Abstract
Objective
To provide an ethical framework for clinicians and companies providing non-invasive prenatal testing using cell-free fetal DNA or whole fetal cells.
Method
In collaboration with an NIH-supported research ethics consultation committee, together with feedback from an inter-disciplinary group of clinicians, members of industry, legal experts and genetic counselors we developed a set of best practices for the provision of non-invasive prenatal genetic testing.
Results
Principal recommendations include the amendment of current informed consent procedures to include attention to the non-invasive nature of new testing and the potential for a broader range of results earlier in the pregnancy. We strongly recommend that tests should only be provided through licensed medical providers and not direct-to-consumer.
Conclusion
Prenatal tests, including new methods using cell-free fetal DNA, are not currently regulated by government agencies and limited professional guidance is available. In the absence of regulation, companies and clinicians should cooperate to adopt responsible best ethical practices in the provision of these tests.
Introduction
In the last several years, the ability to detect fetal characteristics by analyzing cell-free fetal DNA (cffDNA) circulating in the maternal bloodstream has opened the door to a wide range of non-invasive techniques that have the potential to revolutionize prenatal aneuploidy testing. Current data by Palomaki et al,1,2 Bianchi,3 Norton4 and Zimmerman5 have shown high sensitivity (98.9-100% for trisomy 21) and specificity with a false positive rate below 1%. These non-invasive techniques allow for earlier testing than current invasive methods and have no procedure-related risk of miscarriage. Testing is currently available for fetal trisomies 13, 18, and 21, monosomy X and other sex chromosome aneuploidies, RhD status and fetal sex in the United States, Europe and Asia.6-8 Professional societies, such as the International Society for Prenatal Diagnosis (ISPD),9 the National Society of Genetic Counselors (NSGC),10 and the American College of Obstetrics and Gynecology,11 describe cffDNA testing as a highly sensitive aneuploidy screen, and currently encourage validation of abnormal results with invasive prenatal diagnosis. These organizations approve, although do not proactively recommend, the offer of cffDNA testing only to high-risk women - such as those who are of advanced maternal age, screen positive through other methods, or who have ultrasound anomalies. However, given recent progress towards clinical validation of aneuploidy testing in low-risk women,12 it is likely that cffDNA testing will increasingly be offered to all pregnant women within the next few years. Indeed, the most recent guidelines from the American College of Medical Genetics do not distinguish between ‘high risk’ and ‘low risk’ populations, although they continue to recommend confirmatory invasive testing for definitive diagnosis.13
The commercial provision of cffDNA tests has ethical and clinical implications that differ from existing prenatal tests. For one thing, their commercial, and potentially direct-to-consumer, provision differentiates them from existing testing modalities. Their impact will also depend on whether cffDNA is eventually considered a screening or diagnostic test and whether testing is limited to aneuploidies, which have relatively well established prognoses, or is expanded to a wider range of genetic conditions. The underlying normative precepts governing best ethical practices, however, remain similar from the perspective of clinicians and test providers.
Thus far, US regulatory agencies have exercised regulatory discretion in minimally regulating the safety and effectiveness of cffDNA tests,14 although there is some indication that this may be changing.15,16 Likewise, professional societies have offered guidelines for the use of these tests, but have neither provided comprehensive guidance to clinicians on their ethical implications nor addressed the best practices of commercial providers, who also have an obligation to ensure that their products are not generating unethical outcomes.
We believe that validation and guidance from both regulators and professional communities is desirable in ensuring ethical and effective introduction of potentially high impact emerging technologies such as cffDNA tests. In the absence of such guidance, the possibility of inadequate integration of new prenatal testing procedures presents a strong potential for ill-informed patient decision-making, unjust distribution of services and increased stigmatization of disability communities.17-20 We therefore offer a model code of best ethical practices to allow care providers and the commercial entities that develop and sell non-invasive prenatal tests to work together to ensure their ethical provision. While these recommendations are largely aimed at regulatory and clinical entities in the United States, we anticipate that many of the normative principles, and their implementation, will be broadly applicable in other venues.
These practices were developed by an NIH-funded research ethics consultation committee, established in 2010, at the request of a commercial prenatal testing provider. Membership includes representatives of bioethics, clinical ethics, law, genetic counseling, obstetrics and gynecology, genetics and sociology. The committee sought consensus rather than majority on all recommendations. Methods included a thorough review of the relevant literature and guidelines for other prenatal technologies. Feedback on the resulting recommendations was solicited from an interdisciplinary panel of clinicians, legal experts, genetic counselors and representatives from the disability community and industry at an all-day seminar focused on cffDNA testing, which included an open discussion forum for stakeholder representatives. Initial manuscripts were drafted by the first author and underwent extensive review and revision by all co-authors. The commercial provider who initially requested consultation had no input into the development or finalization of these recommendations, nor of this manuscript.
