Abstract
Background
Malaria during pregnancy causes severe anaemia, placental malaria or death to the mother while the fetus may be aborted or stillborn.
Objective
To establish the prevalence and factors associated with Insecticide Treated Net (ITN) utilisation among pregnant women in a post conflict Internally Displaced Persons (IDP) camps of Gulu district.
Methods
We conducted cross-sectional study in 20 IDP camps in which 769 pregnant women were interviewed for ITN utilisation the night before the survey. The 20 IDP camps were selected using simple random sampling technique as clusters. Households that had pregnant women were then consecutively selected. Data were entered in EpiData 3.1 and analyzed using STATA11.
Results
35% of pregnant women (95% CI 31% – 38%) had utilised ITNs. Factors that promoted ITN utilisation includes: antenatal visit (AOR 1.90, p-value 0.000); ITN awareness (AOR 1.57, p-value 0.011), and willingness to purchase ITN (AOR 2.12, p-value 0.000). Factors which hinder ITN utilisation were: hours taken to reach health centre (AOR 0.64, p-value 0.050) and being single/widow/divorced (AOR 0.22, p-value 0.000).
Conclusion
Majority of the respondents were not utilising ITN. Therefore, leaders in Gulu district should encourage pregnant woman to acquire and use ITN to reduce their vulnerability to malaria.
Keywords: Utilisation, ITN, pregnant women, post conflicts, internally displaced persons
Introduction
Worldwide, nearly 500 million people suffer a malaria episode every year1,2 and about 90% of all malaria deaths today occur in sub-Sahara Africa2. In Uganda, malaria accounts for about 30 – 50% of the outpatient burden and 35% of hospital admissions3. During pregnancy, malaria is a common cause of complications to both the mother and her unborn child. The mother may develop severe malaria4, severe anaemia5,6,7, placental malaria4 or may die8. The fetus may be aborted, prematurely delivered or stillborn8,9 and the baby may have a low birth weight4,5.
The prevention and control of malaria during pregnancy is therefore crucial as it helps to promote the health of the mother and her unborn child. There are currently two methods for malaria control during pregnancy being promoted by Ministry of Health in Uganda. These are chemoprophylaxis using sulfadoxine - pyrimethamine (SP) and insecticide treated net (ITN)3. However non adherence to chemoprophylaxis, irregular, late or non antenatal clinic attendance, women not given Intermittent Presumptive Treatment (IPT) by midwife and drug stock outs in most health facilities in Uganda is common10. These problems would not be encountered by pregnant women who own an ITN and thus making ITN more effective mean of malaria prevention in Uganda among pregnant women.
Studies in Western Kenya had shown that ITNs were associated with reductions in the incidence of malaria parasitemia and incidence of severe malarial anemia11. The prevalence of placental or maternal malaria was reduced resulting in reduced risk of low birth weight babies12,13. Studies have shown that free distribution of ITNs leads to increase use14 with 82% of participants reported using an ITN during pregnancy; 76% used it every night, and 79% reported a net re-treatment date within the last 6 months15. In Uganda, the national target of 50% of households to be covered with ITN by the year 2007 has not been met thus leaving many pregnant women at risk of malaria infection during pregnancies3. This study therefore aimed to establish the prevalence and factors associated with the utilisation of ITNs by pregnant women in post conflict Gulu district internally displaced person (IDP) camps.
Methods
We conducted a cross-sectional study using quantitative data collection techniques in the IDP camps of Gulu district which is a post conflict area in northern Uganda from March 3 – 19, 2009. Gulu is one of the districts which had been hit hard by the over two decades of arm conflict. The district has two counties and a Municipality. Generally life had been hard in Gulu district. People movement were restricted since the army had put curfew in both the Municipality and in the IDP camps. Most of the roads outlets outside the Municipality and IDP camps were planted with landmines. The IDP camps were situated in the two counties of Aswa and Omoro which were outside the Municipality. All the inhabitants of the IDPs lived in grass thatched hut or tents provided by the relief agencies. Lives in the IDP camps were generally hard as the population were cramped together in a small place. The IDPs were cut off from their farm land and were relying on relief food given by relief agencies. Few people in the IDP camps were able to have some petty businesses. Most of the health centres were non functional as staffs had abandon them due to insecurity. Also, in the IDP camps which do not have a government health facility, emergency relief organisation erected structures to provide some basic health care services. In all the IDP camps, health care services, education, water and sanitation were services provided by the emergency relief organisations and the United Nations.
