Abstract
Approximately 100 of the known species of mushrooms are poisonous to humans. New toxic mushroom species continue to be identified. Some species initially classified as edible are later reclassified as toxic. This results in a continually expanding list of toxic mushrooms. As new toxic species are identified, some classic teachings about mycetism no longer hold true. As more toxic mushrooms are identified and more toxic syndromes are reported, older classification systems fail to effectively accommodate mycetism. This review provides an update of myscetism and classifies mushroom poisonings by the primary organ system affected, permitting expansion, as new, toxic mushroom species are discovered.
Introduction
This review of mycetism will discuss recently discovered toxic mushrooms and new discoveries about previously described mushrooms. The focus will be clinical. The mushrooms will be categorized for review by organ system most severely affected after consumption of a particular species. Clinical presentation associated with ingestion, diagnosis, treatment, and prognosis will be discussed.
Methods
An advanced PubMed search was performed in May 2013. Keywords mushroom AND toxicity OR mushroom poisoning were utilized. Limitations of English language, human reports, and reports within the last 4 years were set. The searches produced 114 articles. Another search using keywords Amanita mushroom poisoning was performed in May 2013, with the same limitations, but no further articles were retrieved. PubMed-related citation lists were reviewed during the evaluation of these 114 articles. All articles were then collected and evaluated for relevance. When references listed within these 114 articles or within the PubMed-related citations were deemed pertinent, these referenced articles were also evaluated. Limitations of this review include: (1) only the English literature is evaluated (although some of the 114 cited articles have reviewed the literature in other languages), (2) generally, only human studies and reports were evaluated (although some animal and cellular data were evaluated, when mentioned in the 114 cited articles and deemed relevant), and (3) some articles may have been missed by our search criteria and by utilizing only PubMed. Other search engines may have found other articles.
Overview of Mushrooms
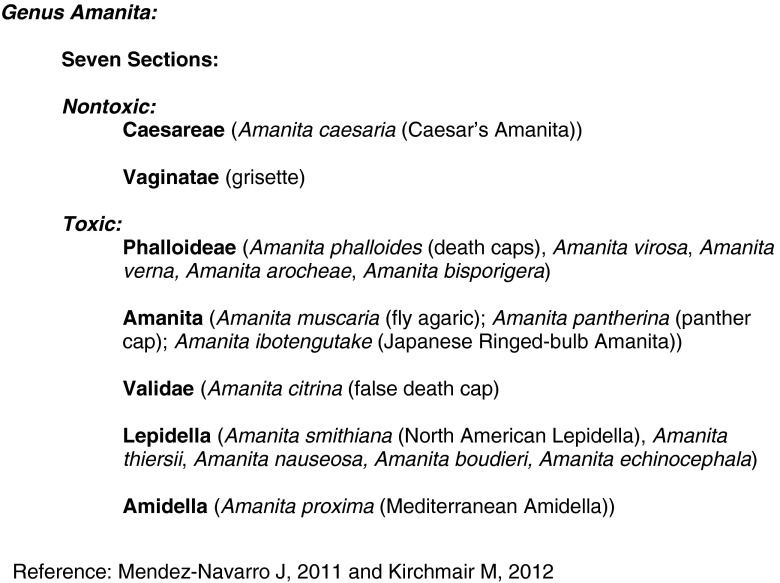
There are approximately 100,000 known species of fungi worldwide, with approximately 800 new species being named each year [1, 2]. Mushrooms are the visible fruit of fungi. Mushroom species are grouped into sections which are grouped into genus. The toxicity of different mushrooms within the same genus may vary greatly. For instance, genus Amanita contains seven sections: two sections contain nontoxic mushrooms and the remaining sections contain some poisonous species. Within this genus, the various poisonous species contain different toxins and produce different clinical syndromes [3, 4] (see Fig. 1).
Fig. 1.
The genus Amanita contains seven sections, two which are nontoxic and five of which are toxic. The clinical syndromes produced after ingestion of mushrooms from different sections are diverse, despite the mushrooms belonging to the same genus. Mushrooms in the Phalloideae section produce fulminant hepatic failure, while mushrooms in the Lepidella and Amidella sections produce primarily acute renal injury and mushrooms in the Amanita class produce an inebriating syndrome. Sources: Mendez-Navarro et al. [3] and Kirchmair et al. [4] and Kirchmair and Poder [5]
Approximately 100 of the known species of mushrooms are poisonous to humans, with new toxic species continually being identified [2, 6, 7]. Some mushrooms initially classified as edible have recently been reclassified as toxic such as Tricholoma equestre (Yellow Trich or Yellow Knight) [8]. As more toxic mushrooms are identified and more toxic syndromes are reported, older classification systems fail to effectively accommodate these diverse poisonings [8]. This review will classify mushroom poisoning by the primary organ system affected and will subclassify the type of syndrome produced within each organ system affected. This classification is summarized in Table 1.
Table 1.
Categorization of primary systems affected by toxic mushrooms
| Section in text | Primary system affected | Syndrome (mushrooms) | Characteristic toxicity | Gastrointestinal distress | Symptom onset |
|---|---|---|---|---|---|
| Neurotoxins | Neurologic | Cholinergic–muscarine (Inocybe, Clitocybe, Boletus, and Robinoboletus species) | Cholinergic syndrome | Present | 15 min–5 h |
| Neurologic (also hepatic and hematologic) | Epileptogenic—Gyromitra (Gyromitra esculenta) | Ataxia, coma, seizures, moderate hepatotoxicity, hemolysis, methemoglobinemia (in springtime) | Present, but delayed (occasionally bloody) | 4–12 h (rarely, as early as 2 h) | |
| Neurologic | Epileptogenic—in renally compromised patients (Pleurocybella porrigens) | Convulsions, myoclonus, dysarthria, ataxia, paresis, paralysis | Not reported | Delayed 1–31 days | |
| Neurologic | Inebriating—glutaminergic/GABAminergic—Pantherina/Muscaria (Amantia muscaria, Amanita pantherina) | Alternating CNS excitation and depression | May occur | 30 min–3 h | |
| Neurologic | Inebriating—Morchella sp. | Ataxia, tremor, visual disorders, paresthesias, confusion | Often present | 5 h for GI; 12 h neuro | |
| Neurologic | Encephalopathic (Hapalopilus rutilans) | Encepahlopathy with hepatorenal insufficiency and purple urine | Present, but delayed | 12 h | |
| Neurologic | Hallucinogenic—psilocybin (Psilocybe and Panaeolus species) | Hallucinations | May occur | 15–30 min | |
| Neurovascular toxins | Neurologic and vascular | (Clitocybe acromelalga, Clitocybe amoenolens) | Erythromelalgia | Generally 6–24 h | |
| Cardiotoxins and sudden death | Cardiovascular | Sudden unexplained death—Trogia venenata | Sudden death—following recurrent syncope, palpitations; ventricular tachycardia and fibrillation; seizures | Present | Initially diarrhea; reports of 3–5 days of syncope or dizziness prior to sudden death |
| Cardiovascular | Sudden unexplained death—Amanita franchetii or Ramaria rufescens | Sudden death—following tremor, muscle spasms; tachycardia, hypotension, and EKG changes | Present | 2–15 h | |
| GI toxins | GI (without other systems) | Gastrointestinal (Chlorophyllum molybdites and Omphalotus illudens) | Nausea, vomiting, abdominal cramping, diarrhea | Mild to marked (occasionally bloody) | Generally < 6 h |
| GI (with flushing) | Disulfiram-like—Coprinus (Coprinus species) | Ethanol intolerance: flushing with nausea and vomiting after ethanol ingestion | Present | 15–30 min after ethanol ingestion | |
| Hepatotoxins | Hepatic, renal, MSOF | Amatoxin-induced hepatic failure—Phalloides (Amanita, Galerina, and Lepiota species) | Fulminant hepatic failure, coagulopathy, renal failure, pancreatitis (in autumn) | Severe, but delayed (occasionally bloody) | Generally 6–24 h (but may occur sooner) |
| Nephrotoxins | Renal | Renal Failure—Orellanus (Cortinarius species) | Weakness, flank pain and oligo-anuria | Generally mild; may be absent | 30 hours to 20 days |
| Renal (slight hepatic) | (Amanita proxima, A. smithiana) | Acute kidney injury with mild hepatitis | Present | Generally 20 min–24 h for GI; 1–6 days for nephrotoxicity | |
| Myotoxins | Musculoskeletal, Cardiopulmonary, MSOF | Rhabdomyolysis (Tricholoma equestre, Russula subnigricans) | Muscle weakness, myalgias, respiratory failure, renal failure, myocarditis, seizures | Present | GI in 30 min–2 h; systemic toxicity generally >1 day |
| Immune/heme toxins | Immunologic, Hematologic, MSOF | Allergic—Paxillus (Paxillus involutus) | Immunohemolytic anemia, followed by acute renal failure, multiple organ dysfunction | Present | 30 min–3 h |
| Immunologic, Hematologic, MSOF | Immunosuppressive (Podostroma cornu-damae) | Pancytopenia, purpura, desquamation of the palms and face, alopecia, DIC | Present | Early GI, followed by complications of fluid loss, MSOF, pancytopenia and DIC |
GI gastrointestinal, neuro neurological
Overview of Exposure
Mushroom poisoning, termed mycetism or mycetismus, most commonly ensues after mushrooms are foraged, misidentified and then consumed [1, 7, 9–20]. The incidence of ingesting wild, toxic mushrooms is increasingly reported [8, 21, 22]. Worldwide, hundreds of mushroom poisonings are fatal each year [6, 8, 23, 24]. Most fatalities are secondary to Amanita phalloides ingestions [8, 9, 12, 23].
