Abstract
A 44-year-old woman presented with recurrent episodes of thunderclap headache. Neurological examination and computed tomography brain imaging were unremarkable. Cerebrospinal fluid findings were consistent with subarachnoid hemorrhage. Computed tomography angiography of the circle of Willis showed multiple areas of segmental vasoconstriction. This finding was confirmed on cerebral catheter angiography, with segmental vasoconstriction involving bilateral internal carotid, posterior cerebral, and external carotid branches. No aneurysm or other vascular abnormality was identified. She received treatment with nimodipine. A selective serotonin reuptake inhibitor, started 4 weeks earlier, was discontinued. Follow-up angiography after 3 months demonstrated complete resolution of the segmental vasoconstriction, confirming the diagnosis of reversible cerebral vasoconstriction syndrome (RCVS). She remained headache free at follow-up. To our knowledge, external carotid artery branch involvement in RCVS has been described only in one previous occasion.
Keywords: stroke and cerebrovascular disease, clinical specialty, headache, disorders, secondary, headache disorders, imaging, techniques
Case Report
A 44-year-old woman presented with recurrent episodes of sudden onset severe headache consistent with thunderclap headache. On the first occasion, she woke from sleep with difficulty in breathing and a choking sensation, followed by a sudden onset, severe, global headache, which reached maximal intensity within 30 seconds and was associated with vomiting. The pain eased over the next 2 hours. She attended her local hospital where the neurological examination was found to be normal. A computed tomography (CT) brain scan was normal. She was discharged with simple analgesia. Two days later, she had an identical episode, which again woke her from sleep, prompting a further visit to her local hospital. Two days after this, she experienced a third episode, this time without associated symptoms, during the daytime while talking to her husband. She attended our hospital on this third occasion. The neurological examination was normal. She had no significant past medical history apart from the commencement of a selective serotonin reuptake inhibitor (citalopram) for depression 4 weeks earlier. She was not taking any other medications and denied use of any illicit drugs.
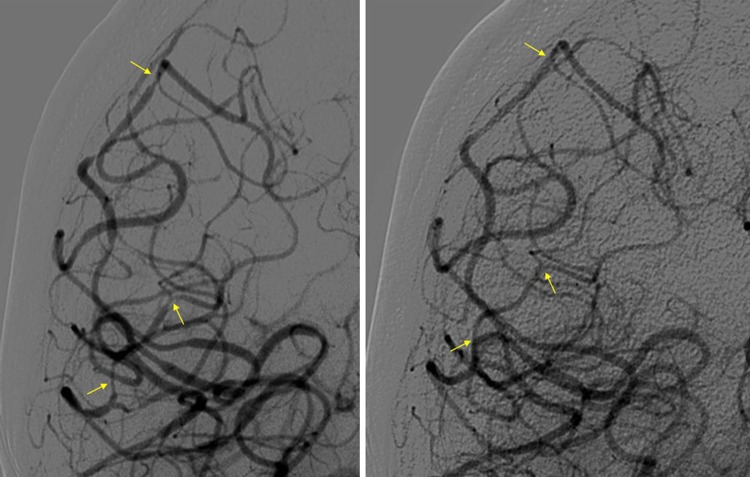
A repeat brain CT scan was obtained, which was again normal. A lumbar puncture showed findings consistent with subarachnoid hemorrhage, based on cerebrospinal fluid (CSF) spectrophotometry (net bilirubin absorbance > 0.007 AU and net oxyhemoglobin absorbance < 0.02 AU).1 Cerebrospinal fluid red blood cell count was 950 per mL. Cerebrospinal fluid constituents were otherwise normal (white blood cell count < 1 per mL, protein 0.42 g/L, and normal CSF–plasma glucose ratio). She then proceeded to have a CT angiogram of the circle of Willis, which showed focal areas of segmental narrowing involving the intracranial vessels, especially prominent in the left posterior cerebral and right M1 segment of the middle cerebral artery (MCA). There was no evidence of obvious aneurysm or intracranial vascular malformation. A cerebral catheter angiogram was undertaken. The right internal carotid artery (ICA) angiogram showed focal areas of vasoconstriction in the branches of the MCA and anterior cerebral artery (ACA). There was also flash filling of the posterior cerebral artery, which showed focal areas of vasoconstriction. Left ICA angiogram also revealed similar areas of focal narrowing. Bilateral vertebral angiograms showed several areas of narrowing affecting the bilateral posterior cerebral arteries, together with involvement of the posterior inferior cerebellar arteries. Figures 1A and 2A show representative images from right ICA and right VA angiography. Bilateral external carotid artery (ECA) angiograms also revealed areas of focal narrowing in the ECA branches to the scalp, particularly on the right side (Figure 3). There was no evidence of any aneurysm or other vascular abnormality.