Gulu district had thirty one (31) IDP camps with a population of 108,099 inhabitants as of June, 200816. The district is a high transmission area for malaria in Uganda. Unpublished data summary from Health Management Information System (HMIS) record of Gulu for malaria cases among pregnant women from July 2007 to June 2008 indicates that on average there were four hundred fifteen (415) cases of malaria among pregnant women per month17. Because of the appalling life situation in IDPs camps, non governmental organisations (NGOs) had distributed ITNs to the IDP camps and others through antenatal clinics.
Sample size estimation and Sampling method
The sample size was estimated using the modified Kish and Leslie formula of 196518
n = [z2pq/d2]*2Where: n = the sample size, z = the standard normal deviate (1.96 for a 95% confidence level), d = the level of precision desired (set at 0.05), p = the proportion of the population having ITN (0.5) (The proportion is unknown), q = the proportion of the population that does not have ITN (1-p) and 2 = Design effect. This gave sample size of 769 pregnant women.
A total of twenty (20) IDP camps were selected using simple random sampling as clusters for survey with ten (10) IDP camps in each County. The name of the IDP camps in each county was written on a piece of paper, folded and put inside a non transparent polythene bag for each county. The pieces of paper with the IDP camp name in them were then picked once at a time without putting it back into the polythene bag until we have generated the names of the 10 IDP camps in each of the two counties. The numbers of pregnant women to be interviewed in each IDP camp was determined using proportion to size cluster sampling method. The numbers of pregnant women to be interviewed in each IDP camp was got by dividing the population of pregnant women in the IDP camp by the total numbers of pregnant women in all the clusters and multiplying by the sample size (769). Within each IDP camp, we determined the centre first and then the direction of movement was got by spinning a bottle. The direction of movement was where the top faced when the bottle stopped spinning. We counted all the households from the centre to the end of the IDP camps/clusters. Each household was given a number on a piece of paper from the first to the last. To determine the starting household for the survey, we randomly picked a piece of paper containing the number assigned to the household. We then use consecutive sampling method by moving to the next nearest household to select pregnant women to be interviewed in each IDP camp.
The inclusion criteria for the study subjects were pregnant women who confirmed that they were pregnant and were resident of the twenty (20) selected IDP camps during the survey and present on the interview date who gave written informed consent to participate in the study. The study was approved by the Faculty of Medicine Research and Ethic Committee, Makerere University.
Data collection
Data was collected on socio-demographic characteristics, sources of ITN and ITN utilisation using a pretested, semi-structured questionnaire by trained research assistants. The respondents were asked whether they have slept under an ITN the night before the survey. ITN utilisation was taken as sleeping under an ITN the night before the survey. The questionnaire was translated into the local language (Acholi) and back translated to English to ensure consistency in meaning.
Data management and analysis
Data was entered into Epidata version 3.1, cleaned, coded, edited and exported to STATA version 11 for analysis. Categorical variables were displayed into frequencies and histogram while continuous variables were grouped into category using mean. We performed univariate, bivariate and multivariate analysis. Any factor at the bivariate level with p-value 0.2 was included in the multivariate analysis model to assess for interaction, confounding and also to determine the independent predictors of ITN utilization. We performed logistic regression model using the stepwise method for the predictors of ITN utilisation to first obtained the crude Odds Ratio and then run the model after adjusting for clustering of the data among the IDP camps. The result was considered to be statistically significance if the p-value < 0.05.
