Abstract
When food is heated to high temperatures, the characteristic “browning” generates advanced glycation end products (AGEs). AGEs are associated with an increased risk of cardiovascular disease, diabetes, and other adverse outcomes. Whether dietary AGEs are absorbed and are harmful to human health remains highly controversial. The objective of this study was to compare the effects of a diet high or low in AGEs on endothelial function, circulating AGEs, inflammatory mediators, and circulating receptors for AGEs in healthy adults. A randomized, parallel-arm, controlled dietary intervention was conducted for 6 wk with 24 healthy adults, aged 50–69 y, that compared isocaloric, food-equivalent diets that were prepared at either high or mild temperatures. Peripheral arterial tonometry, serum and urine carboxymethyl-lysine (CML), inflammatory mediators (interleukin-6, C-reactive protein, vascular adhesion molecule-1, and tumor necrosis factor-α receptors I and II), soluble receptor for AGEs, and endogenous secretory receptor for AGEs were measured at baseline and after 6 wk of dietary intervention. In the low-AGE diet group, the following changed from baseline to 6 wk (mean ± SE): serum CML from 763 ± 24 to 679 ± 29 ng/mL (P = 0.03) and urine CML from 1.37 ± 1.47 to 0.77 ± 2.01 μg/mL creatinine (P = 0.02). There were no significant changes in serum and urinary CML concentrations from baseline to follow-up in the high-AGE diet group. A high- or low-AGE diet had no significant impact on peripheral arterial tonometry or any inflammatory mediators after 6 wk of dietary intervention. In healthy middle-aged to older adults, consumption of a diet high or low in AGEs for 6 wk had no impact on endothelial function and inflammatory mediators, 2 precursors of cardiovascular disease. This trial was registered at clinicaltrials.gov as NCT01402973.
Introduction
Advanced glycation end products (AGEs)8 are possible dietary risk factors for adverse health outcomes (1). Major sources of systemic AGEs are endogenous AGEs generated in the body and exogenous AGEs in foods. When food is heated to high temperatures, the characteristic “browning” generates Maillard reaction products, also known as AGEs. The Western diet is rich in AGEs that are formed when food is processed at high temperatures (2).
AGEs in food are absorbed in the gut, enter the circulation, are deposited in tissues, metabolized, and/or excreted in the urine. AGEs play a role in atherosclerosis by cross-linking collagen in vessel walls, oxidizing of LDL, and increasing inflammation through the receptor for AGE (RAGE) (3). RAGE is also found in the circulation in 2 major forms: 1) RAGE cleaved from the surface of cells; and 2) endogenous secretory RAGE (esRAGE) secreted by cells (4). Older adults with elevated serum carboxymethyl-lysine (CML), a well-characterized circulating AGE, have an increased risk of arterial stiffness (5, 6), greater carotid diameter (7), and death (8–10).
Whether AGEs in foods represent a risk to human health remains highly controversial (11). A barrier to understanding whether dietary AGEs are a health risk has been the lack of rigorously conducted, controlled clinical trials of dietary AGEs in healthy adults (12). Human trials involved single meals or oral challenges high in AGEs in patients with diabetes or renal failure (13–15). High dietary intake of AGEs was associated with elevations in inflammatory mediators in diabetics (16). A trial conducted in healthy college students compared diets that were high vs. low in AGEs (17). However, the diets were dissimilar in nutrient content and not isocaloric. Other dietary and lifestyle interventions may influence circulating AGEs (18, 19).
Although AGEs have been implicated in many diseases, including atherosclerosis and cardiovascular disease, the impact of restricting dietary AGEs has not been well characterized in healthy adults. We hypothesized that dietary intake of AGEs would affect serum and urinary CML and have an impact on endothelial dysfunction and inflammation. To address these hypotheses, we conducted a controlled dietary intervention that compared the chronic effects of diets that were high vs. low in AGEs in healthy adults.
Participants and Methods
Study design and participants.
