Abstract
First-degree relatives (FDRs) of melanoma survivors are at heightened risk for developing melanoma, but sporadically use sun protection. To develop appropriate interventions, in this article we identify factors related to sun protection inconsistency in melanoma FDRs using ethnographic decision tree modeling. We conducted in-home interviews with 25 melanoma FDRs balanced across gender and sunbathing attitudes and identified factors related to daily decision making about use of sunscreen, shade seeking, hats, and clothing. Results indicated primary facilitators for sun protection involved water settings and sunny weather. Physical activities such as exercise served to promote as well as inhibit sun protection. If participants anticipated shade cover, they tended to forgo other sun protection. The use of hats and clothing was often dictated by non-sun protection goals. Understanding factors related to inconsistent sun protection with detail and nuance is an important prerequisite to interventions aimed to improve sun protection maintenance in this population.
Keywords: behavior change, cancer, decision making, ethnography, risk, behaviors
Melanoma accounts for about 70% of skin cancer deaths each year, making it the most fatal form of skin cancer (American Cancer Society [ACS], 2010). Ultraviolet radiation delivered via sunlight is the predominant modifiable cause of melanoma, with approximately 65% to 90% of melanomas caused by sun exposure (Armstrong & Kricker, 1993; Dal, Boldemann, & Lindelof, 2007; Thomas et al., 2007; Whiteman, Whiteman, & Green, 2001). As such, general population skin cancer risk reduction recommendations include consistent sun protection strategies such as sun avoidance in the middle of the day when ultraviolet exposure is the highest, use of hats and long-sleeved clothing to block exposure, and the use of sunscreen on exposed body parts (ACS, 2010; Centers for Disease Control and Prevention [CDCP], 2011; Green, Williams, Logan, & Strutton, 2011). Those at increased risk for melanoma include those with a first-degree family history (i.e., biological parent, sibling, or child; Ford et al., 1995), or a sun-sensitive phenotype, including light skin and eyes, red hair, or the presence of many moles with irregular borders or coloring (Tucker et al., 1997).
In addition to cumulative sun exposure, diverse patterns of sun protection might result in different levels of melanoma risk. For example, Kricker and colleagues (2007) found that individuals exposed to intermittent or recreational sun exposure had much higher risk than those exposed to chronic occupational exposure. Furthermore, melanoma risk can be substantially increased by inconsistent sun protection that results in even a few sunburns (Armstrong & Kricker, 2001; Gandini et al., 2005; Kricker et al., 2007). However, current widely used self-report assessments of sun protection behavior, including the National Health Interview Survey (Coups, Manne, & Heckman, 2008) and the Behavioral Risk Factor Surveillance System (CDCP, 2007) are based on global self-report assessments (e.g., sometimes or most of the time using sunscreen while outside on a sunny day) and are not designed to assess patterns of sun protection. Using these global self-report methods, irregular sun protection is the norm for individuals with a family history of melanoma (Azzarello, Dessureault, & Jacobsen, 2006; Bishop et al., 2007; Geller et al., 2003; Geller et al., 2006; Manne et al., 2004). For instance, Azzarello and colleagues (2006) found that 47% of first-degree relatives of melanoma survivors used sunscreen on their face inconsistently and 71% sought shade inconsistently (e.g., rarely, sometimes, often, or more than half the time). Geller and colleagues (2003) found that 46% of siblings of melanoma survivors did not regularly use sunscreen.
Geller and colleagues (2006) conducted a randomized trial with melanoma siblings to test whether tailored educational materials and multiple health educator telephone motivational interviewing sessions could improve siblings' skin cancer risk reduction practices over 1 year. Risk reduction strategies included sunscreen use of sunburn protection factor (SPF) 15 or higher during periods of summer sun exposure of 15 minutes or longer. SPF is a measure of the effectiveness of sunscreen and represents the amount of ultraviolet radiation necessary to cause sunburn on protected skin as a multiple of the amount required to produce sunburn on unprotected skin (U.S. Food and Drug Administration [FDA], 2009). During the counseling calls the health educator asked siblings to share their personal barriers to improving their skin screening and sunscreen use practices, and then provided constructive ways to address each barrier. One year later, 30% of siblings in control as well as treatment groups used sunscreen sporadically or not at all, indicating no intervention effect.
In a recent study Manne and colleagues (2010) found that an intervention tailored to first-degree family members' skin cancer cognitions was useful in improving their sun protection over the course of 1 year, yet on average sun protection remained less than consistent even in the intervention group (mean= 3.4, where 1 = never, 3 = sometimes, and 5 = always). Understanding sun protection patterns with detail and nuance, as well as the facilitators and barriers to these patterns, is an important prerequisite to improving the effectiveness of intervention strategies that aim to enhance sun protection consistency through the development of habitual behaviors across sun exposure contexts.
In the current study we used ethnographic decision tree modeling (EDTM; Beck, 2005; Gladwin, 1989), a qualitative approach used to describe and predict decision-making processes in real-world settings. This methodology has been used in anthropology and psychology for 25 years to model decisions such as medical treatment decision making (Weller, Ruebush, & Klein, 1997; Young, 1980), needle-sharing decisions among drug users (Johnson & Williams, 1993), and the decision to recycle beverage cans (Ryan & Bernard, 2006). Accordingly, our research aim involved the identification of facilitators and barriers related to daily decision making regarding the use of sun protection (sunscreen use of at least SPF 15, shade seeking, hats, and sun protective clothing such as long-sleeved shirts or pants) in melanoma FDRs. In the next phase of our research we will validate the facilitators and barriers quantitatively using ecological momentary assessment methods among a separate sample of 60 melanoma FDRs. The validation of sun protection facilitators and barriers reported in this article will enable development of predictive models and intervention strategies to address inconsistency in sun protection in those at risk for developing melanoma.
Methods
Guided by decision-making theory, EDTM is based on the assumption that individuals make everyday decisions through a serial consideration of factors that maximize outcomes subject to constraints, and that these simplifying rules serve to reduce the cognitive demand of decisions (Lancaster, 1966; Tversky, 1972). A belief that decision makers, rather than external parties, are best positioned to explain how they make behavioral decisions also represents a guiding principle of EDTM (Gladwin, 1989). A central goal of EDTM is to identify decision criteria that contain “emic” categories that hold meaning to decision makers through ethnographic techniques (Spradley, 1979).
