Introduction
Sudden cardiac arrest is a leading cause of death worldwide [1]. Despite advances in cardiopulmonary resuscitation (CPR) methods, including the introduction of the automatic electrical defibrillator (AED) and therapeutic hypothermia [2], [3], only about 10 % of adult out-of-hospital cardiac arrest (OHCA) victims survive to hospital discharge [4], and the majority of survivors have moderate to severe cognitive deficits 3 months after resuscitation [5]. Resuscitation from cardiac arrest is the ultimate whole body ischemia-reperfusion (I/R) injury affecting multiple organ systems including brain and heart [6]. No pharmacological agent is available to im¬prove outcome from post-cardiac arrest syndrome.
Inhaled nitric oxide (NO) has been widely used for the treatment of neonatal hypoxemia with acute pulmonary hypertension. However, accumulating evidence has demonstrated that inhaled NO exerts beneficial effects on I/R injury in extrapulmonary organs without causing hypotension. Along these lines, we recently reported that inhaled NO improved outcomes after cardiac arrest/CPR in mice. This chapter provides insights into the potential salutary effects of inhaled NO in ischemic brain injury associated with sudden cardiac arrest.
Importance of sudden cardiac arrest to public health
Approximately 360,000 Americans experience OHCA each year [4]. In a recent meta-analysis of more than 140,000 patients with OHCA, survival to hospital admis¬sion was 23.8 %, and survival to hospital discharge was only 7.6 % [7]. Densely populated urban areas such as New York, NY, and Chicago, Ill, where a large number of cardiac arrests occur, report even lower (1.4 % to 2 %) survival rates [8],[9]. Unlike other areas of cardiovascular health, such as myocardial infarction (MI) which has seen a 3-fold decrease in acute mortality [10], improve¬ments in outcome from OHCA have remained modest over the last 25 years [11]. Although OHCA is obviously a life-threatening condition, it is a 'treatable disease' in the sense that medical interventions can improve survival significantly [12-14]. A nearly 500 % difference in survival rates exists across communities in the United States, suggesting that variability in the quality of resus¬citation care is driving large differences in community survival rates [15]. Collectively, these data suggest the potential that a major improvement in survival rates could save tens of thousands of lives. Moreover, the financial burden of care of post-arrest patients on society is enormous. A recent estimate suggests that on average it costs $ 102,017 to take care of a patient after OHCA with conventional care (without therapeutic hypother¬mia) [16]. More than $ 33 billion of health care cost is spent on OHCA annually in US.
Pathophysiology and current treatment for post-cardiac arrest syndrome
The greatest proportion of post-cardiac arrest mortality and morbidity is caused by global ischemic brain injury [17]. The mechanisms responsible for post-cardiac arrest brain injury include excitotoxicity, free radical formation, pathological activation of proteases, and cell death signaling [18],[19]. Many of the injurious pathways are executed over hours to days following return of spon¬taneous circulation (ROSC) [20],[21]. While the pro¬tracted time-course of brain injury suggests a broad therapeutic window for neuroprotective strategies following cardiac arrest [19], no pharmacological agents have been proven to be effective in improving neuro¬logical outcomes in post-cardiac arrest patients. Two randomized clinical trials have shown that therapeutic hypothermia confers significant protective effects when applied for 12-24 h after ventricular fibrillation (VF)- induced cardiac arrest in adults [2], [3]. Based on these findings, the American Heart Association 2010 ACLS guidelines gave the highest level of recommendation for the use of hypothermia in comatose patients after OHCA. Currently, mortality at six months after cardiac arrest in patients treated with or without therapeutic hypothermia is 41 % and 55 %, respectively. At six months, 55 % and 39 % of the patients treated with or without therapeutic hypothermia, respectively, have a favorable neurologic outcome. A meta-analysis con¬cluded that the number needed to treat to achieve one additional patient with good neurological outcome was 6 [22]. Although therapeutic hypothermia clearly provides a statistically significant improvement in OHCA patients, the benefit is clinically quite modest [22]. In 40 %-66 % of patients treated with therapeutic hypothermia after cardiac arrest, consciousness never returns [2], [3], [23]. Therefore, additional therapies are urgently needed [6].
Nitric oxide
NO is synthesized from L-arginine by NO synthases (NOS1, NOS2, and NOS3). One of the primary targets of NO is soluble guanylate cyclase (sGC), which generates the second messenger, cGMP, upon activation. sGC is a heme-containing heterodimeric enzyme composed of one α and one β subunit. In most tissues, including heart, lung, and vascular smooth muscle cells, the sGCα1β1 heterodimer is the predominant isoform. NO binds to the heme moiety of sGC and stimulates the synthesis of cGMP [24]. cGMP exerts its effects by interacting with cGMP-dependent protein kinase (PKG), cGMP-regulated phosphodiesterases (PDE), and cGMP-regulated ion channels. Although the biological effects of NO are mainly mediated via a cGMP-dependent mechanism, studies have demonstrated that cGMP-independent signaling plays an important role in diverse aspects of NO signaling. For example, a number of effects of NO are mediated by S-nitrosylation, which is the covalent modification of a protein cysteine thiol (-SH) to generate an S-nitrosothiol (-SNO) by NO [25].