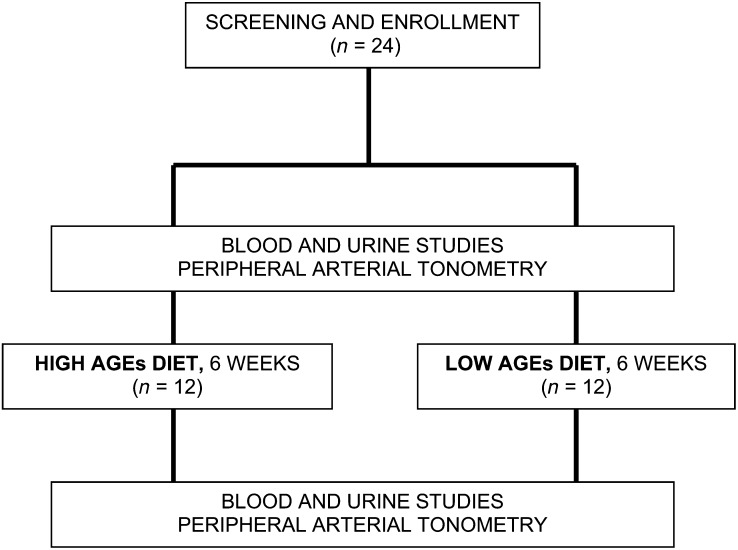
The study was a randomized, parallel-arm, controlled 6-wk dietary intervention involving 24 community-dwelling adults, aged 50–69 y, at the USDA Beltsville Human Nutrition Research Center (BHNRC) in Beltsville, Maryland, in October and November 2011 (Fig. 1). The study was publicized by advertisements. Potential participants attended an information session at the BHNRC in which the study protocol and informed consent document were reviewed by the project coordinator (S.K.G). A Mini-Mental State Examination (20) was given to all potential participants. Participants who gave written, informed consent returned on a subsequent morning for screening tests that included blood pressure and BMI measurements, fasting venous blood samples, and a spot urine sample collection.
FIGURE 1.
Flow diagram of the clinical trial. AGE, advanced glycation end product.
Individuals were eligible if they fit these criteria: 1) aged ≥50 and <70 y; 2) non-smokers; 3) no history of diabetes, thyroid disease, cardiovascular disease, chronic obstructive pulmonary disease, inflammatory bowel disease, liver disease, chronic kidney disease, or Raynaud’s disease; 4) not taking regular vitamin supplements or, if taking supplements, willing to discontinue taking supplements during the duration of the study; 5) not taking vitamin B-6 (pyridoxamine) (≥50 mg), a known AGE inhibitor (21); 6) not taking aspirin or nonsteroidal anti-inflammatory medications or, if so, willing to discontinue taking them during the duration of the study; 7) BMI of ≥18.5 to <30 mg/kg2; 8) no major food allergies; 9) no history of eating disorders or other dietary patterns different from the typical American diet; 10) no loss of >10% of body weight within the past 12 mo or plan to initiate a weight loss program during the next 2 mo; 11) no medical, psychiatric, or behavioral factors that might interfere with study participation; 12) willing to consume the experimental diets; 13) Mini-Mental State Examination score of <23; 14) TGs ≤ 300 mg/dL, hemoglobin > 11 g/dL, creatinine < 1.5 mg/dL, fasting glucose ≤ 125 mg/dL, and no proteinuria; and 15) gave written, informed consent.
Experimental diets.
Participants were matched by sex and BMI (±3 kg/m2) and randomly assigned to consume either diet using a computer random-number generator. The project coordinator assigned participants to interventions using a color-coded scheme to maintain blinding. Investigators and staff were unaware of the treatment through the intervention and during all analyses. Diets were prepared in the research kitchen of the BHNRC under the observation of a dietitian, research associate, or investigator. The kitchen staff was aware of the treatment assignment. Participants received breakfast and dinner in the dining room of the BHNRC, Monday through Friday. Lunch and weekend meals were provided as carryout for offsite consumption.
Diets consisted of 3 meals per day and 1 evening snack. Using a reference database for AGE content in foods (22), the high-AGE diet was ∼4 times higher in AGEs than the low-AGE diet. Diets were either high or low in AGEs depending on how the same foods were prepared: 1) beef and chicken were either roasted in the oven at 204.4°C until brown or covered with foil (to prevent browning) and heated to 121.1°C; 2) shrimp was roasted in the oven or steamed; 3) bread products were toasted or untoasted; 4) ice cream was made with high temperature–treated evaporated milk or with regular milk; 5) nuts were toasted or served raw; and 6) croutons for salads were toasted brown or dried to prevent browning.