CLINICIANS AND CARE PROVIDERS
Access
Since 2007, the American Congress of Obstetricians and Gynecologists (ACOG) has recommended that all pregnant women be offered prenatal screening for fetal aneuploidy, regardless of maternal age.21 All women should therefore be offered the most reliable prenatal tests that have medical significance and demonstrated safety and effectiveness in the patient's risk population. Five main factors influence patient access to prenatal testing: 1) availability of qualified providers to perform testing and interpretation, 2) patient presentation for prenatal care in time to obtain prenatal testing, 3) patient and provider knowledge and preferences, 4) financial resources, and 5) regulatory policies.
One benefit of cffDNA testing is the lack of required local procedural expertise, making testing feasible in geographic areas where certified nuchal translucency or chorionic villus sampling (CVS) providers are not available. cffDNA testing is also less dependent on gestational age than serum screening. Since many women do not undergo invasive testing until the second trimester, the early use of cffDNA, which may occur as early as 10 weeks gestation, may mean that, elective termination procedures might be performed earlier and with fewer complications. This advantage may be significant in jurisdictions that limit elective termination by gestational age. These factors may serve to increase overall access to prenatal testing.
Financially, however, the cost of cffDNA testing remains prohibitive for many women. The course of several ongoing patent lawsuits in the US may alleviate or exacerbate this issue. There remain questions about the extent to which private and state health insurance programs will cover cffDNA testing and confirmatory diagnostic testing. Lack of coverage may result in the exclusion of uninsured individuals and those with limited resources from cffDNA testing. On the other hand, cffDNA testing is covered by Medicare in some states, but not by private insurers, creating potential inequalities in the opposite direction.22 Care providers should encourage policies to support universal access to prenatal testing and, where possible, work with third party payers to arrange coverage of medically desirable testing.
Pilot studies suggest that obstetricians23 and patients24,25 are generally interested in incorporating cffDNA testing into their practice and care. Although some physicians may have reservations about expanding the range of prenatal testing - because they believe it may lead to an increase in elective terminations - codes of medical ethics suggest that all clinicians should be prepared to offer, or offer referrals for, cffDNA testing unless local regulation constrains its availability. Some international governments prohibit sex testing, for example, which might impact access to certain test results.
Informed Consent
A critical clinical and ethical concern surrounding the uptake of cffDNA testing is how the informed consent and counseling process, both before and after cffDNA testing, will occur. Historically, prenatal screening has been held to a lower standard of pre-test informed consent than invasive diagnostic testing. However, published data and anecdotal experience suggest that many women who receive an abnormal screening result do not fully understand its implications, and in some cases were not fully aware that they were undergoing screening at all.26-31 In the past, the genetic counseling process preceding invasive prenatal diagnosis allowed women to consider an informed refusal of invasive testing. As cffDNA testing becomes more available, however, women will receive test results with a significantly higher positive predictive value without a chance to deliberate on whether they truly desire the information. This suggests that the informed consent process for cffDNA testing should be held to a higher standard than current noninvasive screening measures.
Clinicians should ensure that a qualified care provider is prepared to discuss the implications of cffDNA testing with their patients in an interactive manner that accurately reflects both the statistical and subjective aspects of the results, including the medical and social elements of raising a child with the condition in question.32-34 While we recognize that written consent is only one part of the informed consent process, we propose that after an in-depth discussion of the implications of the proposed testing, a standardized informed consent form, stating either an acceptance or refusal of testing, should be reviewed and signed by the patient.
Components should include: 1) a list of indicated tests which patients may choose to undergo, 2) a description of all possible findings and their validity (including the potential for assay failure), utility, and limitations, 3) a list of alternative tests for similar indications if applicable, and 4) options for patients who do not wish to receive all results.
When faced with the time constraints of a busy practice, we recognize that most care providers do not have the resources to facilitate a more complex discussion of prenatal testing. It will therefore be necessary to consider alternative methods of achieving informed consent for the large population that may be offered cffDNA testing in the future. Options for educating patients include referrals, educational classes, and static or interactive educational approaches, all of which can facilitate both education and a values-based consideration of testing options.
It is also critical that clinicians be sensitive to the desire of some women not to undergo prenatal testing.35-37 The decreased physical risk involved in non-invasive testing may lead to the assumption that there is ‘no downside’ to undergoing cffDNA testing. This can lead to practices that give the unspoken impression that prenatal testing is inevitable or expected.38-40 In addition, the possible combination of cffDNA sampling with other routine blood draws may significantly erode informed consent.41,42 ACOG's Committee Opinion specifically recommends that cffDNA should not be part of routine prenatal labwork. Clinicians offering cffDNA must strike a delicate balance in giving patients the opportunity to understand their growing choices in prenatal testing and make clear, informed choices without undue pressure.
