Abstract
Context
Although many previous studies have examined the preference of patients for different pain measurement scales, preference for anchor descriptors has not been thoroughly discussed.
Objectives
To examine (1) the preferred end-phrases used in the VAS as anchor labels for Japanese patients with chronic pain, and (2) whether the preference differs according to factors such as age, sex, educational level, duration of pain, and pain intensity.
Methods
We performed an observational study in patients suffering from non-cancer chronic pain for more than 3 months at a pain center in Japan. The patients were asked to rate their pain intensity using four types of VAS that used the following different anchor descriptors: “worst pain” (“Worst”), “worst pain bearable” (“Bearable”), “worst pain imaginable” (“Imaginable”), and “worst pain you have ever experienced” (“Experienced”). They were also asked to rank the four scales according to ease of responding, and asked which descriptor best reflected their perceived pain.
Results
In total, 183 patients participated in the study. They consisted of 119 (65.0%) women and 64 (35.0%) men aged 18–84 years with the mean age of 56.9 years. “Experienced” was most preferred (69.8%), followed by “Bearable” (66.3%), “Worst” (48.8%), and “Imaginable” (16.9%). Factors such as age, sex, educational background, duration of pain, and pain intensity did not significantly affect the results. In 83.1% of patients, the preferred descriptor corresponded to the descriptor that best reflected patients' perceived pain.
Conclusion
The frequently used expression “worst pain imaginable” is considered to be difficult to understand for most patients. Widely preferred descriptors, such as “worst pain you have ever experienced” and “worst pain bearable”, should be used when evaluating perceived pain. The preference of anchor descriptors was not significantly affected by the factors such as age, sex, educational level, duration of pain, and pain intensity.
Introduction
The International Association for the Study of Pain (IASP) states that “Pain is always subjective. Each individual learns the application of the word through experiences related to injury in early life” [1]. Pain is thus an individual experience with multi-dimensional aspects [2]–[4], and, theoretically speaking, pain intensity is impossible to measure objectively and quantitatively [5]. However, accurate quantitative evaluation of perceived pain intensity is a prerequisite for both clinical practice and research purposes [5]–[8].
Over the past few decades, several self-reporting unidimensional pain scales have been developed, such as the Visual Analogue Scale (VAS), Numerical Rating Scale (NRS), Verbal Rating Scale (VRS), and the Faces Pain Scale. Of these scales, the VAS and NRS have been used most frequently worldwide because of their outstanding simplicity, and their reliability and validity have been proved [6]–[10]. These scales are designed to measure pain intensity using extremely painful conditions or situations as a point of reference. However, many descriptors have been used as anchor labels with the VAS and NRS in Japanese as well as other languages, and these descriptors have not yet been standardized [11]. Pain intensity cannot be precisely compared without using standardized anchor descriptors, even if the same pain measurement scale is used.
Several studies have investigated the preferred pain assessment tool among the VAS, NRS, VRS, and so on [8], [12]–[16]. However, very few researchers have paid attention to the descriptors used as anchor labels. Many studies have recommended the use of the NRS [6], [12], [17]–[25] and VAS [14], [26]–[28] to evaluate pain intensity; nevertheless, patients are sometimes unable to use these scales to correctly rate their perceived pain intensity in clinical and research settings. Some studies have shown that categorical scales such as the VRS are preferred over the VAS or NRS by elderly patients [2], [8], [14], [29], less educated patients [13], cognitively impaired patients [30], and children [31]. These results might be due not only to difficulties with abstract thinking [2], [30]–[32] but also to the ambiguity of anchor descriptors used in the VAS or NRS. Because appropriate quantitative evaluation of patients' pain intensity requires the patients to be able to obtain a clear image of the situations described in the anchor label, investigation of preferred anchor descriptors is expected to contribute to the improvement of pain intensity evaluations.
The two major purposes of this study are to examine (1) the preferred end-phrases used in the VAS as anchor labels for Japanese patients with chronic pain, and (2) whether the preference differs according to factors such as age, sex, educational level, duration of pain, and pain intensity.