High- and low-AGE diets were isocaloric and nutrient equivalent (Table 1). Meals were designed using The Food Processor software (ESHA Research). Diets comprised traditional American foods incorporated into a 7-d menu cycle. Participants were instructed to consume all and only foods provided by the BHNRC. Meals were fed in amounts that maintained body weight at enrollment. Participants were weighed daily, Monday through Friday, and if a consistent pattern of weight gain or loss were observed, adjustments were made to individual caloric intake [in 837 kJ (200 kcal) increments], if necessary, to keep participants at a steady weight. Participants were encouraged to maintain their normal exercise routine. Daily questionnaires were competed by participants to assess general health, use of over-the-counter medications, and diet and exercise over the past 24 h. The follow-up rate of the participants was 100%.
TABLE 1.
Nutrient composition of the study diet1
| Unit/d | |
| Weight, g | 1229 |
| Energy, kcal | 1800 |
| Protein, g | 77 |
| Carbohydrate, g | 244 |
| Fiber, g | 13.4 |
| Sugar, g | 126 |
| Total fat, g | 59 |
| Saturated fat | 23.4 |
| trans fat, g | 0.9 |
| Cholesterol, mg | 485 |
| Vitamin A, IU | 7812 |
| Thiamin, mg | 1.02 |
| Riboflavin, mg | 1.56 |
| Niacin, mg | 16.9 |
| Vitamin B-6, mg | 1.27 |
| Vitamin B-12, μg | 3.52 |
| Biotin, μg | 26.6 |
| Vitamin C, mg | 46.6 |
| Vitamin D, IU | 127 |
| Calcium, mg | 933 |
| Iron, mg | 12.0 |
| Sodium, mg | 2211 |
Diet composition was analyzed using The Food Processor (ESHA Research). The nutrient composition reported represents an example of an 1800 kcal diet. Participants were assigned to a calorie amount to meet their energy requirements.
The Johns Hopkins University School of Medicine and MedStar Health Research Institute institutional review boards approved the protocol. This trial was registered at clinicaltrials.gov as NCT01402973.
Data collection.
Demographic and health data were collected using standardized questionnaires at screening. All staff involved with phlebotomy, sample collection, measurement of endothelial function, and administration of questionnaires were unaware of the treatment. Endothelial function and serum and urinary biomarkers were measured on the first day of the 6-wk experimental diet period and the day after completion of the period. Participants were seen in the early morning after a 12-h fast. Endothelial function was measured using peripheral arterial tonometry (EndoPAT; Itamar Medical) (23). The same 2 technicians performed the test during the entire study, and technicians were assigned to do pre- and post-measurements on the same study participants following the protocol of the manufacturer (EndoPAT). Fasting venous blood samples were drawn twice during the study for analyte measurements in duplicate. All laboratory studies were run in a blinded manner. Total cholesterol, HDL cholesterol, TGs, and glucose were measured at enrollment and 6 wk. ELISA was used for measurement of serum and urine CML (Microcoat) (24, 25), IL-6, secretory RAGE (sRAGE), vascular cell adhesion molecule-1 (VCAM-1), TNF-α receptor I (TNF-α RI), TNF-α receptor II (TNF-α RII) (all Quantikine; R&D Systems), high-sensitivity C-reactive protein (CRP) (Alpco), and esRAGE (B-Bridge). The interassay and intra-assay CVs for all analytes measured by ELISA were <5%. Plasma TGs and total cholesterol were measured by an enzymatic method (ABA-200 ATC Biochromatic Analyzer; Abbott Laboratories). HDL cholesterol was determined by a dextran sulfate-magnesium precipitation procedure (26). LDL cholesterol was estimated using the Friedewald formula (27). Serum glucose was measured by the glucose oxidase method (Beckman Coulter). Urine creatinine was measured using a colorimetric assay (Creatinine assay kit; Abcam).
Statistical analysis.
Primary outcome measures were endothelial function, as indicated by reactive hyperemia index (RHI), and serum and urinary CML concentrations. Secondary outcome measures were CRP, IL-6, VCAM-1, TNF-α RI, TNF-α RII, lipids, fasting plasma glucose, sRAGE, and esRAGE. The sample size of 12 participants in a group gave >80% power to detect the following between the groups: 1) a priori 30% difference in the RHI, given mean RHI of 2.25, σ = 0.58; 2) 8% difference in urinary CML, given mean log-transformed urinary CML of 7.00, σ = 0.45; and 3) 3% difference in serum CML, given mean log-transformed serum CML of 6.62, σ = 0.11, and for all power calculations, α = 0.05, and a 2-sided test.
Continuous variables were reported as means ± SDs or least-square means ± SEs. Spearman correlations were used to examine relations between variables at baseline. Both repeated-measures ANOVA and multiple linear regression that controls for within-participant repeated measures were used to examine the effects due to age, sex, diet, time, and their interaction. All analyses were conducted using SAS 9.1 (SAS Institute) with a type I error of 0.05.