Overview of Initial General Assessment
Some toxic mushroom ingestions will produce self-limited toxicity. Others will prove fatal. Generally, most toxic mushrooms produce some gastrointestinal (GI) distress and commonly GI symptoms are the first symptoms reported. The diagnostic and prognostic value of GI symptoms are limited [6, 7, 11, 15]. In the past, some have promoted reliance on an initial time to development of GI symptoms to predict prognosis. Specifically, a latency of <6 h to development of GI symptoms was utilized to predict that a mushroom ingestion should produce limited toxicity. This practice has limitations and these limitations have become more apparent as new toxic mushrooms are recognized and more cases are reported. Yardan reported on 317 cases of mycetism in Turkey, without delineating which mushrooms produced toxicity, and found that common symptoms include nausea (86.6 %), vomiting (79.8 %) and diarrhea (21.1 %). Nine of these patients developed moderate to severe acute hepatic failure, with 2/9 patients having a latent phase of <6 h and the remaining 7/9 patients having a latent phase of >6 h. Thus, 22 % of patients who eventually developed hepatic failure had a latent phase of <6 h [6]. Similarly, Syed reported on three patients developing severe mushroom-induced hepatitis; 1/3 (33 %) had initial symptoms within <6 h of ingestion [15]. Escudie reported on eight mushroom-poisoned patients that had either fatal intoxication or required liver transplantation and noted that the onset to diarrhea in these patients ranged from 4 to 8 h after ingestion [25]. The practice of predicting prognosis by utilizing the latency to GI symptom development should be reconsidered. Not all patients presenting with symptoms within 6 h of ingestion have a benign course [8, 20, 26]. Interestingly, if A. phalloides ingestion is known, or strongly suspected, to have occurred and diarrhea develops in <8 h, the prognosis is poorer [25]. Conversely, GI symptoms occurring >6 h after ingestion remain concerning for a possible serious clinical course and possible fatality [3, 6, 11, 12, 27].
Overview of Initial General Treatment
In general, supportive care is the mainstay for mycetism. Providing recommendations regarding activated charcoal administration is challenging, due to the lack of prospective, controlled studies [28]. Beuhler retrospectively collected data from North American poison control center cases of unintentional pediatric mushroom ingestions and found that activated charcoal did not improve outcome. Of note, there were no deaths reported, suggesting a less severely poisoned group of patients than other patient populations [28]. If a patient is actively vomiting, activated charcoal may not contribute to decontamination. Antiemetics may limit natural decontamination.
Determining what mushrooms are likely to have been ingested, and therefore what treatments are most appropriate, will likely be based on the geographic location of mushroom harvesting (see Table 2). If a hepatotoxic mushroom, such as A. phalloides, has been ingested or is suspected, prompt treatment with an antidote seems prudent [26] (see Table 3 and hepatotoxic mushroom section below).
Table 2.
Geographical distribution of recently described toxic mushrooms
| Primary system affected by toxins (effects) | Geographical location of mushroom harvest | Mushrooms |
|---|---|---|
| Neurological (encephalopathy) | Germany | Hapalopilus rutilans (Purple Dye Polypore) |
| Neurological (convulsive encephalopathy) | Japan | Pleurocybella porrigens (Angel’s Wing) |
| Neurovascular (red, swollen, painful extremities) | Japan, South Korea | Clitocybe acromelalgia |
| Neurovascular (red, swollen, painful extremities) | France, Italy, Morocco | Clitocybe amoenolens (Poison Dwarf Bamboo or Burn Mushroom) |
| Cardiac (sudden death) | Yunnan Province, China | Trogia venenata (Little White) |
| Cardiac (sudden death) | Jiangxi Province, China | Amanita franchetii a |
| Ramaria rufescens a | ||
| Renal | Canada (South-West), USA (Pacific Coast to North-West) | Amanita smithiana (Toxic Lepidella or North American Lepidella) |
| Renal | France (South), Spain, Italy | Amanita proxima (Mediterranean Amidella) |
| Renal | Japan | Amanita pseudoporphyria Hongo |
| Muscular (rhabdomyolysis, myocarditis) | France, Poland | Tricholoma equestre (Yellow Trich or Yellow Knight or Man on Horseback) |
| Muscular (rhabdomyolysis, myocarditis) | Taiwan, Japan, Korea, China, Nepal | Russula subnigricans (Blackening Russula) |
| Immune/heme (hemolysis, hepatorenal failure) | Northern Hemisphere | Paxillus involutus (Poison Pax or Brown Roll Rim) |
| Immune/Heme (pancytopenia) | Northeastern Asia | Ganoderma neojaponicum Imazekia |
| Immune/Heme (pancytopenia) | Japan, China, Korea, Java | Podostroma cornu-damae |
aNewly reported and association not as well established as other causes of mycetism
Table 3.
Antidotes for Amatoxin poisoning (recommended doses are based on previously published reports)
| Antidote | Mechanism of action | Dose |
|---|---|---|
| Silibinina | Competes with amatoxins for transmembrane transport; inhibits penetration of amanitin into hepatocytes; scavenges free radicals; produces anti-inflammatory effects; increases ribosomal RNA synthesis, resulting in increased protein synthesis | 5 mg/kg IV over 1 h; then 20 mg/kg/24 h continuous infusion (diluted in 5 % glucose to a concentration of 2 mg silibinin/ml) for 3 days (alternatively, the 20 mg/kg/24 h can be divided into six hourly doses) |
| N-acetylcysteine (NAC) | Promotes glutathione regeneration; scavenges free radicals | Follow dosing for APAP treatment: 150 mg/kg IV over 1 h, followed by 12.5 mg/kg/h for 4 h, followed by 6.25 mg/kg/h until evidence of hepatic failure resolution |
Sources: Ahishali et al. [26]; Berger and Guss [29] and Berger and Guss [30]; Bergis et al. [31]; Diaz [8, 32]; Karlson-Stiber and Persson [33]; Magdalan et al. [34] and Magdalan et al. [35]; Roberts et al. [36]; Sorodoc et al. [37]; Trabulus and Altiparmak [38]; Ward et al. [19]
aSilibinin is not approved as a therapeutic treatment for hepatic disease by the Food and Drug Administration in the USA; it may be available through clinicaltrials.gov; it is approved and available in parts of Europe and Australia
Neurotoxins
Neurotoxic mushrooms may produce cholinergic, epileptogenic, inebriating, encephalopathic, or hallucinogenic syndromes. Many of these syndromes have associated visual disturbances. Some contain toxins that affect vasculature and are classified under neurovascular toxins.
Cholinergic Syndromes
Some mushrooms contain muscarine which stimulates peripheral muscarinic receptors. Muscarine acts like acetylcholine, but is not degraded by cholinesterase, and therefore has a longer duration of action [21]. The amount of muscarine in A. muscaria is very low and muscarinic symptoms are rarely seen after its consumption [16]. Inocybe (Fiber Heads), Clitocybe (Funnel Caps), Boletus, and Rubinoboletus species can contain sufficient muscarine to produce muscarinic toxicity. Onset of toxicity is 15 min to 5 h after ingestion. Flushing, vasodilation, diaphoresis, lacrimation, miosis, blurred vision, hypersalivation, bronchorrhea, bronchospasm, vomiting, diarrhea, abdominal pain, tremor, restlessness, and bladder contraction can follow ingestion. Bradycardia or tachycardia, hypotension or hypertension, syncope, shock, and confusion may be seen. Hallucinations have been reported [2, 39]. Treatment is supportive. Fluid and electrolyte replacement may be necessary. Atropine has been used to treat bronchorrhea and bradycardia. Vasopressors may be needed. Toxicity generally resolves within 12 h of ingestion [16, 21, 29, 30, 40].
