Polynuclear neutrophils can play dual roles in sepsis: on the one hand they mediate major antimicrobial activities and on the other hand they can contribute to the development of multiple organ failure [1]. Nonetheless, in spite of the importance of these cells in sepsis, the influence of the circulating neutrophil count (CNC) on the prognosis of septic patients with this pathology has not been properly evaluated.
We analyzed the association between CNC and outcome in two cohorts of patients with diagnostic criteria of septic shock (SS) [2]: the first was recruited in the context of a single center study (EXPRESS study, discovery cohort, n = 195; Table 1), and the second in the context of a multi-centric study (GRECIA study, validation cohort, n = 194; Table 2). Written informed consent was obtained from each patient or their legal representative. The two studies were approved by the Research Ethics Committee of the Hospital Clínico Universitario, Valladolid, Spain (for the EXPRESS study) and Hospital Universitario Río Hortega, Valladolid, Spain (coordinating center for the GRECIA study).
Table 1.
Clinical characteristics of the patients in the discovery study in survivors and non-survivors at 28 days
| Total (n = 195) | Survivors (n = 125) | Non-survivors (n = 70) | P | |
|---|---|---|---|---|
|
Patient details |
|
|
|
|
| Gender (male) |
125 (64.1%) |
79 (63.2%) |
46 (65.7%) |
NS |
| Age (years) |
71.6 ± 11.1 |
70.2 ± 11.1 |
74.2 ± 10.7 |
0.014 |
| Hypertension |
109 (55.9%) |
71 (56.8%) |
38 (54.3%) |
NS |
| Cardiovascular disease |
87 (44.6%) |
54 (43.2%) |
33 (47.1%) |
NS |
| Cancer |
44 (22.5%) |
21 (16.8%) |
23 (32.8%) |
0.010 |
| COPD |
33 (16.9%) |
24 (19.2%) |
9 (12.8%) |
NS |
| Diabetes |
31 (15.9%) |
24 (19.2%) |
7 (10%) |
NS |
| Obesity |
32 (16.4%) |
21 (16.8%) |
11 (15.7%) |
NS |
| Smoker |
27 (13.8%) |
17 (13.6%) |
10 (14.2%) |
NS |
| Chronic renal failure |
26 (13.3%) |
15 (12.0%) |
11 (15.7%) |
NS |
| Alcohol abuse |
12 (6.1%) |
8 (6.4%) |
4 (5.7%) |
NS |
| Inmunosuppression |
9 (4.6%) |
5 (4.0%) |
4 (5.7%) |
NS |
| Hepatic disease |
6 (3.1%) |
4 (3.2%) |
2 (2.8%) |
NS |
|
Clinical status at admission |
|
|
|
|
| APACHE II |
14.7 ± 5.9 |
13.9 ± 5.8 |
16.2 ± 5.9 |
0.013 |
| Mechanical ventilation |
134 (68.7%) |
83 (66.4%) |
51 (72.9%) |
NS |
| OARF |
41 (21.0%) |
19 (15.2%) |
22 (31.4%) |
0.008 |
|
Presumed source of infection |
|
|
|
|
| Digestive system |
115 (58.9%) |
76 (60.8%) |
39 (55.7%) |
NS |
| Respiratory system |
19 (9.7%) |
14 (11.2%) |
5 (7.1%) |
NS |
| Central nervous system |
20 (10.2%) |
14 (11.2%) |
6 (8.5%) |
NS |
| Urinary system |
10 (5.1%) |
5 (4.0%) |
5 (7.1%) |
NS |
| Endocardium |
7 (3.5%) |
5 (4.0%) |
2 (2.8%) |
NS |
| Catheter |
34 (17.4%) |
26 (20.8%) |
8 (11.4%) |
NS |
| Wound/skin, soft tissue |
28 (14.3%) |
20 (16.0%) |
8 (11.4%) |
NS |
| Other/unknown |
55 (28.2%) |
35 (28.0%) |
20 (28.5%) |
NS |
|
Type of surgery |
|
|
|
|
| Abdominal |
99 (50.7%) |
56 (44.8%) |
43 (61.4%) |
0.030 |
| Cardiac |
71 (36.4%) |
54 (43.2%) |
17 (24.3%) |
|
| Other |
25 (12.8%) |
15 (12.0%) |
10 (14.3%) |
|
|
Urgent surgery |