Results
Characteristics of the study participants at baseline are shown in Table 2. There were no significant differences between the participants in 2 diet groups by age, sex, BMI, and systolic or diastolic blood pressure. Spearman correlations for selected variables at baseline are shown in Supplemental Table 1. Serum CML was positively correlated with age and negatively correlated with BMI. BMI was positively correlated with IL-6 and CRP. Serum VCAM-1 was positively correlated with TNF-α RI. There was a positive correlation between sRAGE and esRAGE. There were no significant correlations between the remaining variables.
TABLE 2.
Characteristics of the study participants at baseline by dietary group1
| Characteristic | Low-AGE diet (n = 12) | High-AGE diet (n = 12) |
| Age, y | 57.9 ± 6.0 | 60.6 ± 4.3 |
| Sex, % | ||
| Male | 41.7 | 41.7 |
| Female | 58.3 | 58.3 |
| BMI, kg/m2 | 26.4 ± 4.0 | 26.1 ± 3.4 |
| Systolic blood pressure, mm Hg | 130 ± 18 | 126 ± 13 |
| Diastolic blood pressure, mm Hg | 79 ± 11 | 75 ± 10 |
Presented as means ± SDs for continuous variables and percentages for categorical variables. AGE, advanced glycation end product.
Endothelial function, serum and urinary CML, markers of inflammation, lipids, fasting plasma glucose, and receptors for AGEs at enrollment and 6 wk are shown in Table 3. There were no significant differences in RHI, serum CML, urinary CML, IL-6, CRP, VCAM-1, TNF-α RI, TNF-α RII, total cholesterol, HDL cholesterol, LDL cholesterol, TGs, fasting plasma glucose, sRAGE, or esRAGE between the low- vs. high-AGE diet groups at baseline or the 6 wk follow-up visit. There was an 11% decrease in serum CML (P = 0.03) and 44% decrease in urinary CML (P = 0.02) from baseline to follow-up within the group that was fed a low-AGE diet. There were no significant changes in serum or urinary CML from baseline to follow-up in the group that was fed a high-AGE diet. There were no significant changes in any of the other measures from baseline to follow-up within each dietary group.
TABLE 3.
Endothelial function, serum and urinary CML concentrations, markers of inflammation, and receptors for AGEs at baseline and after 6 wk of dietary intervention in 24 healthy adults, aged 50–69 y1
| Characteristic | Low-AGE diet (n = 12) | P within group, baseline to 6-wk low-AGE diet | High-AGE diet (n = 12) | P within group, baseline to 6-wk high-AGE diet | P between diet groups |
| Reactive hyperemia index | 0.34 | 0.77 | |||
| Baseline | 2.29 ± 0.17 | 2.22 ± 0.17 | 0.84 | ||
| 6 wk | 2.03 ± 0.17 | 2.31 ± 0.17 | 0.31 | ||
| Serum CML, ng/mL | 0.03 | 0.28 | |||
| Baseline | 763 ± 24 | 751 ± 24 | 0.79 | ||
| 6 wk | 678 ± 29 | 711 ± 29 | 0.42 | ||
| Urinary CML, μg/mg creatinine | 0.02 | 0.56 | |||
| Baseline | 1.37 ± 1.47 | 1.03 ± 1.47 | 0.21 | ||
| 6 wk | 0.77 ± 2.01 | 1.21 ± 2.01 | 0.12 | ||
| Serum IL-6, pg/mL | 0.94 | 0.81 | |||
| Baseline | 1.48 ± 0.53 | 2.25 ± 0.53 | 0.25 | ||
| 6 wk | 1.53 ± 0.39 | 2.09 ± 0.39 | 0.39 | ||
| Serum CRP, mg/L | 0.60 | 0.93 | |||
| Baseline | 2.11 ± 0.42 | 1.57 ± 0.42 | 0.39 | ||
| 6 wk | 2.62 ± 0.65 | 1.38 ± 0.65 | 0.16 | ||
| Serum VCAM-1, μg/mL | 0.30 | 0.87 | |||
| Baseline | 1.26 ± 0.23 | 1.39 ± 0.23 | 0.95 | ||
| 6 wk | 1.01 ± 0.26 | 1.34 ± 0.26 | 0.22 | ||
| Serum TNF-α RI, ng/mL | 0.65 | 0.61 | |||
| Baseline | 2.03 ± 0.09 | 1.96 ± 0.09 | 0.76 | ||
| 6 wk | 1.93 ± 0.19 | 2.07 ± 0.19 | 0.52 | ||
| Serum TNF-α RII, ng/mL | 0.56 | 0.52 | |||
| Baseline | 3.44 ± 0.29 | 2.94 ± 0.29 | 0.31 | ||
| 6 wk | 3.17 ± 0.30 | 3.28 ± 0.30 | 0.85 | ||
