physicians, physician assistants, nurse practitioners) to provide preventive oral health services to children younger than 3 years. Training is provided at the request of PCPs working in private offices and public health clinics. As described on the program’s Web site,6 IMB visits include an oral evaluation and risk assessment, anticipatory guidance for parents, and application of fluoride varnish to prevent dental caries—services similar to those provided during preventive visits in a dental office. Children suspected to have caries or to be at elevated risk are referred to dentists when they are available in the community. This program and similar programs in other states have helped increase access to oral health services and reduce treatments for young children enrolled in Medicaid.7–9 By 2006, nearly 30% of well-child medical visits for children younger than 3 years included IMB services.9 Overall, the percentage of Medicaid children younger than 5 years obtaining oral health services in North Carolina increased from 17% in 2002 to 59% in 2011.10
Although the benefits of IMB services are well-documented,8,9 less is known about the oral health status of these children after their third birthday when they are no longer eligible to receive preventive oral health services from PCPs. The IMB services are intended to coincide with recommended well-child medical visits at 6, 9, 12, 15, 18, and 24 months of age and end at an age when well-child visits in the medical office become less frequent and more dentists are willing to accept them as patients.11,12 Previous research indicates that children who had 4 or more IMB visits (compared with zero IMB visits) between 2000 and 2006 received fewer caries-related treatments after their IMB eligibility expired (ages 40 to 72 months).8 Although this finding suggests that IMB visits may be associated with better oral health, the study did not control for preventive services received from dentists or examine the program’s effect on clinical disease, which provides a better measure of overall oral health and access to dental care. Some barriers to dental care for children may ease as they age because dentists are more willing to care for older children12; however, workforce shortages and dentists’ low rate of participation in Medicaid remain as barriers to dental care as children age.13,14
Widespread support exists for the integration of dentistry and medicine to promote young children’s oral health,15–18 yet, to date, no study has directly compared the oral health outcomes of children receiving preventive oral health services from PCPs or dentists (with or without PCP visits). This comparison is important because more than 40 state Medicaid programs reimburse PCPs for application of fluoride varnish.5 By using a unique combination of oral health surveillance data and Medicaid claims to help overcome limitations of dental claims data, we aimed to determine whether the provider of preventive oral health services is associated with (1) the number of decayed, missing, and filled primary teeth (dmft) per child, a measure of lifetime caries experience at 5 years of age; and (2) the proportion of dmft that is untreated, a measure of the extent to which a child’s treatment needs are being met.
Because children who receive preventive oral health services before their third birthday during IMB or dentist visits are expected to benefit from early screenings, anticipatory guidance, and applications of fluoride varnish,2,19 we hypothesized that these children will have a similar number of dmft in kindergarten. Furthermore, because IMB providers are trained to refer children suspected to have, or be at elevated risk for, caries to dentists when they are available in the community, we hypothesized that the IMB program will improve access to dental treatment and thus children with IMB or dentist visits will have a similar proportion of dmft that is untreated in kindergarten.
METHODS
In this retrospective cohort study, we used North Carolina oral health surveillance data and Medicaid files for children enrolled in kindergarten during the 2005–2006 school year. Public health dental hygienists conduct annual standardized screenings, providing information about the overall dental caries experience and the amount of dental treatment received among children in kindergarten.20,21 Surveillance data have demonstrated good reliability when compared with an experienced dentist performing a standard dental examination.22 Data were available for 92 127 kindergarten children, which includes 82% of the state’s public school kindergarten enrollment from 98 of 100 North Carolina counties.21 Medicaid enrollment and claims files from the NC Division of Medical Assistance provided information about demographic characteristics, length of Medicaid enrollment, and whether the child had a preventive oral health visit from a PCP or dentist.
The surveillance data and Medicaid files were previously linked with Link King software version 6.4.9 (Camelot Consulting), which utilizes probabilistic and deterministic methods to link individual records based on the child’s name, date of birth, gender, race, and county of residence.23,24 Of the children included in the kindergarten surveillance data, 34 743 were successfully matched to Medicaid claims of children enrolled before age 1 and still enrolled after their first birthday. We excluded children from the analysis if they had a nonunique identification number (n = 442), less than 12 months of continuous enrollment in NC Medicaid before age 3 years (n = 3095), IMB claims posteligibility (n = 82), or missing oral health surveillance measures (n = 1951), resulting in a sample size of 29 173 children, which is comparable to the proportion of children enrolled in NC Medicaid.25 Because the objective of this study was to compare the effectiveness of different providers of preventive oral health services, we excluded children who did not receive preventive services before aged 3 years, resulting in a sample size of 10 893 children.
Ideally we would compare the effectiveness of children receiving more than 3 preventive oral health visits before their thirs birthday, which has been shown to reduce caries-related treatments in previous studies of the IMB program.8,26 However, only 1% of our sample (n = 132) had more than 3 dentist visits before age 3 years. Therefore, we constructed a sample including children with 2 or more IMB visits, 2 or more dentist visits, or both dentist and IMB visits before their third birthday (n = 5235). Within each category, children in our sample were most likely to have 2 visits than to have 3 or 4 or more visits.
