Abstract
During a disaster or prolonged power outage, individuals who use electricity-dependent medical equipment are often unable to operate it and seek care in acute care settings or local shelters. Public health officials often report that they do not have proactive and systematic ways to rapidly identify and assist these individuals.
In June 2013, we piloted a first-in-the-nation emergency preparedness drill in which we used Medicare claims data to identify individuals with electricity-dependent durable medical equipment during a disaster and securely disclosed it to a local health department. We found that Medicare claims data were 93% accurate in identifying individuals using a home oxygen concentrator or ventilator.
The drill findings suggest that claims data can be useful in improving preparedness and response for electricity-dependent populations.
Advances in health care delivery and an aging population have meant that increasing numbers of people with serious chronic conditions can live at home independently or with assistance. New technologies, including many types of life-sustaining durable medical equipment (DME), have facilitated this transition. Although many people with significant medical needs function well day to day, disasters, particularly those that cause power outages, can cause life-threatening situations that may lead them to seek care in the acute care setting, such as an emergency department or hospital.1–3 Some may also seek care in shelters but, because of their special medical needs, may be turned away from commonly available general population shelters or placed in “special needs” shelters where they may become separated from their caregivers and loved ones. Others choose to shelter in their homes rather than seek help in hospitals or shelters, potentially endangering themselves.
Recognition of this problem is not new. For example, during the historic 2003 blackout in New York City, Prezant et al. found that chronically ill patients with respiratory device failure were responsible for the greatest increase in health care utilization, accounting for 65 emergency department visits and 37 hospitalizations during the 48-hour postblackout period.3 More recently, during Hurricane Isaac and Superstorm Sandy, multiple special needs shelters were established to assist these and other medically vulnerable populations. All required around-the-clock staffing by medical teams from the Medical Reserve Corps, local health departments, the US Public Health Service, or the National Disaster Medical System to ensure continuity of care.
Local public health officials continue to report during informal postemergency debriefings that they do not have proactive and systematic ways to accurately identify those with special medical needs, including those who require electricity-dependent DME. Given the local health departments’ role in providing for those with special medical needs in a disaster, some communities and utility companies maintain registries for which individuals can self-register; however, their timeliness, completeness, and accuracy vary. There is broad acknowledgment that having information for populations with special medical needs would be useful for emergency planning and preparedness efforts, and could be life-saving during a prolonged power outage or disaster.1,2,4–8
Medical claims data are a potential source of information for identifying individuals with life-sustaining medical equipment, either in advance of or after a disaster. However, the accuracy and usability of such information for this purpose is not thoroughly understood. To assess the accuracy of this information and its utility for a local public health response, we conducted a preparedness drill that used claims data from Medicare to identify individuals who required electricity-dependent respiratory DME.
METHODS
In June 2013, we simulated a hurricane that resulted in prolonged and widespread power outages in the city of New Orleans, Louisiana. The New Orleans Health Department provided written assurance that they would comply with requisite privacy and Health Insurance Portability and Accountability Act (HIPAA) requirements, per a protocol developed for the drill, and sent a formal electronic request to the Centers for Medicare & Medicaid Services (CMS) for a list of individuals using oxygen concentrators or ventilators. We used claims from the CMS DataLink Project, which uses preadjudicated Medicare claims data to conduct near-real-time monitoring and research and quality improvement analyses, to identify a limited data set of individuals living in New Orleans who had an oxygen concentrator or ventilator. We included individuals if they met the following criteria: they (1) were enrolled in Medicare Fee For Service Parts A and B in April 2013; (2) were alive in April 2013, as determined by the Medicare Enrollment Database; and (3) had either a Medicare Fee For Service Part B claim for a ventilator between May 31, 2012, and May 31, 2013, or a claim for an oxygen concentrator between May 31, 2010, and May 31, 2013. We excluded individuals residing in a skilled nursing facility, as determined by Medicare Fee For Service Part A and B claims and information from the Medicare Long-Term Care Minimum Data Set. The limited data set was securely disclosed, under the CMS’s oversight, by the CMS Datalink Project contractor to preauthorized HIPAA-trained New Orleans Health Department staff via a secure and password-protected Web portal.
The New Orleans Health Department, in partnership with the City of New Orleans Office of Homeland Security and Emergency Preparedness and the City of New Orleans Information Technology and Innovation Team, downloaded and mapped the data. We randomly selected 8 zip codes for the drill and 200 people residing within those zip codes whose names, addresses, and DME we sought to confirm. Eight teams composed of 3 or more HIPAA-trained individuals (personnel from the New Orleans health, fire, and police departments and emergency medical services and federal public health personnel) conducted visits to the residences of those randomly selected to confirm the accuracy of the information contained in the Medicare data. The New Orleans Health Department instructed the teams to confirm whether the person they spoke with was the person identified in the CMS data set, and whether the individual had an oxygen concentrator or ventilator. Each team attempted to visit the residences of 25 individuals during a 5-hour period.