Methods
Participants
The subjects for this study were recruited from chronic pain patients who attended the multi-disciplinary outpatient pain clinic of the Jikei University Hospital between June 2012 and May 2013. Most of the patients who attend the clinic were suffering from multiple types of chronic pain. The clinic consists of doctors, nurses, physiotherapists, clinical psychologists, and acupuncturists. The patients were basically treated with medication, therapeutic exercise, psychophysiological approach, and acupuncture. Inclusion criteria were a diagnosis of chronic non-cancer pain with a duration of more than 3 months and age 18 years or older. Patients who had visual disturbance, were unable to speak Japanese, or were suspected to have impaired cognition (Mini-Mental State Examination (MMSE) score < 23 points) were excluded.
Anchor descriptors
The following four commonly used descriptors of the anchor labels used in the VAS in Japan were selected.
“worst pain” (hereafter “Worst”)
“worst pain bearable” (hereafter “Bearable”)
“worst pain imaginable” (hereafter “Imaginable”)
“worst pain you have ever experienced” (hereafter “Experienced”)
An American psychologist who was proficient in Japanese validated the translations of anchor descriptors used in Japanese to make sure that they were consistent with the expressions used in English [11].
Questionnaire
A traditional VAS with a straight, horizontal 10-cm line was used, with the anchor label “no pain” at the left side and one of the translated Japanese descriptors at the right side. The four different VASs were placed on a sheet of paper in fixed order. The participants were asked to mark a vertical line on each VAS corresponding to their perceived average pain during the previous 24 hours. The participants were also asked to rank the scales in order of preference, from first to fourth place, on the basis of ease of responding, and they were also asked which descriptor best expressed their own pain.
Ethics Statement
The protocol of this study was approved by the ethics committees of the Jikei University Hospital, and the study was carried out in accordance with the Declaration of Helsinki. Written informed consent was obtained before study entry from all patients who participated in the study.
Data collection
The questionnaire written in Japanese was distributed to the participants when they gave consent after attending the pain clinic, and was collected on the same day. Age, sex, educational background, duration of pain, VAS, VRS, Hospital Anxiety and Depression Scale (HADS) [33]–[34], and Pain Catastrophizing Scale (PCS) score [35] data, which were administered on the same day, were obtained from medical records. Because the participants of this study are from the multi-disciplinary pain clinic, it is expected that their psychological factors have severely influenced on their pain condition. Therefore, we used HADS and PCS to verify that we could regard the participants to be the representatives of chronic pain patients in Japan. HADS includes two subscales which are anxiety and depression. The total score of each subscale is 21. The cut-off point of the each subscale of HADS is usually set as 8 and 11. The point between 8 and 10 indicates that the patient probably has anxiety or depression; the point of 11 and over definitely has anxiety or depression. The cut-off point of PCS is usually set as 30. The point of 30 and over indicates that the patient is in pain catastrophizing state.
Statistical analysis
All data were analyzed statistically using the SPSS program (version 21.0, SPSS Inc., Chicago, IL, USA). Data treated as a continuous scale are presented as median and range, and categorical and ordinal data are presented as counts and percentages. Wilcoxon signed-rank test and chisquare test was used to compare the values and proportions between elderly and young group (Table 1). Chisquare test was applied to compare the proportions of preference between two groups (Table 2).
Table 1. General characteristics of study participants (n = 183).