Epileptogenic Syndromes
The classic epileptogenic mushroom is Gyromitra esculenta (False Morel), which may be confused with Morchella sp. (True Morel, which is deemed edible, but which can produce neurological symptoms if poorly cooked) or Verpa bohemica (Early Morel, which can produce disulfiram-like reactions) [41]. G. esculenta contains gyromitrin, which is hydrolyzed to monomethylhydrazine, an inhibitor of pyridoxal phosphate. Interference with pyridoxine-dependent pathways, such as production of gamma-aminobutyric acid (GABA) from glutamate, results. This promotes seizure activity. Symptoms begin 4–12 h after ingestion. Clinical progression is vomiting and diarrhea followed by neurological symptoms (vertigo, ataxia, nystagmus, tremor, convulsions, and coma) [2, 29, 30, 42]. Hepatic necrosis, methemoglobinemia, hemolysis and rhabdomyolysis are also reported. Jaundice may be noted [30, 33, 42–44]. Approximately 10 % of patients poisoned will die [42]. Treatment is supportive, including fluid, electrolyte and glucose replacement. Pyridoxine is recommended for neurologic symptoms including seizures [29, 30, 33, 45]. While there is not an established dosing regimen for pyridoxine treat of mycetism, it seems reasonable to utilize the dosing recommended for INH overdose, which is 70 mg/kg up to 5 g, intravenously. Benzodiazepines and barbiturates may also be helpful; however, seizures may be resistant to benzodiazepines and barbiturates prior to GABA repletion aided by pyridoxine treatment [33].
In Japan, 2004, convulsive encephalopathy occurred epidemically when patients with hemodialysis-dependent renal failure ingested Pleurocybella porrigens (also called Nothopanus porrigens, Sugihiratake, and Angel’s Wing). Gastrointestinal symptoms were not reported. A 1–31 day latency was noted. Patients exhibited convulsions (78 %), myoclonus (47 %), dysarthria (31 %), ataxia (25 %), and paresis or paralysis (22 %) [46]. Intractable status epilepticus has also been reported [47–49]. MRI may reveal intracranial lesions involving the subcortical white matter of the insular cortex, claustrum, external capsule, putamen, and globus pallidus [48]. Autopsy of a man who succumbed to P. porrigens poisoning after developing encephalopathy and status epilepticus demonstrated postinfarction-like cystic necrosis of the putamen and spotty necrosis of the deep cerebral and cerebellar cortices [2, 50]. The mortality rate is approximately 30 % [46, 47].
Other mushroom ingestions that may produce seizures as part of their toxidrome include Trogia venenata, Russula subnigricans, Amanita muscaria, Amanita pantherina, Psilocybe spp., and Morchella spp. The mushrooms are discussed later in the review.
Inebriating Syndromes
Glutaminergic/GABAminergic syndrome (or pantherina–muscaria syndrome) is an inebriating syndrome that occurs after eating mushrooms containing ibotenic acid and muscimol, such as Amanita muscaria (Fly Agaric), Amanita pantherina (Panther Cap), and Amanita ibotengutake (Japanese Ringed-Bulb). Amanita pantherina may be mistaken for the edible Amanita rubescens, Amanita spissa, or Macrolepiota procera; while A. muscaria ingestion is usually intentional and recreational [2, 51]. Ibotenic acid and muscimol are derivatives of glutamate and GABA, respectively. Ibotenic acid is a non-protein amino acid that is unstable and easily decarboxylated to muscimol. Ibotenic acid is a glutamate agonist, acting at N-methyl-d-aspartate (NMDA) receptors. Muscimol is a GABAA agonist [2, 52]. Symptoms occur 30–180 min after ingestion. Symptoms usually peak at 2–3 h and disappear within 6–9 h [39, 52]. Vomiting has been reported. Central nervous system effects may be excitatory (hysteria, hyperkinetic behavior, seizures, myoclonic twitching) or depressive (waxing and waning obtundation). Alterations of time and space perception, auditory and visual hallucinations, and ataxia have been reported [51–56]. Rarely, tachycardia, hypertension, mydriasis, or flushing are seen [16, 39]. In severe intoxication, coma and respiratory failure may be seen [51]. Spores may be identified in the stomach or intestinal contents. Ibotenic acid and muscimol may be isolated from urine with a cation exchanger, with derivatives analyzed by gas chromatography/mass spectrometry (GC/MS) [51]. Treatment is supportive. Benzodiazepine and barbiturates may control agitation and seizures. Patients occasionally require ventilator support [51].
Morchella spp. (True Morels and Half-Free Morels) can produce neurological toxicity including an inebriating syndrome. Toxicity is more likely if the mushrooms are ingested after insufficient cooking or in large quantities. Toxicity is thought to be due to thermolabile hemolysins. The neurological syndrome generally begins 10 to 12 h after ingestion and may follow GI symptoms, which may include nausea, vomiting, diarrhea, and abdominal pain. Occasionally, the GI symptoms are associated with urticarial rash or itching. A review of 129 patients who presented with a neurological syndrome after Morchella sp. ingestion noted that patients most commonly experienced tremor (53 %), dizziness/inebriation (53 %), or unsteadiness/ataxia (21 %), with or without GI symptoms. Some patients were also found to have ocular/visual disorders (26 %), paresthesias (7 %), drowsiness or confusion (6 %), and muscle disorders (6 %). The visual problems were generally diplopia or blurred vision. Within 24 h, 90 % of patients had recovered [41].
Encephalopathic Syndromes
In Germany, encephalopathy and hepatorenal insufficiency associated with purple urine have been reported following ingestion of Hapalopilus rutilans (Purple Dye Polypore) [8, 15, 49]. Polyporic acid (2,5-diphenyl-3,6-dihydroxy-1,4-benzoquinone) may be responsible. The syndrome begins with nausea, vomiting, and abdominal pain approximately 12 h after ingestion. Neurological symptoms, such as vertigo, ataxia, drowsiness, hypotonia, and visual complaints, follow. Hepatorenal laboratory abnormalities have been reported [2, 49]. P. porrigens (Angel’s Wing), Grifola frondosa, and Pleurotus eringii poisonings may present with encephalopathy (see “Mitochondrial Toxins” section below). Any mushroom that produces fulminant hepatic failure (e.g., A. phalloides) or that is epileptogenic (e.g., G. esculenta) may be associated with encephalopathy.
Hallucinogenic Syndromes
Hallucinogenic mushrooms generally contain psilocybin and include Psilocybe spp., Panaeolus spp., and Stropharia aeruginosa [1]. Psilocybe semilanceata, P. cubensis, P. mexicana, P. bohemica, and P. baeocistis are the most commonly consumed [2]. The highest concentration of psilocybin is reportedly found in P. azurescens (blue angels) of the Pacific Northwest [1]. Psilocybin-containing species may turn bluish (bruise) upon handling especially the stalks; however, this is nonspecific, as some other species that do not contain psilocybin bruise similarly [1]. Symptoms begin 15–30 min after ingestion and generally last up to 6 h and rarely last 12 h [2]. Altered time-space perceptions, and auditory and visual hallucinations, are seen. Mydriasis, hypertension, tachycardia, dysrhythmias, and myocardial infarction have also been reported [29, 30, 57, 58]. Seizures and hyperthermia have been reported in children [59]. Occasionally, foragers seeking hallucinogenic mushrooms will misidentify mushrooms and ingest other, more toxic mushrooms. This can result in delayed symptoms and possibly organ failure [10]. Treatment is supportive. Benzodiazepine and barbiturates have been used to control agitation and seizures [58, 60, 61]. Psilocybin and its derivative, psilocin, can be detected by GC/MS, gas liquid chromatography, high performance liquid chromatography (HPLC) and spectroscopy [1].