Sample
We recruited melanoma FDRs through referrals from melanoma survivors who were treated at a large metropolitan comprehensive cancer center. Eligible FDRs were English-fluent, age 18 or older, reported at least some use of sun protection, and had to affirm that they could recall two separate periods when they were out in the sun for 60 minutes or longer during the prior summer. It was imperative that FDRs reported some prior use of sun protection because we wanted to uncover decision factors that led to both use and non-use of sun protection. We would not have been able to explore variation in sun protection use if FDRs never used sun protection at all. We excluded FDRs under age 18 because of limited resources; future work will include children. Participants also needed to live within a 50-mile radius of the study site to ensure feasible home visits for the interviews. Our research was approved by our institution's Institutional Review Board.
Recruitment Strategy
We approached melanoma survivors at their postsurgical follow-up appointments. With the approval of each survivor's physician, a research study assistant (RSA) described the study to survivors, provided them with a study brochure, and requested survivors' permission to contact their potentially eligible FDRs. If the FDR was present at the clinic, the RSA assessed interest and eligibility in person. If referred FDRs were not present in clinic, the RSA reached out to them by telephone if the survivor agreed to this approach. Over the course of 4 months of recruitment, we approached 179 melanoma survivors in clinic, 70 of whom referred a total of 80 FDRs. From this pool, 15 FDRs (19%) were deemed ineligible, 9 (11%) were not able to be contacted, 3 (4%) had scheduling conflicts preventing their participation, 9 (11%) refused to participate, and 19 (24%) were not screened because we had already attained our targeted sample size of 25 FDRs. The most common reasons FDRs cited for study refusal were lack of interest in the study and being too busy to participate.
We utilized an a priori purposive sampling strategy (Strauss & Corbin, 1998) where we recruited equal numbers of men and women, and equal numbers of those with higher versus lower perceived advantages of sunbathing within each gender group, to increase the chances that a wide range of decision factors and sun exposure contexts would be elicited. To identify potential participants' perceived advantages of sunbathing within each gender group, we used a 7-item questionnaire (Jackson & Aiken, 2000) of individuals' beliefs concerning advantages of sunbathing. We designated participants scoring above the mean (4.0) identified in prior research as perceiving advantages of sunbathing, and those scoring below the mean as not perceiving advantages of sunbathing for the purposes of stratification assignment. We then recruited equal numbers of participants who scored above and below the reported mean for this scale. Participants included 6 men who reported high perceived advantages of sunbathing, 7 men who reported low perceived advantages of sunbathing, 6 women who reported high perceived advantages of sunbathing, and 6 women who reported low perceived advantages of sunbathing. Each FDR who participated in the study came from a unique family.
Ethnographic In-Home Interview
In contrast with traditional focus groups or interviews conducted in clinical or health care settings, the in-home interview is drawn from an ethnographic research tradition (Spradley, 1980) and is the recommended strategy for EDTM (Beck, 2005; Gladwin, 1989). The interviewer was able to obtain a first-hand sense of participants' sun protection behavioral habits and contexts in which sun protection is performed through conducting the interviews in participants' homes. We designed our interview according to Gladwin's (1989) guidelines indicating that the interviewer ask the participant to describe their decision-making processes for two distinct episodes that vary according to setting and activity; through inquiring about multiple episodes of behavioral performance the interviewer is able to uncover situational conditions that lead the participant to choose contrasting outcomes. This strategy is a central feature of the data collection approach for EDTM that directly highlights issues of behavioral inconsistency across different settings.
As such, we focused the structure of the interview on asking FDRs to recall two separate recent sun exposure periods (varying by setting and activity) when they were outdoors for 1 hour or more. For each sun exposure period, we asked participants to report on their use (or non-use) of the four sun protection methods under examination (sunscreen of at least SPF 15, shade seeking, hats, and sun protective clothing), as well as contextual background information about the sun exposure period, including the outdoor activity and setting, other individuals present, weather conditions, time of day, and the length of time they spent outdoors. We specifically prompted participants to describe the reasons why they used sun protection and reasons why they did not use sun protection so that we could identify central decision factors that might result in variation in sun protection use (The full interview guide is available from the first author.).
To enhance recall and to prompt detailed description of participants' sun protection practices, we requested that participants take us to where they stored and used sun protection items during an in-home tour. The interviewer asked participants to describe how they used sun protection items they had in their home while showing the interviewer the items. We concluded the interview by asking participants a set of demographic questions and thanking them for their valued time. Participants received $50 for their participation, and interviews were audio-recorded and transcribed for analysis.
Data Analysis
We constructed four decision tree models (one for each sun protection behavior) for each participant. In each decision tree model we depicted a series of ordered, discrete decision factors, both facilitators and barriers, followed by yes-no choice points (Gladwin, 1983, 1989). The development of the trees involved three steps. In Step 1, each of six analysis team members (JH and JB, clinical health psychologists; ES, a qualitative methods specialist who also served as the interviewer; CB, an advanced psychology graduate student; and SH and AP, two trained research staff members) read the in-home interview transcript and identified decision factors for the participant.