The timing of patient education is further complicated by the ability to perform cffDNA testing relatively early in a pregnancy. In the US, most women present for their first prenatal visit between 8-12 weeks gestation. If cffDNA testing is performed late in the first trimester, pregnant women will need to decide whether they wish to undergo testing shortly after their first prenatal visit, a time when many women are still adjusting to the news of a pregnancy. Although some professionals have raised the possibility of preconception education, this may not benefit the approximately 50% of pregnancies that are unplanned and even higher percentages of pregnant women that do not attend preconception visits with their obstetrician.43
Returning results
Another concern is that patients may make decisions about their reproductive options following prenatal screening without a comprehensive understanding of their test results. We strongly recommend that a full genetic counseling session, including the recommendation of confirmatory testing, be provided after a positive cffDNA screen.10 It is critical that prenatal decisions be made on the basis of accurate and up to date medical information combined with information about the psychosocial aspects of life with the specific condition .44-46
Further complicating the return of results, pilot studies in cffDNA analysis have demonstrated the ability to map the whole fetal genome, meaning that many of the same issues that arise in the conduct of genomic research in adults may now extend to the fetus.47-49 These include the role of ethnicity and environmental factors in genetic expression, the difficulty in interpreting low-penetrance variants and the possibility of non-medical findings such as paternity.50,51 If parental samples are involved in the testing process then additional complications will apply. Patients should make decisions in advance about which categories of findings they wish to receive and both clinicians and laboratories should take note of existing professional recommendations and standards when planning reporting of results.52-54 As cffDNA technology expands, ethical considerations should be a significant factor in planning the provision of test results, particularly predictive or pre-dispositional testing, in order to preserve the autonomy of the parents and the potential child.55
COMPANIES AND TEST PROVIDERS
Direct-to-Consumer Testing
Non-invasive prenatal tests should be offered by and through qualified clinicians and never directly to consumers. The clinician ordering the test should be a clinical provider who is familiar with the patient and in a position to tailor a testing regime to her personal needs and obtain proper informed consent. Although offering tests directly to consumers may be seen as an opportunity to expand the potential market for cffDNA testing, potential irregularities in quality, customer misinterpretation of results and a lack of comprehensive consent or counseling procedures pose a risk of negative public feedback, loss of trust in the methodology and the potential for overly-restrictive regulation.56-60
Legal and Regulatory Issues
There is currently no legal obligation in the US to demonstrate safety and effectiveness for laboratory developed tests. However, the most ethical approach is to offer only tests that have proven clinical validity in the populations to which they are being offered. Furthermore, laboratories should implement independently verified proficiency testing procedures to assure analytic validity and set transparent standards for data interpretation and error rates. Advertising and marketing materials, whether directed to clinicians or the public, should comply with relevant standards for accuracy and clarity with regards to the sensitivity, specificity and medical relevance of their tests. One possible model for such standards is the U.S. System of Oversight of Genetic Testing: A Response to the Charge of the Secretary of Health and Human Services Report of the Secretary's Advisory Committee on Genetics, Health, and Society.61
Unlike existing invasive methods, cffDNA testing can be offered remotely, which opens the door to the international provision of cffDNA testing and the heterogeneity of jurisdictions and law. In some jurisdictions, for instance, governments have responded to practices of sex-linked abortions by restricting parental access to information about fetal sex; providing information on fetal sex, even as an incidental finding, in these jurisdictions poses significant ethical and legal concern. To the best of their ability, companies should attempt to ensure that any tests they offer are legal in both their local jurisdiction and the one in which the patient resides.
Responsibilities to assure informed consent
Companies and clinical laboratories should: develop clear and accurate consent forms that clinicians can use to order their services, provide clinicians with educational materials explaining, in a value neutral manner, the purpose of testing and the potential risks and benefits of undergoing the testing, and require verification that the informed consent process has occurred before processing samples.62 While companies do not have a direct responsibility to obtain informed consent, they should require certification of informed consent before testing is provided.
We also suggest that the written consent for cffDNA testing should include the company's intentions regarding the storage of samples and genetic data and its policies regarding any research it intends to conduct using samples or test results. In the past, failure to obtain consent for the use of samples has resulted in lawsuits such as those against Texas and Minnesota's Departments of Health; after parents objected to the use of their newborn children's genetic samples, states were forced to destroy them.63-66 Samples should not be used for research without explicit consent separate from the consent obtained to use samples for clinical purposes; unless specific consent for future use has been obtained samples should be destroyed after clinical testing. Research conducted on customer samples that is intended to generate new knowledge or be published in a scientific journal should also be reviewed by an institutional review board (IRB).67
Avoiding Stigmatization
Prenatal testing for genetic conditions is often seen as sending a message of stigmatization towards families who live with these conditions. This is complicated, in the case of cffDNA testing, by the fact that companies offering these tests are highly competitive, for-profit entities with financial obligations to investors. This may encourage more aggressive marketing efforts than existing prenatal testing modalities. While some may argue that any form of marketing prenatal screening or testing sets up an inherent bias towards encouraging uptake and stigmatizes those with the condition for which testing is being offered, it is unreasonable to expect that marketing will be eliminated. Instead, companies offering cffDNA testing should avoid marketing strategies that focus on ‘prevention’ or suggesting that any condition, or potential disability, ‘justifies’ or ‘demands’ testing. We also suggest that prenatal testing companies maintain a position that neither advocates or encourages termination on the basis of a genetic condition.