Measures
We examined 2 primary outcomes. First, we examined caries experience by using a composite index of the number of dmft, derived from a visual inspection of the primary dentition of kindergarten students. We excluded primary incisors from the count of missing teeth because they could be missing for noncarious reasons, mostly natural exfoliation. This outcome measure provides information on the child’s lifetime caries experience in all primary teeth with the exception of missing incisors, thus providing a measure of a child’s overall oral health status.27
The second outcome variable provided a measure of the proportion of dmft that are untreated (decayed teeth, dt) at the time of the clinical assessment. We constructed a binomial count of the number of dt out of the total dmft score for all children with dmft greater than 0. Although the prevention of dental caries is ideal, filled teeth are regarded as healthier than dt.27 This variable reflects a child’s use of dental treatment by providing a measure of the extent to which a child’s treatment needs related to dental caries are being met.
We operationalized the main explanatory variable, provider of preventive oral health services before age 3 years, as a 3-category variable indicating IMB visits, dentist visits only (reference group), or both IMB and dentist visits. We defined a visit in a dental office with preventive services, reimbursed by Medicaid up to twice annually after any tooth erupts, as having paid claims for a comprehensive or periodic evaluation (Current Dental Terminology codes28 D0150, D0120) with fluoride (D1203, D1201). Some dental visits included caries-related treatment because the purpose of the visit could not be determined. We identified IMB visits with any of the following paid claims filed by physicians for preventive oral health services (D0120, D0150, D1201, D1203, D1330, W8002, and W8003). Although PCPs are encouraged to provide IMB services to all eligible children, delivery is at the discretion of the provider. Children may receive IMB services during an already scheduled well- or sick-child visit if they visit a trained provider and the provider chooses to deliver IMB services during the visit. The time period of this study coincides with the beginning of IMB implementation and a time that access to Medicaid dental providers was limited; thus, many children did not visit participating providers.
We also included child- and county-level characteristics that may affect dental caries status, measured at or before age 3 years. The child-level covariates in the models included sex, race (White, Black, other), Hispanic ethnicity, total number of months enrolled in Medicaid, number of well-child visits, indicators of special health care needs, receipt of caries-related treatment, and whether any preventive oral health services were received in a federally qualified health center, health department, or rural health clinic. At the county level, covariates included proportion of population with access to fluoridated public drinking water,29 indicators of rural or urban status,30 and, per 10 000 people, the number of dentists, pediatricians and family practice physicians,31 and Medicaid-eligible children younger than 18 years.32
Propensity Score Estimation
Because of the lack of use of diagnostic terms or codes in dentistry,33 it is unknown if dentist visits are because of existing disease or demand for preventive services. To address confounding attributable to observed systematic differences between children, we utilized propensity scores with inverse-probability-of-treatment weights (IPTWs).34,35 With control for the aforementioned covariates, including squared terms of continuous variables (excluding the variable indicating receipt of treatment before age 3 years because of its relationship with the exposure variable), we estimated propensity scores by using logistic regression to predict the likelihood of having a dentist visit with preventive services before age 3 years. We calculated standardized weights for each child, an approach that assigns greater weight to children who received a dentist visit before age 3 years, but have characteristics more similar to children who did not have a dentist visit before age 3 years and vice versa.35 Adjustment of IPTWs provides greater precision than propensity score matching and estimates the average treatment effect.36 Following IPTW adjustment, the distribution of propensity scores was more similar among children with dentist visits and children with only IMB visits (Figure A, available as a supplement to this article at http://www.ajph.org) and covariate balance was improved as evidenced by absolute standardized differences less than 10% (Figure B, available as a supplement to this article at http://www.ajph.org).37
Analytical Approach
We used a 1-way rank analysis of variance (Kruskal–Wallis test) to test for differences in dmft and dt/dmft among children with IMB visits, dentist visits, or both. Combining the 2 parts of a zero-inflated negative binomial (ZINB) regression model, we estimated the adjusted overall mean number of dmft for children in kindergarten by provider type.38 For the logit part of the ZINB model, odds ratios (ORs) indicate the odds of having excess zero dmft, a nonrandom zero in the sense of being considered not at risk for caries. The negative binomial part describes the mean number of dmft among children considered to be at risk for caries, with exponentiated parameter estimates giving incident rate ratios. To estimate the proportion of dt among dmft for children with any caries, we used a binomial logistic regression (where dt/dmft is the number of “events” divided by the number of “trials”).39
The regression models controlled for the aforementioned covariates and used Huber–White empirical standard errors to adjust for intragroup correlation attributable to clustering of children within counties. We estimated Wald test statistics to determine the joint significance of the key explanatory variables indicating the provider of oral health services. We predicted covariate-adjusted overall mean outcomes for an average child utilizing each provider (dentist only, IMB only, or both) by using the full sample with 95% confidence intervals (CIs) generated with 500 bootstrap replications. In addition, we examined differences in adjusted mean outcomes by subtracting the predicted outcomes for children with IMB visits or both dentist and IMB visits from the predicted outcomes for children with only dentist visits. We assessed differences in predicted outcomes with the Wald test and 95% CIs. We performed all tests in Stata/IC 12 (StataCorp, College Station, TX) using a .05 significance level.