RESULTS
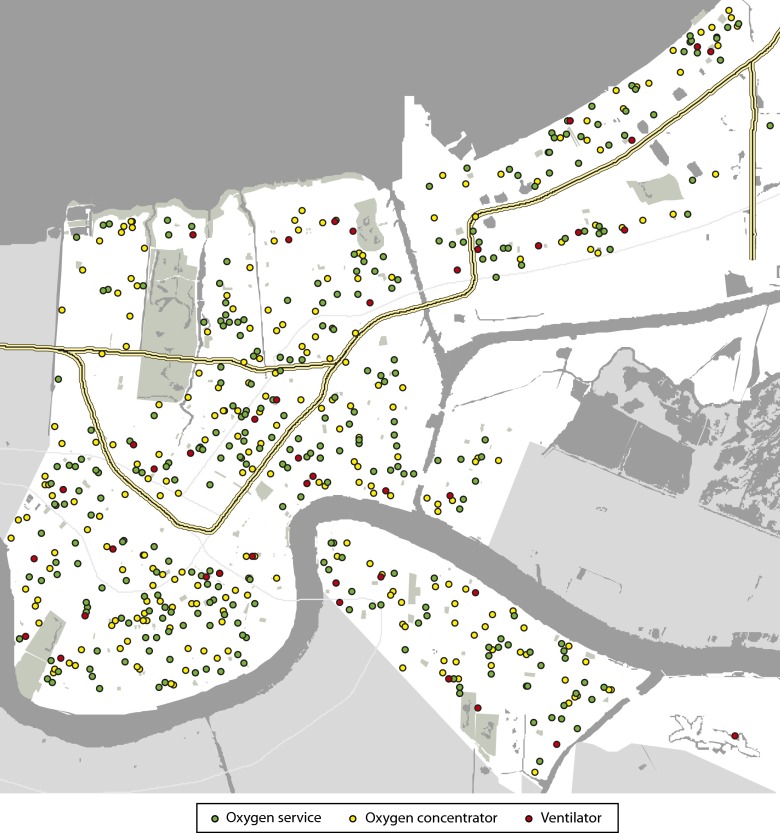
CMS claims data identified a total of 611 individuals in the city of New Orleans who had an oxygen concentrator or ventilator, and mapping of this data revealed no localized clusters of these individuals (Figure 1). Only 15 of these individuals were already on the city’s special medical needs registry. A total of 397 (65%) of these individuals lived in 1 of the 8 zip codes the city selected for the drill. Teams were able to visit 191 of the 200 addresses randomly selected for verification during the 5-hour drill period (Figure 2). Of these, 12 (6%) were not residential addresses. Someone was at home at 134 (75%) of the residences visited; we were able to confirm that 119 (89%) lived there and that 3 (2%) had recently died. Teams asked 99 of those visited about the type of DME they had; 92 (93%) of those asked confirmed that they had an oxygen concentrator or ventilator.
FIGURE 1—
Geographic distribution of Medicare beneficiaries using oxygen services, an oxygen concentrator, or a ventilator: New Orleans, LA; March 1–May 31, 2013.
FIGURE 2—
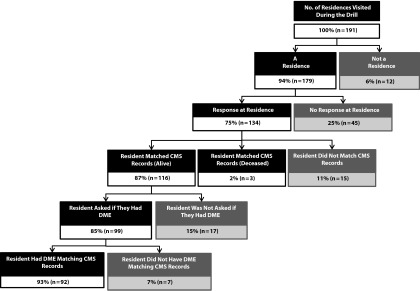
Flowchart showing results of emergency preparedness drill to identify users of electricity-dependent durable medical equipment: New Orleans, LA; June 10, 2013.
Note. CMS = Centers for Medicare & Medicaid Services; DME = durable medical equipment.
The drill demonstrated the feasibility of using claims data from Medicare to identify individuals living at home but dependent on electrically powered DME, and to do so in sufficient time to be useful for emergency response during a disaster. Furthermore, we demonstrated that a local health department was able to access and make meaningful and actionable use of this information while maintaining privacy and confidentiality.