Enhancing Access and Quality
A number of patents on cffDNA analytic methods have been filed and litigation is currently in progress regarding the ultimate ownership of cffDNA intellectual property.68 The conduct of patent holders in the matter of licensing and pricing cffDNA testing will have an effect on its accessibility. Restrictive licensing strategies, an unwillingness to work with third party payers and high price points for individual tests restrict access to potentially valuable tests, test development data and quality assurance and improvement measures.69 Such outcomes represent a failure of distributive justice and exacerbate the fact that those in lower socioeconomic strata already face challenges of limited access to relevant prenatal care and fewer resources to care for children with special needs. Furthermore, restrictive intellectual property and licensing practices can essentially dictate the standard of care for a technology. Companies that develop and patent cffDNA testing should design intellectual property, licensing and data sharing strategies that afford the greatest quality, availability and access of testing while maintaining a viable business model. In addition, de-identified, aggregate testing data should be available in the public domain to enhance test interpretation and improvement.
Conclusion
If cffDNA testing continues to expand at its current pace, it will provide an increasing range of prenatal information. While increasing patient autonomy and reassurance on the one hand, this expansion in fetal information may also increase patient anxiety or generate unjust outcomes surrounding fetal selection and elective abortion. We urge cffDNA testing providers, both clinicians and test suppliers, to be sensitive to the very real ethical issues incumbent in this type of testing. Ethical practices will improve the professional conduct of those who provide prenatal testing and benefit the many families that non-invasive prenatal testing has the potential to help.
Non-invasive prenatal genetic testing using cell-free fetal DNA or whole fetal cells has ethical implications pertaining to its commercial and clinical provision.
This paper provides a set of ethical best practices for clinicians and companies providing non-invasive prenatal genetic testing.
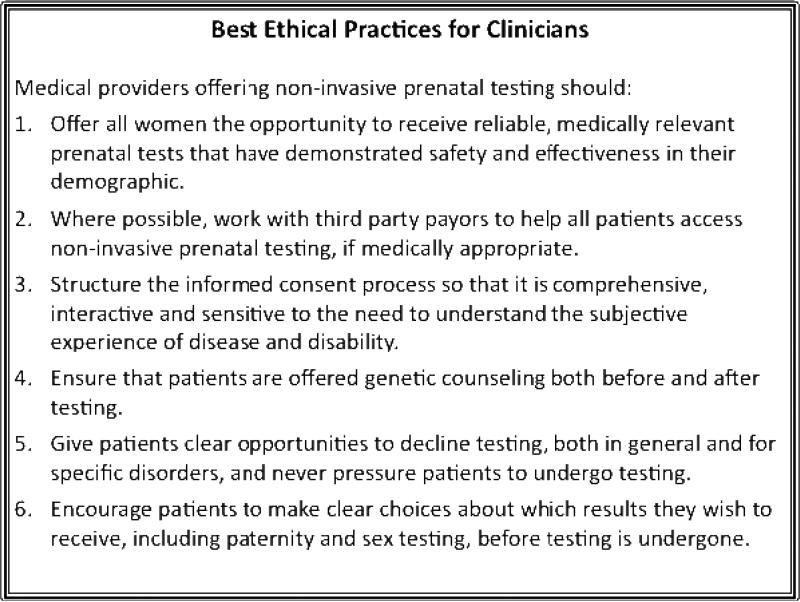
Figure 1.
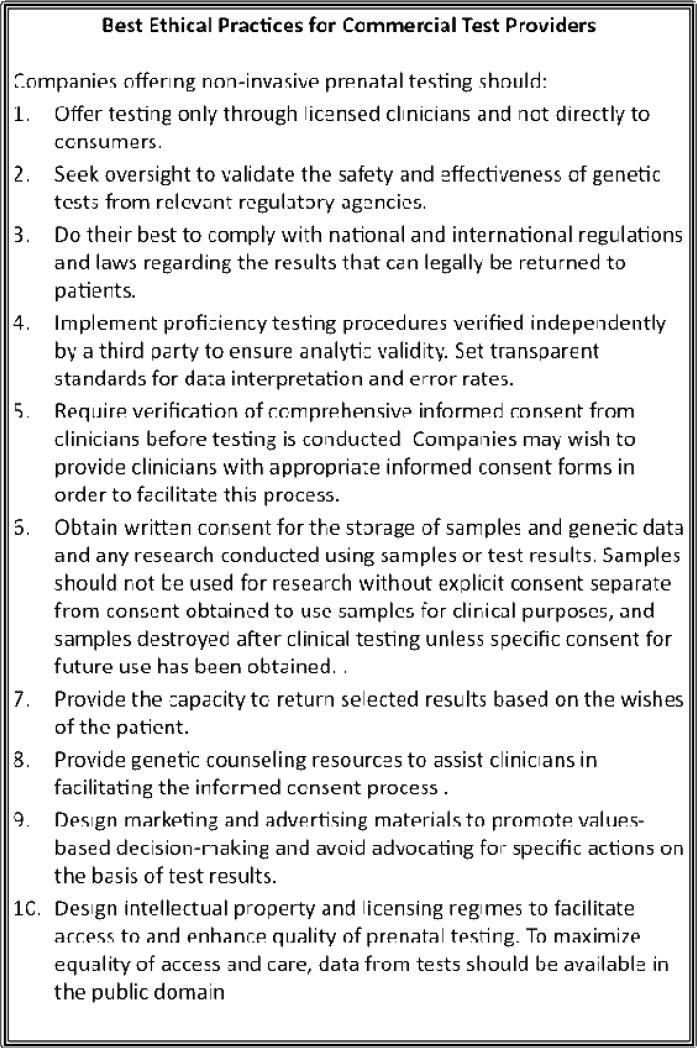
Figure 2.