Figure 1.
A and B, Baseline and 3-month follow-up right internal carotid artery angiograms showing segmental vasoconstriction (arrowed, A) with subsequent resolution at follow-up (arrowed, B).
Figure 2.
A and B, Baseline and 3-month follow-up right vertebral artery angiograms showing segmental vasoconstriction (arrowed, A) with subsequent resolution at follow-up (arrowed, B).
Figure 3.
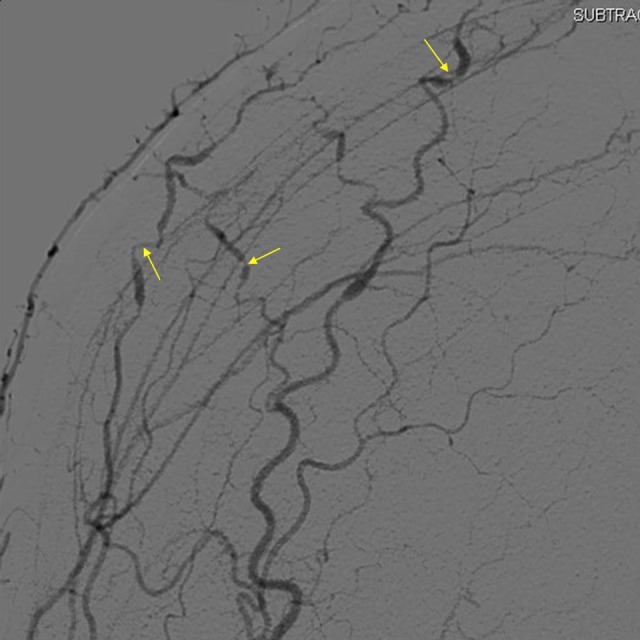
Baseline right external carotid artery angiogram showing segmental vasoconstriction.
On account of the likely diagnosis of reversible cerebral vasoconstriction syndrome (RCVS), she received treatment with nimodipine 60 mg 4 times a day for 4 weeks. Citalopram was discontinued. Her headaches resolved. In the absence of other features to support an inflammatory etiology (including noninflammatory CSF) and the clinical improvement without immunosuppression, cerebral vasculitis was considered extremely unlikely. A follow-up cerebral angiogram after 3 months showed complete resolution of the previously noted focal areas of narrowing involving the intracranial circulation (Figures 1B and 2B), confirming the diagnosis of RCVS. Right ECA angiogram follow-up images were not obtained. She has subsequently remained headache free after follow-up at 6 months.
Reversible cerebral vasoconstriction syndrome has been expertly reviewed recently.2 In essence, RCVS is thought to be attributable to a transient disturbance in the control of cerebrovascular tone. More than half the cases occur postpartum or after exposure to adrenergic or serotonergic drugs. Of course, peripheral vasoconstriction is known to occur with exposure to other vasoactive substances such as ergotamine.3 Manifestations of RCVS have a monophasic course and vary from pure cephalalgic forms to rare catastrophic forms associated with severe hemorrhagic and ischemic strokes, brain edema, and death. The spectrum of extracranial manifestations is expanding, including a recently reported association with cervical arterial dissection in RCVS.4 To our knowledge, involvement of ECA branches has been described only in one other case.5 This case adds to the literature on account of the unusual nature of ECA involvement and clear demonstration of the radiological findings and their reversibility.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Cruickshank A, Auld P, Beetham R, et al. Revised national guidelines for analysis of cerebrospinal fluid for bilirubin in suspected subarachnoid haemorrhage. Ann Clin Biochem. 2008;45(pt 3):238–244 [DOI] [PubMed] [Google Scholar]
- 2. Ducros A. Reversible cerebral vasoconstriction syndrome. Lancet Neurol. 2012;11(10):906–917 [DOI] [PubMed] [Google Scholar]
- 3. Ruano-Calderón LA, Zermeño-Pohls F. Ergotism. a case report and review of the literature. Rev Neurol. 2005;40(7):412–416 [PubMed] [Google Scholar]
- 4. Mawet J, Boukobza M, Franc J, et al. Reversible cerebral vasoconstriction syndrome and cervical artery dissection in 20 patients. Neurology. 2013;81(9):821–824 [DOI] [PubMed] [Google Scholar]
- 5. Melki E, Denier C, Théaudin-Saliou M, Sachet M, Ducreux D, Saliou G. External carotid artery branches involvement in reversible cerebral vasoconstriction syndrome. J Neurol Sci. 2012;313(1-2):46–47 [DOI] [PubMed] [Google Scholar]