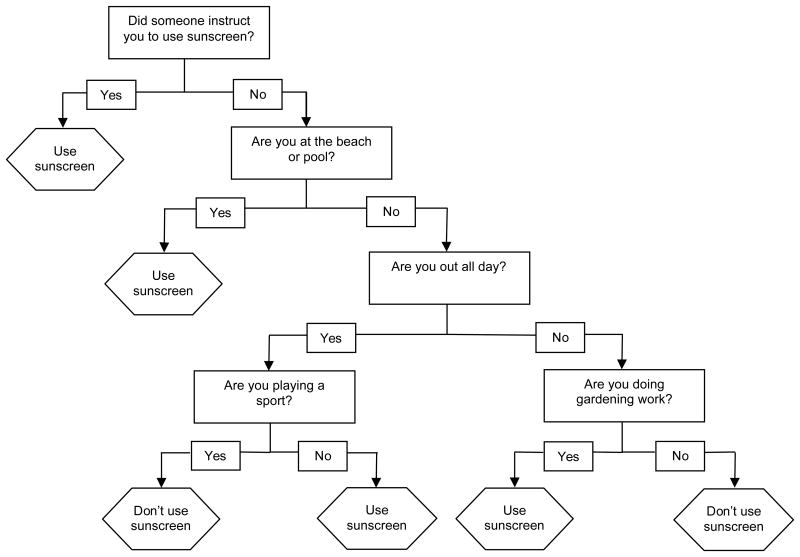
In Step 2, the team met to collaboratively develop the decision tree models for each sun protection behavior. This collaborative process involved detailed discussion of how the participant's behaviors varied across contexts, to accommodate and condense decision factors identified by team members. In some cases, the team identified additional factors to explain the participant's inconsistent sun protection during these discussions. As an example, Figure 1 presents a sunscreen use decision tree model generated from analysis of one FDR participant's description of his sunscreen use. The facilitators and barriers presented in this model are those that we identified solely for this one participant.
Figure 1. Sunscreen use decision tree model from one melanoma first-degree relative participant.
In Step 3, rather than generate composite decision tree models as suggested by Gladwin (1989), we identified a composite set of facilitators and barriers for each sun protection behavior using a combination of independent and collaborative analyses by our team. We chose to develop a composite set of facilitators and barriers so that we could attain high comprehensiveness in our data, and because participants' recalled sun exposure episodes varied considerably across the sample; we were impeded in constructing composite models that could fully account for all participants' decision factors because of this variation. We used a “divide and conquer” approach to identify facilitators and barriers across the entire sample for each sun protection behavior. We split our six-person analysis team into three pairs; two pairs were assigned responsibility to generate a proposed set of facilitators and barriers for one sun protection behavior for all participants, and one pair was responsible for generating a set of facilitators and barriers for two sun protection behaviors for all participants.
First, each team member of a given pair reviewed all participants' decision trees for their assigned sun protection behavior and independently developed groupings of facilitators and barriers based on conceptual similarity. The pair then met to compare their respective decision factor groupings and reach agreement on a set of composite facilitators and barriers for the sun protection behavior. Two investigator pairs proposed a final set of composite facilitators and barriers for each behavior. We assessed the reliability of the facilitators and barriers identified by each pair for each behavior, and ranged from 65% to 83%. The primary study investigators examined and resolved differences in the facilitator and barrier categories.
Results
The sample comprised 25 FDRs of melanoma survivors, which included 13 men and 12 women aged 19 to 78 years (mean = 39 years; SD=15.87). Participants were White (100%), well-educated (all were at least college educated), primarily married (56%), employed (68%), and primarily adult children of melanoma survivors (84%). Three (12%) were parents of melanoma survivors, and two (8%) were siblings of melanoma survivors. Fifteen FDRs (60%) reported having one family member diagnosed with melanoma, and 10 (40%) reported having two or three family members diagnosed with melanoma. We comprehensively report decision factors for sunscreen use, shade seeking, hat usage, and protective clothing use; below we describe the most important decision factors for each sun protection behavior.1
Sunscreen Use
We identified frequently mentioned facilitators for sunscreen use that helped to explain inconsistency in participants' use of this sun protection strategy (see Table 1). Participants often used sunscreen because they planned to be in the sun for a long period of time. Perceptions of what constituted a long period of time varied widely, from 30 minutes to being in the sun “all day.” Participants reported that they thought ahead, and considered the length of time they planned to be outdoors when deciding whether to use sunscreen. Others brought sunscreen with them and then applied it when their time threshold had been reached.
Table 1. Facilitators and Barriers to Use Sunscreen.
| Frequency | Facilitators | Barriers |
|---|---|---|
| Frequently useda | In the sun for a longer period of time | Shade conveniently available |
| At a beach/pool/water setting | Engaged in a physical activity | |
| Moderately usedb | Engaged in a physical activity | In the sun during nonpeak times |
| Sunny or hot outside | In the sun for a shorter period of time | |
| Encouraged to use sunscreen by others | No time to apply sunscreen | |
| Getting a sunburn | ||
| Infrequently usedc | It is the summer | Rainy outside |
| With other people who were using sunscreen | Cloudy outside | |
| Wanted to be a role model for others | Cool outside | |
| In the sun during peak times | Not the summer | |
| Starting to get some color on skin | Have a base tan | |
| Remembered to use or bring sunscreen or sunscreen was available | Trying to get a tan | |
| Wearing a bathing suit | Using tanning oil | |
| Willing to spend time applying sunscreen | Forgot to use or bring sunscreen | |
| Shade not conveniently available | Felt already protected by clothing | |
| Trying to get a tan | Concerned the smell of sunscreen could attract mosquitoes attract mosquitoes |
Frequently used facilitators were reported at least once by 11 or more participants. Frequently used barriers were reported by four or more participants.
Moderately used facilitators were reported by between five and 10 participants. Moderately used barriers were reported by three participants.
Infrequently used facilitators were reported by between one and four participants. Infrequently used barriers were reported by one or two participants.
Another important sunscreen facilitator involved being at a beach, pool, or water setting, where many reported that their use of sunscreen was nearly habitual, regardless of weather conditions. For example, one participant explained, “I try to use sunscreen every time at the beach, because I feel like I'm more prone to sunburn at the beach.” Other important facilitators involved hot and sunny weather, as well as the experience of starting to get sunburned or feeling that one's skin is burning. Finally, social encouragement was also a critical facilitator of sunscreen use. Social encouragement was manifest in three ways among these participants, including being with other people who were using sunscreen, verbal directives from others to use sunscreen, as well as using sunscreen to provide a good example to children. One participant described the importance of receiving social directives in dictating his sunscreen use: “I have to say honestly, the presence of an authority figure, female authority figure, either my mom or future wife prodding to put sunscreen on is a big, big factor.”
In terms of barriers to sunscreen use, the availability of shade was most frequently reported. Participants often chose to not use sunscreen if they had access to shade, even when they had sunscreen with them. Other barriers included exposure during non-peak times (morning or late afternoon), and spending a shorter period of time in the sun, even during peak times. Shorter periods of time comprised anything up to 2 hours in the sun. Finally, participants often abstained from using sunscreen if they felt they did not have time to apply it, such as when people needed to rush out the door, or to get started on their outdoor activities.