NO/sGC and ischemia-reperfusion injury
NO exerts a variety of effects that would be expected to be beneficial during I/R injury [26]. For example, NO is a potent vasodilator that inhibits platelet and leukocyte activation and adhesion, inhibits reactive oxygen species (ROS)-producing enzymes, and directly scavenges ROS [27]. Deficiency of NOS3 has been shown to aggravate I/R injury in brain and heart [28], [29]. We reported that deficiency of NOS3 or sGCα1 worsened outcomes of cardiac arrest/CPR, whereas cardiomyocyte-specific overexpression of NOS3 rescued NOS3-deficient mice from myocardial and neurological dysfunction and death after cardiac arrest/CPR [30]. Along these lines, Beiser and colleagues reported that poor cardiovascular outcomes and survival in NOS3-deficient mice after cardiac arrest/CPR were associated with decreased myocardial cGMP levels [31].
The salutary effects of NO in I/R appear to be mediated via multiple mechanisms. Dezfulian and colleagues showed that systemic administration of nitrite, which is converted in vivo to NO, improves outcomes in mice 24 h after cardiac arrest/CPR by reducing pathological cardiac mitochondrial oxygen consumption resulting from ROS formation [32]. Systemic administration of nitrite pre¬vented oxidative enzymatic injury via reversible specific inhibition of mitochondrial respiratory chain complex I after cardiac arrest/CPR. cGMP may elicit its cyto- protective effects via protein kinase G (PKG), which, in turn, activates mitochondrial protein kinase Cε via ERK signaling [33]. Recent studies showed that activation of cGMP-PKG-dependent signaling altered the glial inflam¬matory response and decreased oxidative stress and cell death induced by focal brain injury [34].
Inhaled NO and I/R injury
Inhaled NO is a selective pulmonary vasodilator that does not produce systemic hypotension when inhaled at concentrations up to 80 ppm in multiple species, including man [35]. The absence of systemic vasodilation during NO inhalation is due to the rapid scavenging of NO by hemoglobin in the blood. Inhaled NO has been approved for the treatment of neonatal hypoxemia with acute pulmonary hypertension [36]. However, breathing NO also has systemic effects [37]. Breathing NO was shown to reduce I/R injury of extrapulmonary organs in a variety of animal models [38-42]. For example, Hataishi and colleagues examined the ability of breathing NO to decrease cardiac I/R injury in intact mice [40]. They observed that breathing NO for the final 20 minutes of ischemia and for 24 h after reperfusion decreased the size of MI and improved systolic and diastolic function. Breathing 80 ppm NO decreased MI size similarly after 30, 60, or 120 min of ischemia. Breathing 40 and 80 ppm NO decreased myocardial I/R injury to a similar degree, but 20 ppm was not effective. Breathing NO decreased cardiac neutrophil accumulation, and leukocyte deple¬tion prevented the beneficial effects of NO on MI size. Observations in rodents have been extended to a clinically-relevant porcine model of cardiac I/R injury: Liu and colleagues reported that, in pigs subjected to 50 min of cardiac ischemia and 4 h of reperfusion, breathing 80 ppm NO decreased MI size and improved myocardial perfusion [41]. Taken together, these obser¬vations suggest that inhaled NO exerts beneficial effects on I/R and protects extrapulmonary organs from I/R injury in small and large mammals.
The ability of inhaled NO to reduce I/R injury was subsequently reproduced in 'proof-of-concept' human studies [43-45]. Lang and colleagues reported a prospective, blinded, placebo-controlled study that demonstrated that 80 ppm NO inhalation during liver transplantation prevented hepatic I/R injury after transplantation. The investigators observed significantly decreased hospital length of stay, serum transaminases, coagulation times, and hepatic apoptosis after liver transplantation [43]. Gianetti and colleagues reported that breathing 20 ppm NO during and after cardio¬pulmonary bypass decreased myocardial injury and left ventricular dysfunction in patients undergoing aortic valve replacement via anti-inflammatory properties [44]. Mathru and colleagues reported that breathing 80 ppm NO reduced I/R induced inflammatory injury in patients undergoing knee surgery [45]. Based on these obser¬vations, we hypothesized that NO inhalation could improve outcomes after cardiac arrest/CPR.