RESULTS
Our sample included 5235 children who received 2 or more preventive oral health visits from a PCP, dentist, or both before their third birthday (Table 1). Twenty-five percent of children in this sample received preventive oral health services during only dentist visits (n = 480) or both dentist and IMB visits (n = 848). Most children (75%) received preventive oral health services during only IMB visits (n = 3907). Among these children, about 13% (n = 503) received the recommended 4 or more IMB visits before their third birthday.
TABLE 1—
Baseline Characteristics of North Carolina Medicaid Enrollees in Kindergarten During 2005–2006
| Variable Descriptiona | Full Sample (n = 5235), % or Mean (SD) | Children With Both Dentist and IMB Visits (n = 848), % or Mean (SD) | Children With ≥ 2 Dentist Visits Only (n = 480), % or Mean (SD) | Children With ≥ 2 IMB Visits Only (n = 3907), % or Mean (SD) |
| Clinical outcome variables | ||||
| dmft score* | 2.25 (3.28) | 3.00 (3.66) | 3.40 (3.98) | 1.95 (3.03) |
| Percentage with any dmft | 48.2 | 57.9 | 59.4 | 44.7 |
| Proportion of dt/dmft among children with dmft* | 0.39 (0.46) | 0.26 (0.40) | 0.15 (0.32) | 0.47 (0.47) |
| Child-level characteristics | ||||
| Number of months enrolled in Medicaid | 32.3 (2.7) | 32.7 (1.9) | 32.7 (1.6) | 32.2 (2.9) |
| Race | ||||
| White | 38.5 | 36.4 | 34.4 | 39.4 |
| Black | 41.8 | 42.7 | 42.1 | 41.6 |
| Hispanic ethnicity | 8.4 | 11.9 | 14.2 | 7 |
| Male | 51.8 | 53.4 | 50 | 51.6 |
| Special health care needs | 4.3 | 4.5 | 2.5 | 4.5 |
| Number of well-child visits before age 3 y | 4.9 (1.5) | 4.9 (1.6) | 4.0 (2.2) | 5.0 (1.4) |
| Any caries-related treatments before age 3 y | 10.4 | 31 | 39.2 | 2.4 |
| Any oral health services received in public clinic before age 3 y | 30 | 42.2 | 29.2 | 27.4 |
| County-level characteristics | ||||
| Medicaid eligible < 18 y per 10 000 people | 493.2 (142.8) | 452.8 (124.4) | 417.7 (123.5) | 511.2 (144.0) |
| Primary care providers per 10 000 people | 4.1 (1.7) | 4.1 (2.0) | 4.5 (1.8) | 4.0 (1.6) |
| Dentists per 10 000 people | 3.5 (1.5) | 3.8 (1.7) | 4.6 (1.7) | 3.3 (1.4) |
Note. dmft = number of decayed, missing, and filled primary teeth; dt = untreated decayed teeth; IMB = Into the Mouths of Babes program. Kruskal–Wallis tests examined differences in dmft and dt/dmft among children with IMB visits, dentist visits, or both.
Explanatory variables included in the regression models, but not presented in this table include the rural or urban status of the child’s county of residence and the percentage of the county population with fluoridated drinking water.
*P < .001.
The unadjusted mean number of dmft was lowest among children who received preventive oral health services during IMB visits (mean = 1.95; standard deviation [SD] = 3.03) and highest among children with dentist visits before their third birthday (dentist only = 3.40; SD = 3.98; both = 3.00; SD = 3.66). Overall, 48% of children had dmft by the time they entered kindergarten. Among these children, the mean proportion dt/dmft was lowest for children who received preventive oral health services during dentist visits (dentist only = 0.15; SD = 0.32; both = 0.26; SD = 0.40) and greatest for children with IMB visits (0.47; SD = 0.47). Kruskal–Wallis test results indicated dmft and dt/dmft differed significantly among children with IMB visits, dentist visits, or both.
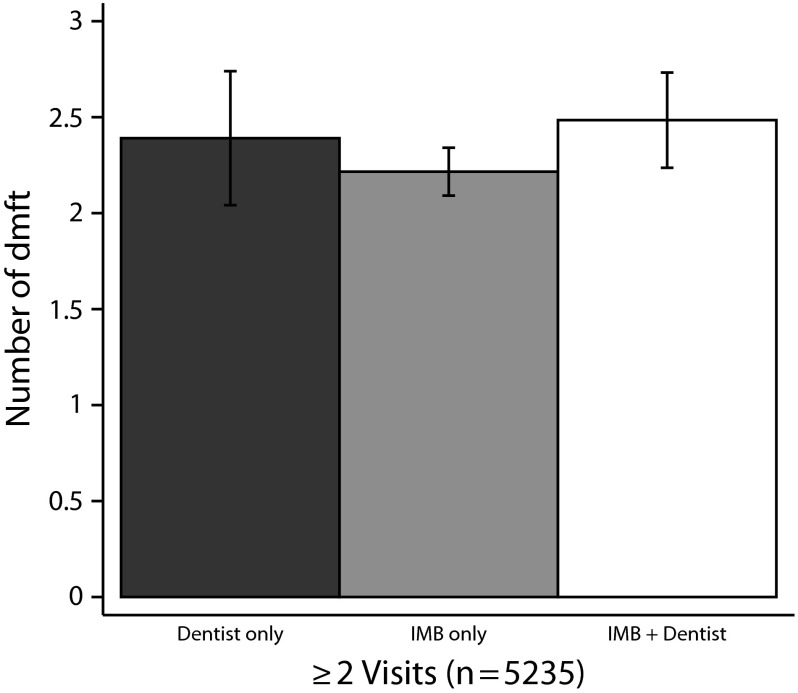
Results from both parts of the ZINB regression model used to predict mean dmft are provided in Table 2. The variables indicating only IMB visits, only dentist visits, and both IMB and dentist visits were jointly insignificant in the ZINB model (Wald test statistic = 8.28; df = 4). Children who received preventive oral health services during IMB or dentist visits had similar overall mean dmft (Figure 1). Mean predicted dmft ranged from 2.22 (95% CI = 2.05, 2.39) for children with only IMB visits to 2.48 (95% CI = 2.12, 2.83) for children with both IMB and dentist visits.