| Total (n = 183) | Elderly (n = 87) | Young (n = 96) | p-value | |
| Age, years | 59 (18–84) | 69 (61–84) | 46 (18–60) | < 0.0001** |
| 10–19 | 1 (0.6) | |||
| 20–29 | 9 (4.9) | |||
| 30–39 | 17 (9.3) | |||
| 40–49 | 33 (18.0) | |||
| 50–59 | 32 (17.5) | |||
| 60–69 | 49 (26.8) | |||
| 70–79 | 34 (18.6) | |||
| 80- | 8 (4.4) | |||
| Sex | 0.42 | |||
| Female | 119 (65.0) | 54 (62.1) | 65 (67.7) | |
| Male | 64 (35.0) | 33 (37.9) | 31 (32.3) | |
| Educational level | 0.03* | |||
| Junior high school | 12 (6.8) | 7 (8.5) | 5 (5.3) | |
| High school | 79 (44.6) | 44 (53.7) | 35 (36.8) | |
| College/University | 86 (48.6) | 31 (37.8) | 55 (57.9) | |
| Duration of pain, months | 36 (3–480) | 40 (3–240) | 33 (3–480) | 0.82 |
| HADS (Anxiety) | 7 (0–16) | 7 (0–15) | 7 (0–16) | 0.31 |
| HADS (Depression) | 7 (0–20) | 7 (0–17) | 8 (0–20) | 0.35 |
| PCS | 32.5 (7–51) | 32 (9–51) | 33 (7–50) | 0.58 |
| VRS | 0.27 | |||
| None | 3 (1.7) | 2 (2.3) | 1 (1.1) | |
| Mild | 62 (34.3) | 25 (29.1) | 37 (38.9) | |
| Moderate | 96 (53.0) | 45 (52.3) | 51 (53.7) | |
| Severe | 20 (11.0) | 14 (16.3) | 6 (6.3) | |
| VAS ("Worst") | 59 (0–100) | 65 (0–100) | 55 (2–100) | 0.27 |
| VAS ("Bearable") | 61 (0–100) | 59 (0–100) | 61.5 (2–100) | 0.70 |
| VAS ("Imaginable") | 58 (0–100) | 68 (0–100) | 51 (0–100) | 0.03** |
| VAS ("Experienced") | 66 (0–100) | 73 (0–100) | 55.5 (0–100) | < 0.01** |
Values are expressed as the median (range) or as number (percentage).
HADS = Hospital Anxiety and Depression Scale; PCS = Pain Catastrophizing Scale;
VRS = Verbal Rating Scale; VAS = Visual Analogue Scale
chi-square test statistically significant (p<0.05).
Wilcoxon rank sum test statistically significant (p<0.05).
Table 2. Percentage of participants who considered each descriptor as preferable (sum of 1st and 2nd place).
| A ("Worst") | B ("Bearable") | C ("Imaginable") | D ("Experienced") | p-value | |
| All (n = 183) | 48.8% | 66.3% | 16.9% | 69.8% | |
| Young (n = 96) | 46.2% | 66.3% | 13.2% | 75.0% | |
| 0.41 | |||||
| Elderly (n = 87) | 51.9% | 66.3% | 21.0% | 63.8% | |
| Low education (n = 91) | 47.8% | 60.4% | 20.9% | 72.8% | |
| 0.34 | |||||
| High education (n = 86) | 50.0% | 72.8% | 12.3% | 66.3% | |
| Female (n = 119) | 52.2% | 62.8% | 17.5% | 69.3% | |
| 0.74 | |||||
| Male (n = 64) | 42.4% | 72.9% | 15.5% | 70.7% | |
| Short duration (n = 94) | 48.9% | 66.7% | 14.6% | 71.9% | |
| 0.87 | |||||
| Long duration(n = 89) | 48.8% | 65.9% | 19.3% | 67.5% | |
| Low pain intensity (n = 65) | 55.0% | 63.9% | 18.3% | 67.2% | |
| 0.87 | |||||
| High pain intensity (n = 116) | 45.3% | 67.6% | 17.0% | 70.5% |
Elderly, older than 60 years; Young, 60 years or younger;
Low education, junior high school or high school only; high education, college/university or graduate school;
Short duration, thirty six months or less; Long duration, more than thirty six months;
Low pain intensity, sum of "none" and "mild"; High pain intensity, sum of "moderate" and "severe" of Verbal Rating Scale (VRS)
Friedman test was used for analyzing the differences in preference among the different descriptors (Figure 1). Bonferroni correction was employed for post-hoc comparison of each pair. Wilcoxon signed-rank test was used for analyzing the relationship between the most-preferred descriptor and best-expressing descriptor (Figure 2). Spearman's rank correlation coefficient was calculated to examine whether the reported VAS pain levels using the different anchor descriptors correlate with each other (Table 3). Wilcoxon signed-rank test of the VAS values between the most-preferred descriptor and the least-preferred descriptor, was also performed to examine if the reported pain level significantly differed depending on the anchor descriptor. P-values less than 0.05 were considered statistically significant.