In some cases, participants were prompted to use sunscreen, and to avoid it, because of the same decision factors. For instance, some participants used sunscreen during physical activity (such as going for a run, playing golf, skiing, and gardening), and others avoided sunscreen use when physically active. Several participants reported that they used sunscreen during certain physical activities that they associated with longer outdoor exposure. In contrast, others said that they disliked using sunscreen during intense physical activity, because they found that when they sweated, sunscreen would get into their eyes and drip down their face, causing discomfort. Some participants felt that while physically active they were less aware of the sun on their skin, eliminating an important cue to sunscreen use.
Shade Seeking
Quite often, participants sought shade to get relief or a break from the discomfort of heat, strong sun, or glare (see Table 2). As such, some noted that they sought shade to read or to have a meal. Being at a beach, pool, or water setting also strongly facilitated participants to seek shade. For example, one participant stated:
We always bring a sun umbrella, if I'm going to the beach I bring a sun umbrella, for the same reason, to have relief from the heat and sun and everything … I always want to be under the umbrella. That is my first choice … If it was up to me and I was at the beach, I would be under an umbrella, pretty much without exception.
Table 2. Facilitators and Barriers to Shade seeking.
| Frequency | Facilitators | Barriers |
|---|---|---|
| Frequently useda | Feeling hot or uncomfortable in the sun | Seeking shade interferes with activity |
| At a beach/pool/water setting | ||
| Shade conveniently available | ||
| Moderately usedb | Sunny outside | |
| In the sun during peak times | ||
| In the sun for a longer period of time | ||
| Starting to get a sunburn or skin starting to hurt | ||
| Infrequently usedc | Eating outdoors in sunny or warm weather | Shade not conveniently available |
| Encouraged to seek shade by others | Chilly in the shade | |
| With other people who sought shade | Cool outside | |
| Sun in eyes | Outdoors for a brief period of time | |
| Engaged in a physical activity | With other people who were not seeking shade | |
| Feasible to seek shade given current activities | In the sun during nonpeak times |
Frequently used facilitators were reported at least once by 11 or more participants. Frequently used barriers were reported by four or more participants.
Moderately used facilitators were reported by between five and 10 participants. Moderately used barriers were reported by three participants.
Infrequently used facilitators were reported by between one and four participants. Infrequently used barriers were reported by one or two participants.
Many participants, however, were inconsistent in their shade seeking when at the beach, and only sought shade after a lengthy period of exposure. For example, one participant explained, “If we're there [at the beach] for more than an hour I'll prefer to sit under the umbrella … I feel like I'll have had enough sun.” Shade seeking was also tied to convenience and availability; whereas some thought ahead and brought sun umbrellas along with them, more often the use of shade was dictated by it being naturally present in the environment, such as by trees, overhangs, or awnings. Some participants sought shade in any sunny weather or during times of the day thought to be related to peak sun exposure, such as midday or during the summer, or when planning to be in the sun for longer periods of time. One participant noted:
I will not be under the umbrella after 2:00 or 3:00 in the afternoon, I will lay on the beach from 7:00 in the morning until 10:00 without an umbrella, I have no problem doing that, but from 10:00 until 2:00, 10:00 till 3:00, maybe even 10:00 till 4:00, I won't, it's just too intense. Too intense for me … I feel vulnerable, I guess that's the word to say, I feel most vulnerable to negative effects of skin burning.
Several participants sought shade if they were starting to get sunburned, and reported monitoring the color of their skin to determine when they should seek shade. Barriers to shade seeking often involved outdoor activities that were seen to preclude shade seeking, such as playing golf, as well as monitoring or playing with children. In these cases participants reported the impossibility or impracticality of shade seeking. One father said, “… I'd push the limits if he [son] wanted to play ball in the sun and there really wasn't an opportunity for shade. You know, most likely I wouldn't deprive him of that.”
Hat Use
Participants often wore hats to complement other sun protection strategies, or to meet a goal separate from sun protection alone. Many used hats when engaged in outdoor activities in the sun, including midday sun in the summer, when in the sun for 10 minutes or more, and while wearing glasses in the sun (see Table 3). Some participants prioritized hat usage because it helped prevent sunburn on the face and nose. Several used hats when engaged in physical activities, such as sports or gardening. Participants often wore hats during physical activity to meet multiple goals: as a tool to block glare, as a tool to protect one's hair from getting dirty or to keep hair out of the eyes, as well as a targeted form of sun protection for the scalp or the back of the neck.
Table 3. Facilitators and Barriers to Use Hats.
| Frequency | Facilitators | Barriers |
|---|---|---|
| Frequently useda | Sunny outside | Shade conveniently available |
| Wanted to dress nicely | ||
| Moderately usedb | Engaged in or watching a physical activity | Cloudy out or sun was less intense |
| Sun in eyes or hitting face | ||
| Outdoors for a longer period of time | ||
| Hat conveniently available | ||
| At a beach/pool/water setting | ||
| Cool outside | ||
| Infrequently usedc | It is the summer | Did not have a hat |
| Encouraged to use hat by others | Felt wearing a hat would mess up hair | |
| Hat comfortable or attractive to wear | Hair was wet | |
| Hot outside | Too hot for a hat | |
| Not wearing sunscreen and felt skin burning | Too windy for a hat | |
| Likely to sweat sunscreen off face | Wearing sunglasses | |
| Dressed casually | Have a base tan | |
| Wanted to hide hair | Wanted a tan or color on face | |
| Hat would have interfered with activities |
Frequently used facilitators were reported at least once by 11 or more participants. Frequently used barriers were reported by four or more participants.
Moderately used facilitators were reported by between five and 10 participants. Moderately used barriers were reported by three participants.
Infrequently used facilitators were reported by between one and four participants. Infrequently used barriers were reported by one or two participants.