Neurovascular Toxins
Clitocybe amoenolens (Poison Dwarf Bamboo Mushroom; Burn Mushroom) and Clitocybe acromelalgia are associated with erythromelalgia. Erythromelalgia involves erythema, swelling and pain of the distal extremities. Ingestion of only a few mushrooms can produce toxicity. C. acromelalgia and C. amoenolens contain acromelic acids A–E, amino acids and kainate analogs, which may be responsible for neurologic excitotoxicity. Peripheral glutamate receptors of cutaneous nerve endings may be involved. In rats, intrathecal administration of acromelic acid damages lower spinal neurons, with spastic paraplegia ensuing. In humans, symptoms appear 24 h after ingestion, and patients present with paresthesia of the digits followed by paroxysmal burning pain. Paroxysmal dilation of the blood vessels of the skin occurs. This is associated with tactile and burning pain, and red, swollen hands and feet. Heat and a declive position induce paroxysmal crises, which generally occur nocturnally. Cyanosis or erhythema may worsen during pain paroxysms. More severe cases are associated with local diaphoresis and trophic changes of the digits. The pain can be incapacitating. Electromyograms reveal evidence of toxic polyneuropathy with sensorimotor fiber impairment. Dipping the extremities in cold water often provides relief, while traditional analgesics may be ineffective. The syndrome can last for weeks to months [15, 32, 49, 62–64].
Cardiotoxins and Sudden Death
Epidemic syndromes of sudden death have been described in two different provinces in China and linked to mushroom ingestions.
More than 400 villagers in the Yunnan Province of China have died suddenly over the past several decades. A seasonal illness, called Yunnan sudden unexplained death (SUD), has been epidemiologically traced to T. venenata (Little White) mushroom consumption. T. venenata contains two toxic unsaturated amino acids, 2R-amino-4S-hydroxy-5-hexynoic acid and 2R-amino-5-hexynoic acid, which were initially felt to be responsible for the toxicity. These amino acids have proved lethal in mice. A patient with SUD was found to have 2R-amino-4S-hydroxy-5-hexynoic acid in his post mortem blood by LC-MS/MS. Structural similarity between these hexynoic acids and hypoglycin A, found in Ackee fruit, has been noted. Mice given extracts of T. venenata develop profound hypoglycemia [65] However, it is unclear if the toxins in T. venenata interfere with beta-oxidation of fatty acids or ATP production (as does the metabolite of hypoglycin A). Overall, SUD does not closely resemble the clinical presentation of Ackee fruit poisoning, and these amino acids do not adequately account for all the symptoms seen in SUD. These mushrooms also contain the proconvulsant toxin, gamma-guanidinobutyric acid, which is structurally similar to GABA [22, 66]. The exact toxin responsible for the syndrome is not yet well established [67, 68] Initially, patients report nausea, vomiting, diarrhea, abdominal pain, and fatigue. Recurrent syncope and eventual sudden unexpected death may occur. Many patients report palpitations, chest discomfort, dizziness, syncope, and seizures in the hours preceding death. Ventricular tachycardia and fibrillation may precede death. Elevated AST, ALT, LDH, and CK are also reported [65, 68, 69]; however, in one study, only elevation of AST was statistically significant, when compared to controls [68]. Postmortem examinations of 29 cases revealed mild, focal lymphocytic myocarditis, with breakage of the muscle fibers [68]. Postmortem examination also revealed occasional lymphocytic infiltration of the liver, pulmonary alveolar edema, acute kidney necrosis, hepatocyte necrosis, and congestion of the liver, lung, or spleen [68]. The public campaign to educate against T. venenata consumption has dramatically reduced the incidence of SUD [66, 68].
Approximately 1,000 miles away from the Yunnan Province, in the Jiangxi Province of China, a small epidemic of fatal mycetism occurred in 2005. Amanita franchetii and Ramaria rufescens are the suspected culprits. Ten patients died within 5–7 days of mushroom ingestion. Early symptoms began 2–15 h after ingestion and included nausea, vomiting, dizziness, aching or pain, and occasionally abdominal distention. Many patients experienced muscle spasms or tremors. This was followed by some clinical improvement, only to be followed by cardiovascular collapse and sudden death. Of the patients who survived to hospital evaluation, marked hypotension and tachycardia were noted. Moderately elevated AST and EKG abnormalities were noted. Minimally symptomatic and surviving family members had slightly elevated ALT, sinus tachycardia, and transient T-wave inversions on EKG [70].
Other mushrooms may produce cardiotoxicity concurrent with their principal toxicity. Mushrooms that produce rhabdomyolysis may produce myocarditis, cardiomyopathy, dysrhythmias, and cardiovascular collapse (see “Myotoxins” section below) [32, 49, 71, 72]. A. phalloides ingestion rarely produces cardiogenic shock with ventricular systolic dysfunction and hypotension. The EKG may reveal ST–T wave changes, and the echocardiogram may reveal hypokinesia and a low ejection fraction [73]. An amatoxin-poisoned patient with cardiogenic shock and multi-organ failure was treated with intra-aortic balloon counterpulsation support until eventual recovery (see “Hepatotoxins” section below) [73]. Amanita proxima has also been associated with cardiotoxicity (see “Nephrotoxins” section below) [74, 75].
Gastrointestinal (GI) Toxins
Many mushrooms produce GI distress after ingestion and most mushrooms that produce severe systemic toxicity also produce GI toxicity.
Gastritis/Gastroenteritis Reactions
Mushrooms containing GI toxins belong to several genera including Chlorophyllum, Boletus, Entoloma, Lactarius, Omphalotus (such as Omphalotus olearius or Jack-O’-Lantern mushroom), Clitocybe, Paxillus, and Tricholoma [15, 76]. Chlorophyllum molybdites (Green-spored Parasol) is commonly found on lawns and is the most frequently ingested toxic mushroom in the USA. It is representative of GI toxic mushrooms. Vomiting, profuse diarrhea, and abdominal pain follow ingestion. The diarrhea may be bloody. Treatment is supportive including fluid and electrolyte replacement. Vasopressors are rarely needed [15, 24, 77, 78].
Disulfiram-Like Reactions
Alcohol intolerance has been reported following consumption of Coprinus species, Lepiota aspera (Freckled Dapperling), Boletus luridus (Lurid Bolete), Verpa bohemica (Early Morel), Clitocybe clavipes (Clubfoot), Pholiota squarrosa (Shaggy Scalycap), and T. equestre (Yellow Trich or Yellow Knight). This intolerance is best described after Coprinus atramentarius (Inky Cap) consumption [79]. C. atramentarius contains coprine, a pro-toxin of 1-amino-cyclopropanol which inhibits acetaldehyde dehydrogenase; however, it does not inhibit dopamine-beta hydroxylase, as does disulfiram [79, 80]. A disulfiram-like reaction ensues if ethanol is ingested within 30 min to 3 days after mushroom ingestion and can occur within several minutes of ingesting ethanol [79]. The reaction comprises headache, flushing, diaphoresis, nausea, vomiting, tachycardia, hypotension, palpitations, dizziness, and dyspnea [79]. Treatment is supportive including fluid and electrolyte replacement. Symptoms generally resolve within 6 h of ethanol consumption but may recur with repeat ethanol consumption [29, 30, 32, 81, 82].
Hepatotoxins
Amatoxins and gyromitrin are protoplasmic poisons that produce hepatotoxicity [33]. Gyromitrin was discussed previously. This section focuses on amatoxin. Amatoxin-containing mushrooms cause the vast majority of fatalities from mycetism [6, 9, 29, 34, 38, 83–85]. A. phalloides (Death Cap), A. bisporigera, A. rubescens, A. ocreata, A. verna, and Amanita virosa (the last three are referred to as Death Angels and Destroying Angels; however, A. phalloides is also sometimes referred to as Death Angel and A. verna is sometimes referred to as White Death Cap), A. fuliginea, A. subjunquillea, A. exitialis, A. suballiacea, A. tenuifolia, A. hygroscopica as well as some Galerina and Lepiota (e.g., L. brunneoincarnata and L. helveola) species contain amatoxin. As little as 0.1 mg amatoxin/kg body weight may be lethal in adults [36, 37, 84–88].
The Toxins
Mushrooms that contain amatoxin may also contain phallotoxins, virotoxin, and toxophallin (l-amino acid oxidase). While the amount of amatoxin varies among species, a single mushroom may contain 5–7 mg of amatoxin and could be fatal if ingested [36, 37, 84–88]. Children are particularly sensitive to amatoxin [14, 37, 89–92]. Toxophallin is an enzyme that induces chromatin condensation, DNA and nucleus fragmentation, and apoptosis. It is hypothesized that toxophallin induces cell damage via generation of free radicals and oxidants, resulting in apoptosis [2, 93]. Phallotoxins are not absorbed from the intestine and are not thought to contribute significantly to clinical toxicity [84, 85]. Virotoxin appears to be restricted to A. virosa [85].