Figure 1. Preference of VAS with the four different descriptors.
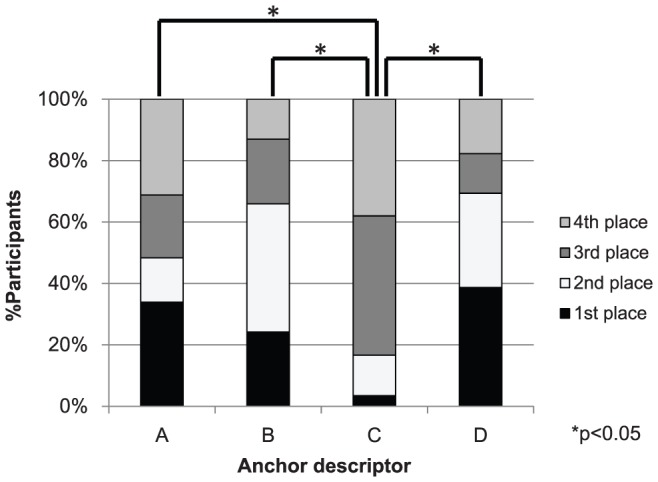
Friedman test demonstrated a significant difference between the four different descriptors (p<0.001); Bonferroni's post-hoc tests demonstrated significant differences between “Imaginable” and “Worst”, “Bearable”, and “Experienced” (p<0.05). A: worst pain (“Worst”). B: worst pain bearable (“Bearable”). C: worst pain imaginable (“Imaginable”). D: worst pain you have ever experienced (“Experienced”).
Figure 2. Comparison of percentages between the most-preferred and best-expressing descriptor.
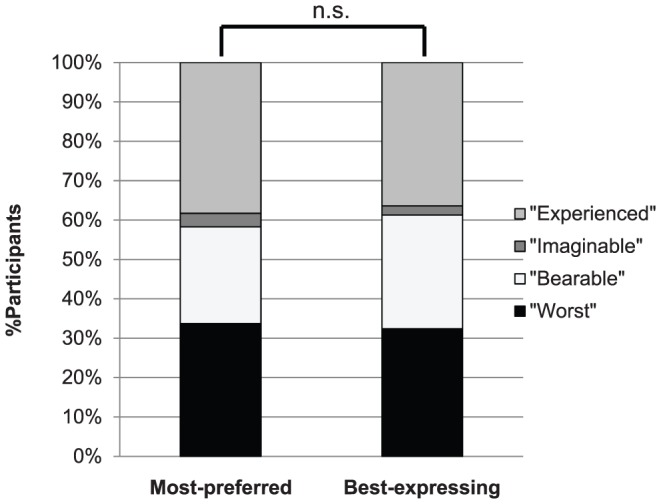
n.s., not significant; Wilcoxon's signed rank test, “Worst”: worst pain, “Bearable”: worst pain bearable, “Imaginable”: worst pain imaginable, “Experienced”: worst pain you have ever experienced.
Table 3. Pairwise Spearman's rank correlation coefficient between the pain intensity measured by VASs using four anchor descriptors.
| A | B | C | D | |
| A ("Worst") | - | |||
| B ("Bearable") | 0.79* | - | ||
| C ("Imaginable") | 0.82* | 0.78* | - | |
| D ("Experienced") | 0.81* | 0.77* | 0.87* | - |
* Spearman's rank correlation coefficient statistically significant (p<0.05).
Results
One hundred and eighty-three patients gave consent to participate in the study. Table 1 shows the demographic characteristics of study participants. Almost all of the participants were able to answer the VASs with four different descriptors; only four participants failed to mark at least one of the four VASs. The HADS score suggested that 27.9% of the respondents were in a depressive state, and 26.8% had anxiety. The PCS score indicated that 60.1% of the respondents were catastrophized.
Table 4 shows the characteristics of the participants' pain (some patients have multiple nature of pain). The majority of the participants are suffering from some of musculoskeletal pain.