Results
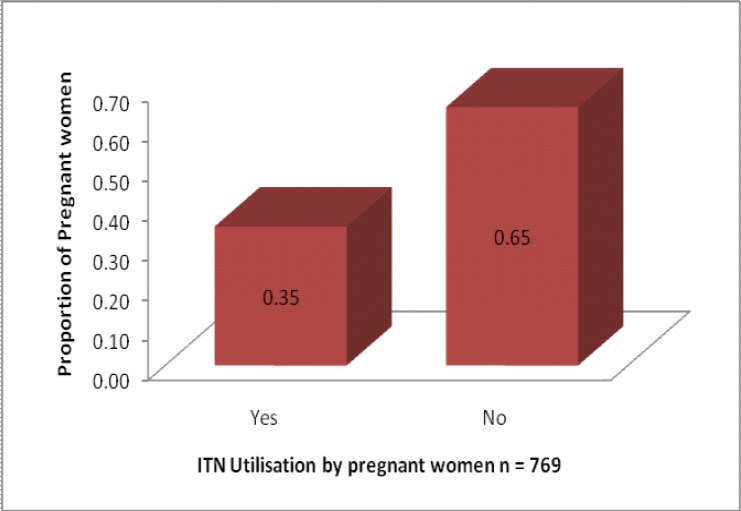
A total of 769 pregnant women were interviewed with age ranging from 14 to 45 years with a mean age of 25.3years and standard deviation (SD) of 6.2. 571 (74%) of the pregnant women had formal education. 477 (62%) of the pregnant women were cohabiting. 442 (58%) of the pregnant women took an hour or more to reach health centre. 648 (84%) of the pregnant women were multigravidae. The mean number of births was 3.6 with SD=2.1 and it ranges from 1 – 13 births. The mean gestation age was 5.7 months and ranges from 1 – 10 months. The mean income was Uganda shillings 14406 with SD = 41858 Shillings and ranges from zero Shillings per month to Shillings 500,000 per month. Figure 1 shows Univariate results for prevalence of ITN utilisation among pregnant women from Gulu district IDP camps. Prevalence of ITN utilisation among pregnant women in a post conflict district of Gulu was quite low at 35% (95% CI 31% – 38%) only.
Figure 1.
Prevalence of Insecticide treated net (ITN) utilisation
Factors which promoted ITN use at the bivariate level were ante-natal attendance (OR = 1.99, 95% CI 1.42 – 2.79, p-value 0.000), willingness to purchase ITN (OR = 2.51, 95% CI 1.83 – 3.44, p-value 0.000), being engaged in business (OR = 1.56, 95% CI 1.08 – 2.26, p-value = 0.017) and awareness about ITN (OR = 1.61, 95% CI 1.15 – 2.26, p-value = 0.005). Factors which hinder ITN utilisation among pregnant women were being Single/Widow/Divorce (OR = 0.19, 95% CI 0.08 – 0.45, p-value = 0.000) and time taken to reach health centre in hours (OR = 0.69, 95% CI = 0.50 – 0.94, p-value = 0.017). Table 2 summarises results for bivariate analysis of factors associated with ITN utilisation.
Table 2.
Bivariate analysis of factors associated with ITN utilisation
| Variables | Frequency | Utilised ITN | OR | 95% CI | P-value | |
| N | Yes | No | ||||
| Age | ||||||
| 14 – 25 | 423 | 157 | 262 | 1.00 | ||
| 26 – 45 | 346 | 114 | 232 | 0.84 | 0.62 – 1.14 | 0.262 |
| Education | ||||||
| No Formal education | 198 | 063 | 135 | 1.00 | ||
| Had Formal education | 571 | 208 | 363 | 0.80 | 0.57 – 1.14 | 0.214 |
| Religion | ||||||
| Catholic | 627 | 219 | 408 | 1.00 | ||
| Anglican (Protestant) | 088 | 027 | 061 | 0.82 | 0.51 – 1.33 | 0.427 |
| Moslem | 005 | 002 | 003 | 1.24 | 0.21 – 7.48 | 0.815 |
| Pentecostal | 046 | 021 | 025 | 1.56 | 0.85 –2.86 | 0.145 |
| Others | 002 | 000 | 002 | 0.00 | 0.300 | |
| Engage in Business | ||||||
| No | 620 | 205 | 415 | 1.00 | ||
| Yes | 147 | 064 | 083 | 1.56 | 1.08 – 2.26 | 0.017 |
| Marital status | ||||||
| Married/Cohabiting | 709 | 263 | 446 | 1.00 | ||
| Single/Widow/Divorce | 060 | 006 | 054 | 0.19 | 0.08 – 0.45 | 0.000 |
| Willingness to purchase ITN | ||||||
| No | 382 | 096 | 286 | 1.00 | ||
| Yes | 374 | 171 | 203 | 2.51 | 1.83 –3.44 | 0.000 |
| Time taken to reach Health Unit in hours | ||||||
| <1 | 442 | 169 | 273 | 1.00 | ||
| >1 | 315 | 094 | 221 | 0.69 | 0.50 – 0.94 | 0.017 |
| Awareness about ITN | ||||||
| No | 230 | 064 | 166 | 1.00 | ||
| Yes | 535 | 205 | 330 | 1.61 | 1.15 – 2.26 | 0.005 |
| Sources of Information about ITN | ||||||
| From Community | 095 | 029 | 066 | 1.00 | ||
| Health Centre | 202 | 096 | 106 | 2.06 | 1.22 – 3.48 | 0.006 |
| Radio | 228 | 077 | 151 | 1.16 | 0.69 – 1.95 | 0.572 |
| ITN Sources | ||||||
| Given from Health Centre | 233 | 200 | 033 | 1.00 | ||
| Given by NGO | 041 | 029 | 012 | 0.40 | 0.18 – 0.87 | 0.016 |
| Bought it Myself | 041 | 034 | 007 | 0.80 | 0.33 – 1.96 | 0.627 |
| Others | 008 | 005 | 003 | 0.28 | 0.06 – 1.22 | 0.069 |
| Ante-Natal Visit | ||||||
| No | 255 | 064 | 191 | 1.00 | ||
| Yes | 512 | 205 | 307 | 1.99 | 1.42 – 2.79 | 0.000 |
| Income per Month | ||||||