TABLE 2—
Results of Adjusted Regression Models Estimating Number of dmft and Proportion of dt/dmft Among North Carolina Medicaid Enrollees in Kindergarten During 2005–2006
| Results From ZINB |
|||
| Variable Description | Logit Estimating Odds of Excess Zero dmft (n = 5235), OR (95% CI) | NB Estimating Expected Number of dmft for Children at Risk for dmft (n = 2521), IRR (95% CI) | Results From Binomial Logistic Regression, Estimating Proportion of dt/dmft (n = 2521), OR (95% CI) |
| Provider of preventive oral health services before age 3 y | |||
| ≥ 2 dentist visits only (Ref) | 1.00 | 1.00 | 1.00 |
| ≥ 2 IMB visits only | 1.06 (0.78, 1.46) | 0.95 (0.82, 1.09) | 2.05** (1.28, 3.30) |
| Both dentist and IMB visits | 0.77 (0.52, 1.14) | 0.94 (0.82, 1.08) | 1.34 (0.82, 2.19) |
| No. of months enrolled in Medicaid | 0.99 (0.97, 1.01) | 1.01 (0.99, 1.02) | 1.00 (0.97, 1.03) |
| Race | |||
| White | 1.43*** (1.17, 1.74) | 0.97 (0.88, 1.06) | 1.11 (0.87, 1.42) |
| Black | 1.68*** (1.38, 2.06) | 0.90* (0.82, 0.99) | 1.19 (0.95, 1.49) |
| Other (Ref) | 1.00 | 1.00 | 1.00 |
| Male | 0.84* (0.73, 0.96) | 1.05* (1.00, 1.09) | 1.05 (0.95, 1.17) |
| Indicator of Hispanic ethnicity | 1.08 (0.80, 1.45) | 1.13* (1.01, 1.26) | 0.74 (0.55, 1.01) |
| Indicator that child has special health care needs | 1.26 (0.86, 1.82) | 0.92 (0.77, 1.09) | 1.26 (0.91, 1.74) |
| Number of well-child visits before age 3 y | 1.11*** (1.05, 1.18) | 0.98 (0.95, 1.01) | 0.96 (0.89, 1.03) |
| Indicator of caries-related treatments before age 3 y | 0.12*** (0.08, 0.18) | 1.66*** (1.51, 1.82) | 0.31*** (0.24, 0.41) |
| Oral health services before age 3 y received in public clinic | 1.02 (0.87, 1.19) | 0.94 (0.86, 1.02) | 1.11 (0.89, 1.38) |
| No. Medicaid eligible < 18 y per 10 000 people | 0.999* (0.998, 0.999) | 0.9997 (0.999, 1.00) | 1.001* (1.000, 1.002) |
| No. primary care providers per 10 000 people | 0.96 (0.90, 1.02) | 1.03* (1.01, 1.06) | 0.92* (0.85, 0.99) |
| No. dentists per 10 000 people | 1.11** (1.03, 1.20) | 0.94*** (0.90, 0.97) | 1.10* (1.01, 1.21) |
| Constant term | 0.89 (0.35, 2.27) | 4.27*** (2.45, 7.44) | 0.05*** (0.02, 0.17) |
Note. CI = confidence interval; dmft = decayed, missing, or filled primary teeth; dt = untreated decayed teeth; IMB = Into the Mouths of Babes program; IRR = incidence rate ratios; OR = odds ratio; ZINB = zero-inflated negative binomial. Models also controlled for the rural or urban status of the child’s county of residence and the percentage of the county population with fluoridated drinking water.
*P < .05; **P < .01; ***P < .001.
FIGURE 1—
Adjusted overall mean number of decayed, missing, and filled primary teeth (dmft) per child: North Carolina Medicaid enrollees in kindergarten during 2005–2006.
Note. IMB = Into the Mouths of Babes program. The overall mean (ν) is given by combining the 2 parts of the zero-inflated negative binomial model as ν = (1 - ψ) μ where ψ is the probability of an excess zero dmft and μ is the mean number of dmft given by the negative binomial part of the model that describes the (unobserved) latent class of children that are at risk for dmft.