Inhaled NO improves outcomes after cardiac arrest and CPR in mice
To examine the effects of NO inhalation on the outcome of cardiac arrest/CPR in a clinically relevant manner, we developed and thoroughly characterized a murine model of cardiac arrest/CPR, in which mice exhibit poor neurological outcomes and survival rates after successful resuscitation from cardiac arrest [30], [46-48]. Briefly, after instrumentation under general anesthesia, cardiac arrest was induced by an intravenous injection of potassium chloride (KCl). After 7.5 min of arrest time, chest compressions were delivered with a finger at a rate of 300-350 per minute with resumption of mechanical ventilation (FiO2 = 1.0) and continuous intravenous infusion of epinephrine. Mice were weaned from mechanical ventilation and extubated at 1 h after CPR. Mice were then randomized to breath air with or without 40 ppm NO for 23 h in custom-made chambers. Whereas only 4 out of 13 mice that breathed air alone survived 10 days after CPR, 11 out of 13 mice that breathed air combined with NO survived for 10 days (p = 0.003, Figure 1).
Figure 1.
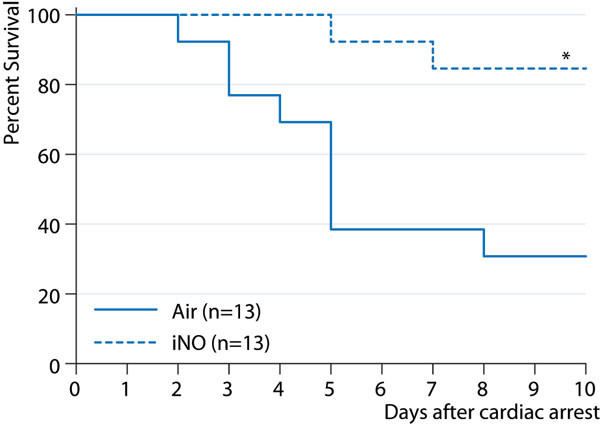
Survival rate of wild-type mice during the first 10 days after cardiac arrest and CPR. Air: mice breathed air for 23 hours starting 1 hour after CPR; iNO: mice breathed air supplemented with NO for 23 hours starting 1 hour after CPR. * p = 0.003 vs. air.
It is increasingly recognized that post-cardiac arrest care after ROSC can improve the likelihood of patient survival with good neurological function. Clinical trials showed that therapeutic hypothermia conferred neuroprotective effects when it was applied for 12-24 h starting minutes to hours after successful CPR from cardiac arrest due to ventricular fibrillation [2], [3]. The apparent presence of a temporal therapeutic window after successful CPR is consistent with the observations that many of the pathogenetic mechanisms responsible for post-cardiac arrest brain injury are executed over hours to days following ROSC [18-21]. The protective effects of breathing NO for 23 h beginning 1 h after successful CPR further support the notion that outcomes from sudden cardiac arrest can be improved by implementing innovative therapies in the post-cardiac arrest 'golden hours' after successful CPR.
Mice that breathed air alone exhibited a marked abnormality in water diffusion in the hippocampus, caudoputamen, and cortex 24 h after CPR (Figure 2). The presence of abnormal diffusion-weighted imaging (DWI) signals in the vulnerable regions of the brain 24 h after cardiac arrest/CPR correlated with worse neurological function and increased apoptosis of hippocampal neurons 4 days after CPR, as well as a poor survival rate. In contrast, NO breathing markedly attenuated the development of abnormality in water diffusion in the brain and improved neurological outcomes and survival rate. These observations are consistent with a recent clinical study that showed that diffuse cortical abnor¬malities in DWI were associated with poor outcomes in patients resuscitated from cardiac arrest [49]. Hyper¬intense DWI signals indicate the presence of brain edema, presumably due to disruption of ion pump function and membrane failure. Therefore, these obser¬vations suggest that NO inhalation after successful CPR can preserve ion pump homeostasis and membrane integrity early after cardiac arrest/CPR.
Figure 2.