| <Shs 14406 | 600 | 205 | 395 | 1.00 | ||
| >Shs 14406 | 160 | 064 | 096 | 1.29 | 0.90 – 1.85 | 0.163 |
| Gestation Age (Months) | ||||||
| First Trimester | 152 | 041 | 111 | 1.00 | ||
| Second Trimester | 295 | 100 | 195 | 1.39 | 0.90 – 2.14 | 0.136 |
| Third Trimester | 314 | 126 | 188 | 1.81 | 1.18 – 2.78 | 0.006 |
The study showed that pregnant women who are single/widow/divorce were significantly less likely to utilise ITN than married/cohabiting pregnant women (AOR = 0.21, 95% CI 0.09 – 0.46, p-value = 0.000) and pregnant women who take more than one hour to reach health unit were significantly less likely to utilise ITN than their counter part who take an hour or less to reach health centre (AOR = 0.64, 95% CI 0.40 – 1.00, p-value = 0.050). However, pregnant women who were aware of ITN were 1.65 times more likely to utilise ITN than pregnant women who were not aware of ITN (AOR = 1.65, 95% CI 1.17 – 2.32, p-value = 0.004). Also pregnant women who were willing to purchase ITN were 2.37 times more likely to utilise ITN than those who were not willing (AOR = 2.37, 95% CI 1.43 – 3.93, p-value = 0.001), and pregnant women who have gone for antenatal visit were 1.83 times more likely to utilise ITN than those who have not gone for antenatal services (AOR = 1.83, 95% CI 1.25 – 2.66, p-value = 0.002).
Discussion
Our study indicates that ITN utilisation by pregnant women in Gulu district IDP camps was low at about only 35% compared with national target of 50% to have been achieved by the year 20073. This low ITN utilisation could be because of fewer pregnant women owning at least one ITN in Gulu district IDP camps as shown by the result of the Uganda Demographic and Health Survey (UDHS) of 2006 which indicates that 41.8% of the households in the IDP camps had at least one ITN. The report further reveals that only 20.9% of pregnant women had slept under an ITN a night before the survey in the IDP camps19. Our finding was similar to other studies done in Luwero district of central Uganda which showed that 31.3% of pregnant women reported using mosquito net during their previous pregnancy20, in Ethiopia which indicates that 58% of pregnant women slept under ITN21 and in Kenya which found that only 5% of pregnant women slept under ITN22. Our study has revealed several factors that promoted ITN utilization including ANC attendance, awareness about ITN and willingness to purchase ITN. The findings revealed that those who have at least attended ante-natal services were 1.83 times more likely to utilise ITN than those who had not (p-value = 0.002). This could be explained by the fact that those who initially had no ITN got it from health centre during ANC visit and was told the benefits of utilising ITN. A study by Gikandi et al in Kenya found that more than half of the net used by pregnant women were obtained from antenatal clinics23. Also, those who were having ITN were encouraged to utilise their ITN because of the benefits that they and their unborn baby will have if she utilise ITN. Also, warning of the consequences of not utilising ITN both to her and her unborn baby could have been given which ensure compliance with ITN utilisation.
Also pregnant women who had indicated that they would be willingness to purchase ITN were 2.37 times more likely to utilize ITN than those who were not willing to purchase ITN (p-value = 0.001). This could be attributed to the benefits of using ITN which they knew and that is why they were willing to purchase ITN. Other studies have indicated that cost was a barrier to ownership and use of ITN24,25,26. In our study, the majority of ITNs owned by the pregnant women were provided through health centres which were free of charge.