Table 4. Characteristics of pain (n = 183).
| n | |
| Diagnosis | |
| Myofascial pain | 132 |
| Peripheral neuropathy | 19 |
| Spinal degenerative disease | 19 |
| Sacroiliac joint dysfunction | 18 |
| Failed back syndrome | 12 |
| Post-operative pain | 9 |
| Postherpetic neuralgia | 8 |
| Arthritis | 7 |
| Other spinal diseases | 6 |
| Complex regional pain syndrome | 4 |
| Fibromyalgia | 3 |
| Non-specific low back pain | 3 |
| Trigeminal neuralgia | 3 |
| Headache | 2 |
| Type of pain | |
| Nociceptive | 185 |
| Neuropathic | 50 |
| Mixed | 31 |
| Site of pain | |
| Face, head, and neck | 44 |
| Shoulder and upper extremities | 40 |
| Chest and abdomen | 16 |
| Back | 25 |
| Lumber and buttock | 65 |
| Inguinal region and lower extremities | 60 |
| Others | 5 |
Figure 1 shows the rankings given to the four different descriptors used with the VASs in this study. “Experienced” was most preferred by the largest number of participants (38.5%), followed by “Worst” (33.9%), “Bearable” (24.1%), and “Imaginable” (3.4%). The descriptor ranked as least preferred by most participants was “Imaginable” (38.2%), followed by “Worst” (31.2%), “Experienced” (17.6%), and “Bearable” (12.9%). Friedman test demonstrated the differences among the four different descriptors to be statistically significant (p<0.001); Bonferroni post-hoc tests demonstrated significant differences between “Imaginable” and “Worst”, “Bearable”, and “Experienced” (p<0.05).
Figure 2 compares percentages between the most-preferred and the best-expressing descriptor. Overall, 83.1% of the descriptors were consistent with each other.
Table 2 shows the percentage of participants that ranked each of the descriptors first or second in terms of preference. “Experienced” and “Bearable” were regarded as preferable by 69.8% and 66.3% of the participants, respectively. Almost half of the participants regarded “Worst” as preferable; “Imaginable” was regarded as preferable by only 16.9% of the participants. As Table 2 shows, approximately the same percentage of preference was observed even when the participants were stratified by age, sex, educational level, duration of pain, and pain intensity, with p-values, analyzed by chi-square test, of 0.41, 0.34, 0.74, 0.87, and 0.87, respectively. Table 3 shows pairwise Spearman's rank correlation coefficient between the pain intensity measured by VASs using the four anchor descriptors. The Spearman's rank correlation coefficient indicated that there were strong correlations between each pair of the anchor descriptors. There was a significant difference between the VAS values with the most-preferred descriptor and the least-preferred descriptor, analyzed by Wilcoxon signed-rank test, with the p-value of 0.038.
Discussion
The key findings of this study are that (1) Japanese patients with chronic pain show a certain preference concerning the anchor descriptors of extremes; (2) most participants found that one descriptor was both easy to answer and best described their own pain; and (3) preference is not significantly influenced by factors such as age, sex, educational background, duration of pain, and pain intensity of the patient.
Comparison of preference among different anchor descriptors
We found in this study that Japanese patients with chronic pain show a certain preference concerning the descriptors of extremes (Figure 1). The participants preferred “Experienced” and “Bearable” over the other two descriptors, while “Imaginable” was preferred significantly less often than the other descriptors. “Experienced” represents the “real” pain that an individual has actually experienced; almost all individuals, except for some who may have forgotten episodes of severe pain, should be able to remember and imagine such pain. One plausible explanation for the high preference of the descriptors “Experienced” and “Bearable” is that they are relatively easy to relate to.
On the other hand, “Imaginable” required the participants to imagine unexperienced pain, making it difficult to create a concrete image. Some participants mentioned that rather than imagining unexperienced pain, they remembered pain episodes that they had actually experienced.
Interestingly, approximately half of the participants regarded “Worst” as preferable and half as not preferable. Some participants interpreted “the worst pain imaginable” to mean pain they had experienced, while others interpreted this to mean unexperienced pain. The IASP defines pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage” [1]. “Worst” seems to involve affective and emotional aspects more than the other three descriptors, which may have influenced participants' preference.