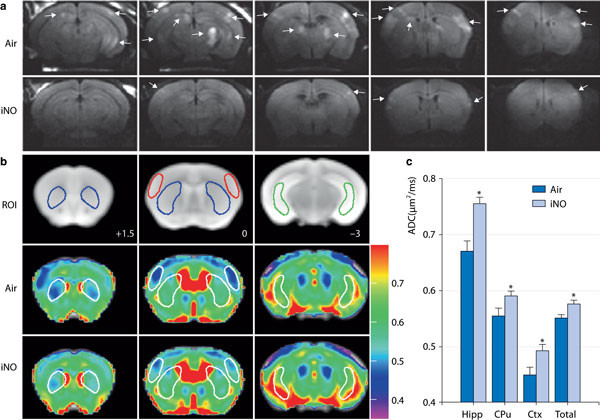
a Representative diffusion weighted image (DWI) of brain in mice that breathed air (Air) or air supplemented with NO (iNO). White arrows indicate areas of hyperintense DWI. b Representative magnetic resonance images showing three brain slices containing regions of interest (ROI). Slice positions are identified in millimeters (+1.5, 0, or 3 mm) with respect to bregma in the coordinate space of the Allen Mouse Brain Atlas. Colored outlines indicate portions of ROI (blue: caudoputamen; red: lateral cortex; green: ventral lateral hippocampus) that intersect with these slice planes. Average apparent diffusion coefficient (ADC) values of the slice plane for mice that breathed air (Air) or NO (iNO) after cardiac arrest and cardiopulmonary resuscitation (CPR). The color bar on the right side indicates the color-code for the ADC values (μm2/ms). c Average ADC values of each three-dimensional ROI (Hipp: ventral lateral hippocampus; CPu: caudoputamen; Ctx: lateral cortex; Total: total brain) across all planes in mice that breathed air (Air, n = 6) or NO (iNO, n = 7) after cardiac arrest and CPR. p < 0.05 vs. Air.
Neuroinflammation induced by the whole body I/R injury associated with cardiac arrest/CPR hinders the neurological recovery from cardiac arrest. We observed that cardiac arrest/CPR markedly upregulated the expression of genes encoding inflammatory cytokines and NADPH oxidase in the brain of mice that breathed air alone, but not in mice that breathed air combined with NO. These observations suggest that NO inhalation prevents neuroinflammation after cardiac arrest/CPR. Furthermore, these results demonstrate a correlation between neuroinflammation, neurological dysfunction, and mortality after resuscitation.
NO elicits biological effects via sGC-dependent and/or independent mechanisms. To examine the role of sGC in the beneficial effects of inhaled NO on outcomes after resuscitation, sGCα1-/- mice were subjected to cardiac arrest/CPR. We observed that sGCαl-deficiency abolished the ability of inhaled NO to prevent induction of inflammatory cytokines in the brain and to improve neurological function and 10-day survival rate after resuscitation [48]. These observations suggest that bene¬ficial effects of inhaled NO on outcomes after cardiac arrest/CPR are largely mediated via sGC-dependent mechanisms.
Inhaled NO may exert systemic effects via interaction with circulating bone marrow-derived cells (e. g., leuko¬cytes) as they transit lungs. We previously reported that neutrophils are required for inhaled NO to reduce MI size in wild-type (WT) mice subjected to transient left coronary artery occlusion [40]. Along these lines, we recently observed that NO breathing markedly decreased MI size in WT but not in sGCα1-/- mice [50]. Furthermore, breathing NO decreased MI size in chimeric sGCα1-/- mice carrying WT bone marrow generated by bone marrow transplantation. These results raise the possibility that the neuroprotective effects of inhaled NO after cardiac arrest/CPR may be mediated by bone marrow-derived cells in a sGC-dependent manner.
From the viewpoint of translating our results into clinical benefit, it is of particular importance that NO inhalation started 1 h after CPR can improve neurological and myocardial function and survival rate after cardiac arrest and CPR. Although the therapeutic window in humans remains to be determined, our observations suggest that inhaled NO can be started after patients are transported to the hospital, and informed consent is obtained. To date, therapeutic hypothermia is the only therapeutic approach that has been proved to improve outcomes after cardiac arrest/CPR when applied hours after successful CPR [2], [3]. Since the body temperature of the mice was allowed to decrease to ~ 30 °C in the early period after CPR in our recent study, these obser¬vations raise the possibility that inhaled NO may confer additional protective effects in the setting of mild hypothermia. Nonetheless, whether inhaled NO com¬bined with therapeutic hypothermia further improves outcomes after cardiac arrest/CPR compared to mice treated with therapeutic hypothermia alone remains to be formally determined in future studies.
Conclusions
Although mounting evidence suggests that NO¬dependent signaling exerts multi-faceted protection against I/R injury, the vasodilating effects of systemically- administered NO-donor compounds preclude their use in post-cardiac arrest patients with unstable blood pressure. Based upon our prior studies of the beneficial effects of breathing NO on cardiac I/R injury, which were not associated with systemic hypotension [40], we tested the hypothesis that breathing NO could improve outcomes after cardiac arrest/CPR. We observed that breathing NO beginning 1 h after ROSC markedly improved neurological and myocardial function, as well as survival at 10 days without causing hypotension. Of note, the protective effects of inhaled NO in I/R injury of remote organs were first demonstrated in small animals [38], [39] and then later confirmed in patients [43-45], suggesting that the beneficial effects of inhaled NO in mice subjected to cardiac arrest/CPR are likely to be readily translated to benefit patients. Moreover, the established safety profile of NO inhalation (including FDA approval in 1999 for babies with hypoxic respiratory failure and pulmonary hypertension) further enhances the probability that observations in animal models will be rapidly translatable to patients with post-cardiac arrest syndrome.