| Plasma total cholesterol, mg/dL | 0.08 | 0.15 | |||
| Baseline | 191 ± 13 | 196 ± 13 | 0.66 | ||
| 6 wk | 221 ± 13 | 220 ± 13 | 0.96 | ||
| Plasma HDL cholesterol, mg/dL | 0.40 | 0.98 | |||
| Baseline | 57 ± 4 | 67 ± 4 | 0.09 | ||
| 6 wk | 61 ± 5 | 66 ± 5 | 0.37 | ||
| Plasma LDL cholesterol, mg/dL | 0.06 | 0.13 | |||
| Baseline | 111 ± 11 | 110 ± 11 | 0.99 | ||
| 6 wk | 141 ± 12 | 132 ± 12 | 0.66 | ||
| Plasma TGs, mg/dL | 0.41 | 0.59 | |||
| Baseline | 114 ± 19 | 96 ± 19 | 0.53 | ||
| 6 wk | 91 ± 15 | 110 ± 15 | 0.48 | ||
| Fasting plasma glucose, mg/dL | 0.64 | 0.64 | |||
| Baseline | 97 ± 3 | 93 ± 3 | 0.61 | ||
| 6 wk | 93 ± 3 | 96 ± 3 | 0.69 | ||
| Serum sRAGE, ng/mL | 0.77 | 0.74 | |||
| Baseline | 1.42 ± 0.25 | 1.78 ± 0.25 | 0.21 | ||
| 6 wk | 1.30 ± 0.19 | 1.91 ± 0.20 | 0.07 | ||
| Serum esRAGE, ng/mL | 0.80 | 0.78 | |||
| Baseline | 0.52 ± 0.07 | 0.45 ± 0.07 | 0.48 | ||
| 6 wk | 0.54 ± 0.07 | 0.48 ± 0.07 | 0.49 |
Values expressed as least-square means ± SEs. P values were calculated using multivariate linear regression controlling for within-participant repeated measures that examined effects due to age, sex, diet, time, and interaction of diet × time. AGE, advanced glycation end product; CML, carboxymethyl-lysine; CRP, C-reactive protein; esRAGE, endogenous secretory receptor for AGE; sRAGE, secretory receptor for AGE; TNF-α RI, TNF-α receptor I; TNF-α RII, TNF-α receptor II; VCAM-1, vascular cell adhesion molecule-1.
Discussion
The present study showed that, contrary to our original hypothesis, endothelial function after a 12-h fast was not affected by a diet that was high or low in AGEs in healthy adults. To our knowledge, this is the only trial that examined the chronic effects of meals that are high or low in AGEs on endothelial function in healthy adults. Healthy adults were the participants of this study, because modulation of dietary intake of AGEs has been discussed as a possible strategy in reducing risk of diabetes and cardiovascular disease (1). Endothelial function was measured using peripheral arterial tonometry, a tool that was validated (23) and applied for assessment of microvascular function in the Framingham Heart Study (28). Previous studies examined the effect of single meals on flow-mediated dilation in the postprandial period (14, 15) and are not directly comparable with the present study. Participants who consumed low-AGE meals had a significant decrease in both serum and urinary CML concentrations by the 6-wk follow-up visit, which verifies that the relative restriction of AGE-rich foods had an effect in lowering circulating and excreted CML. The participants who consumed meals that were high in AGEs did not have a significant increase in serum and urinary CML concentrations by the 6-wk follow-up visit. The lack of an apparent increase may be due to the fact that the usual American diet contains AGEs in amounts similar to what was fed in the high-AGE diet. The present study corroborates the inverse relation between BMI and serum CML that was described previously (29). Serum CML may be affected by body fat possibly because CML is preferentially deposited in adipose tissue or because adipocytes affect the metabolism of AGEs (29).
The study is limited in that the AGE content of the experimental diets was estimated using a database for foods that was based on an antibody to CML rather than the gold-standard HPLC analysis (22). Another limitation is that the AGE composition of the individual meals was not measured using HPLC.