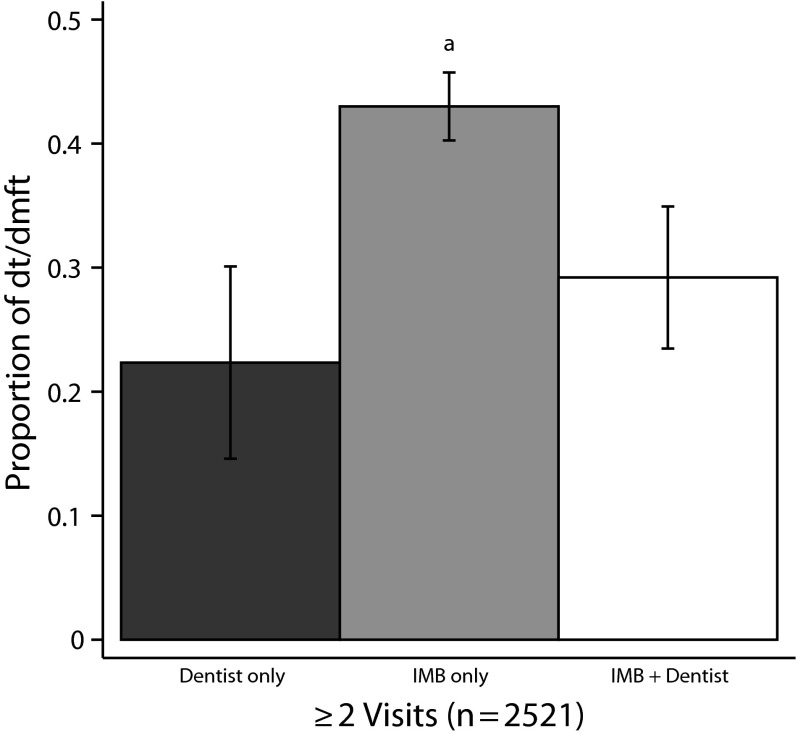
To examine a child’s receipt of treatment of dental caries, we estimated the adjusted proportion of a child’s dt/dmft for children with any dmft (last column of Table 2). The 2 variables indicating the provider of oral health services were jointly significant (Wald test statistic = 11.97; df = 2). As illustrated in Figure 2, the estimated proportion of dt/dmft was significantly higher among children with 2 or more IMB visits (0.43; 95% CI = 0.39, 0.48) than children with 2 or more dentist visits (0.22; 95% CI = 0.13, 0.38).
FIGURE 2—
Adjusted mean proportion of untreated decayed teeth (dt) per child among children with decayed, missing, and filled primary teeth (dmft): North Carolina Medicaid enrollees in kindergarten during 2005–2006.
Note. IMB = Into the Mouths of Babes program.
aIndicates significantly greater mean value than visits to dentists only (P < .001) and both IMB and dentists (P < .01).
DISCUSSION
We sought to compare the effectiveness of dentists, the traditional providers of preventive oral health services, with nondental PCPs, a new model in many states for providing these same services to children insured by Medicaid. We did so by examining the oral health status of kindergarten students who received these services before they were aged 3 years. First, we found that children with multiple IMB or dentist visits before they were aged 3 years tended to have a similar number of dmft in kindergarten. This finding suggests that the setting and type of provider do not influence the effectiveness of preventive oral health services, which is encouraging because more than 130 000 IMB visits were reimbursed in North Carolina in 2012.40 Children from low-income families are more likely to experience dental caries and less likely to visit a dentist than children from higher-income families.41 Thus Medicaid programs that reimburse preventive oral health services provided in medical offices can help to increase access for children living in poverty and help reduce disparities. Our results suggest that PCPs can play a key role in meeting the Healthy People 2020 oral health objective to increase the number of low-income children receiving preventive dental services.42
We also examined the proportion of dt/dmft, a measure of the extent to which a child’s treatment needs are being met. Although children with multiple IMB and dentist visits experienced a similar amount of dmft by the time they were enrolled in kindergarten, children who had only IMB visits before their third birthday had a higher proportion of dt/dmft, which was contrary to our hypothesis. Thus, the treatment needs of children with only IMB visits are not being fully met; nor are they met to the same level as those who get preventive services in dental offices at a young age. However, this finding could be because many children in this study did not receive the full complement of 4 or more IMB visits. In addition, barriers to dentist visits for Medicaid-enrolled children, which can include parental knowledge and beliefs about oral health and dental workforce shortages,13,43–45 may affect untreated decay. Children who received preventive oral health services from only PCPs lived in counties with fewer dentists per capita on average. A previous study reported that IMB services were more likely to be provided in rural counties where dental workforce shortages are most pronounced.9
Initiatives like the IMB program enable PCPs to deliver preventive oral health services to children at an age when they frequently visit medical offices and find it most difficult to access dentists. However, services provided in medical offices are not intended to replace regular dental visits, where potential problems can be detected early, treated, and monitored. Treatment is particularly important as untreated dental caries has been found to be associated with missed days of school, pain, and decreased quality of life.46–48 The American Academy of Pediatric Dentistry recommends that, by their first birthday, children establish a dental home that provides “comprehensive, continuously-accessible, family-centered, coordinated, compassionate, and culturally-effective” oral health care.49
The transition from receiving care in a medical office to a dental office may affect children’s continuity of oral health services because barriers to dental care are common in many communities. Although referrals by PCPs increase young children’s likelihood of having a dental visit,50,51 an early study of the IMB program found that few children obtaining IMB services receive referrals.52 Among parents receiving referrals, only 41% reported receiving help scheduling a dental appointment.53 States in the early stages of implementing similar programs need to consider children’s transition from receiving care in medical offices to dental offices and be proactive in finding dental homes for Medicaid-enrolled children. To improve care coordination between PCPs and dentists, risk assessment and referral tools have been developed to identify children at greatest risk of developing caries and prioritize referrals on the basis of this risk.3,51,54 A study examining a risk assessment tool used by IMB providers reported that caries presence was the strongest predictor of dental referral.51 Preliminary research suggests that quality improvement activities utilizing risk assessment tools can increase referrals.55
Limitations
This study has several limitations. Although we used IPTWs to address provider selection on the basis of observed characteristics, unobserved factors could still bias our estimates because of reverse causality. Lacking dental diagnosis codes, we are unable to determine if these early dentist visits were because of existing disease or demand for preventive services. Having additional information about children and families, including information on brushing practices, dietary habits, and parent knowledge and opinions about oral health would help us to better understand oral health outcomes.