Acknowledgements
This work was supported by NIH grant P50 HG003389 (Center for Integrating Ethics and Genetic Research) and NIH grant 1 U54 RR024374-01A1
Footnotes
Conflicts of Interest: Mary Norton is a principal investigator on clinical trial NCT0145167, sponsored by Ariosa Diagnostics.
Contributor Information
MA Allyse, Stanford Center for Biomedical Ethics 1215 Welch Road, Modular A Stanford, Ca 94305.
LC Sayres, Duke Medical School.
M Havard, Georgetown University.
JS King, University of California, Hastings College of the Law.
HT Greely, Stanford School of Law and Department of Genetics.
L Hudgins, Stanford Department of Medical Genetics.
J Taylor, Stanford Department of Pediatrics.
ME Norton, Stanford Department of Obstetrics and Gynecology.
MK Cho, Stanford Center for Biomedical Ethics and Department of Pediatrics.
D Magnus, Stanford Center for Biomedical Ethics and Department of Pediatrics.
KE Ormond, Stanford Center for Biomedical Ethics and Department of Medical Genetics.
References
- 1.Palomaki GE, Kloza EM, Lambert-Messerlian GM, Haddow JE, Neveux LM, Ehrich M, et al. DNA sequencing of maternal plasma to detect Down syndrome: An international clinical validation study. Genet Med. 2011;13(11):913. doi: 10.1097/GIM.0b013e3182368a0e. [DOI] [PubMed] [Google Scholar]
- 2.Palomaki GE, Deciu C, Kloza EM, Lambert-Messerlian GM, Haddow JE, Neveux LM, et al. DNA sequencing of maternal plasma reliably identifies trisomy 18 and trisomy 13 as well as Down syndrome: An international collaborative study. Genet Med. 2012;13(3):296–305. doi: 10.1038/gim.2011.73. 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bianchi D, Platt L, Golberg J, Abuhamad A, Sehnert A, Rava R. Whole genome maternal plasma DNA sequencing detects autosomal and sex chromosome aneuploidies. Prenat Diagn. 2012;32(Suppl. 1):3–4. [Google Scholar]
- 4.Norton ME, Brar H, Weiss J, Karimi A, Laurent LC, Caughey AB, et al. Non-Invasive chromosomal evaluation (NICE) study: Results of a multicenter prospective cohort study for detection of fetal trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;207(2):137, e1–8. doi: 10.1016/j.ajog.2012.05.021. [DOI] [PubMed] [Google Scholar]
- 5.Zimmermann B, Hill M, Gemelos G, Demko Z, Banjevic M, Baner J, et al. Noninvasive prenatal aneuploidy testing of chromosomes 13, 18, 21, X, and Y, using targeted sequencing of polymorphic loci. Prenat Diagn. 2012;32(13):1233–1241. doi: 10.1002/pd.3993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Proffitt A. Fruitful market: Berry genomics tackles prenatal testing in china. Bio IT World. 2013 Feb; 20. [Google Scholar]
- 7.Karow J. Focusing on Chinese market, berry genomics expects to run 100K noninvasive prenatal tests in 2013. [April 2013];GenomeWeb. 2013 Jan 23; Available at http://www.genomeweb.com/sequencing/focusing-chinese-market-berry-genomics-expects-run-100k-noninvasive-prenatal-tes.
- 8.Heger M. Sequenom inks additional distribution deals for T21 test. [April 2013];GenomeWeb. 2012 Aug 28; Available at http://www.genomeweb.com/sequencing/sequenominks-additional-distribution-deals-t21-test.