A recent review of trials involving AGE-restricted dietary interventions showed that most trials had limited generalizability and involved dietary interventions of <6 wk duration (12). In addition, the majority of trials were undertaken by the same research group, which may have introduced “similar methodologic constraints into the majority of the studies conducted on this topic” (12). Many of the trials had poor methodologic quality because of multiple shortcomings, such as not keeping researchers unaware of treatment, inadequate randomization, no provision of sample size and power calculations for main outcomes, no mention of dropouts or withdrawals from the trials, and lack of an intention-to-treat analysis (12).
The present study showed that a diet high or low in AGEs did not influence circulating inflammatory mediators after 6-wk duration. We were unable to corroborate a previous study in which large changes in serum CRP and VCAM-1 concentrations were found in a small sample of adults with diabetes on a high- or low-AGE diet for 6 wk (16). In the present study, we did not measure plasma TNF-α directly, because TNF-α is relatively labile to storage, handling, and freeze thaw (30). Instead, we measured TNF-α RI and TNF-α RII, which can reflect activity of TNF-α (31). A high- or low-AGE diet had no apparent effect on TNF-α RI and TNF-α RII concentrations.
Circulating RAGE and esRAGE were hypothesized to act as decoy receptors by binding with circulating AGEs and thus prevent direct binding of AGEs with cell-surface RAGE (1). Whether modulation of dietary intake of AGEs would influence circulating RAGE and esRAGE is unknown. The present study suggests that a diet high or low in AGEs did not affect circulating RAGE and esRAGE.
The strengths of the present study include the standardized preparation of meals, the control of food intake during the intervention, the nutritional and dietary equivalence of the 2 types of meals that differed only in the temperature used to process the food, and the 100% follow-up rate. Rigorous randomization was undertaken, both groups were comparable at baseline, strict inclusion and exclusion criteria of participants was followed, and study and laboratory staff involved in data collection were unaware of the dietary allocation. To our knowledge, this is the only rigorous, highly controlled dietary intervention in healthy adults that has measured the effects of chronic consumption of high- or low-AGE diet on markers of cardiovascular disease risk. The findings from this study suggest that consumption of a diet high or low in AGEs does not affect endothelial function and inflammation, 2 precursors of coronary artery atherosclerotic disease. It is also possible that any physiologic processes related to dietary AGEs are slow, small, and not detectable by 6 wk but may have a cumulative health impact over many years. Another possibility is that the effects of high dietary AGEs on endothelial function are only seen in the postprandial rather than fasting state. The rate of clearance of dietary AGEs is not well understood. Studies in rats and humans show that urinary AGE concentrations are significantly correlated with dietary AGE intake (32, 33). Nonetheless, the lack of measurable effect of dietary AGEs in this intervention demonstrates that, if dietary AGEs were to affect inflammation or endothelial function, the impact of AGEs over the longer term is likely at most small. The results of this study cannot necessarily be generalized to other study populations.
In conclusion, to our knowledge, this paper describes the most rigorously conducted study to date on the impact of dietary AGEs on biomarkers of health. The results support minimal if any effect of dietary AGEs on endothelial function and inflammation, 2 important indicators of health and underlining processes of cardiovascular disease that were implicated previously as targets of negative actions of AGEs.
Supplementary Material
Acknowledgments
R.D.S., D.J.B., S.T., L.F., H.A.S., and J.A.N. designed the research; S.K.G., D.J.B., J.A.N., and R.T. conducted the research; D.J.B., J.A.N., L.F., R.D.S., and H.A.S. provided essential materials; K.S. analyzed the data; R.D.S., S.K.G., D.J.B., K.S., R.T., H.A.S., S.T., L.F., and J.A.N. wrote the paper; R.D.S., L.F., and J.A.N. had primary responsibility for the final content. All authors read and approved the final manuscript.
Footnotes
Abbreviations used: AGE, advanced glycation end product; BHNRC, Beltsville Human Nutrition Research Center; CML, carboxymethyl-lysine; CRP, C-reactive protein; esRAGE, endogenous secretory receptor for advanced glycation end product; RAGE, receptor for advanced glycation end product; RHI, reactive hyperemia index; sRAGE, secretory receptor for advanced glycation end product; TNF-α RI, TNF-α receptor I; TNF-α RII, TNF-α receptor II; VCAM-1, vascular cell adhesion molecule-1.