|
|
|
|
| Yes |
130 (66.6%) |
77 (61.6)% |
53 (75.7%) |
0.045 |
|
Documented microbial agent |
|
|
|
|
| Gram-negative |
67 (41.6%) |
48 (44.4%) |
19 (35.8%) |
NS |
| Gram-positive |
68 (42.2%) |
47 (43.5%) |
21 (39.6%) |
NS |
| Fungi |
24 (14.9%) |
16 (14.8%) |
8 (15.1%) |
NS |
|
Laboratory data |
|
|
|
|
| Bilirubin (mg/dL) |
1.4 ± 1.3 |
1.5 ± 1.4 |
1.2 ± 1.0 |
NS |
| Glycemia (mg/dL) |
166.4 ± 65.1 |
165.4 ± 58.3 |
168.2 ± 76.0 |
NS |
| Procalcitonin (ng/mL) |
19.3 ± 32.5 |
16.5 ± 28.6 |
24.3 ± 38.1 |
NS |
| CRP (mg/mL) |
231.8 ± 119.2 |
221.9 ± 106.6 |
249.4 ± 138.1 |
NS |
| INR |
1.7 ± 0.9 |
1.6 ± 0.9 |
1.7 ± 0.8 |
NS |
| Platelets (×103/μl) |
190.2 ± 140.0 |
196.9 ± 143.5 |
178.2 ± 133.5 |
NS |
| Leukocytes (×103/μl) |
16.3 ± 10.1 |
16.4 ± 9.0 |
16.2 ± 11.7 |
NS |
| Monocytes (×103/μl) |
0.7 ± 0.4 |
0.7 ± 0.4 |
0.6 ± 0.5 |
NS |
| Lymphocyte (×103/μl) |
1.1 ± 0.7 |
1.1 ± 0.8 |
1.0 ± 0.6 |
NS |
| Neutrophils (×103/μl) |
14.4 ± 9.4 |
14.4 ± 8.4 |
14.3 ± 11.1 |
NS |
| Basophils (×103/μl) |
0.1 ± 0.0 |
0.1 ± 0.1 |
0.1 ± 0.0 |
NS |
| Eosinophils (×103/μl) | 0.1 ± 0.0 | 0.1 ± 0.0 | 0.1 ± 0.0 | NS |
For the demographic characteristics of the patients, differences between groups were assessed using the χ2 test for categorical variables and the Student's t-test for continuous variables when appropriate. Continuous variables are expressed as mean ± standard deviation. APACHE, Acute Physiology and Chronic Health Evaluation; COPD, chronic obstructive pulmonary disease; CRP, C reactive protein; INR, international normalized ratio; NS, not significant; OARF, oliguric acute renal failure.
Table 2.
Clinical characteristics of the patients in the validation study in survivors and non-survivors at 28 days
| Total (n = 194) | Survivors (n = 132) | Non-survivors (n = 62) | P | |
|---|---|---|---|---|
|
Patient details |
|
|
|
|
| Gender (male) |
126 (64.9%) |
85 (64.3%) |
41 (66.1%) |
NS |
| Age (years) |
67.1 ± 13.3 |
65.3 ± 14.3 |
71.1 ± 9.5 |
<0.001 |
| Inmunosuppression |
35 (18.0%) |
15 (11.3%) |
20 (32.2%) |
<0.001 |
| Diabetes |
32 (16.4%) |
21 (15.9%) |
11 (17.7%) |
NS |
| Cardiovascular disease |
24 (12.3%) |
14 (10.6%) |
10 (16.1%) |
NS |
| Cancer |
18 (9.2%) |
10 (7.5%) |
8 (12.9%) |
NS |
| COPD |
23 (11.8%) |
12 (9.0%) |
11 (17.7%) |
NS |
| Chronic renal failure |
15 (7.7%) |
10 (7.5%) |
5 (8.0%) |
NS |
| Alcohol abuse |
12 (6.1%) |
7 (5.3%) |
5 (8.0%) |
NS |
| Hepatic disease |
4 (2.0%) |
1 (0.7%) |
3 (4.8%) |
NS |
|
Clinical status at admission |
|
|
|
|
| APACHE II score |
22.6 ± 7.0 |
21.0 ± 6.5 |
25.9 ± 7.1 |
<0.001 |
| Mechanical ventilation |
150 (77.7%) |
93 (70.9%) |
57 (91.9%) |
<0.001 |
| OARF |
39 (20.1%) |
17 (12.8%) |
22 (35.4%) |
<0.001 |
|
Presumed source of infection |
|
|
|
|
| Respiratory system |
67 (34.5%) |
45 (34.1%) |
22 (35.5%) |
NS |
| Digestive system |
52 (26.8%) |
32 (24.2%) |
20 (32.3%) |
NS |
| Urinary system |
26 (13.4%) |
21 (15.9%) |
5 (8.1%) |
NS |
| Catheter |
16 (8.2%) |
11 (8.3%) |
5 (8.1%) |
NS |
| Wound/skin, soft tissue |
15 (7.7%) |
11 (8.3%) |
4 (6.5%) |
NS |
| Other/unknown |
18 (9.3%) |
12 (9.1%) |
6 (9.7%) |