We also found in this study that participants tended to regard one descriptor as both easy to answer and best to describe their own pain. We defined “preference” as easiest to answer in this study. Peters et al. found that there was little difference between the scales that patients regarded as best describing, “most easy”, and “preferred” [8]. Similarly, our results suggest that the anchor label that best described participants' own pain tended to be the one they answered most easily.
As Table 3 showed, the anchor descriptor did not have a great influence on VAS values of the whole group. However, the result of the Wilcoxon signed-rank test indicated that preference of the anchor descriptor could affect the intra-personal pain intensity. Therefore, the easiest descriptor for each patient to understand should be used to evaluate that patient's pain accurately. Moreover, we had probably better not to use the less preferred anchor descriptor, such as “worst pain imaginable” to obtain precise data.
Comparison of preference by subgroups
Although Table 2 shows that participants who were female, younger, and had a low level of education tended to prefer “Experienced” to “Bearable” and, conversely, that male, older, and highly educated participants tended to prefer “Bearable” to “Experienced”, the effect of these factors did not reach statistical significance. Previous studies have found that sex influenced the preference of pain scales to a certain extent [8], [14]–[15]. In any case, the percentage of participants that considered “Experienced” to be preferable was similar to the percentage that preferred “Bearable”. On the other hand, few participants preferred “Imaginable”, and the rank of preference of “Worst” and “Imaginable” did not differ according to subcategories. One plausible explanation is that some patients may have difficulty with the abstract concepts of inexperienced pain such as “Worst” and “Imaginable”.
Although “Imaginable” is a frequently used descriptor in Japan, its use as an anchor label in pain measurement may not provide an appropriate evaluation, because “preference” was defined as ease in understanding or answering in this study. Therefore, we consider it more suitable to use descriptors such as “Experienced” or “Bearable” for the evaluation of pain intensity in Japanese patients with chronic pain.
Many previous studies have investigated the preferences of patients for pain assessment tools. However, to the best of our knowledge, very few studies have dealt with the preference for anchor labels. Hjermstad et al.’s review article concerning pain intensity assessment tools written in English reports the use of 24 different descriptors in 239 papers with the VAS and NRS [11]. Thus, a range of non-standardized descriptors are used to evaluate pain intensity both domestically and internationally. Our study indicates that the preference of patients for descriptors can determine how precisely patients are able to communicate their perceived pain intensity.
These results suggest that anchor descriptors should be standardized as soon as possible for more appropriate evaluation of pain intensity. The findings from this study can contribute to more accurate assessment of the intensity of chronic pain. It should be noted that the participants in this study were from a limited population and that factors such as race, ethnicity, and culture are also known to influence pain perception [36]. To what extent our results extend to patients from other racial and cultural backgrounds is unclear and requires further study.
Study limitations
This study has several limitations. First, patients with other types of pain, such as acute pain and cancer pain, were not included. It remains to be clarified whether the findings from this study can be generalized to all Japanese patients.
Second, participants in this study attended a multi-disciplinary pain clinic, introducing a probable selection bias. However, the range of pain intensity measured by the VAS and VRS, as well as psychometric factors such as the HADS and PCS, were distributed widely, so the participants can be considered to represent common Japanese chronic pain patients.
Third, the meaning of the descriptors in Japanese might not necessarily correspond exactly to their English counterparts. However, as the translated descriptors were checked by an American psychologist who is proficient in Japanese, we do not consider this to be a serious problem.
Conclusions
The result of this study indicate that “worst pain you have ever experienced” and “worst pain bearable” are appropriate descriptors for Japanese chronic pain patients. “Worst pain imaginable”, though it is frequently used worldwide, may be inappropriate for evaluating pain intensity, at least among Japanese chronic pain patients. Widely preferred descriptors, i.e., most patients can respond without difficulty, should be used when evaluating perceived pain.
The preference of anchor descriptors was not significantly affected by the factors such as such as age, sex, educational level, duration of pain, and pain intensity.