Amatoxins are generally accepted as the principal toxins producing hepatotoxicity. There are ten known amatoxins, including alpha-, beta- and gamma-amanitins. Alpha-amanitin, the primary toxin, is a heat-stable, bicyclic octapeptide which damages the liver and kidneys by irreversibly binding to RNA polymerase II. This diminishes mRNA production, which diminishes protein production, and eventually produces cell death [34–36, 89, 94]. Alpha-amanitin may also be transformed into free radical intermediates that increase production of reactive oxygen species such as hydrogen peroxide, superoxide, and hydroxyl radicals. This contributes to cell membrane damage [34]. Alpha-amanitin may also act synergistically with endogenous cytokines, such as tumor necrosis factors, to produce cell damage and induce apoptosis [84, 85].
Alpha-amanitin is easily absorbed in the intestines. Gastrointestinal epithelial cells, hepatocytes, and proximal tubular cells are very susceptible to amatoxins, in part, due to increased amatoxin uptake via organic anion-transporting polypeptides within cell membranes [19, 35, 89]. Alpha-amanitin may also be transported into the cell via Na + −taurocholate cotransporter polypeptides [19]. Ultimately, hepatic necrosis and acute tubular necrosis of the kidneys ensue [35, 89, 95].
Clinical Presentation
Clinical progression may be divided into four stages: (1) latency or quiescent phase, (2) gastrointestinal phase, (3) clinical remission (progressive organ damage despite apparent clinical improvement), and (4) acute liver failure or multiorgan failure [84, 85]. Typically, an asymptomatic latency of 6–24 h proceeds severe gastroenteritis; however, shorter latencies have been reported [6, 27, 89]. Others have reported latencies as long as 40 h [84]. Gastroenteritis, including vomiting, watery diarrhea, and abdominal pain follows and typically lasts 1–2 days. This may be associated with tachycardia, hypotension, and electrolyte abnormalities. Gastroenteritis may be followed by a brief clinical remission. Liver enzymes begin to rise within 16–48 h of ingestion and can increase despite apparent clinical improvement [38, 84]. The final stage is hepatorenal or multiorgan failure within 2–7 days of mushroom ingestion. Fulminant hepatic failure is characteristic of severe toxicity. Liver pathology is characterized by fatty degeneration and centrilobular necrosis [84, 90, 94, 96]. Acute tubular necrosis, with damage to the proximal tubules, can also be seen [84, 85]. Death, when it occurs, is generally at 4–16 days but may occur later [6, 83, 84, 89, 94, 96–101]. Less severely poisoned patients may recover, rather than progress to fulminant hepatic failure [84]. Approximately 20 % of survivors develop immune complex-mediated chronic hepatitis with anti-smooth muscle autoantibodies [29, 102, 103]. Pancreatitis, prior to the development of fulminant hepatic failure, has been reported after Lepiota subincarnata ingestion [14]. Thrombocytopenia may occur and is generally noted 3 days after ingestion [38].
Toxin Detection
The Meixner test can be performed by adding hydrochloric acid to a sample of mushroom placed on newspaper. A blue color change suggests amatoxin is present; however, the test may produce false positives [36, 86]. Alpha-amanitin can be detected in serum by HPLC [38, 89, 103]. Amatoxins can also be detected in the urine [85, 101]. Some have used RIA, ELISA, or EPLC to detect amatoxin [84]. Others have developed LC/MS/MS and mass LC/MS methods to detect these toxins [104]. Recently, a DNA-based macroarray was developed to detect Amanita species from left-over mushroom meals [103].
Prognosis
Mortality rates have historically been reported as high as 20–30 % in adults and >50 % in children; however, more recent data indicates that the mortality rates are declining and are currently often reported at <10 %; however, in some current reports, mortality rates continue to be higher than 10 % [26, 31, 36, 38]. Trabulus found that patients who died were more likely to have low mean arterial pressures (MAP < 70 mmHg), encephalopathy (confusion, stupor, and coma), mucosal hemorrhage, and oliguria–anuria. The laboratory studies of patients who died revealed greater elevation of urea, aspartate aminotransferase (AST), alanine aminotransferase (ALT), lactate dehydrogenase (LDH), total bilirubin, prothrombin time (PT), INR and partial thromboplastin time (PTT) levels, but lower sodium concentrations, platelet counts (platelet count < 100,000/μl) and plasma glucose levels (<60 mg/dl) [38]. All patients who died developed acute hepatic failure with encephalopathy and died within 1–7 days of hospitalization. Encephalopathy was the strongest predictor of death from amatoxin-containing mushroom poisoning [odds ratio (OR) of 232], followed by oliguria–anuria (OR of 52) and thrombocytopenia (OR of 15.5) [38]. Similarly, Fantozzi et al. [105] reports that elevation of ALT or AST > 2000 IU, hepatic encephalopathy, or PT > 50 s are prognostic of impending death. Jan et al. [106] reports that, in children (as in adults), signs of hepatic encephalopathy, prolonged PT, and elevation of hepatic transaminases are associated with increased mortality. It is rare for a patient without encephalopathy to succumb to multi-organ failure after Amanita sp. poisoning [25]. Death from hepatic failure may be secondary to sepsis, brain herniation, or bleeding complications.
Treatment
There are not universally accepted antidotes or standardized treatments for amatoxin poisoning. Treatment generally comprises intensive supportive care, with attention paid to fluid and electrolyte imbalances, coagulation disorders, and hypoglycemia [38]. Standard treatments for acute liver failure (ALF) should be utilized [107–109]. Some recommend multiple-dose activated charcoal (20–40 g every 3–4 h for 24 h or 50 g every 6 h) and nasoduodenal suctioning to limit enterohepatic recirculation of amatoxin, because approximately 60 % of absorbed alpha-amanitin is excreted into the bile and is then returned to the liver via recirculation [29, 38, 73, 84, 85]. The antidotes benzylpenicillin, ceftazidime, N-acetyl-cysteine (NAC), rifamycin, and silibinin have been advocated by some [26, 34, 36, 88, 110–112], and questioned by others [113, 114]. Of these, silibinin and NAC show the most promise [32, 34, 111, 115]. Magdalan [34] performed cell culture studies and found that hepatocytes poisoned with alpha-amanitin and simultaneously treated with NAC or silibinin showed less evidence of lipid peroxidation than poisoned hepatocytes simultaneously treated with benzylpenicillin or without an antidote treatment. Studies performed in beagle dogs poisoned with lyophilized A. phalloides reveal silibinin treatment lessened lab abnormalities associated ALF, hemorrhagic necrosis of the liver and mortality [85]. Silibinin is the most active component of silymarin, found in Silybum marianum (milk thistle). It is a scavenger of free radicals, has anti-inflammatory effects, stimulates protein synthesis, and inhibits amatoxin uptake by hepatocytes [26, 34]. If silibinin is available, its administration seems reasonable [19, 31, 85, 97, 111, 115, 116]. Silibinin could potentially be obtained by contacting the researchers using this antidote through clinicaltrials.gov, using identifier NCT00915681. In Europe, Legalon® SIL is available. Its active ingredient is silibinin-C-2′3-dihydrogen sussinate, disodium salt [85]. Amanita virosa decreases intracellular glutathione content; NAC may be useful as a glutathione precursor [34]. Since NAC is readily available and relatively safe, its administration seems reasonable [19, 85, 111] (Table 3).
There are not randomized, controlled trials evaluating extracorporeal treatments for amatoxin-poisoned patients; thus, these treatments remain controversial. Patients studied by Trabulus received hemoperfusion (HP) upstream of concurrent hemodialysis (HD) and had a relatively low mortality rate; however, HP–HD was not compared to optimal medical care without extracorporeal decontamination [38]. Mullins reported on the apparent futility of HP and HD in the treatment of A. phalloides poisoning after noting that amatoxin was not detected before, during or after HP and HD treatments in blood or in HP or HD circuits of two patients treated with HP and HD after A. phalloides poisoning [117]. This is not surprising, since amatoxin is rapidly absorbed and distributed into body compartments. Amatoxins are rarely detected in plasma 36–48 h after mushroom ingestion; despite being detectable in the liver and kidneys after 5 days [31, 84, 89]. Amatoxins may be detectable in the urine for 4 days [31]. Similarly, some report that plasmapheresis reduces mortality [26, 99, 118]; others doubt its efficacy [8, 32, 33]. Liver albumin dialysis [molecular absorbent recirculating system (MARS) or fractionated plasma separation and adsorption with high-flux dialysis (Prometheus)] has been successfully utilized, while awaiting liver transplantation; however, patients may die awaiting organ donation [3, 25, 31, 37, 38, 83, 90, 94, 119–121].