DISCUSSION
Claims information can be used for emergency preparedness and planning by providing public health officials with de-identified information about the size and location of people with special medical needs in their communities, and by facilitating outreach to ensure that electricity-dependent individuals have a well-thought-out disaster plan. This information can also help preparedness planners even when focal clustering of electricity-dependent residents is not present, as it can help identify optimal shelter locations and potential backup power requirements needed to support these individuals. During an actual disaster, more specific information can be used to quickly identify individuals who may need direct outreach and assistance with fully charged backup batteries, evacuating, and sheltering, and to advise utility companies of priority power restoration needs. Although many utility companies and local health departments encourage such individuals to self-register for such priority, many of these registries where available are incomplete. Of particular concern was that a significant number of those visited noted that they were not aware of the opportunity to get registered despite the city’s recurrent public communication efforts to encourage registration.
Increasingly, claims data are being used to better manage and inform response operations during a disaster and to examine the health care system’s response. For example, during recent US Department of Health and Human Services (HHS) deployments, such as those of the Haiti earthquake and Superstorm Sandy, real-time data from the National Disaster Medical System’s Electronic Health Records were used to determine the demographic and clinical mix of patients presenting for care, therefore facilitating the deployment of the appropriate types of providers. In addition, following Superstorm Sandy, 2012 Medicare data were used to examine how well the end-stage renal disease system performed in ensuring that dialysis patients did not experience interruptions in care leading to adverse outcomes (J. Kelman et al., 2012, unpublished data). Although the use of claims data to identify and intervene with those who may be particularly vulnerable in a disaster may seem intuitive, neither our literature review nor discussions with numerous public health officials identified previous efforts to do so.
The data reported here are from a preparedness drill, and the teams received limited, just-in-time training at the onset of the drill. Unfortunately, a few teams neglected to verify the type of DME the residents had during the visit, thus resulting in incomplete information for 17 individuals.
Nonetheless, in this proof-of-concept drill, we found that claims data were highly accurate in identifying people with electricity-dependent DME. We believe that the primary reason was that data are available to the Medicare program quickly, often within weeks of service. We recognize that many individuals with electricity-dependent DME are not covered by Medicare, although many qualify for Medicare because of their disability status. We also cannot be certain that the claims data identified all of the Medicare beneficiaries living in the area with the DME of interest. Future work will focus on ways to further validate the information in additional localities, from other potential insurers, the Medicaid program, or other nongovernmental sources. It will also seek to identify other population groups that may need special assistance in disasters.
The success of this model depends on having appropriate protocols and privacy protections in place in advance of a disaster. It also depends on local capabilities to receive and manage the data for preparedness purposes. Furthermore, local health departments and governments will need the capacity not only to act upon the information in the emergency setting but to build resilience during nonemergency times. To that end, using the Flu Vaccination Map9 model developed for health departments to track Medicare flu vaccine uptake, HHS is developing an interactive zip code–level map that will contain de-identified information on the numbers of individuals reliant upon electricity-dependent DME. This information will help health care, public health, and emergency planners to better understand the needs of this population and can be expanded to other categories of at-risk individuals as appropriate. In our preparedness drill, the individuals we contacted were universally pleased that the New Orleans Health Department had contacted them during the drill, but we recognize that not all individuals may feel the same. We do not yet know how individuals will respond to being contacted during a major disaster, but we recognize that there are instances in which it could be lifesaving. We went to great lengths to ensure the protection of patients’ privacy during all aspects of the drill, including the secure disclosure of data. It will be crucial to implement appropriate safeguards to ensure that future users of this information protect personally identifiable information, even in the context of a disaster.
As we move toward providing claims-based information, such as this, to health departments during disasters, we will be paying special attention to whether the speed of making such information available can be replicated during a real-world, no-notice event. To that end, we were heartened when, in response to a boil water alert, the New Orleans Health Department requested information from the CMS regarding end-stage renal disease patients who require dialysis and those with parenteral feedings in the affected zip codes. Within 5 hours of the request, all of the required privacy and HIPAA assurances were in place, and a similar password-protected Web portal had been set up, populated, and accessed by preauthorized health department staff. They used this information to map the individuals residing within the boil water advisory zone and to reach out to them to ensure they were aware of the public health recommendation. The ability to do so resulted from close collaboration, coordination, and efforts to administratively prepare for such a scenario.
Although the use of medical claims data to identify those at high medical risk is a dramatic advance over the current more passive system used by most local entities, more can and should be done to improve the resilience of people living independently with DME every day and during a disaster. For example, batteries that enable equipment to maintain a charge for 72 hours would enable such people to align with Federal Emergency Management Agency “shelter in place” guidelines.10 DME could also incorporate a signaling device that might read the remaining battery power of a piece of equipment and signal caregivers or emergency responders with the global positioning system (GPS) coordinates of the device once it fell below a given battery charge threshold. HHS is using innovation challenges and competitions to identify additional ways to ensure resilience for those with special medical needs, including those who are electricity dependent, during a disaster.