Acknowledgments
We would like to thank Keiko Kojima, Shumpei Kitamura, Makihiko Hirabayashi, Fumitaka Matsuno, and Jin Shinohara for data collection.
We very much appreciate all the patients who participated in this study.
Funding Statement
The authors have no support or funding to report.
References
- 1.Taxonomy ITFo (1994) Part III: Pain Terms: A Current List with Definitions and Notes on Usage. In: Merskey H, Bogduk N, editors. Classification of Chronic Pain. 2nd ed. Seattle: IASP Press. pp. 209–214. [Google Scholar]
- 2. Kremer E, Atkinson JH, Ignelzi RJ (1981) Measurement of pain: patient preference does not confound pain measurement. Pain 10: 241–248. [DOI] [PubMed] [Google Scholar]
- 3.Melzack R, Katz J (2006) Pain assessment in adult patients. In: McMahon SB, Klotzenburg M, editors. Wall and Melzack's Textbook of Pain. 5th ed. Philadelphia: Elsevier. pp. 291–304. [Google Scholar]
- 4.McQuay HJ, Moore A (2006) Methods of therapeutic trials. In: McMahon SB, Klotzenburg M, editors. Wall and Melzack's Textbook of Pain. 5th ed. Philadelphia: Elsevier. pp. 415–425. [Google Scholar]
- 5. Loder E, Burch R (2012) Measuring pain intensity in headache trials: which scale to use? Cephalalgia 32: 179–182. [DOI] [PubMed] [Google Scholar]
- 6. Jensen MP, Karoly P, Braver S (1986) The measurement of clinical pain intensity: a comparison of six methods. Pain 27: 117–126. [DOI] [PubMed] [Google Scholar]
- 7. Flaherty SA (1996) Pain measurement tools for clinical practice and research. AANA J 64: 133–140. [PubMed] [Google Scholar]
- 8. Peters ML, Patijn J, Lamé I (2007) Pain assessment in younger and older pain patients: psychometric properties and patient preference of five commonly used measures of pain intensity. Pain Med 8: 601–610. [DOI] [PubMed] [Google Scholar]
- 9. Carlsson AM (1983) Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain 16: 87–101. [DOI] [PubMed] [Google Scholar]
- 10. Langley GB, Sheppeard H (1985) The visual analogue scale: its use in pain measurement. Rheumatol Int 5: 145–148. [DOI] [PubMed] [Google Scholar]
- 11. Hjermstad MJ, Fayers PM, Haugen DF, Caraceni A (2011) European Palliative Care Research Collaborative (EPCRC), (2011) et al. Studies comparing Numerical Rating Scales, Verbal Rating Scales, and Visual Analogue Scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage 41: 1073–1093. [DOI] [PubMed] [Google Scholar]
- 12. Rodriguez CS, McMillan S, Yarandi H (2004) Pain measurement in older adults with head and neck cancer and communication impairments. Cancer Nurs 27: 425–433. [DOI] [PubMed] [Google Scholar]
- 13. Clark P, Lavielle P, Martínez H (2003) Learning from pain scales: patient perspective. J Rheumatol 30: 1584–1588. [PubMed] [Google Scholar]
- 14. Herr KA, Mobily PR (1993) Comparison of selected pain assessment tools for use with the elderly. Appl Nurs Res 6: 39–46. [DOI] [PubMed] [Google Scholar]
- 15. Herr KA, Spratt K, Mobily PR, Richardson G (2004) Pain intensity assessment in older adults: use of experimental pain to compare psychometric properties and usability of selected pain scales with younger adults. Clin J Pain 20: 207–219. [DOI] [PubMed] [Google Scholar]
- 16. de C Williams AC, Davies HT, Chadury Y (2000) Simple pain rating scales hide complex idiosyncratic meanings. Pain 85: 457–463. [DOI] [PubMed] [Google Scholar]
- 17. Paice JA, Cohen FL (1997) Validity of a verbally administered numeric rating scale to measure cancer pain intensity. Cancer Nurs 20: 88–93. [DOI] [PubMed] [Google Scholar]
- 18. Gagliese L, Weizblit N, Ellis W, Chan VW (2005) The measurement of postoperative pain: a comparison of intensity scales in younger and older surgical patients. Pain 117: 412–420. [DOI] [PubMed] [Google Scholar]