References
- 1.Semba RD, Nicklett EJ, Ferrucci L. Does accumulation of advanced glycation end products contribute to the aging phenotype? J Gerontol A Biol Sci Med Sci. 2010;65:963–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ames JM. Determination of Nε-(carboxymethyl)lysine in foods and related systems. Ann N Y Acad Sci. 2008;1126:20–4. [DOI] [PubMed] [Google Scholar]
- 3.Basta G, Schmidt AM, de Caterina R. Advanced glycation end products and vascular inflammation: implications for accelerated atherosclerosis in diabetes. Cardiovasc Res. 2004;63:582–92. [DOI] [PubMed] [Google Scholar]
- 4.Basta G. Receptor for advanced glycation endproducts and atherosclerosis: from basic mechanisms to clinical implications. Atherosclerosis 2008;196:9–21. [DOI] [PubMed] [Google Scholar]
- 5.Schram MT, Schalkwijk CG, Bootsma AH, Fuller JH, Chaturvedi N, Stehouwer CD; EURODIAB Prospective Complications Study Group. Advanced glycation end products are associated with pulse pressure in type 1 diabetes: the EURODIAB Prospective Complications Study. Hypertension 2005;46:232–7. [DOI] [PubMed] [Google Scholar]
- 6.Baumann M, Richart T, Sollinger D, Pelisek J, Roos M, Kouznetsova T, Eckstein HH, Heemann U, Staessen JA. Association between carotid diameter and the advanced glycation end product N-epsilon-carboxymethyllysine (CML). Cardiovasc Diabetol. 2009;8:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Semba RD, Najjar SS, Sun K, Lakatta EG, Ferrucci L. Serum carboxymethyl-lysine, an advanced glycation end product, is associated with increased aortic pulse wave velocity in adults. Am J Hypertens. 2009;22:74–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kilhovd BK, Juutilainen A, Lehto S, Rönnemaa T, Torjesen PA, Hanssen KF, Laakso M. Increased serum levels of advanced glycation end products predict total, cardiovascular and coronary mortality in women with type 2 diabetes: a population-based 18 year follow-up study. Diabetologia 2007;50:1409–17. [DOI] [PubMed] [Google Scholar]
- 9.Semba RD, Ferrucci L, Sun K, Guralnik JM, Ferrucci L. Advanced glycation end products and their circulating receptors predict cardiovascular disease mortality in older community-dwelling women. Aging Clin Exp Res. 2009;21:182–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Semba RD, Bandinelli S, Sun K, Guralnik JM, Ferrucci L. Plasma carboxymethyl-lysine, and advanced glycation end product, and all-cause and cardiovascular disease mortality in older community-dwelling adults. J Am Geriatr Soc. 2009;57:1874–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pischetsrieder M. (editor). Special issue: Are dietary AGEs/ALEs a health risk? Mol Nutr Food Res. 2007;51:1069–70. [DOI] [PubMed] [Google Scholar]
- 12.Kellow NJ, Savige GS. Dietary advanced glycation end-product restriction for the attenuation of insulin resistance, oxidative stress and endothelial dysfunction: a systematic review. Eur J Clin Nutr. 2013;67:239–48. [DOI] [PubMed] [Google Scholar]
- 13.Koschinsky T, He CJ, Mitsuhashi T, Bucala R, Liu C, Buenting C, Heitmann K, Vlassara H. Orally absorbed reactive glycation products (glycotoxins): an environmental risk factor in diabetic nephropathy. Proc Natl Acad Sci USA 1997;94:6474–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Negrean M, Stirban A, Stratmann B, Gawlowski T, Horstmann T, Götting C, Kleesiek K, Mueller-Roesel M, Koschinsky T, Uribarri J, et al. Effects of low- and high-advanced glycation endproduct meals on macro- and microvascular endothelial function and oxidative stress in patients with type 2 diabetes mellitus. Am J Clin Nutr. 2007;85:1236–43. [DOI] [PubMed] [Google Scholar]
- 15.Uribarri J, Stirban A, Sander D, Cai W, Negrean M, Buenting CE, Koschinsky T, Vlassara H. Single oral challenge by advanced glycation end products acutely impairs endothelial function in diabetic and nondiabetic subjects. Diabetes Care 2007;30:2579–82. [DOI] [PubMed] [Google Scholar]