The pregnant women who reported to be aware of ITN were 1.65 times more likely to utilise ITN than those who were not aware of ITN (P-value = 0.004). However, when this was stratified according to the various sources, those who attributed hearing about ITN for the first time from health centre were about twice more likely to utilise ITN than those who reported hearing from the community (P-value = 0.006). While those who reported hearing about ITN for the first time over the radios were about 1.2 times more likely to utilise ITN though this was not statistically significant (P-value > 0.05). This could be because in the health centres, pregnant women are usually taught on the importance of protecting themselves against malaria during pregnancy and the danger associated with malaria during pregnancy to themselves and their unborn babies. Pregnant women who indicated that they have heard about ITN from within community were less likely to utilise ITN because the message given to them may not stress the importance of ITN utilisation by pregnant women and thus fail at influencing ITN utilisation. Other study had found that having ever heard a message about ITN was not associated with ITN use27.The study also revealed other factors that hindered ITN utilisation including marital status i.e. being single/widowed/divorce and time taken to reach Health Unit in hours. Marital status when adjusted for clustering was found to be highly significant at determining ITN utilisation with pregnant women who were single/widow/divorce were 0.21 times less likely to utilise ITN than married/cohabiting pregnant women (P-value = 0.000). This could be because of social support that married women received from their husbands, i.e. reminding them in case they had forgotten to hang their ITN up or encouraging them to use their ITN in case they are feeling lazy/reluctant to use ITN. Similar results were obtained in other studies14,27. Also a study in Kinshasa among pregnant women indicated that husbands were supportive of their wives to sleeping under their nets29.
We found that the time taken to reach health unit in hours was significant at determining ITN utilisation with those who reported to take more than an hour to reach health unit were 0.64 times less likely to utilise ITN than those who took an hour or less to reach health unit (P-value = 0.050). Similar result was obtained in a study by Gikandi et al where fewer women reported ITN use if they lived more than an hour walking distance to ante-natal clinic23. This could be because of lack of transport to the health unit or because of social responsibility in the home which can not make them free and they missed out ITN and vital health messages from the antenatal clinics, which could have influence over their attitude toward ITN utilisation.
Conclusion
Majority of the pregnant women in the post conflict IDP camps in Gulu district had not utilised ITN Only about a third of the pregnant women had utilized ITN which is below the 50% target set by the Ministry of Health of ITN coverage among vulnerable people by the year 2007.
Recommendations
Stakeholders (Ministry of Health and NGOs) should ensure adequate supply of ITN to pregnant women who live in post conflict areas like Gulu district and also sensitise them on the benefits of ITN utilisation. Also encourage pregnant women to acquire and use ITN as a mean of reducing their vulnerability to malaria disease since they live in housing that offers little protection aagainst mosquitoes.
Table 1.
Socio-demographic characteristics of respondents
| Variable | n (%) |
| Age | |
| 14 – 25 | 423 (55) |
| 26 – 45 | 346 (45) |
| Education | |
| No Formal education | 198 (26) |
| Had Formal education | 571 (74) |
| Education level | |
| Primary | 541 (95) |
| Secondary | 026 (05) |
| Tertiary | 002 (00) |
| Marital status | |
| Married | 232 (30) |
| Single | 058 (08) |
| Cohabiting | 477 (62) |
| Divorced | 001 (00) |
| Widowed | 001 (00) |
| Religion | |
| Catholic | 627 (82) |
| Anglican (Protestant) | 088 (11) |
| Moslem | 005 (01) |
| Pentecostal | 046 (06) |
| Others | 002 (00) |
| Time taken to reach Health unit in hours | |
| <1 | 442 (58) |
| >1 | 315 (42) |
| Gravidity | |
| Multigravidae | 648 (84) |
| Primigravidae | 121 (16) |
| Parity | |
| Para 0 | 127 (17) |
| Para 1 – 2 | 232 (30) |
| Para >3 | 410 (53) |
| Engage in business | |
| No | 620 (81) |
| Yes | 147 (19) |
| Awareness about ITN | |
| No | 230 (30) |
| Yes | 535 (70) |
| Being Employed (Salary earning) | |
| No | 761 (99) |
| Yes | 007 (01) |
| Gestation age in Trimesters | |
| First Trimester | 152 (20) |
| Second Trimester | 296 (39) |
| Third Trimester | 314 (41) |
| Income per month | |
| <Shs 14406 | 600 (79) |
| >Shs 14406 | 160 (21) |
Table 3.