MARS is an extracorporeal decontamination technique that removes albumin-bound substances that may play a role in ALF. Blood is dialyzed against an albumin-containing solution across a high flux permeable membrane [89]. While MARS would not likely remove amatoxins, it could remove protein-bound endogenous toxins, allowing the liver to spontaneously recover. Treatment with MARS could improve medical conditions enough that a critically ill patient would better tolerate, or survive until, liver transplantation [89]. Sorodoc et al. [37] evaluated six patients with amanitin-induced fulminant hepatic failure treated with either MARS or optimal intensive care alone and found that MARS treatments decreased ammonia, ALT, PT, and mortality rate (from 100 % to 66.7 %). However, it is difficult to draw prognostic conclusions about MARS treatment from Sorodoc’s data because only 1/6 patients survived. The surviving patient received MARS, but was also the only patient with normal vital signs on admission (non-survivors had hypotension and/or tachycardia on admission). The surviving patient also had the lowest initial model for end-stage liver disease (MELD) score [37]. Sorodoc et al. [37] also notes that the survivor consumed the smallest meal of mushrooms. Based on history and initial presentation, one might have predicted this patient would be the most likely to survive, with or without MARS. Covic utilized MARS treatment in six children with hepatic encephalopathy after mushroom poisoning. Covic et al. [119] found that 4/6 patients survived with intact liver function, compared to matched controls in which MARS was not utilized and 6/6 died (mortality rate of 33 % compared to 100 %). Faybik reports on six patients treated with extracorporeal albumin dialysis after A. phalloides poisoning and notes that: two patients had spontaneous regeneration of liver function; two patients were bridged to liver transplantation; one patient avoided re-transplantation after graft dysfunction following liver transplantation; and one patient died secondary to cerebral herniation [122]. MARS has been utilized in a pregnant patient with hepatic encephalopathy due to A. phalloides poisoning. Her hepatic encephalopathy resolved after MARS treatment, after initial HP–HD, plasma exchange, and aggressive supportive care had been ineffective [27]. Wittebole reviewed the cumulative, international, experience of MARS use in 48 cases of A. phalloides-related liver failure [89]. Wittebole and Hantson [89] note improvement of encephalopathy, often with resolution of encephalopathy, and improvement of hemodynamic parameters.
Vardar evaluated a fractionated plasma separation and adsorption system (FPSA, Prometheus) in eight patients with hepatic failure after wild mushroom ingestion in Turkey. All patients received FPSA, Penicillin G, and NAC. Vardar noted improvement of AST and ALT, a complete response rate of 75 %, and a survival rate of 87.5 % [121]. More recently, Bergis et al. [31] studied 20 patients with proven A. phalloides intoxication (positive urinary amanitin toxin by ELISA). In this study, 9/20 received Prometheus treatment, 11/20 did not. All 20 patients received activated charcoal, fluids, NAC, and silibinin. The study was not randomized and used matched controls; however, some of the matched controls were treated years earlier than some of the patients in the treatment group (some are historical controls). Bergis et al. found that mean urinary amanitin levels and mortality were reduced by Prometheus, with a mortality rate of 0 %, without liver transplantation. The mortality rate for the control group was 9 %; however, this difference was not statistically significant [31].
In the absence of randomized controlled trials, limited numbers of patients treated with liver albumin dialysis, and differences in supportive care measures, it is difficult to make definitive recommendations regarding liver albumin dialysis treatment. However, it appears that liver albumin dialysis treatments often improve encephalopathy and hemodynamic parameters, lower AST, ALT, and ammonia levels, and allow some patients to undergo liver transplantation in better condition [31, 37, 89, 98, 121]. Conversely, there are also case reports of patients with fulminant hepatic failure and encephalopathy who recover without MARS, FPSA, or liver transplantation [123].
Liver transplantation dramatically increases the survival rate of amatoxin-induced ALF [116]. While orthotopic liver transplantation (OLT) has been generally considered the gold-standard treatment of amatoxin-induced ALF, there are also reports of auxiliary partial liver transplantation resulting in eventual regeneration of the native liver, allowing for eventual successful cessation of immunosupressive therapy. Therefore, auxiliary, rather than orthotopic, liver transplantation may be considered in some cases [25, 124]. The specific criteria for emergent transplantation have been debated and many sets of criteria exist [100, 116, 125, 126] (see Table 4). Various reports discuss the successful and unsuccessful application of these criteria. Ferreira et al. [100] reported on ten patients poisoned with A. phalloides, including four deaths, and found that the Escudie’s criteria provided better prognostic indicators than Clichy or King’s College criteria. However, some have criticized Escudie’s criteria because the study analyzed data assuming that transplanted patients would have otherwise died; half of the patients in the ‘fatal intoxication group’ actually received OLT [127]. Escudie has criticized Ganzert’s criteria after finding that 2/19 patients that meet Ganzert’s criteria for transplant recovered without transplantation, while one patient died despite not meeting Ganzert’s criteria [128]. Escudie found that both the Clichy’s and Ganzert’s criteria failed to predict some fatal outcomes. Escudie et al. [25] reports that later in a patient’s clinical course, King’s College criteria were superior to Clichy’s and Ganzert’s criteria. However, Ganzert et al. [127] rebuts, stating that Escudie did not implement the Ganzert’s criteria correctly to draw these conclusions. Garcia de la Fuente reports on an infant that survived amatoxin-induced ALF without transplantation, noting that the King’s College criteria and Clichy’s criteria predicted a poor outcome, while Ganzert’s and Escudie’s criteria correctly predicted a good outcome [116]. In an Australian case series, the prognostic value of (1) onset of diarrhea < 8 h after mushroom ingestion and INR ≥ 6 on day 4 was compared to (2) INR ≥ 2.5 and serum Cr > 106 μmol/l on Day 3, based on previous reports by Ferreira and Ganzert [36, 100, 127]. These prognostic factors for mortality did not prove useful in this series. In this Australian report, patients who died had higher blood lactate levels (>5 mmol/l), compared with survivors [36]. These conflicting reports and debates among experts in the field make utilizing appropriate predictors of outcome and need for OLT difficult. Further, the studies generally have limitations of: limited patient enrollment, retrospective analyses, and utilization of historical controls.
Table 4.
Various liver transplant criteria (e.g. poor prognosis without transplantation)
| Criteria name | OLT criteria (fatal outcome likely without OLT) |
|---|---|
| Clichy’sa | Grade 3 or 4 encephalopathy with either a decrease of factor V below 30 % of normal in patients > 30 y.o. or a decrease of factor V below 20 % of normal in patients < 30 y.o. |
| Escudie’sb | Interval between ingestion of mushroom and the onset of diarrhea < 8 h OR decrease in prothrombin index below 10 % of normal (approximately an INR > 6) 4 or more days after ingestion |
| Ganzert’sb | Prothrombin index < 25 % of normal in conjunction with a serum creatinine > 106 μmol/l (both measured between days 3 and 10 post-ingestion) |
| King’s College (non-paracetamol)c | INR > 6.5 or any three of the following: patient < 11 y.o. or >40 y.o.; serum bilirubin > 300 μmol/l; time from onset of jaundice to development of coma > 7 days; INR > 3.5; drug toxicity regardless of whether it was the cause of the acute liver failure |
| King’s College (paracetamol) | Arterial pH below 7.3 or arterial lactate above 3 mmol/l after adequate fluid resuscitation or concurrent serum Cr > 300 μmol/l, INR > 6.5, and grade 3 or 4 encephalopathy |
y.o. years old
aLate in course, King’s criteria more useful
bCriteria specifically developed for amatoxin
cNon-paracetamol criteria best
Nephrotoxins
Most severe, mycetism-induced renal failure is due to Cortinarius species [5].
Toxins and Pathophysiology
Orellanine (which occurs as orellanine-4,4′-diglucopyranoside in some species) is a nephrotoxic bipyridine N-dioxide found in some Cortinarius species, including C. orellanus (Fool’s Webcap), C. speciosissimus, or C. rubellus (Deadly Webcap), and Cortinarius orellanosus [2, 8, 10, 18, 29, 30, 129, 130]. C. orellanosus has been found in Michigan, while C. orellanus is found in Europe [129]. These mushrooms have been mistaken for edible Cantharellus cibarius, Cantharellus tabaeformis, Boletus edulis (Ceps or Porcinis) and for hallucinogenic Psilocybe mushrooms [2, 18, 130]. Orellanine is concentrated in the kidney [10]. Further, oxidation of orellanine in renal tissue may accumulate quinone compounds, producing cell damage [2]. Orellanine interferes with RNA polymerase B and inhibits alkaline phosphatase in the proximal tubule cells, leading to disruption of ATP production [10, 15]. Extracts of Cortinarius orellanus diminish the number of sulfhydrilic groups and deplete glutathione in renal and hepatic tissue [10]. Oxygen-free radical formation may contribute to the cytotoxic damage as well [10, 130]. The tubular epithelium is the toxin’s primary target [131].