- 16.Vlassara H, Cai W, Crandall J, Goldberg T, Oberstein R, Dardaine V, Peppa M, Rayfield EJ. Inflammatory mediators are induced by dietary glycotoxins, a major risk factor for diabetic angiopathy. Proc Natl Acad Sci USA 2002;99:15596–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Birlouez-Aragon I, Saavedra G, Tessier FJ, Galinier A, Ait-Ameur L, Lacoste F, Niamba CN, Alt N, Somoza V, Lecerf JM. A diet based on high-heat-treated foods promotes risk factors for diabetes mellitus and cardiovascular diseases. Am J Clin Nutr. 2010;91:1220–6. [DOI] [PubMed] [Google Scholar]
- 18.Gugliucci A, Kotani K, Taing J, Matsuoka Y, Sano Y, Yoshimura M, Egawa K, Horikawa C, Kitagawa Y, Kiso Y, et al. Short-term low calorie diet intervention reduces serum advanced glycation end products in healthy overweight or obese adults. Ann Nutr Metab. 2009;54:197–201. [DOI] [PubMed] [Google Scholar]
- 19.Yoshikawa T, Miyazaki A, Fujimoto S. Decrease in serum levels of advanced glycation end-products by short-term lifestyle modification in non-diabetic middle-aged females. Med Sci Monit. 2009;15:PH65–73. [PubMed] [Google Scholar]
- 20.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- 21.Wu ET, Liang JT, Wu MS, Chang KC. Pyridoxamine prevents age-related aortic stiffening and vascular resistance in association with reduced collagen glycation. Exp Gerontol. 2011;46:482–8. [DOI] [PubMed] [Google Scholar]
- 22.Goldberg T, Cai W, Peppa M, Dardaine V, Baliga BW, Uribarri J, Vlassara H. Advanced glycoxidation end products in commonly consumed foods. J Am Diet Assoc. 2004;104:1287–91. [DOI] [PubMed] [Google Scholar]
- 23.Hamburg NM, Benjamin EJ. Assessment of endothelial function using digital pulse amplitude tonometry. Trends Cardiovasc Med. 2009;19:6–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang X, Frischmann M, Kientsch-Engel R, Steinmann K, Stopper H, Niwa T, Pischetsrieder M. Two immunochemical assays to measure advanced glycation end-products in serum from dialysis patients. Clin Chem Lab Med. 2005;43:503–11. [DOI] [PubMed] [Google Scholar]
- 25.Boehm BO, Schilling S, Rosinger S, Lang GE, Lang GK, Kietsch-Engel R, Stahl P. Elevated serum levels of Nε-carboymethyl-lysine, an advanced glycation end product, are associated with proliferative diabetic retinopathy and macular oedema. Diabetologia 2004;47:1376–9. [DOI] [PubMed] [Google Scholar]
- 26.Warnick GR, Benderson J, Albers J. Dextran sulfate-Mg2+ precipitation procedure for quantification of high-density-lipoprotein cholesterol. Clin Chem. 1982;28:1379–88. [PubMed] [Google Scholar]
- 27.Friedewald WT, Levy RI, Frederikson DS. Estimation of the concentration of low-density-lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 28.Hamburg NM, Keyes MJ, Larson MG, Vasan RS, Schnabel R, Pryde MM, Mitchell GF, Sheffy J, Vita JA, Benjamin EJ. Cross-sectional relations of digital vascular function to cardiovascular risk factors in the Framingham Heart Study. Circulation 2008;117:2467–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Semba RD, Arab L, Sun K, Nicklett EJ, Ferrucci L. Fat mass is inversely associated with serum carboxymethyl-lysine, an advanced glycation end product, in adults. J Nutr. 2011;141:1726–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Flower L, Ahuja RH, Humphries SE, Mohamed-Ali V. Effects of sample handling on the stability of interleukin 6, tumour necrosis factor-alpha and leptin. Cytokine 2000;12:1712–6. [DOI] [PubMed] [Google Scholar]
- 31.Nilsson L, Szymanowski A, Swahn E, Jonasson L. Soluble TNF receptors are associated with infarct size and ventricular dysfunction in ST-elevation myocardial infarction. PLoS One 2013;8:e55477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Förster A, Kühne Y, Henle T. Studies on absorption and elimination of dietary Maillard reaction products. Ann N Y Acad Sci. 2005;1043:474–81. [DOI] [PubMed] [Google Scholar]
- 33.Roncero-Ramos I, Delgado-Andrade C, Tessier FJ, Niquet-Léridon C, Strauch C, Monnier VM, Navarro MP. Metabolic transit of Nε-carboxymethyl-lysine after consumption of AGEs from bread crust. Food Funct. 2013;4:1032–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.