- 9.Benn P, Borell A, Chiu R, Cuckle H, Dugoff L, Faas B, et al. Position statement from the aneuploidy screening committee on behalf of the board of the International Society for Prenatal Diagnosis. 2013 Apr; doi: 10.1002/pd.4139. [DOI] [PubMed] [Google Scholar]
- 10.Devers P, Cronister S, Ormond K, Facio F, Brasington C, Flodman P. Noninvasive prenatal testing/noninvasive prenatal diagnosis: The position of the National Society of Genetic Counselors. J Genet Couns. 2013 doi: 10.1007/s10897-012-9564-0. [DOI] [PubMed] [Google Scholar]
- 11.The American College of Obstetricians and Gynecologists Committee on Genetics, The Society for Maternal-Fetal Medicine Publications Committee Committee Opinion Number 545 . 2012 [Google Scholar]
- 12.Nicolaides Syngelaki A, Ashoor G, Birdir Touzet G. Noninvasive prenatal testing for fetal trisomies in a routinely screened first-trimester population. AJOG. 2012;207(5):374, e1–6. doi: 10.1016/j.ajog.2012.08.033. [DOI] [PubMed] [Google Scholar]
- 13.Gregg AR, Gross SJ, Best RG, Monaghan KG, Bajaj K, Skotko BG, et al. ACMG statement on noninvasive prenatal screening for fetal aneuploidy. Genet Med. 2013 doi: 10.1038/gim.2013.29. [DOI] [PubMed] [Google Scholar]
- 14.Secretary's Advisory Committee on Genetic Testing . Enhancing the oversight of genetic tests: Recommendation of the SACGT. National Institutes of Health; Bethesda, Ma: 2000. [Google Scholar]
- 15.Guttierez A. Informing Reproductive Choice? Prenatal Genetic Testing in the 21st Century. Stanford Law School; Stanford, California: May 29, 2012. 2012. [April 2013]. director of the FDA's office of in vitro diagnostics. Video available at http://www.youtube.com/watch?v=32uqVqbBvIQ&feature=youtu.be. [Google Scholar]
- 16.Ray T. Amid ‘chaos,’ FDA's Gutierrez offers insights on agency's regulatory stance on molecular tests. [April 2013];GenomeWeb. 2013 Feb 13; Available at http://www.genomeweb.com/clinical-genomics/amid-chaos-fdas-gutierrez-offers-insights-agencys-regulatory-stance-molecular-te.
- 17.Benn PA, Chapman AR. Ethical challenges in providing noninvasive prenatal diagnosis. Curr Opin Obstet Gynecol. 2010;22(2):128–34. doi: 10.1097/GCO.0b013e3283372352. [DOI] [PubMed] [Google Scholar]
- 18.Benn PA, Chapman AR. Practical and ethical considerations of noninvasive prenatal diagnosis. JAMA. 2009;301(20):2154–6. doi: 10.1001/jama.2009.707. [DOI] [PubMed] [Google Scholar]
- 19.de Jong A, Dondorp WJ, de Die-Smulders CE, Frints SG, de Wert GM. Non-invasive prenatal testing: Ethical issues explored. Eur J Hum Genet. 2010;18(3):272–7. doi: 10.1038/ejhg.2009.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Jong A, Dondorp WJ, Frints SG, de Die-Smulders CE, de Wert GM. Advances in prenatal screening: The ethical dimension. Nat Rev Genet. 2011;12(9):657–63. doi: 10.1038/nrg3036. [DOI] [PubMed] [Google Scholar]
- 21.ACOG Committee ACOG committee opinion no. 363: Patient testing: Ethical issues in selection and counseling. Obstet Gynecol. 2007;109(4):1021–3. doi: 10.1097/01.AOG.0000263889.07297.d1. [DOI] [PubMed] [Google Scholar]
- 22.Mozersky J, Mennuti MT. Cell-free fetal DNA testing: Who is driving implementation? Genet Med. 2012 doi: 10.1038/gim.2012.156. [DOI] [PubMed] [Google Scholar]
- 23.Sayres LC, Allyse M, Norton ME, Cho MK. Cell-free fetal DNA testing: A pilot study of obstetric healthcare provider attitudes toward clinical implementation. Prenat Diagn. 2011;31(11):1070–6. doi: 10.1002/pd.2835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hill M, Fisher J, Chitty LS, Morris S. Women's and health professionals’ preferences for prenatal tests for down syndrome: A discrete choice experiment to contrast noninvasive prenatal diagnosis with current invasive tests. Genet Med. 2012;14(11):905–913. doi: 10.1038/gim.2012.68. [DOI] [PubMed] [Google Scholar]
- 25.Tischler R, Hudgins L, Blumenfeld YJ, Greely HT, Ormond KE. Noninvasive prenatal diagnosis: Pregnant women's interest and expected uptake. Prenat Diagn. 2011;31(13):1292–9. doi: 10.1002/pd.2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Favre R, Duchange N, Vayssiere C, Kohler M, Bouffard N, Hunsinger MC, et al. How important is consent in maternal serum screening for Down syndrome in France? Information and consent evaluation in maternal serum screening for Down syndrome: A French study. Prenat Diagn. 2007;27(3):197–205. doi: 10.1002/pd.1656. [DOI] [PubMed] [Google Scholar]