Several participants wore hats to shield their eyes and face from the sun when they planned to be outdoors for a longer period of time (30 minutes to an “all-day outing”), or when they were likely to get wet. One participant was “very consistent” in her use of a hat when she was at a beach and would wear it even if she had applied sunscreen to her face. She explained, “I don't think you always cover everything [with sunscreen], you know, the part in your hair, your ears, that sort of thing. It [a hat] is easy, it's just an additional kind of protection that's pretty easy.” Finally, participants used hats when outdoors in cool weather as a method to keep warm rather than as a method of sun protection.
Participants avoided hat use when shade was available to them. Many explained that they did not believe it was necessary to wear a hat if they were in the shade because they were not exposed to the sun. If participants went outdoors at the last minute or spontaneously, hats were less likely to be accessible or available. Several participants chose not to wear hats for sun protection if they were attending a social activity where they wanted to dress nicely. This reflects a perception that the kinds of hats that are used for sun protection fit with casual attire, and are unsuitable to wear in contexts where one wants to appear presentable and attractive. One participant who routinely wore a hat on exercise walks after work indicated that she would be less likely to wear a hat if she were planning on a social activity after completing her walk. Finally, participants often chose to forgo hats in cloudy weather. A participant explained:
If it was overcast probably, that might dictate it [hat use] because I know at times when I'm doing something like biking, when you're working up a sweat it would be great not to wear the hat but I do wear it because it's sunny, but I know at times I would prefer not to be wearing it.
Protective Clothing Use
Overall, the majority of the sample did not use long-sleeved shirts or long pants as a form of sun protection, but rather as a means to say warm in cooler weather (see Table 4). The most frequently reported barrier to clothing use was whether shade was conveniently available. Several participants preferred to seek shade if it was available when outdoors in the summer rather than put on clothing. Many participants also avoided wearing protective clothing if they felt it was “too hot” outside. Participants generally felt that wearing longer clothing in warm or hot weather would make them feel even hotter, sweat more, and become uncomfortable. One participant stored away all her long-sleeved shirts in the summer, and stated, “I wouldn't even ever consider wearing long sleeves in the summer. Even though I know they make those that are [cooler]—I just feel like it's so hot I would never think to put on a long-sleeved shirt.”
Table 4. Facilitators and Barriers to Use Protective Clothing.
| Frequency | Facilitators | Barriers |
|---|---|---|
| Frequently useda | Cool outside | Shade conveniently available |
| Too hot for clothing | ||
| At a beach/pool/water setting | ||
| Engaged in a physical activity | ||
| Moderately usedb | Engaged in a physical activity | Already wearing sunscreen and did not need additional sun protection |
| Infrequently usedc | Outdoors in the summer during peak hours hours hours | Have a base tan |
| Wanted to protect skin for reasons other than sun protection | Wanted to look fashionable | |
| Outdoors for a longer period of time | Alone at the beach | |
| Sunny outside | ||
| Starting to get a sunburn | ||
| Comfortable clothing was available | ||
| Wanted to use clothing for modesty | ||
| Did not want to use sunscreen | ||
| At a beach/pool/water setting | ||
| Hot outside |
Frequently used facilitators were reported at least once by 11 or more participants. Frequently used barriers were reported by four or more participants.
Moderately used facilitators were reported by between five and 10 participants. Moderately used barriers were reported by three participants.
Infrequently used facilitators were reported by between one and four participants. Infrequently used barriers were reported by one or two participants. We acknowledge the valued aid of our study consultants, Jeanne Shoveller and Joni Mayer, as well as the valued assistance of Valerie Zamor with data analysis.
Participants also felt that wearing clothing was a barrier to going into and out of the water at the beach or pool. Several stated that wearing longer clothing impedes enjoyment of activities that one typically engages in when at a beach, pool, or water setting, such as laying out in the sun or swimming. Some participants explained that when in these environments they purposely wear less clothing with the aim of getting some color on their skin, or to enjoy the feeling of the sun on their skin. One participant consistently avoided wearing longer clothing when at the beach, and explained:
I've never really worn clothing on the beach. I've always worn a bathing suit … So kind of the way that I was raised and the way that I grew up was not to, you know, you just wear a bathing suit to the beach. You don't cover up and protect yourself from the sun.
Finally, participants avoided wearing sun protective clothing when using sunscreen during periods of sun exposure, because they felt sufficiently protected from the sun.
Participants both used and avoided use of protective clothing when engaged in outdoor physical activities. Many wore clothing during sporting activities, such as golf; leisure activities in water settings, such as snorkeling and fishing; physical activities where participants needed clothing to protect or cover their skin for safety reasons, such as performing manual labor, and gardening so as to prevent getting exposed to poisonous plants; and activities that involved bending down on pavement so as to prevent knees from getting scuffed or scratched. In general, participants chose to use longer clothing when physically active if it was not too warm outside, and if they knew they would be spending a longer period of time outdoors. In contrast, participants refrained from wearing protective clothing if they were engaged in outdoor physical activities in very hot weather. Thus, current weather conditions represented a moderator to clothing use as a sun protection strategy when participants were physically active. One participant explained his choice to not use longer clothing when playing basketball:
Because it's about the comfort. Me and I guess most people like they want to be comfortable when they're doing things so when you're wearing a long-sleeve shirt you feel a little more restricted I guess in your movements or you sweat easier and faster, you get hotter; I don't like it.
Discussion
In this article we provide a first step toward understanding the basis for inconsistent sun protection in first-degree family members of melanoma survivors, who are at an at least twofold increased risk of developing melanoma themselves (Ford et al., 1995). We used EDTM (Beck, 2005; Gladwin, 1989) to identify factors related to sun protection in these high-risk participants because it is ideally suited to generate decision factors utilized in the real-world setting of sun protection choices. Assessment of sun protection behavioral patterns, and the factors dictating those patterns, is an unaddressed, important priority for the development of sun protection interventions, particularly among individuals at increased risk for melanoma. Understanding nuanced behavioral patterns—rather than merely global sun protection—is critical in developing interventions to increase the consistency with which sun protection is performed.