NS |
|
Documented microbial agent |
|
|
|
|
| Gram-negative |
52 (26.8%) |
36 (27.2%) |
16 (25.8%) |
NS |
| Gram-positive |
33 (17.0%) |
25 (18.9%) |
8 (12.9%) |
NS |
| Fungi |
12 (6.1%) |
4 (3.0%) |
8 (12.9%) |
0.020 |
|
Laboratory data |
|
|
|
|
| Bilirubin (mg/dL) |
1.4 ± 2.2 |
1.4 ± 2.1 |
1.6 ± 2.4 |
NS |
| Glycemia (mg/dL) |
168 ± 64.0 |
167 ± 62.4 |
172.0 ± 67.6 |
NS |
| INR |
1.8 ± 3.1 |
1.9 ± 3.8 |
1.6 ± 0.6 |
NS |
| Platelets (×103/μl) |
177.4 ± 118.5 |
173.6 ± 105.2 |
186.4 ± 146.1 |
NS |
| Leukocytes (×103/μl) |
18.0 ± 16.4 |
18.4 ± 17.0 |
17.3 ± 15.3 |
NS |
| Monocytes (×103/μl) |
0.7 ± 1.7 |
0.8 ± 20.2 |
0.6 ± 0.9 |
NS |
| Lymphocyte (×103/μl) |
1.8 ± 70.5 |
1.6 ± 73.5 |
2.3 ± 64.1 |
NS |
| Neutrophils (×103/μl) |
14.9 ± 12.5 |
15.6 ± 12.9 |
13.6 ± 11.5 |
NS |
| Basophils (×103/μl) |
0.1 ± 0.0 |
0.1 ± 0.0 |
0.1 ± 0.0 |
NS |
| Eosinophils (×103/μl) | 0.1 ± 0.0 | 0.1 ± 0.0 | 0.1 ± 0.0 | NS |
For the demographic characteristics of the patients, differences between groups were assessed using the χ2 test for categorical variables and the Student's t-test for continuous variables when appropriate. Continuous variables are expressed as mean ± standard deviation. APACHE, Acute Physiology and Chronic Health Evaluation; COPD, chronic obstructive pulmonary disease; INR, international normalized ratio; NS, not significant; OARF, oliguric acute renal failure.
When patients of the discovery cohort were split based on deciles for CNC at SS diagnosis, those with CNC <7,226 cells/mm3 (decile 2) died earlier than the other non-survivors (Figure 1). Multivariate Cox regression analysis showed that patients with CNC below this cutoff value had an almost two-fold risk of death (Figure 1). The cutoff value was evaluated again in the validation cohort, with similar results (Figure 1). Counts of other leukocyte subtypes had no significant association with outcome.
Figure 1.
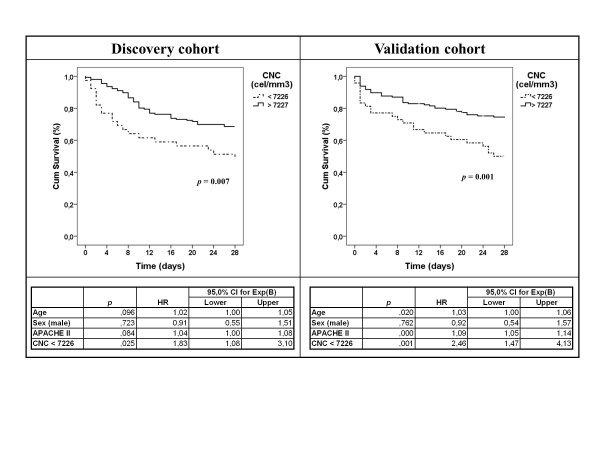
Impact of circulating neutrophil count on mortality: Kaplan-Meier survival curves. Groups were compared by the log-rank test (Mantel- Haenzel). Bottom: multivariate Cox regression analysis for mortality risk. Circulating neutrophil count (CNC) was adjusted by age, sex and Acute Physiology and Chronic Health Evaluation II score. Time was censored at 28 days following diagnosis. CI, confidence interval; Cum, cumulative; HR, hazard ratio.
Although normal reference values in blood vary depending on sex, race and age, available literature supports that 7,226 cells/mm3 is at the upper limit of normal CNC values [3]. Patients with insufficient numbers of circulating neutrophils during the early stages of SS could have difficulties mounting effective innate responses against the invading microbe(s). Increased neutrophil adhesion to the vascular endothelium in sepsis could contribute to lower CNC. Neutrophils adhered to the blood vessel wall seem to induce endothelial damage [4], forming leukocyte aggregates that could lead to microvascular thrombosis [1,5]. Host immunity compromise and/or increased endothelial damage could both impair outcome in these patients.