List of abbreviations used
AED: automatic electrical defibrillator; CPR: cardiopulmonary resuscitation; DWI: diffusion-weighted imaging; I/R: ischemia-reperfusion; NO: nitric oxide; NOS: NO synthase; OHCA: out-of-hospital cardiac arrest; PDE: phospodiesterases; PKG: protein kinase G; ROS: reactive oxygen species; ROSC: return of spontaneous circulation; sGC: soluble guanylate cyclise; VF: ventricular fibrillation; WT: wild-type.
Competing interests
Dr Ichinose has received a sponsored research agreement from Ikaria, Inc that makets inhaled NO (INOMAX) in the US.
Declarations
Publication of this work was supported by postdoctoral fellowships from the American Heart Association's Founders Affiliate and from the Massachusetts General Hospital Tosteson Fund for Medical Discovery to KK, R01 grants from the NHLBI (HL101930 and HL110378 to FI), and a sponsored research agreement from IKARIA Inc. to FI.
Contributor Information
Kotaro Kida, Email: kkida@mgh.harvard.edu.
Fumito Ichinose, Email: fichinose@partners.org.
References
- Field JM, Hazinski MF, Sayre MR, Chameides L, Schexnayder SM, Hemphill R, Samson RA, Kattwinkel J, Berg RA, Bhanji F, Cave DM, Jauch EC, Kudenchuk PJ, Neumar RW, Peberdy MA, Perlman JM, Sinz E, Travers AH, Berg MD, Billi JE, Eigel B, Hickey RW, Kleinman ME, Link MS, Morrison LJ, O-Connor RE, Shuster M, Callaway CW, Cucchiara B, Ferguson JD, Rea TD, Vanden Hoek TL. Part 1: Executive Summary: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S640–S656. doi: 10.1161/CIRCULATIONAHA.110.970889. [DOI] [PubMed] [Google Scholar]
- Bernard SA, Gray TW, Buist MD, Jones BM, Silvester W, Gutteridge G, Smith K. Treatment of comatose survivors of out-of-hospital cardiac arrest with induced hypothermia. N Engl J Med. 2002;346:557–563. doi: 10.1056/NEJMoa003289. [DOI] [PubMed] [Google Scholar]
- Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–556. doi: 10.1056/NEJMoa012689. [DOI] [PubMed] [Google Scholar]
- Go AS, Mozaffarian D, Roger V, Benjamin EJ, Berry JD, Bodren WBm, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard Vj, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtmar JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. American Heart Association Statistics Committee and Stroke Statistics Subcommittee: Heart Disease and Stroke Statistics-2013 Update: A report from the American Heart Association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roine RO, Kajaste S, Kaste M. Neuropsychological sequelae of cardiac arrest. JAMA. 1993;269:237–242. doi: 10.1001/jama.1993.03500020071034. [DOI] [PubMed] [Google Scholar]
- Peberdy MA, Callaway CW, Neumar RW, Geocardin RG, Zimmerman JL, Donníno M, Gabrielli A, Silvers SM, Zaritsky AL, Merchant R, Vanden Hoek TL, Kronick SL. American Heart Association. Part 9: Post-Cardiac Arrest Care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S768–S786. doi: 10.1161/CIRCULATIONAHA.110.971002. [DOI] [PubMed] [Google Scholar]
- Sasson C, Rogers MAM, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: A systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- Lombardi G, Gallagher J, Gennis P. Outcome of out-of-hospital cardiac arrest in New York City. The Pre-Hospital Arrest Survival Evaluation (PHASE) Study. JAMA. 1994;271:678–683. doi: 10.1001/jama.1994.03510330056034. [DOI] [PubMed] [Google Scholar]
- Becker LB, Ostrander MP, Barrett J, Kondos GT. Outcome of CPR in a large metropolitan area - where are the survivors? Ann Emerg Medicine. 1991;20:355–361. doi: 10.1016/S0196-0644(05)81654-3. [DOI] [PubMed] [Google Scholar]
- Heidenreich PA, McClellan M. Trends in treatment and outcomes for acute myocardial infarction 1975-1995. Am J Med. 2011;110:165–174. doi: 10.1016/s0002-9343(00)00712-9. [DOI] [PubMed] [Google Scholar]
- Weil MH, Becker L, Budinger T, Kern K, Nichol G, Shechter I, Traystman R, Wiedemann H, Wise R, Weisfeldt M, Sopko G. Workshop Executive Summary Report: Post-Resuscitative and Initial Utility in Life Saving Efforts (PULSE) Circulation. 2001;103:1182–1184. doi: 10.1161/01.CIR.103.9.1182. [DOI] [PubMed] [Google Scholar]