As previously mentioned, we would ideally examine children receiving 3 or more preventive oral health visits before their third birthday, which has been shown to reduce caries-related treatments, and thus may lead to a further reduction in dmft.8,26 In addition, although more than 40 state Medicaid programs reimburse PCPs for providing fluoride varnish, generalizability of our study findings beyond North Carolina may be limited.5 Moreover, our study of Medicaid beneficiaries may have limited generalizability to privately insured and uninsured populations.
Conclusions
We compared the oral health outcomes of children receiving preventive oral health services from PCPs, dentists, or both. Regardless of the provider type, children who received multiple preventive oral health visits before their third birthday had a similar number of dmft in kindergarten, leading us to conclude that PCPs and dentists are equally effective providers of preventive oral health services. We also found that children who had only IMB visits had a significantly greater proportion of dt/dmft, suggesting that more efforts are needed to improve referrals from PCPs to dentists to help children obtain needed dental treatment. Further research is needed to examine best practices to increase utilization of preventive oral health services and to link medical and dental homes through effective referrals.
Acknowledgments
This study was supported by grants R01 DE013949 and R03 DE017350 from the National Institute of Dental and Craniofacial Research (NIDCR). A. Kranz was partially supported by a National Research Service Award Pre-Doctoral Traineeship from the Agency for Health Care Research and Quality sponsored by the Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, grant T32-HS000032. M. Weinberger was supported by a Health Services Research and Development Senior Career Scientist Award from the Department of Veterans Affairs.
Note. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIDCR or the National Institutes of Health.
Human Participant Protection
This study was approved by an institutional review board at the University of North Carolina at Chapel Hill. This research meets criteria for waiver of informed consent for research and waiver of Health Insurance Portability and Accountability Act authorization as this study is a secondary data analysis.
References
- 1. American Dental Association. Current policies. 2013. Available at: http://www.ada.org/sections/about/pdfs/doc_policies.pdf. Accessed November 18, 2013.
- 2. American Academy of Pediatric Dentistry. Guideline on periodicity of examination, preventive dental services, anticipatory guidance/counseling, and oral treatment for infants, children, and adolescents. 2009. Available at: http://www.aapd.org/media/Policies_Guidelines/G_Periodicity.pdf. Accessed August 1, 2013.
- 3.American Academy of Pediatrics, Section on Pediatric Dentistry and Oral Health. Oral health risk assessment timing and establishment of the dental home. Pediatrics. 2003;111(5):1113–1116. doi: 10.1542/peds.111.5.1113. [DOI] [PubMed] [Google Scholar]
- 4.Hakim RB, Babish JD, Davis AC. State of dental care among Medicaid-enrolled children in the United States. Pediatrics. 2012;130(1):5–14. doi: 10.1542/peds.2011-2800. [DOI] [PubMed] [Google Scholar]
- 5.Deinard A. State Medicaid payment for caries prevention services by non-dental professionals. 2013. Available at: http://www2.aap.org/oralhealth/docs/OHReimbursementChart.pdf. Accessed July 20, 2013.
- 6.North Carolina Oral Health Section. Into the Mouths of Babes: Medicaid oral evaluation for infants and children up to forty two months of age. 2009. Available at: http://www.ncdhhs.gov/dph/oralhealth/library/includes/IMBresources/2_Medicaid%20Oral%20evaluation-%20toolkit.pdf. Accessed June 14, 2011.
- 7.Pierce KM, Rozier RG, Vann WF., Jr Accuracy of pediatric primary care providers’ screening and referral for early childhood caries. Pediatrics. 2002;109(5):E82–E2. doi: 10.1542/peds.109.5.e82. [DOI] [PubMed] [Google Scholar]
- 8.Pahel BT, Rozier RG, Stearns SC, Quinonez RB. Effectiveness of preventive dental treatments by physicians for young Medicaid enrollees. Pediatrics. 2011;127(3):e682–e689. doi: 10.1542/peds.2010-1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rozier RG, Stearns SC, Pahel BT, Quinonez RB, Park J. How a North Carolina program boosted preventive oral health services for low-income children. Health Aff (Millwood) 2010;29(12):2278–2285. doi: 10.1377/hlthaff.2009.0768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.North Carolina Institute of Medicine. North Carolina child health report card. 2008. Available at: http://nciom.org/wp-content/uploads/2010/08/card2008.pdf. Accessed January 12, 2013.