- 27.Dahl K, Hvidman L, Jørgensen FS, Kesmodel US. Knowledge of prenatal screening and psychological management of test decisions. Ultrasound Obstet Gynecol. 2011;38(2):152–7. doi: 10.1002/uog.8856. [DOI] [PubMed] [Google Scholar]
- 28.Ormond KE, Banuvar S, Daly A, Iris M, Minogue J, Elias S. Information preferences of high literacy pregnant women regarding informed consent models for genetic carrier screening. Patient Educ Couns. 2009;75(2):244–50. doi: 10.1016/j.pec.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 29.Ahmed S, Bryant LD, Tizro Z, Shickle D. Interpretations of informed choice in antenatal screening: A cross-cultural, q-methodology study. Soc Sci Med. 2012;74(7):997–1004. doi: 10.1016/j.socscimed.2011.12.021. [DOI] [PubMed] [Google Scholar]
- 30.Federman DG, Goyal S, Kamina A, Peduzzi P, Concato J. Informed consent for PSA screening: Does it happen? Eff Clin Pract. 1999;2(4):152–7. [PubMed] [Google Scholar]
- 31.van den Berg M, Timmermans DR, ten Kate LP, van Vugt JM, van der Wal G. Informed decision making in the context of prenatal screening. Patient Educ Couns. 2006;63(1-2):110–7. doi: 10.1016/j.pec.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 32.Sheets KB, Crissman BG, Feist CD, Sell SL, Johnson LR, Donahue KC, et al. Practice guidelines for communicating a prenatal or postnatal diagnosis of Down syndrome: Recommendations of the National Society of Genetic Counselors. J Genet Couns. 2011;20(5):432–41. doi: 10.1007/s10897-011-9375-8. [DOI] [PubMed] [Google Scholar]
- 33.Skotko BG, Kishnani PS, Capone GT. Prenatal diagnosis of Down syndrome: How best to deliver the news. American Journal of Medical Genetics Part A. 2009;149(11):2361–7. doi: 10.1002/ajmg.a.33082. [DOI] [PubMed] [Google Scholar]
- 34.Raz AE. Disability rights, prenatal diagnosis and eugenics: A cross-cultural view. J Genet Couns. 2005;14(3):183–7. doi: 10.1007/s10897-005-0573-0. [DOI] [PubMed] [Google Scholar]
- 35.Markens S, Browner C, Press N. ‘Because of the risks’: How US pregnant women account for refusing prenatal screening. Social Science & Medicine. 1999;49:359–69. doi: 10.1016/s0277-9536(99)00097-0. [DOI] [PubMed] [Google Scholar]
- 36.Lichtenbelt KD, Alizadeh BZ, Scheffer PG, Stoutenbeek P. Schielen PCJI, Page-Christiaens LCML, Schuring-Blom GH. Trends in the utilization of invasive prenatal diagnosis in the Netherlands during 2000-2009. Prenat Diagn. 2011;31(8):765–72. doi: 10.1002/pd.2764. [DOI] [PubMed] [Google Scholar]
- 37.Nakata N, Wang Y, Bhatt S. Trends in prenatal screening and diagnostic testing among women referred for advanced maternal age. Prenat Diagn. 2010;30(3):198–206. doi: 10.1002/pd.2434. [DOI] [PubMed] [Google Scholar]
- 38.Deans Z, Newson AJ. Should non-invasiveness change informed consent procedures for prenatal diagnosis? Health Care Anal. 2011;19(2):122–32. doi: 10.1007/s10728-010-0146-8. [DOI] [PubMed] [Google Scholar]
- 39.King J. And genetic testing for all...The coming revolution in non-invasive prenatal genetic testing. Rutger Law Journal. 2011;42(3):599–658. [Google Scholar]
- 40.Schmitz D, Henn W, Netzer C. Clinical review: Commentary: No risk, no objections? Ethical pitfalls of cell-free fetal DNA and RNA testing. BMJ. 2009;339:b2690. doi: 10.1136/bmj.b2690. [DOI] [PubMed] [Google Scholar]
- 41.van den Heuvel A, Chitty L, Dormandy E, Newson A, Deans Z, Attwood S, et al. Will the introduction of non-invasive prenatal diagnostic testing erode informed choices? An experimental study of health care professionals. Patient Educ Couns. 2010;78(1):24–8. doi: 10.1016/j.pec.2009.05.014. [DOI] [PubMed] [Google Scholar]
- 42.Newson AJ. Ethical aspects arising from non-invasive fetal diagnosis. Semin Fetal Neonatal Med. 2008;13(2):103–8. doi: 10.1016/j.siny.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 43.Utah Department of Health Preconception health and health care among Utah women. [April 2013];PRAMS Perspective: A Pregnancy Risk Assessment Monitoring System Report. 2008 Available at http://utah.ptfs.com/awweb/awarchive?item=16003.