Logistic regression analysis of predictors of ITN utilisation among pregnant women
| Variables | Crude | 95% CI (P-value) | Adjusted | 95% CI (P-value) |
| OR | OR | |||
| Being Single/Widow/Divorce | 0.21 | 0.08 – 0.54 (0.001) | 0.21 | 0.09 – 0.46 (0.000) |
| Awareness about ITN | 1.65 | 1.15 –2.37 (0.007) | 1.65 | 1.17 – 2.32 (0.004) |
| Willing to buy ITN | 2.37 | 1.71 – 3.27 (0.000) | 2.37 | 1.43 – 3.93 (0.001) |
| Antenatal Visit | 1.83 | 1.28 – 2.60 (0.001) | 1.83 | 1.25 – 2.66 (0.002) |
| Time taken to reach Health Unit in hours | 0.64 | 0.46 – 0 .88 (0.007) | 0.64 | 0.40 –1.00 (0.050) |
Variables in the model were adjusted for clustering of data among the IDP camps
Acknowledgements
The authors acknowledge with thanks the following: Gulu University Faculty of Medicine, Makerere Uni Belgian Scholarship which made this study possible.
References
- 1.WHO, author. The World Health Report, Making a Difference. 1999. Downloaded on 31/3/2008 at http://www.who.int/whr/1999/en/whr99en.pdf.
- 2.WHO, author. The African Malaria Report 2003 from WHO and UNICEF. 2003. Downloaded on 31/3/2008 at http://www.rbm.who.int/amd2003/amr2003/amr_doc.htm.
- 3.Ministry of Health. Republic of Uganda, author. Annual Health Sector Performance Report. 2007. Oct, [Google Scholar]
- 4.Stephen JR, Elena P, Abera G, Eyob T, Valentino ML, Malcolm EM. Placental Monocyte Infiltrates in Response to Plasmodium Falciparum Malaria Infection and Their Association With Adverse Pregnancy Outcomes. Am J Trop Med Hyg. 2003;68:115–119. [PubMed] [Google Scholar]
- 5.Adeyemi AS, Adekunle DA, Akinota SE. Use of Prevalence of insecticide treated mosquito bednets among pregnant population in Osogbo, Nigeria. Nigerian Medical Pract. 2007;52(2):29–23. [Google Scholar]
- 6.Brabin BJ. An analysis of malaria in pregnancy in Africa. Bulletin of the World Health Organization. 1983;61:1005–1016. [PMC free article] [PubMed] [Google Scholar]
- 7.Menendez C. Malaria during pregnancy: a priority area of malaria research and control. Parasitology Today. 1995;11:178–183. doi: 10.1016/0169-4758(95)80151-0. [DOI] [PubMed] [Google Scholar]
- 8.Menendez C, Ordi J, Ismail MR, Ventura PJ, Aponte JJ, Kahigwa E, Font F, Alonso PL. The Impact of Placental Malaria on Gestational Age and Birth Weight. The Journal of Infectious Diseases. 2000;181:1740–1745. doi: 10.1086/315449. [DOI] [PubMed] [Google Scholar]
- 9.Steketee RW, Nahlen BL, Parise ME, Menendez C. The Burden of Malaria in Pregnancy in Malaria-Endemic Areas. Am J Trop Med Hyg. 2001;64:28–35. doi: 10.4269/ajtmh.2001.64.28. [DOI] [PubMed] [Google Scholar]
- 10.Ndyomugyenyia R, Katamanywa J. Intermittent preventive treatment of malaria in pregnancy (IPTp): do frequent antenatal care visits ensure access and compliance to IPTp in Ugandan rural communities? Transactions of the Royal Society of Tropical Medicine and Hygiene. 2010;104:536–540. doi: 10.1016/j.trstmh.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Gamble C, Ekwaru JP, Ter Kuile FO. Insecticide-treated nets for preventing malaria in pregnancy. Cochrane Database Systematic Reviews. 2006:CD003755. doi: 10.1002/14651858.CD003755.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ter Kuile FO, Dianne JT, Penelope APH, et al. Reduction of Malaria during Pregnancy by Permethrin-Treated Bed Nets in an Area of Intense Perennial Malaria Transmission in Western Kenya. Am J Trop Med Hyg. 2003;68:50–60. [PubMed] [Google Scholar]
- 13.William AH, Ter Kuile FO, Steketee RW, et al. Implications of the Western Kenya Permethrin-Treated Bed Net Study for Policy, Program Implementation, and Future Research. Am J Trop Med Hyg. 2003;68:168–173. [PubMed] [Google Scholar]