The experience reported here provides tangible evidence of progress in better preparing, supporting, and responding to the needs of vulnerable medical populations in a community prior to a disaster. It also demonstrates a successful model for medicine, public health, and emergency management collaboration. If this work can be expanded to include claims data from other payors, it could provide a nearly complete picture of the populations with special medical needs in a community and be a central tool for emergency responders to assist those most in need, prioritize resources and power restoration, and help strengthen individual and community resilience between disasters.
Acknowledgments
The project was supported through the Centers for Medicare & Medicaid Services DataLink Project contract.
We thank staff and R. Erich Caulfield from the White House Strong Cities, Strong Communities Initiative; city of New Orleans police, fire, and emergency medical services agencies; Capt C. Mick Cote, Capt Louis Lightner, and Stacy Elmer from the HHS Office of the Assistant Secretary for Preparedness and Response; and Donald Moulds, PhD, and Jonathan Moore, MPP, from the HHS Office of the Assistant Secretary for Planning and Evaluation, for their participation in the drill. We thank Greg Reece from the City of New Orleans Office of Homeland Security and Emergency Preparedness, Sara Hudson from the New Orleans Information Technology and Innovation Team, and Charlotte Parent, RN, MCHM, and staff from the New Orleans Health Department for technical assistance. We thank Thomas E. MaCurdy, PhD, Maria Jauregui, BA, and Sasha Kapralov, MA, for data analytical assistance and Alicia Livinski, MPH, MA, for literature search assistance.
Note. The views expressed herein are solely those of the authors and do not necessarily represent those of the US Department of Health and Human Services or the City of New Orleans Health Department.
Human Participant Protection
Protocol approval was not sought because the drill was a response operations quality improvement project. All required procedures to protect patient privacy and confidentiality were followed.
References
- 1.Geehr EC, Salluzzo R, Bosco S, Braaten J, Wahl T, Wallenkampf V. Emergency health impact of a severe storm. Am J Emerg Med. 1989;7(6):598–604. doi: 10.1016/0735-6757(89)90282-9. [DOI] [PubMed] [Google Scholar]
- 2.Greenwald PW, Rutherford AF, Green RA, Giglio J. Emergency department visits for home medical device failure during the 2003 North America blackout. Acad Emerg Med. 2004;11(7):786–789. doi: 10.1197/j.aem.2003.12.032. [DOI] [PubMed] [Google Scholar]
- 3.Prezant D, Clair J, Belyaev S et al. Effects of the August 2003 blackout on the New York City healthcare delivery system: a lesson for disaster preparedness. Crit Care Med. 2005;33(1 suppl):S96–S101. doi: 10.1097/01.ccm.0000150956.90030.23. [DOI] [PubMed] [Google Scholar]
- 4.Beatty ME, Phelps S, Rohner C, Weisfuse I. Blackout of 2003: public health effects and emergency response. Public Health Rep. 2006;121(1):36–44. doi: 10.1177/003335490612100109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Platz E, Cooper H, Silvestri S, Siebert C. The impact of a series of hurricanes on the visits to two central Florida emergency departments. J Emerg Med. 2007;33(1):39–46. doi: 10.1016/j.jemermed.2007.02.023. [DOI] [PubMed] [Google Scholar]
- 6.Anderson G, Bell ML. Lights out: impact of the August 2003 power outage on mortality in New York, NY. Epidemiology. 2012;23(2):189–193. doi: 10.1097/EDE.0b013e318245c61c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fink S. Hurricane Isaac tests the region’s readiness to care for its neediest citizens. September 9, 2012. Available at: http://blog.nola.com/hurricane_impact. Accessed September 6, 2013.
- 8.Jan S, Lurie N. Disaster resilience and people with functional needs. N Engl J Med. 2012;367(24):2272–2273. doi: 10.1056/NEJMp1213492. [DOI] [PubMed] [Google Scholar]
- 9.US Dept of Health and Human Services. National Vaccine Program Office. Flu vaccination map, live tracking influenza vaccinations of Medicare beneficiaries: how is your community doing? November 8, 2013. Available at: http://www.hhs.gov/nvpo/flu-vaccination-map. Accessed January 25, 2014.
- 10.Federal Emergency Management Agency. Guidelines for staying put (sheltering in place) Available at: http://www.ready.gov/shelter. Accessed November 1, 2013.