We identified three factors that most often facilitated some form of sun protection (use of sunscreen of SPF 15 or above, shade seeking, hats, and protective clothing). These included being at a beach, pool, or water setting; being engaged in a physical activity; and being outdoors in sunny or hot weather. Of these facilitators, use of sun protection (specifically sunscreen, shade seeking, and hats) in beach, pool, or water settings was often reported to be routinely practiced across sun exposure episodes. Some participants stated that they were instructed to use sun protection in these environments since their youth, and that they regarded these settings as locations for prime sunburn risk. In contrast, the influence of sunny or hot weather as a facilitator of sun protection was more variable and dependent on an individual's ad hoc assessment of the perceived intensity of the sun and the length of time planned to be outdoors, which resulted in higher inconsistency in sun protection. Participants assessed the sun's perceived intensity according to the time of day and time of year. Fortunately, they were most likely to use sun protection in sunny or hot weather during midday hours in the summer, and less likely to do so if they felt the sun to be less intense, such as in the morning or late afternoon, and during nonsummer months.
Similarly, participants used sun protection if they were spending a longer period of time in the sun, yet perceptions of what constituted a longer time varied widely. As such, certain prominent facilitators had a more consistent influence over sun protection behavior, whereas the influence of other facilitators was more dependent on perceptual dimensions of the specific sun exposure event, which resulted in inconsistent sun protection use and thus opportunities for high levels of sun exposure and sunburn. Overall, these participants showed higher levels of sun protection consistency in the highest risk contexts. Additionally, the findings indicated where the use of sun protection is more variable, providing clear guidance for intervention strategies with these individuals.
The most prominent barrier to sun protection was the availability of shade, followed by engagement in physical activities. Shade availability served as a barrier to use of sunscreen, hats, and sun protective clothing but was a useful sun protection strategy in itself. Some participants strongly preferred to seek shade rather than to use other sun protection methods. Accordingly, if shade was not available participants were more likely to use other forms of sun protection. With the exception of bringing sun umbrellas and other shade-providing items, the availability of shade in an outdoor setting is highly context specific and variable. As a result, study participants inconsistently used sunscreen, hats, or protective clothing when outdoors because of this inherent variability. Participants judged the necessity of using sun protection when spending time outdoors according to the anticipated presence or absence of certain environmental conditions. Unfortunately, they might be left unprotected in situations where anticipated shade is unexpectedly unavailable.
Participants both used and avoided use of sunscreen and sun protective clothing during physical activity. With regard to sunscreen, participants considered the intensity of the physical activity they planned to engage in as well as the length of time they planned to spend outdoors when deciding to use sunscreen or not. Accordingly, they abstained from sunscreen use when engaged in sporting activities that involved physical exertion and sweating. However, if participants knew that their physical activity dictated being outdoors for a longer period of time, such as playing golf, they were likely to use sunscreen. In these instances participants accurately equated longer sun exposure periods with greater sunburn risk. There was a similar set of decision factors related to clothing use during physical activity. With these findings we suggest that use or non-use of sun protection during outdoor physical activities is based on an assessment of weather conditions, length of time outdoors, and the type of physical activity, all of which can vary across episodes. In these results we illustrate the need for interventions to directly address sun protection during physical activity, presenting choices for how to keep cool and comfortable, as well as sun-safe, during sporting events and exercise.
We found evidence that participants used certain sun protection methods to complement or replace the use of other methods. For example, participants often wore hats to augment sunscreen use when outdoors in intense sun for longer periods of time. Many sought shade to replace use of other sun protection strategies, so that the use of sunscreen, hats, or protective clothing was thus partially dependent on either planned or ad hoc availability of shade. This important finding has implications for quantitative assessment of sun protection behaviors, such that it might not be appropriate to summarize level of sun protection usage across many strategies, because one would not expect some approaches (e.g., sunscreen use and shade seeking) to be highly intercorrelated. In fact, some sun protection behaviors might be negatively correlated, making for an unclear interpretation of an overall sun protection summary score. Additionally, with this finding we provide an important explanation for the presence of sunburns in those who intend to be protected because shade might not be ultimately available in a setting where it is expected. Our results clearly indicate how individuals negotiate decisions about sun protection in real-world contexts, where environmental, social, and contextual cues and expectations vary greatly, and may serve to subsequently influence sun protection.
Researchers have extensively examined the role of individual differences in attitudes such as perceived skin cancer risk, self-efficacy for sunscreen use, or risk status (higher versus average risk), many of which are significantly related to sun protection behavior uptake in melanoma FDRs (Azzarello et al., 2006; Bishop et al., 2007; Geller et al., 2003; Geller et al., 2006; Manne et al., 2004). By design, our work is focused elsewhere, on decision factors that vary by sun exposure event, within-person, to illuminate how individuals might behave inconsistently despite their constant level of an attitude (such as perceived skin cancer risk) or their objective risk status. In accordance with EDTM, we will validate our models in the next step of our work, to examine the quantitative importance of facilitators and barriers to sun protection usage that were identified in the work reported here. This next phase will involve longitudinal ecological momentary assessment (Allport, 1951; Hufford, 2007; Stone & Shiffman, 2002) to evaluate the varied decision factors related to summer sun protection in melanoma FDRs.
An important avenue of future research should include investigating how both melanoma patients and family members respond to new sunscreen labeling requirements announced by the U.S. Food and Drug Administration in June 2011, indicating that sunscreen manufacturers clarify the strength of sunscreen protection in their labeling (FDA Sunscreen Drug Products for Over-the-Counter Human Use Rule, 2011). Based on these new requirements, it is critical to explore melanoma patients' and family members' knowledge regarding the terms UVA and UVB, and how they interpret the new labeling guidelines when making purchasing decisions, and when choosing what strength of sunscreen to use during periods of sun exposure.
We note several limitations to our research. First, our sample size of 25 FDRs is small, and thus we are not able to generalize the decision factors we identified to a broader population of melanoma FDRs. Second, in our ethnographic interviews we relied on participants' retrospective accounts of their sun protection decision making, which might have varied in accuracy. Additionally, by employing an ethnographic approach we may have oversampled those participants who were highly cooperative and invested in preventive health research in skin cancer. We tried to limit bias to our sampling by selecting equal numbers of those who reported high and low perceived advantages of sunbathing. Finally, we did not assess eye protection because of time constraints for the interview.