Clinical Presentation
This presentation is sometimes referred to as the “Orellanus syndrome” [4]. Patients present with delayed vomiting and diarrhea followed by oliguria or anuria [129–132]. A clinical latency of 36 h to 21 days has been reported. A shorter latency period is associated with a poorer prognosis [10]. Typically, vomiting and diarrhea occur 3 days after ingestion, which is followed by intense thirst, chills and evidence of acute renal failure which develops 8–9 days after ingestion [2, 129, 132]. Patients may present with fatigue, nausea, vomiting, headache, weakness, myalgias, and flank pain [10]. Polyuria is followed by oligo-anuria [10]. Creatinine and BUN rise. Associated electrolyte abnormalities, such as hyponatremia, hyperkalemia, and acidosis, may be noted [10, 129, 131]. Ultrasound may reveal enlarged kidneys with reduced echogenicity of the medulla and papillae [10]. Renal biopsy reveals evidence of acute tubular necrosis with interstitial nephritis and edema. The glomeruli and renal vessels are typically intact [10, 33, 129, 131]. Progressive fibrosis may ensue [123].
Toxin Detection
Diagnosis may be made by microscopic evaluation of mushroom spores [10, 131]. Alternatively, orellanine can be tested for by adding a drop of 2 % iron (III) chloride in 0.5 N HCl to the liquid pressed from fresh or rehydrated mushroom fragments. If orellanine is present, the initially yellow liquid immediately stains purple red to violet [5, 10]. Orellanine can be detected by thin-layer chromatography (TLC), electrophoresis, UV detection, and HPLC-ESI-MS/MS [130]. If orellanine is going to be assessed in renal biopsy tissue, care must be taken to protect the specimen from light, as orellanine is light-sensitive [5]. In renal biopsy tissue, orellanine is detectable TLC up to 6 months after poisoning [10].
Prognosis
Acute renal failure occurs in 30 % to 75 % of patients [10, 29, 30]. As many as 50 % of those requiring early dialysis will develop chronic renal failure [10, 123, 129, 131, 133]. Some patients, who do not require hemodialysis, will still show evidence of chronic renal insufficiency. Only 30 % of those poisoned have complete recovery of renal function [10, 131]. Case series suggest that children may suffer a worse prognosis than adults [131].
Treatment
Treatment is supportive and includes renal replacement therapy. Some have recommended anti-oxidant treatment with steroids and NAC; however, these treatments are based on anecdotal reports [10, 131, 134]. Furosemide may worsen injury, possibly due to concentrating orellanine in the kidney [131]. Renal transplantation has been utilized [10, 32, 129, 131].
Other Nephrotoxic Mushrooms
Relatively accelerated nephrotoxic mushroom syndromes are described after Amanita proxima (Mediterranean Amidella) and Amanita smithiana (toxic Lepidella Amanita or North American Lepidella) ingestions [4]. This is sometimes referred to as the “Amanita nephrotoxic syndrome” [4]. A. smithiana has been found along the Pacific coast of North America and less commonly in Idaho, Nevada and New Mexico [135]. A. smithiana contains A. smithiana toxin. Amanita boudieri, A. echinocephala, and A. gracilior also contain A. smithiana toxin and present similarly [4, 5, 129, 135–139]. A. smithiana toxin is not present in A. proxima, but the presentation, is nonetheless, similar [5, 46]. A. smithiana toxin may be detected by TLC [135].
A 20 min–24 h latency period is followed by GI symptoms. The GI symptoms occur more rapidly when the mushrooms are ingested raw. This is followed by nephrotoxicity within 1–6 days. Tubulointerstitial nephritis is characteristic. Mild cytolytic hepatitis can also be seen and the liver enzymes may rise before the creatinine rises [4, 15, 32, 129, 135–138]. De Haro et al. [140] reported on 53 patients poisoned by A. proxima and found 38 % had an increased creatinine, 32 % were oliguric or anuric, and 24.5 % required hemodialysis. The renal failure is secondary to interstitial nephritis and is generally reversible [5]. Some patients require hemodialysis, but this requirement generally resolves within several weeks [5].
Amanita psuedoporphyria Hongo ingestion has also been associated with delayed onset acute renal failure. This mushroom does not contain A. smithiana toxin, but it does contain 2-amino-4,5-hexadienoic acid (allenic norleucine), which is also found in A. smithiana [4, 5, 135, 137]. However, allenic norleucine is no longer thought to be responsible for A. proxima or A. smithiana toxicity [4, 5, 135]. Regardless, acute tubular necrosis is seen and hemodialysis may be required for several weeks [137].
A. phalloides can produce acute renal failure characterized by tubular necrosis particularly of the proximal renal tubules. Biopsy has revealed epithelial damage with tubular epithelial cell-shedding, apoptosis, and tubular epithelium atrophy. The renal failure associated with A. phalloides ingestion may ensue after the liver has recovered or after OLT. Renal replacement therapy has been utilized and long-term hemodialysis is occasionally required [14, 95, 123].
Mushroom ingestions that cause rhabdomyolysis (discussed next) may also produce renal injury.
Myotoxins
Rhabdomyolysis has been associated with repetitive ingestions of T. equestre (also known as T. flavovirens, T. auratum, and Yellow Trich or Yellow Knight or Man on Horseback). Several, generally three to nine consecutive, meals of T. equestre mushrooms (100–400 g) must be consumed to develop toxicity [2]. Rhabdomyolysis also follows ingestions of R. subnigricans (Blackening Russula), and some Cortinarius species [10, 15, 33, 49, 141].
Clinical presentation
Four patients presented after consuming T. equestre for several days. Adults presented with fatigue, muscle weakness, myalgias, nausea, and profuse diaphoresis, 1–2 days after their last mushroom meals. A young child presented with coma, cyanosis, hypertonia, and convulsions within 4 h of his last mushroom meal. Two of four patients required ventilatory support for respiratory failure, and one died from cardiac arrest. The maximal CK was nearly 50,000 U/l [141]. In other case reports, the CK has risen to 600,000 U/l. Moderate elevation of liver transaminases is also reported (AST 800 to 2,000 U/l; ALT 400 U/l) in some patients; this may be secondary to rhabdomyolysis. Occasionally, marked elevation of liver transaminases is noted (AST > 8,000 U/l); this may represent hepatic injury [142]. The mortality rate is 20 % [141].
R. subnigricans contains cycloprop-2-ene carboxylic acid, which triggers rhabdomyolysis [143]. In Asia, ingestion of R. subnigricans typically results in nausea, vomiting, and diarrhea within 30 min to 2 h of ingestion. Patients may recover or may present with delayed complaints of muscle pain and weakness, with associated rhabdomyolysis, myoglobinuria, renal failure, and hyperkalemia. Speech impairment, convulsions, and loss of consciousness have also been reported [143, 144].
Myotoxic mushrooms may cause profound muscle weakness and patients may be unable to sit or stand, require mechanical ventilation, and require prolonged bladder catheterization [141]. When patients recover, they may experience muscle weakness for several weeks to months [71, 72, 143, 144].
Myotoxic mushrooms may injure cardiac muscle, resulting in cardiopulmonary complications including respiratory failure, pulmonary edema, myocarditis, dysrhythmias (e.g., ventricular tachycardia), and cardiovascular collapse. Death may occur. This is reported after ingestions of R. subnigricans and T. equestre [141].
Muscle biopsies after T. equestre poisoning have revealed myofibrils that appear nibbled and separated by edema. Autopsies have revealed acute myopathy of skeletal muscle, diaphragm muscle, and myocardium [32, 71, 72, 141].
Immunologic/Hematologic Toxins
Repeated ingestion of Paxillus involutus (Poison Pax; Brown Roll-Rim) may produce immunohemolytic anemia. Antibodies against the mushroom produce immune-complex-mediated hemolysis. Symptoms may begin < 6 h from ingestion and include gastroenteritis and shock. Interstitial nephritis and hepatorenal failure may ensue. Hemodialysis may be required. Some have recommended corticosteroid and plasma exchange treatment [32, 49, 145, 146].
Yoon reports [17] that, in northeast Asia, a reversible pancytopenia, with a normocytic, normochromic anemia, and associated fever has been reported after consuming a decoction of Ganoderma neojaponicum Imazeki, as an herbal medicine.