- 14.Marchant T, Schellenberg JA, Edgar T, et al. Socially marketed insecticide-treated nets improve malaria and anaemia in pregnancy in southern Tanzania. Tropical Medicine and International Health. 2002;7:149–158. doi: 10.1046/j.1365-3156.2002.00840.x. [DOI] [PubMed] [Google Scholar]
- 15.Van Eijk AM, Blokland IE, Slutsker L, et al. Use of intermittent preventive treatment for malaria in pregnancy in a rural area of western Kenya with high coverage of insecticide-treated bed nets. Tropical Medicine and International Health. 2005;10:1134–1140. doi: 10.1111/j.1365-3156.2005.01497.x. [DOI] [PubMed] [Google Scholar]
- 16.United Nation High Commissioner for Refugee. unpublished data from Gulu office 2008. [Google Scholar]
- 17.Gulu district Health Management and Information System record. Unpublished data from July 2007 – June 2008. [Google Scholar]
- 18.Kish Leslie, et al. survey sampling. NY: John Wiley and Sons; 1965. [Google Scholar]
- 19.Uganda Bureau of Statistics, author. Uganda Demographic and Health Survey report. 2007. [Google Scholar]
- 20.Mpungu KS, Mufubenga P. Use of antenatal care, maternity services, intermittent presumptive treatment and insecticide treated bed nets by pregnant women in Luwero district, Uganda. Malaria Journal 2008. 7 doi: 10.1186/1475-2875-7-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mebrahtom B, Wakgari D. Use of insecticide treated nets by pregnant women and associated factors in a pre-dominantly rural population in northern Ethiopia. Tropical Medicine and International Health. 2008;13:1303–1313. doi: 10.1111/j.1365-3156.2008.02159.x. [DOI] [PubMed] [Google Scholar]
- 22.Guyatt HL, Noor AM, Ochola SA, Snow RW. Use of intermittent presumptive treatment and insecticide treated bed nets by pregnant women in four Kenyan districts. Tropical Medicine and International Health. 2004;9:255–261. doi: 10.1046/j.1365-3156.2003.01193.x. [DOI] [PubMed] [Google Scholar]
- 23.Gikandi PW, Noor AM, Gitonga CW, Ajanga AA, Snow RW. Access and barriers to measures targeted to prevent malaria in pregnancy in rural Kenya. Tropical Medicine and International Health. 2008;13:208–217. doi: 10.1111/j.1365-3156.2007.01992.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Noor AM, Omumbo JA, Amin AA, Zurovac D, Snow RW. Wealth, mother's education and physical access as determinants of retail sector net use in rural Kenya. Malar J. 2006:5. doi: 10.1186/1475-2875-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guyatt HL, Ochola SA, Snow RW. Too poor to pay: charging for insecticide-treated bednets in highland Kenya. Trop Med Int Health. 2002;7:846–850. doi: 10.1046/j.1365-3156.2002.00929.x. [DOI] [PubMed] [Google Scholar]
- 26.Osero JS, Otieno MF, Orago AS. Mothers' knowledge on malaria and vector management strategies in Nyamira District, Kenya. East Afr Med J. 2006;83:507–514. doi: 10.4314/eamj.v83i09.46774. [DOI] [PubMed] [Google Scholar]
- 27.Gashaw D, Wakgari D. Knowledge and Utilisation of insecticide treated mosquito nets among freely supplied households in Wonago Woreda, Southern Ethiopia. Ethiop J Health Dev. 2008;22:34–41. [Google Scholar]
- 28.Kagoma SM, Kabalimu TK, Mbaruku G. Determinants of Utilisation of Mosquito Bednets for Malaria Prevention among Pregnant Women in Kigoma Urban District, Western Tanzania. East African Journal of Public Health. 2006;3:31–34. [Google Scholar]
- 29.Audrey P, Eboni T, Nku D, et al. Free distribution of insecticide treated bed nets t o pregnant women in Kinshasa: an effective way to achieve 80% use by women and their newborns. Tropical Medicine and International Health. 2009;14:20–28. doi: 10.1111/j.1365-3156.2008.02179.x. [DOI] [PubMed] [Google Scholar]