- Cobb LA, Fahrenbruch CE, Walsh TR. Influence of cardiopulmonary resuscitation prior to defibrillation in patients with out-of-hospital ventricular fibrillation. JAMA. 1999;281:1182–1188. doi: 10.1001/jama.281.13.1182. [DOI] [PubMed] [Google Scholar]
- Hallstrom AP, Ornato JP, Weisfeldt M, Travers A, Christenson J, McBurnie MA, Zalenski R, Becker LB, Schron EB, Proschan M. Public Access Defibrillation Trial Investigators. Public-access defibrillation and survival after out-of-hospital cardiac arrest. N Engl J Med. 2004;351:637–646. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- Bobrow BJ, Clark LL, Ewy GA. Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. JAMA. 2008;299:1158–1165. doi: 10.1001/jama.299.10.1158. [DOI] [PubMed] [Google Scholar]
- Nichol G, Thomas E, Callaway CW. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA. 2008;300:1423–1431. doi: 10.1001/jama.300.12.1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merchant RM, Becker LB, Abella BS, Asch DA, Groeneveld PW. Cost- effectiveness of therapeutic hypothermia after cardiac arrest. Circ Cardiovasc Qual Outcomes. 2009;2:421–428. doi: 10.1161/CIRCOUTCOMES.108.839605. [DOI] [PubMed] [Google Scholar]
- Laver S, Farrow C, Turner D, Nolan J. Mode of death after admission to an intensive care unit following cardiac arrest. Intensive Care Med. 2004;30:2126–2128. doi: 10.1007/s00134-004-2425-z. [DOI] [PubMed] [Google Scholar]
- Neumar RW. Molecular mechanisms of ischemic neuronal injury. Ann Emerg Med. 2000;36:483–506. doi: 10.1067/mem.2000.110995. [DOI] [PubMed] [Google Scholar]
- Neumar RW, Nolan JP, Adrie C, Aibiki M, Berg RA, Bottiger BW, Callaway C, Clark RS, Geocadin RG, Jauch EC, Kern KB, Laurent I, Longstreth WT Jr, Merchant RM, Morley P, Morrison LJ, Nadkarni V, Peberdy MA, Rivers EP, Rodriguez-Nunez A, Sellke FW, Spaulding C, Sunde K, Vanden Hoek T. Post¬cardiac arrest syndrome: Epidemiology, pathophysiology, treatment and prognostication. A Consensus Statement From the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on ResuscitationEuropean Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation. 2008;118:2452–2483. doi: 10.1161/CIRCULATIONAHA.108.190652. [DOI] [PubMed] [Google Scholar]
- Sharma H, Miclescu A, Wiklund L. Cardiac arrest-induced regional blood- brain barrier breakdown, edema formation and brain pathology: a light and electron microscopic study on a new model for neurodegeneration and neuroprotection in porcine brain. J Neural Transm. 2011;118:87–114. doi: 10.1007/s00702-010-0486-4. [DOI] [PubMed] [Google Scholar]
- Fujioka M, Taoka T, Matsuo Y, Mishima K, Ogoshi K, Kondo Y, Tsuda M, Fujiwara M, Asano T, Sakaki T, Miyasaki A, Park D, Siesjo BK. Magnetic resonance imaging shows delayed ischemic striatal neurodegeneration. Ann Neurol. 2003;54:732–747. doi: 10.1002/ana.10751. [DOI] [PubMed] [Google Scholar]
- Holzer M, Bernard SA, Hachimi-Idrissi S, Roine RO, Sterz F, Müllner M. Collaborative Group on Induced Hypothermia for Neuroprotection After Cardiac Arrest. Hypothermia for neuroprotection after cardiac arrest: Systematic review and individual patient data meta-analysis. Crit Care Med. 2005;33:414–418. doi: 10.1097/01.CCM.0000153410.87750.53. [DOI] [PubMed] [Google Scholar]
- Bouwes A, Binnekade JM, Zandstra DF, Koelman JH, van Schaik IN, Hijdra A, Horn J. Somatosensory evoked potentials during mild hypothermia after cardiopulmonary resuscitation. Neurology. 2009;73:1457–1461. doi: 10.1212/WNL.0b013e3181bf98f4. [DOI] [PubMed] [Google Scholar]
- Friebe A, Koesling D. Regulation of nitric oxide-sensitive guanylyl cyclase. CircRes. 2003;93:96–105. doi: 10.1161/01.RES.0000082524.34487.31. [DOI] [PubMed] [Google Scholar]