Despite these limitations, in our findings we help to provide detail and nuance to understanding the daily decision-making context in which melanoma FDRs use sun protection, as well as the diverse episodes and the multilevel, multifactorial nature on which these decisions are based. Recently, Craciun and colleagues (2011) identified sun protection planning as a statistically important mediator of the relationship between sun protection intentions and actual behavior. In this article we illustrate that planning itself is a complex decisional phenomenon that likely requires consideration of the context for planned activities, anticipated shade cover and amount of time in the sun, as well as whether physical activity is planned, among other factors. We also demonstrate that EDTM has strong potential and applicability to describe other naturalistic decision-making processes in the cancer context as well.
Acknowledgments
We acknowledge our study consultants, Jeanne Shoveller and Joni Mayer, and Valerie Zamor for assistance with data analysis.
Funding: The authors disclosed receipt of the following financial support for the research and/or authorship of this article: Grant R21 CA137532, provided by the National Cancer Institute.
Biographies
Elyse Shuk, MA, is a Qualitative Methods Specialist in the Department of Psychiatry and Behavioral Sciences at Memorial Sloan-Kettering Cancer Center in New York, New York, USA.
Jack Burkhalter, PhD, is an Assistant Attending Psychologist in the Department of Psychiatry and Behavioral Sciences at Memorial Sloan-Kettering Cancer Center in New York, New York, USA.
Carlos Baguer, MA, is a Doctoral Candidate in Psychology at The New School for Social Research in New York, New York, USA.
Susan Holland, MA, MPS, is a Clinical Research Manager in the Department of Psychiatry and Behavioral Sciences at Memorial Sloan-Kettering Cancer Center in New York, New York, USA.
Alisa Pinkhasik, BA, is a Research Assistant in the Department of Surgery at Memorial Sloan-Kettering Cancer Center in New York, New York, USA.
Mary Sue Brady, MD, FACS, is an Associate Attending Surgeon in the Gastric and Mixed Tumor Service in the Department of Surgery at Memorial Sloan-Kettering Cancer Center in New York, New York, USA.
Daniel Coit, MD, FACS, is an Attending Surgeon in the Gastric and Mixed Tumor Service in the Department of Surgery at Memorial Sloan-Kettering Cancer Center in New York, New York, USA.
Charlotte Ariyan, MD, PhD, is an Assistant Attending Surgeon in the Gastric and Mixed Tumor Service in the Department of Surgery at Memorial Sloan-Kettering Cancer Center in New York, New York, USA.
Jennifer Hay, PhD, is an Associate Attending Psychologist in the Department of Psychiatry and Behavioral Sciences at Memorial Sloan-Kettering Cancer Center in New York, New York, USA.
Footnotes
Facilitators and barriers.
Portions of this article were presented at the 35thAnnual American Society of Preventive Oncology Conference in Las Vegas, Nevada, March, 2011.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Allport GW. The use of personal documents in psychological science: Prepared for the Committee on Appraisal of Research. New York, NY: Social Science Research Council; 1951. [Google Scholar]
- American Cancer Society. Cancer facts & figures 2010. 2010 Retrieved from http://www.cancer.org/acs/groups/content/@nho/documents/document/acspc-024113.pdf.
- Armstrong BK, Kricker A. How much melanoma is caused by sun exposure? Melanoma Research. 1993;3:395–401. doi: 10.1097/00008390-199311000-00002. [DOI] [PubMed] [Google Scholar]
- Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. Journal of Photochemistry and Photobiology B, Biology. 2001;63:8–18. doi: 10.1016/S1011-1344(01)00198-1. [DOI] [PubMed] [Google Scholar]
- Azzarello LM, Dessureault S, Jacobsen PB. Sun-protective behavior among individuals with a family history of melanoma. Cancer Epidemiology Biomarkers & Prevention. 2006;15:142–145. doi: 10.1158/1055-9965.EPI-05-0478. [DOI] [PubMed] [Google Scholar]
- Beck KA. Ethnographic decision tree modeling: A research method for counseling psychology. Journal of Counseling Psychology. 2005;52:243–249. doi: 10.1158/1055-9965.EPI-05-0478. [DOI] [Google Scholar]
- Bishop JA, Taylor T, Potts HW, Elliott F, Pinney E, Barrett JH, Fallowfield L. Sun-protective behaviors in families at increased risk of melanoma. Journal of Investigative Dermatology. 2007;127:1343–1350. doi: 10.1038/sj.jid.5700764. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Sunburn prevalence among adults -- United States, 1999, 2003 and 2004. Morbidity and Mortality Weekly Report (MMWR) 2007;56:524–528. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5621a2.htm. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Skin cancer. 2011 Retrieved from http://www.cdc.gov/cancer/skin/
- Coups EJ, Manne SL, Heckman CJ. Multiple skin cancer risk behaviors in the U.S. population. American Journal of Preventive Medicine. 2008;34:87–93. doi: 10.1016/j.amepre.2007.09.032. [DOI] [PubMed] [Google Scholar]
- Craciun C, Schuz N, Lippke S, Schwarzer R. A mediator model of sunscreen use: A longitudinal analysis of social-cognitive predictors and mediators. International Journal of Behavioral Medicines. 2011 doi: 10.1007/s12529-011-9153-x. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Dal H, Boldemann C, Lindelof B. Does relative melanoma distribution by body site 1960-2004 reflect changes in intermittent exposure and intentional tanning in the Swedish population? European Journal of Dermatology. 2007;17:428–434. doi: 10.1684/ejd.2007.0242. [DOI] [PubMed] [Google Scholar]
- Ford D, Bliss JM, Swerdlow AJ, Armstrong BK, Franceschi S, Green A, Osterlind A. Risk of cutaneous melanoma associated with a family history of the disease. The International Melanoma Analysis Group (IMAGE) International Journal of Cancer. 1995;62:377–381. doi: 10.1002/ijc.2910620403. [DOI] [PubMed] [Google Scholar]