- 44.Skotko BG, Levine SP, Goldstein R. Self-perceptions from people with Down syndrome. Am J Med Genet A. 2011;155A(10):2360–9. doi: 10.1002/ajmg.a.34235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Skotko BG, Levine SP, Goldstein R. Having a son or daughter with Down syndrome: Perspectives from mothers and fathers. Am J Med Genet A. 2011;155A(10):2335–47. doi: 10.1002/ajmg.a.34293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.US Congress Prenatally and postnatally diagnosed conditions awareness act. 2007 doi: 10.1002/pd.2304. [DOI] [PubMed] [Google Scholar]
- 47.Kitzman JO, Snyder MW, Ventura M, Lewis AP, Qiu R, Simmons LE, et al. Noninvasive whole-genome sequencing of a human fetus. Sci Transl Med. 2012;4(137):137ra76. doi: 10.1126/scitranslmed.3004323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fan C, Quake S. In principle method for noninvasive determination of the fetal genome. Nature Precedings. 2010 [Google Scholar]
- 49.Lo YM, Chan KC, Sun H, Chen EZ, Jiang P, Lun FM, et al. Maternal plasma DNA sequencing reveals the genome-wide genetic and mutational profile of the fetus. Sci Transl Med. 2010;2(61):61ra91. doi: 10.1126/scitranslmed.3001720. [DOI] [PubMed] [Google Scholar]
- 50.Cho MK. Understanding incidental findings in the context of genetics and genomics. J Law Med Ethics. 2008;36(2):280–5. 212. doi: 10.1111/j.1748-720X.2008.00270.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ravitsky V, Wilfond BS. Disclosing individual genetic results to research participants. American Journal of Bioethics. 2006;6:8–17. doi: 10.1080/15265160600934772. [DOI] [PubMed] [Google Scholar]
- 52.Caulfield T, McGuire AL, Cho M, Buchanan JA, Burgess MM, Danilczyk U, et al. Research ethics recommendations for whole-genome research: Consensus statement. PLoS Biol. 2008;6(3):e73. doi: 10.1371/journal.pbio.0060073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McGuire AL, Lupski JR. Personal genome research: What should the participant be told? Trends in Genetics. 2010;26(5):199–201. doi: 10.1016/j.tig.2009.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fabsitz RR, McGuire A, Sharp RR, Puggal M, Beskow LM, Biesecker LG, et al. Ethical and practical guidelines for reporting genetic research results to study participants: Updated guidelines from a national heart, lung, and blood institute working group. Circ Cardiovasc Genet. 2010;3(6):574–80. doi: 10.1161/CIRCGENETICS.110.958827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Boyce A, Borry P. Parental authority, future autonomy, and assessing risks of predictive genetic testing in minors. Journal of Bioethical Inquiry. 2009;6(3):379–85. [Google Scholar]
- 56.Department of Health and Human Services [April 2013];Direct-to-Consumer genetic testing: Reporting of the secretary's advisory committee on genetics, health and society. 2010 Available at http://oba.od.nih.gov/oba/sacghs/reports/SACGHS DTC Report 2010.pdf.
- 57.Caulfield T, McGuire AL. Direct-to-Consumer genetic testing: Perceptions, problems, and policy responses. Annu Rev Med. 2012;63:23–33. doi: 10.1146/annurev-med-062110-123753. [DOI] [PubMed] [Google Scholar]
- 58.Kutz G. Direct-to-Consumer genetic tests: Misleading test results are further complicated by deceptive marketing and other questionable practices: Congressional testimony. DIANE Publishing; 2010. [Google Scholar]
- 59.Hogarth S, Javitt G, Melzer D. The current landscape for direct-to-consumer genetic testing: Legal, ethical, and policy issues. Annu Rev Genomics Hum Genet. 2008;9:161–82. doi: 10.1146/annurev.genom.9.081307.164319. [DOI] [PubMed] [Google Scholar]
- 60.Solberg LB. Over the counter but under the radar: Direct-to-Consumer genetics tests and FDA regulation of medical devices. Vand. J. Ent. & Tech. L. 2009;11:711–1141. [Google Scholar]
- 61.Department of Health and Human Services U.S. System of oversight of genetic testing: A response to the charge of the secretary of health and human services, report of the secretary's advisory committee on genetics, health and human services. 2008 Apr 29; [Google Scholar]
- 62.Cho MK, Arruda M, Holtzman NA. Educational material about genetic tests: Does it provide key information for patients and practitioners? American Journal of Medical Genetics. 1997;73(3):314–20. doi: 10.1002/(sici)1096-8628(19971219)73:3<314::aid-ajmg16>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 63.Bearder vs. State of minnesota. No. A10-101(Minnesota Supreme Court) 2010 [Google Scholar]
- 64.Tarini BA. Storage and use of residual newborn screening blood spots: A public policy emergency. Genet Med. 2011;13(7):619–20. doi: 10.1097/GIM.0b013e31822176df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Drabiak-Syed K. Legal regulation of banking newborn blood spots for research: How Bearder and Beleno resolved the question of consent. Hous. J. Health L. & Pol'y. 2011;11:1–149. [Google Scholar]
- 66.Beleno V. Tex. Dept. Of State Health Servs., No. SA-09-CA-188-FB (W.D. Tex.) 2009. [Google Scholar]
- 67.Tobin SL, Cho MK, Lee SS, Magnus DC, Allyse M, Ormond KE, Garrison NA. Customers or research participants?: Guidance for research practices in commercialization of personal genomics. Genet Med. 2012;14(12):833–835. doi: 10.1038/gim.2012.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sayres L, Goodspeed T, Allyse M, Cho MK. In the public interest? Sci Transl Med. 2012;4(144):144fs23. doi: 10.1126/scitranslmed.3003612. [DOI] [PubMed] [Google Scholar]
- 69.Cho M. Patently unpatentable: Implications of the Myriad court decision on genetic diagnostics. Trends Biotechnol. 2010;28(11):548–51. doi: 10.1016/j.tibtech.2010.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]