CNC at diagnosis is a major prognostic factor in SS. Our work provides a CNC cutoff that is potentially useful as a prognostic indicator.
Abbreviations
CNC: Circulating neutrophil count; SS: Septic shock.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JFBM, GR, DAO, and MFM designed the study, analyzed the data and participated in writing the article; ET, JB, and JIGH helped with the study design, provided a critical review of the results and participated in writing the article; RHM, AMB, MHR, and RC provided a critical review of the results and participated in writing the article. All authors have read and approved the final version for publication.
Contributor Information
Jesús F Bermejo-Martín, Email: jfbermejo@saludcastillayleon.es.
Eduardo Tamayo, Email: tamayo@med.uva.es.
Gema Ruiz, Email: cordoba_sweet@hotmail.com.
David Andaluz-Ojeda, Email: davidandaluz78@yahoo.es.
Rubén Herrán-Monge, Email: ruben.herran.monge@gmail.com.
Arturo Muriel-Bombín, Email: amurielb@saludcastillayleon.es.
Maria Fe Muñoz, Email: marifemunoz@yahoo.es.
María Heredia-Rodríguez, Email: maria_her_05@hotmail.com.
Rafael Citores, Email: rcitores@saludcastillayleon.es.
José Ignacio Gómez-Herreras, Email: jgomez012001@yahoo.es.
Jesús Blanco, Email: jblancov@saludcastillayleon.es.
Acknowledgements
Discovery study (EXPRESS) was supported by ISCIII, 'Proyectos de Investigación Sanitaria, PI 10/01362. Validation study (GRECIA) was supported by Proyectos de investigación en Biomedicina, Health Council, Castilla y León Goverment, Spain (BOCYL-D-26072010). Investigators of the EXPRESS group: Esther Gómez-Sánchez, Sandra Gutiérrez, Felipe Bobillo, Francisco Gandía,Verónica Iglesias , Lucia Rico, Raquel Almansa, Raúl Ortiz de Lejarazu (Hospital Clínico Universitario, Valladolid, Spain). Investigators of the GRECIA group: Pedro Merino, Marta María García-García (Hospital Universitario Río Hortega, Valladolid, Spain); M Jesús López Pueyo, Jose Antonio Fernandez Ratero, Miguel Martinez Barrios, Fernando Callejo Torre, Sergio Ossa Echeverri (Hospital General Yagüe, Burgos, Spain); Demetrio Carriedo Ule, Ana M Domínguez Berrot, Fco Javier Díaz Domínguez (Complejo Hospitalario de León, Spain); Susana Moradillo (Hospital Río Carrión, Palencia, Spain); Braulio Alvarez Martínez (Hospital del Bierzo, Ponferrada, Spain); Noelia Albalá, Juan Carlos Ballesteros, Marta Paz Perez, Elena Perez Losada (Hospital Clínico Universitario de Salamanca, Spain); Santiago Macías, Rafael Pajares García, Noelia Recio García Cervigón (Hospital General de Segovia Spain); M Mar Gobernado Serrano, M José Fernández Calavia, Daniel Moreno Torres (Complejo Hospitalario de Soria, Spain); Concha Tarancón, Teresa Loreto, Priscila Carcelen (Hospital Virgen de la Concha, Spain).
References
- Brown KA, Brain SD, Pearson JD, Edgeworth JD, Lewis SM, Treacher DF. Neutrophils in development of multiple organ failure in sepsis. Lancet. 2006;368:157–169. doi: 10.1016/S0140-6736(06)69005-3. [DOI] [PubMed] [Google Scholar]
- Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ. ACCP/SCCM Consensus Conference Committee. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. 1992. Chest. 2009;136:e28. doi: 10.1378/chest.09-2267. [DOI] [PubMed] [Google Scholar]
- Lim E-M, Cembrowski G, Cembrowski M, Clarke G. Race-specific WBC and neutrophil count reference intervals. Int J Lab Hematol. 2010;32:590–597. doi: 10.1111/j.1751-553X.2010.01223.x. [DOI] [PubMed] [Google Scholar]
- Fox ED, Heffernan DS, Cioffi WG, Reichner JS. Neutrophils from critically ill septic patients mediate profound loss of endothelial barrier integrity. Crit Care. 2013;17:R226. doi: 10.1186/cc13049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KA, Treacher DF. Neutrophils as potential therapeutic targets in sepsis. Discov Med. 2006;6:118–122. [PubMed] [Google Scholar]