- Lima B, Forrester MT, Hess DT, Stamler JS. S-nitrosylation in cardiovascular signaling. Circ Res. 2010;106:633–646. doi: 10.1161/CIRCRESAHA.109.207381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloch KD, Ichinose F, Roberts JD, Zapol WM. Inhaled NO as a therapeutic agent. Cardiovasc Res. 2007;75:339–348. doi: 10.1016/j.cardiores.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kubes P, Suzuki M, Granger DN. Nitric oxide: an endogenous modulator of leukocyte adhesion. Proc Natl Acad Sci USA. 1991;88:4651–4655. doi: 10.1073/pnas.88.11.4651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones SP, Girod WG, Palazzo AJ, Granger DN, Grisham MB, Jourd'Heuil D, Huang PL, Lefer DJ. Myocardial ischemia-reperfusion injury is exacerbated in absence of endothelial cell nitric oxide synthase. Am J Physiol. 1999;276:H1567–H1573. doi: 10.1152/ajpheart.1999.276.5.H1567. [DOI] [PubMed] [Google Scholar]
- Huang Z, Huang PL, Ma J, Meng W, Ayata C, Fishman MC, Moskowitz MA. Enlarged infarcts in endothelial nitric oxide synthase knockout mice are attenuated by nitro-l-arginine. J Cereb Blood Flow Metab. 1996;16:981–987. doi: 10.1097/00004647-199609000-00023. [DOI] [PubMed] [Google Scholar]
- Nishida T, Yu JD, Minamishima S, Sips PY, Searles RJ, Buys ES, Janssens S, Brouckaert P, Bloch KD, Ichinose F. Protective effects of nitric oxide synthase 3 and soluble guanylate cyclase on the outcome of cardiac arrest and cardiopulmonary resuscitation in mice. Crit Care Med. 2009;37:256–262. doi: 10.1097/CCM.0b013e318192face. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beiser DG, Orbelyan GA, Inouye BT, Costakis JG, Hamann KJ, McNally EM, Vanden Hoek TL. Genetic deletion of NOS3 increases lethal cardiac dysfunction following mouse cardiac arrest. Resuscitation. 2011;82:115–121. doi: 10.1016/j.resuscitation.2010.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dezfulian C, Shiva S, Alekseyenko A, Pendyal A, Beiser DG, Munasinghe JP, Anderson SA, Chesley CF, Vanden Hoek TL, Gladwin MT. Nitrite therapy after cardiac arrest reduces reactive oxygen species generation improves cardiac and neurological function and enhances survival via reversible inhibition of mitochondrial complex I. Circulation. 2009;120:897–905. doi: 10.1161/CIRCULATIONAHA.109.853267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ping P, Zhang J, Cao X, Li RC, Kong D, Tang XL, Qiu Y, Manchikalapudi S, Auchampach JA, Black RG, Bolli R. PKC-dependent activation of p44/p42 MAPKs during myocardial ischemia-reperfusion in conscious rabbits. Am J Physiol. 1999;276:H1468–H1481. doi: 10.1152/ajpheart.1999.276.5.H1468. [DOI] [PubMed] [Google Scholar]
- Pifarré P, Prado J, Giralt M, Molinero A, Hidalgo J, Garcia A. Cyclic GMP phosphodiesterase inhibition alters the glial inflammatory response reduces oxidative stress and cell death and increases angiogenesis following focal brain injury. J Neurochem. 2010;112:807–817. doi: 10.1111/j.1471-4159.2009.06518.x. [DOI] [PubMed] [Google Scholar]
- Ichinose F, Roberts JD Jr, Zapol WM. Inhaled nitric oxide: a selective pulmonary vasodilator: current uses and therapeutic potential. Circulation. 2004;109:3106–3111. doi: 10.1161/01.CIR.0000134595.80170.62. [DOI] [PubMed] [Google Scholar]
- Griffiths MJ, Evans TW. Inhaled nitric oxide therapy in adults. N Engl J Med. 2005;353:2683–2695. doi: 10.1056/NEJMra051884. [DOI] [PubMed] [Google Scholar]
- Hogman M, Frostell C, Arnberg H, Hedenstierna G. Bleeding time prolongation and NO inhalation. Lancet. 1993;341:1664–1665. doi: 10.1016/0140-6736(93)90802-n. [DOI] [PubMed] [Google Scholar]
- Fox-Robichaud A, Payne D, Hasan SU, Ostrovsky L, Fairhead T, Reinhardt P, Kubes P. Inhaled NO as a viable antiadhesive therapy for ischemia/ reperfusion injury of distal microvascular beds. J Clin Invest. 1998;101:2497–2505. doi: 10.1172/JCI2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guery B, Neviere R, Viget N, Foucher C, Fialdes P, Wattel F, Beaucaire G. Inhaled NO preadministration modulates local and remote ischemia- reperfusion organ injury in a rat model. J Appl Physiol. 1999;87:47–53. doi: 10.1152/jappl.1999.87.1.47. [DOI] [PubMed] [Google Scholar]