- 11.Bright Futures and the American Academy of Pediatrics. Recommendations for preventive pediatric health care. 2008. Available at: http://www.aap.org/en-us/professional-resources/practice-support/Periodicity/Periodicity%20Schedule_FINAL.pdf. Accessed February 8, 2013.
- 12.Seale NS, Casamassimo PS. Access to dental care for children in the United States: a survey of general practitioners. J Am Dent Assoc. 2003;134(12):1630–1640. doi: 10.14219/jada.archive.2003.0110. [DOI] [PubMed] [Google Scholar]
- 13.Fraher E, McGee V, Hom J, Lyons J, Gaul K. We’re not keeping up with the Joneses: North Carolina has fewer dentists per capita than neighboring (and most other) states. N C Med J. 2012;73(2):111–114. [PubMed] [Google Scholar]
- 14.US Government Accountability Office. Efforts under way to improve children’s access to dental services, but sustained attention needed to address ongoing concerns. 2010. Available at: http://www.gao.gov/assets/320/312818.pdf. Accessed January 10, 2013.
- 15.Pew Center on the States. The cost of delay: state dental policies fail one in five children. 2010. Available at: http://www.pewtrusts.org/uploadedFiles/Cost_of_Delay_web.pdf. Accessed May 18, 2012.
- 16.American Academy of Pediatrics, Section on Pediatric Dentistry and Oral Health. Preventive oral health intervention for pediatricians. Pediatrics. 2008;122(6):1387–1394. doi: 10.1542/peds.2008-2577. [DOI] [PubMed] [Google Scholar]
- 17.Hanlon C. Reimbursing medical providers for preventive oral health services: state policy options. 2010. Available at: http://www.nashp.org/publication/reimbursing-medical-providers-preventive-oral-health-services-state-policy-options. Accessed May 18, 2012.
- 18.Institute of Medicine. Improving access to oral health care for vulnerable and underserved populations. 2011. Available at: http://books.nap.edu/openbook.php?record_id=13116. Accessed January 10, 2013.
- 19.American Dental Association, Council on Scientific Affairs. Professionally applied topical fluoride: evidence-based clinical recommendations. J Am Dent Assoc. 2006;137(8):1151–1159. doi: 10.14219/jada.archive.2006.0356. [DOI] [PubMed] [Google Scholar]
- 20.King RS, Rozier RG. School-based dental disease prevention and oral health education: programs of the North Carolina oral health section. N C Med J. 2008;69(6):490–494. [PubMed] [Google Scholar]
- 21. Division of Public Health, North Carolina Department of Health and Human Services. 2008–2009 annual report: North Carolina Oral Health Section. 2009. Available at: http://www.ncdhhs.gov/dph/oralhealth/library/includes/08-09%20OHS%20Annual%20Report.pdf. Accessed February 12, 2013.
- 22.King RS, Satterfield WC, Rozier RG. A statewide system for dental caries in kindergarten children. J Dent Res. 1998;77(A):224. [Google Scholar]
- 23.Beil H, Preisser JS, Rozier RG. Accuracy of record linkage software in merging dental administrative data sets. J Public Health Dent. 2013;73(2):89–93. doi: 10.1111/j.1752-7325.2012.00343.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beil H, Rozier RG, Preisser JS, Stearns SC, Lee JY. Effect of early dental office visits on dental caries experience. Am J Public Health. 2013 doi: 10.2105/AJPH.2013.301325. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. North Carolina Department of Health and Human Services, Division of Medical Assistance. Medicaid in North Carolina: annual report state fiscal year 2007. 2008. Available at: http://www.ncdhhs.gov/dma/2007report/2007report.pdf. Accessed August 1, 2013.
- 26.Stearns SC, Rozier RG, Kranz AM, Pahel BT, Quinonez RB. Cost-effectiveness of preventive oral health care in medical offices for young Medicaid enrollees. Arch Pediatr Adolesc Med. 2012;166(10):945–951. doi: 10.1001/archpediatrics.2012.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lewit EM, Kerrebrock N. Child indicators: dental health. Future Child. 1998;8(1):133–142. [PubMed] [Google Scholar]
- 28.Current Dental Terminology 2008–2009: The ADA Practical Guide to Dental Procedure Codes. Chicago, IL: American Dental Association; 2007. [Google Scholar]
- 29.North Carolina Oral Health Section. County-Level Water Fluoridation Data. Raleigh, NC: North Carolina Department of Health and Human Services; 2007. [Google Scholar]
- 30.Economic Research Service. Washington, DC: US Department of Agriculture; 2003. Rural–urban continuum codes. Available at: http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx#.U0VSx_ldWSo. Accessed June 29, 2011. [Google Scholar]
- 31.Cecil G. Sheps Center for Health Services Research. North Carolina health professionals data system. 2007. Available at: http://www.shepscenter.unc.edu/hp/profiles.htm. Accessed May 20, 2012.
- 32.North Carolina Division of Medical Assistance. Authorized Medicaid and health choice for children eligibles reports. 2012. Available from: http://www.ncdhhs.gov/dma/elig/index.htm. Accessed October 15, 2011.