- 19. Berthier F, Potel G, Leconte P, Touze MD, Baron D (1998) Comparative study of methods of measuring acute pain intensity in an ED. Am J Emerg Med 16: 132–136. [DOI] [PubMed] [Google Scholar]
- 20. Marquie L, Duarte LR, Marine C, Lauque D, Sorum PC (2008) How patients and physicians rate patients' pain in a French emergency department using a verbally administered numerical rating scale and a visual analog scale. Acute Pain 10: 31–37. [Google Scholar]
- 21. Brunelli C, Zecca E, Martini C, Campa T, Fagnoni E, et al. (2010) Comparison of numerical and verbal rating scales to measure pain exacerbations in patients with chronic cancer pain. Health Qual Life Outcomes 8: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, et al. (1978) Studies with pain rating scales. Ann Rheum Dis 37: 378–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bolton JE, Wilkinson RC (1998) Responsiveness of pain scales: a comparison of three pain intensity measures in chiropractic patients. J Manipulative Physiol Ther 21: 1–7. [PubMed] [Google Scholar]
- 24. Grotle M, Brox JI, Vollestad NK (2004) Concurrent comparison of responsiveness in pain and functional status measurements used for patients with low back pain. Spine (Phila Pa 1976) 29: E492–501. [DOI] [PubMed] [Google Scholar]
- 25. Larroy C (2002) Comparing visual-analog and numeric scales for assessing menstrual pain. Behav Med 27: 179–181. [DOI] [PubMed] [Google Scholar]
- 26. Seymour RA (1982) The use of pain scales in assessing the efficacy of analgesics in post-operative dental pain. Eur J Clin Pharmacol 23: 441–444. [DOI] [PubMed] [Google Scholar]
- 27. Price DD, Bush FM, Long S, Harkins SW (1994) A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain 56: 217–226. [DOI] [PubMed] [Google Scholar]
- 28. Skovlund E, Bretthauer M, Grotmol T, Larsen IK, Hoff G (2005) Sensitivity of pain rating scales in an endoscopy trial. Clin J Pain 21: 292–296. [DOI] [PubMed] [Google Scholar]
- 29. Closs SJ, Barr B, Briggs M, Cash K, Seers K (2004) A comparison of five pain assessment scales for nursing home residents with varying degrees of cognitive impairment. J Pain Symptom Manage 27: 196–205. [DOI] [PubMed] [Google Scholar]
- 30. Radbruch L, Sabatowski R, Loick G, Jonen-Thielemann I, Kasper M, et al. (2000) Cognitive impairment and its influence on pain and symptom assessment in a palliative care unit: development of a Minimal Documentation System. Palliat Med 14: 266–276. [DOI] [PubMed] [Google Scholar]
- 31. Fanurik D, Koh JL, Harrison RD, Conrad TM, Tomerlin C (1998) Pain assessment in children with cognitive impairment. An exploration of self-report skills. Clin Nurs Res 7: 103–119 discussion 120–124. [DOI] [PubMed] [Google Scholar]
- 32. Gabre P, Sjöquist K (2002) Experience and assessment of pain in individuals with cognitive impairments. Spec Care Dentist 22: 174–180. [DOI] [PubMed] [Google Scholar]
- 33. Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67: 361–370. [DOI] [PubMed] [Google Scholar]
- 34. Bjelland I, Dahl AA, Haug TT, Neckelmann D (2002) The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 52: 69–77. [DOI] [PubMed] [Google Scholar]
- 35. Sullivan MJ, Bishop SR, Pivik J (1995) The Pain Catastrophizing Scale: Development and Validation. Psychological Assessment 7: 524–532. [Google Scholar]
- 36. Rahim-Williams B, Riley JL 3rd, Williams AK, Fillingim RB (2012) A quantitative review of ethnic group differences in experimental pain response: do biology, psychology, and culture matter? Pain Med 13: 522–540. [DOI] [PMC free article] [PubMed] [Google Scholar]