- Hataishi R, Rodrigues AC, Neilan TG, Morgan JG, Buys E, Shiva S, Tambouret R, Jassal DS, Raher MJ, Furutani E, Ichinose F, Gladwin MT, Rosenzweig A, Zapol WM, Picard MH, Bloch KD, Scherrer-Crosbie M. Inhaled nitric oxide decreases infarction size and improves left ventricular function in a murine model of myocardial ischemia-reperfusion injury. Am J Physiol Heart Circ Physiol. 2006;291:H379–H384. doi: 10.1152/ajpheart.01172.2005. [DOI] [PubMed] [Google Scholar]
- Liu X, Huang Y, Pokreisz P, Vermeersch P, Marsboom G, Swinnen M, Verbeken E, Santos J, Pellens M, Gillijns H, Van de Werf F, Bloch KD, Jannssens S. Nitric oxide inhalation improves microvascular flow and decreases infarction size after myocardial ischemia and reperfusion. J Am Coll Cardiol. 2007;50:808–817. doi: 10.1016/j.jacc.2007.04.069. [DOI] [PubMed] [Google Scholar]
- Nagasaka Y, Fernandez BO, Garcia-Saura MF, Petersen B, Ichinose F, Bloch KD, Feelisch M, Zapol WM. Brief periods of nitric oxide inhalation protect against myocardial ischemia-reperfusion injury. Anesthesiology. 2008;109:675–682. doi: 10.1097/ALN.0b013e318186316e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang JD Jr, Chumley P, Teng X, Chumley P, Crawford JH, Isbell TS, Chacko BK, Liu Y, Jhala N, Crowe DR, Smith AB, Cross RC, Frenette L, Kelley EE, Wilhite DW, Hall CR, Page GP, Fallon MB, Bynon JS, Eckhoff DE, Patel RP. Inhaled NO accelerates restoration of liver function in adults following orthotopic liver transplantation. J Clin Invest. 2007;117:2583–2591. doi: 10.1172/JCI31892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianetti J, Del Sarto P, Bevilacqua S, Vassalle C, De Filippis R, Kacila M, Farneti PA, Clerico A, Glauber M, Biagini A. Supplemental nitric oxide and its effect on myocardial injury and function in patients undergoing cardiac surgery with extracorporeal circulation. J Thorac Cardiovasc Surg. 2004;127:44–50. doi: 10.1016/j.jtcvs.2002.08.001. [DOI] [PubMed] [Google Scholar]
- Mathru M, Huda R, Solanki DR, Hays S, Lang JD. Inhaled nitric oxide attenuates reperfusion inflammatory responses in humans. Anesthesiology. 2007;106:275–282. doi: 10.1097/00000542-200702000-00015. [DOI] [PubMed] [Google Scholar]
- Kida K, Minamishima S, Wang H, Ren J, Yigitkanil K, Nozari A, Mandeville JB, Liu PK, Liu CH, Ichinose F. Sodium sulfide prevents water diffusion abnormality in the brain and improves long term outcome after cardiac arrest in mice. Resuscitation. 2012;83:1292–1297. doi: 10.1016/j.resuscitation.2012.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minamishima S, Bougaki M, Sips PY, Yu JD, Minamishima YA, Elrod JW, Lefer DJ, Bloch KD, Ichinose F. Hydrogen sulfide improves survival after cardiac arrest and cardiopulmonary resuscitation via a nitric oxide synthase 3-dependent mechanism in mice. Circulation. 2009;120:888–896. doi: 10.1161/CIRCULATIONAHA.108.833491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minamishima S, Kida K, Tokuda K, Wang H, Sips PY, Kosugi S, Mandeville JB, Buys ES, Brouckaert P, Liu PK, Liu CH, Bloch KD, Ichinose F. Inhaled nitric oxide improves outcomes after successful cardiopulmonary resuscitation in mice. Circulation. 2011;124:1645–1653. doi: 10.1161/CIRCULATIONAHA.111.025395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wijman cardiac arrest. Mlynash M, Caulfield AF, Hsia AW, Eyngorn I, Bammer R, Rischbein N, Albers GW, Moseley M. Prognostic value of brain diffusion- weighted imaging after cardiac arrest. Ann Neurol. 2009;65:394–402. doi: 10.1002/ana.21632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagasaka Y, Buys E, Spagnolli E, Steinbecker AU, Hayton SR, Rauwerdink KM, Brouckaert P, Zapol WM, Bloch KD. Soluble guanylate cyclase-α1 is required for the cardioprotective effects of inhaled nitric oxide. Am J Physiol Heart Circ Physiol. 2011;300:H1477–H1483. doi: 10.1152/ajpheart.00948.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]