- 33.Kalenderian E, Ramoni RL, White JM et al. The development of a dental diagnostic terminology. J Dent Educ. 2011;75(1):68–76. [PMC free article] [PubMed] [Google Scholar]
- 34.Rosenbaum PR, Rubin DB. The central role of the propensity score in observation studies for causal effects. Biometrika. 1983;70(1):41–55. [Google Scholar]
- 35.Hirano K, Imbens GW. Estimation of causal effects using propensity score weighting: an application to data on right heart catheterization. Health Serv Outcomes Res Methodol. 2001;2:259–278. [Google Scholar]
- 36.Curtis LH, Hammill BG, Eisenstein EL, Kramer JM, Anstrom KJ. Using inverse probability-weighted estimators in comparative effectiveness analyses with observational databases. Med Care. 2007;45(10 suppl 2):S103–S107. doi: 10.1097/MLR.0b013e31806518ac. [DOI] [PubMed] [Google Scholar]
- 37.Austin PC. A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat Med. 2008;27(12):2037–2049. doi: 10.1002/sim.3150. [DOI] [PubMed] [Google Scholar]
- 38.Preisser JS, Stamm JW, Long DL, Kincade ME. Review and recommendations for zero-inflated count regression modeling of dental caries indices in epidemiological studies. Caries Res. 2012;46(4):413–423. doi: 10.1159/000338992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hilbe J. Logistic Regression Models. Boca Raton, FL: Chapman and Hall/CRC; 2009. [Google Scholar]
- 40.Rozier RG. Oral health in North Carolina: innovations, opportunities, and challenges. N C Med J. 2012;73(2):100–107. [PubMed] [Google Scholar]
- 41.Edelstein BL, Chinn CH. Update on disparities in oral health and access to dental care for America’s children. Acad Pediatr. 2009;9(6):415–419. doi: 10.1016/j.acap.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 42. US Department of Health and Human Services. Healthy People 2020: oral health leading health indicator. 2013. Available at: http://healthypeople.gov/2020/LHI/oralHealth.aspx. Accessed November 15, 2013.
- 43.Sohn W, Ismail A, Amaya A, Lepkowski J. Determinants of dental care visits among low-income African-American children. J Am Dent Assoc. 2007;138(3):309–318. doi: 10.14219/jada.archive.2007.0163. [DOI] [PubMed] [Google Scholar]
- 44.Isong IA, Zuckerman KE, Rao SR, Kuhlthau KA, Winickoff JP, Perrin JM. Association between parents’ and children’s use of oral health services. Pediatrics. 2010;125(3):502–508. doi: 10.1542/peds.2009-1417. [DOI] [PubMed] [Google Scholar]
- 45.Milgrom P, Mancl L, King B, Weinstein P, Wells N, Jeffcott E. An explanatory model of the dental care utilization of low-income children. Med Care. 1998;36(4):554–566. doi: 10.1097/00005650-199804000-00011. [DOI] [PubMed] [Google Scholar]
- 46.Jackson SL, Vann WF, Jr, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children’s school attendance and performance. Am J Public Health. 2011;101(10):1900–1906. doi: 10.2105/AJPH.2010.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Low W, Tan S, Schwartz S. The effect of severe caries on the quality of life in young children. Pediatr Dent. 1999;21(6):325–326. [PubMed] [Google Scholar]
- 48.Filstrup SL, Briskie D, da Fonseca M, Lawrence L, Wandera A, Inglehart MR. Early childhood caries and quality of life: child and parent perspectives. Pediatr Dent. 2003;25(5):431–440. [PubMed] [Google Scholar]
- 49.American Academy of Pediatric Dentistry. Policy on the dental home. 2012. Available at: http://www.aapd.org/media/policies_guidelines/p_dentalhome.pdf. Accessed August 1, 2013.
- 50.Beil HA, Rozier RG. Primary health care providers’ advice for a dental checkup and dental use in children. Pediatrics. 2010;126(2):e435–e441. doi: 10.1542/peds.2009-2311. [DOI] [PubMed] [Google Scholar]
- 51.Long CM, Quinonez RB, Beil HA et al. Pediatricians’ assessments of caries risk and need for a dental evaluation in preschool aged children. BMC Pediatr. 2012;12(1):49–56. doi: 10.1186/1471-2431-12-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pahel BT. Referrals for Dental Care in a Medical Office-Based Preventive Dental Program [dissertation] Chapel Hill, NC: University of North Carolina Chapel Hill; 2008. [Google Scholar]
- 53.Rozier RG, Slade GD, Zeldin LP, Wang H. Parents’ satisfaction with preventive dental care for young children provided by nondental primary care providers. Pediatr Dent. 2005;27(4):313–322. [PubMed] [Google Scholar]
- 54.American Academy of Pediatric Dentistry. Guideline on caries-risk assessment and management for infants, children, and adolescents. 2013. Available at: http://www.aapd.org/media/Policies_Guidelines/G_CariesRiskAssessment.pdf. Accessed July 26, 2013.
- 55.Boulter S. Oral health risk assessment in the medical home. Oral health risk assessment in the medical home webinar: American Academy of Pediatrics, 2012. Available at: http://www2.aap.org/oralhealth/docs/OHRAWebinar.pdf. Accessed May 20, 2012. [Google Scholar]