- Gandini S, Sera F, Cattaruzza MS, Pasquini P, Picconi O, Boyle P, Melchi CF. Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. European Journal of Cancer. 2005;41:45–60. doi: 10.1016/j.ejca.2004.10.016. [DOI] [PubMed] [Google Scholar]
- Geller AC, Emmons KM, Brooks DR, Powers C, Zhang Z, Koh HK, Gilchrest BA. A randomized trial to improve early detection and prevention practices among siblings of melanoma patients. Cancer. 2006;107:806–814. doi: 10.1002/cncr.22050. [DOI] [PubMed] [Google Scholar]
- Geller AC, Emmons K, Brooks DR, Zhang Z, Powers C, Koh HK, Gilchrest BA. Skin cancer prevention and detection practices among siblings of patients with melanoma. Journal of the American Academy of Dermatology. 2003;49:631–638. doi: 10.1067/S0190-9622(03)02126-1. [DOI] [PubMed] [Google Scholar]
- Gladwin CH. Contributions of decision-tree methodology to a farming systems program. Human Organization. 1983;42:146–157. Retrieved from http://sfaa.metapress.com/app/home/journal.asp?referrer=parent&backto=homemainpublications,1,2; [Google Scholar]
- Gladwin CH. Ethnographic decision tree modeling. Newbury Park, CA: Sage; 1989. [Google Scholar]
- Green AC, Williams GM, Logan V, Strutton GM. Reduced melanoma after regular sunscreen use: Randomized trial follow-up. Journal of Clinical Oncology. 2011;29:257–263. doi: 10.1200/JCO.2010.28.7078. [DOI] [PubMed] [Google Scholar]
- Hufford MR. Special methodological challenges and opportunities in ecological momentary assessment. In: Stone AA, editor. The science of real-time data capture: Self-reports in health research. New York, NY: Oxford University Press; 2007. pp. 54–75. [Google Scholar]
- Jackson KM, Aiken LS. A psychosocial model of sun protection and sunbathing in young women: the impact of health beliefs, attitudes, norms, and self-efficacy for sun protection. Health Psychology. 2000;19:469–478. doi: 10.1037/0278-6133.19.5.469. [DOI] [PubMed] [Google Scholar]
- Johnson J, Williams ML. A preliminary ethnographic decision tree model of injection drug users' (IDUs) needle sharing. Substance Use and Misuse. 1993;28:997–1014. doi: 10.3109/10826089309062179. [DOI] [PubMed] [Google Scholar]
- Kricker A, Armstrong BK, Goumas C, Litchfield M, Begg CB, Hummer AJ, Berwick M. Ambient UV, personal sun exposure and risk of multiple primary melanomas. Cancer Causes and Control. 2007;18:295–304. doi: 10.1007/s10552-006-0091-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancaster K. A new approach to consumer theory. Journal of Political Economy. 1966;74:132–157. Retrieved from http://www.jstor.org/stable/1828835. [Google Scholar]
- Manne S, Fasanella N, Connors J, Floyd B, Wang H, Lessin S. Sun protection and skin surveillance practices among relatives of patients with malignant melanoma: prevalence and predictors. Preventive Medicine. 2004;39:36–47. doi: 10.1016/j.ypmed.2004.02.028. [DOI] [PubMed] [Google Scholar]
- Manne S, Jacobsen PB, Ming ME, Winkel G, Dessureault S, Lessin S. Tailored versus generic interventions for skin cancer risk reduction for family members of melanoma patients. Health Psychology. 2010;29:583–593. doi: 10.1037/a0021387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan GW, Bernard HR. Testing an ethnographic decision tree model on a national sample: Recycling beverage cans. Human Organization. 2006;65:103–114. Retrieved from http://sfaa.metapress.com/app/home/journal.asp?referrer=parent&backto=homemainpublications,1,2; [Google Scholar]
- Spradley J. The ethnographic interview. New York, NY: Holt, Rinehart, and Winston; 1979. [Google Scholar]
- Spradley J. Participant observation. New York, NY: Holt, Rinehart, and Winston; 1980. [Google Scholar]
- Stone AA, Shiffman S. Capturing momentary, self-report data: A proposal for reporting guidelines. Annals of Behavioral Medicine. 2002;24:236–243. doi: 10.1207/S15324796ABM2403_09. [DOI] [PubMed] [Google Scholar]
- Strauss A, Corbin J. Basics of qualitative research: Techniques and procedures for developing grounded theory. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Thomas NE, Edmiston SN, Alexander A, Millikan RC, Groben PA, Hao H, Conway K. Number of nevi and early-life ambient UV exposure are associated with BRAF-mutant melanoma. Cancer Epidemiology, Biomarkers and Prevention. 2007;16:991–997. doi: 10.1158/1055-9965.EPI-06-1038. [DOI] [PubMed] [Google Scholar]
- Tucker MA, Halpern A, Holly EA, Hartge P, Elder DE, Sagebiel RW, Clark WH., Jr Clinically recognized dysplastic nevi. A central risk factor for cutaneous melanoma. Journal of the American Medical Association. 1997;277:1439–1444. doi: 10.1001/jama.1997.03540420035026. [DOI] [PubMed] [Google Scholar]
- Tversky A. Elimination by aspects: A theory of choice. Psychological Review. 1972;79:281–289. doi: 10.1037/h0032955. [DOI] [Google Scholar]
- U.S. Food and Drug Administration. Sunburn protection factor (SPF) 2009 Retrieved from http://www.fda.gov/AboutFDA/CentersOffices/CDER/ucm106351.htm.
- U.S. Food and Drug Administration Sunscreen Drug Products for Over-the-Counter Human Use Rule, 76 Fed. Reg. 117 (proposed June 14, 2011) (to be codified at 221 C.F.R. pt.201.327).
- Weller SC, Ruebush TR, II, Klein RE. Predicting treatment-seeking behavior in Guatemala: a comparison of the health services research and decision-theoretic approaches. Medical Anthropology Quarterly. 1997;11:224–245. doi: 10.1525/maq.1997.11.2.224. [DOI] [PubMed] [Google Scholar]
- Whiteman DC, Whiteman CA, Green AC. Childhood sun exposure as a risk factor for melanoma: A systematic review of epidemiologic studies. Cancer Causes and Control. 2001;12:69–82. doi: 10.1023/A:1008980919928. [DOI] [PubMed] [Google Scholar]
- Young JC. A model of illness treatment decisions in a Tarascan town. American Ethnologist. 1980;7:106–131. doi: 10.1525/ae.1980.7.1.02a00070. [DOI] [Google Scholar]