In Japan, China, Korea, and Java, Podostroma cornu-damae may produce toxicity. In one case series, misidentification for Ganoderma lucidum, which is nontoxic, lead to poisoning. Podostroma cornu-damae contains trichothecene mycotoxins including satratoxins, tratoxin, roridin, and verucarin. Ingestion produces GI distress, followed by dehydration and hypotension, oliguria, altered mental status, leukopenia, thrombocytopenia, lamellar desquamation of the palms and face, and alopecia. Multiple organ failure and death may occur. Patients may succumb to sepsis secondary to pancytopenia. Treatment includes supportive care, antibiotics to cover neutropenic fever, and granulocyte colony-stimulating factor for pancytopenia [147].
Allergic reactions to mushrooms have been described with B. edulis (Porcini; King Bolete), Agaricus bisporus (Button Mushroom) and Lentinula edodes (Shiitake). A diffuse, pruritic dermatitis has been reported after touching or eating Shiitake mushrooms [49].
Mitochondrial Toxins
P. porrigens (Angel’s Wing), G. frondosa, and P. eringii are cyanogenic. Poisoning may present like an encephalopathic syndrome. The convulsive encephalopathy seen after P. porrigens ingestion is discussed above, under epileptogenic syndromes [49, 50, 148, 149].
Summary
New toxic mushroom species continue to be identified. Some species initially classified as edible are later reclassified as toxic. This results in a continually expanding list of toxic mushrooms. As new toxic species are identified, some classic teachings about mycetism no longer hold true. One example is the utilization of a time line for development of GI systems as a prognosticator. We now recognize that this time line is flawed, since patients who have early GI symptoms may develop significant systemic toxicity after mushroom ingestion. As more toxic mushrooms are identified and more toxic syndromes are reported, older classification systems fail to effectively accommodate mycetism. This review classified mushroom poisonings by the primary organ system affected and subclassified mushroom poisonings by the type of syndrome produced within each organ system affected. This classification permits expansion, as new, toxic mushroom species are discovered, and it allows clinicians to determine the species most likely responsible for illness in their patients. This approach may facilitate ordering specific diagnostic tests and providing specific treatments in conjunction with intensive, supportive care.
References
- 1.Hawksworth DL, Wiltshire PEJ. Forensic mycology: the use of fungi in criminal investigations. Forensic Sci Int. 2011;206:1–11. doi: 10.1016/j.forsciint.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 2.Lima ADL, Costa Fortes R, Carvalho Garbi Novaes MR, et al. Poisonous mushrooms: a review of the most common intoxications. Nutr Hosp. 2012;27(2):402–408. doi: 10.1590/S0212-16112012000200009. [DOI] [PubMed] [Google Scholar]
- 3.Mendez-Navarro J, Ortiz-Olivera NX, Villegas-Rios M, et al. Hepatotoxicity from ingestion of wild mushrooms of the genus Amanita section Phalloideae collected Mexico City: two case reports. Ann Hepatol. 2011;10(4):568–574. [PubMed] [Google Scholar]
- 4.Kirchmair M, Carrilho P, Pfab R, et al. Amanita poisoning resulting in acute, reversible renal failure: new cases, new toxic Amanita mushrooms. Nephrol Dial Transplant. 2012;27:1380–1386. doi: 10.1093/ndt/gfr511. [DOI] [PubMed] [Google Scholar]
- 5.Kirchmair M, Poder R. Fatal renal failure caused by Cortinarius mushrooms. Pediatr Nephrol. 2011;26:487–488. doi: 10.1007/s00467-010-1664-1. [DOI] [PubMed] [Google Scholar]
- 6.Yardan T, Baydin A, Eden AO, et al. Wild mushroom poisoning in the Middle Black Sea region in Turkey: analysis of 6 years. Hum Exp Toxicol. 2010;29(9):767–771. doi: 10.1177/0960327110361758. [DOI] [PubMed] [Google Scholar]
- 7.Eren SH, Demirel Y, Ugurlu S, et al. Mushroom poisoning: retrospective analysis of 294 cases. Clinics. 2010;65(5):491–496. doi: 10.1590/S1807-59322010000500006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Diaz JH. Evolving global epidemiology, syndromic classification, general management, and prevention of unknown mushroom poisonings. Crit Care Med. 2005;33:419–426. doi: 10.1097/01.ccm.0000153530.32162.b7. [DOI] [PubMed] [Google Scholar]
- 9.Erguven M, Yilmaz O, Deveci M, et al. Mushroom poisoning. Indian J Pediatr. 2007;74(9):847–852. doi: 10.1007/s12098-007-0151-6. [DOI] [PubMed] [Google Scholar]
- 10.Frank H, Zilker T, Kirchmair M, Eyer F, et al. Acute renal failure by ingestion of Cortinarius species confounded with psychoactive mushrooms: a case series and literature survey. Clin Nephrol. 2009;71(5):557–562. doi: 10.5414/cnp71557. [DOI] [PubMed] [Google Scholar]
- 11.Nordt SP, Manoguerra A. 5 year analysis of mushroom exposures in California. West J Med. 2000;173(5):314–317. doi: 10.1136/ewjm.173.5.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levine M, Ruha AM, Graeme K, et al. Toxicology in the ICU: Part 3. Natural toxins. Chest. 2011;140(5):1357–1370. doi: 10.1378/chest.11-0295. [DOI] [PubMed] [Google Scholar]
- 13.French LK, Hendrickson RG, Horowitz BZ. Amanita phalloides poisoning. Clin Toxicol. 2011;49:128–129. doi: 10.3109/15563650.2011.557663. [DOI] [PubMed] [Google Scholar]
- 14.Mootram A, Lazio M, Bryant S. Lepiota subincarnata J.E. Lange induced fulminant hepatic failure presenting with pancreatitis. J Med Toxicol. 2010;6(2):155–157. doi: 10.1007/s13181-010-0062-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Syed VA, Lakshi R, Karki P, et al. Scenario of mushroom poisoning in a tertiary care. JNMA J Nepal Med Assoc. 2009;48(176):296–300. [PubMed] [Google Scholar]
- 16.Lurie Y, Wasser SP, Taha M, et al. Mushroom poisoning from species of genus Inocybe (fiber head mushroom): a case series with exact species. Clin Toxicol. 2009;47(6):562–565. doi: 10.1080/15563650903008448. [DOI] [PubMed] [Google Scholar]
- 17.Yoon YH, Choi SH, Cho HJ, et al. Reversible pancytopenia following the consumption of decoction of Ganoderma neojaponicum Imazeki. Clin Toxicol. 2011;49(2):115–117. doi: 10.3109/15563650.2011.553834. [DOI] [PubMed] [Google Scholar]
- 18.Evans N, Hamilton A, Bello-Villaba MJ, et al. Irreversible renal damage from accidental mushroom poisoning. BMJ. 2012;345:35262. doi: 10.1136/bmj.e5262. [DOI] [PubMed] [Google Scholar]
- 19.Ward J, Kapadia K, Brush E, et al. Amatoxin poisoning: case reports and review of current therapies. J Emerg Med. 2013;44(1):116–121. doi: 10.1016/j.jemermed.2012.02.020. [DOI] [PubMed] [Google Scholar]
- 20.Schenk-Jaeger K, Rauber-Luthy C, Bodmer M, et al. Mushroom poisoning: a study on circumstances of exposure and patterns of toxicity. Eur J Int Med. 2012;23:e85–e91. doi: 10.1016/j.ejim.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 21.Chan TY, Chiu Wild mushroom poisonings in Hong Kong. Southeast Asian J Trop Med Public Health. 2011;42(2):468–469. [PubMed] [Google Scholar]
- 22.Zhong ZY, Shi GQ, Fontaine R, et al. Evidence for the natural toxins from the mushroom Trogia venenata as a cause of sudden unexpected death in Yunnan Province, China. Angew Chem Int Ed Engl. 2012;51(10):2368–2370. doi: 10.1002/anie.201106502. [DOI] [PubMed] [Google Scholar]
- 23.Koppel C. Clinical symptomatology and management of mushroom. Toxicon. 1993;31(12):1513–1540. doi: 10.1016/0041-0101(93)90337-i. [DOI] [PubMed] [Google Scholar]
- 24.Lehmann PF, Khazan U. Mushroom poisoning by Chlorophyllum molybdites in the Midwest United States. Cases and a review of the syndrome. Mycopathologia. 1992;118(1):3–13. doi: 10.1007/BF00472564. [DOI] [PubMed] [Google Scholar]
- 25.Escudie L, Francoz C, Vinel JP, Moucari R, Cournot M, Paradis V, et al. Amanita phalloides poisoning: reassessment of prognostic factors and indications for emergency liver transplantation. J Hepatol. 2007;46(3):466–473. doi: 10.1016/j.jhep.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 26.Ahishali E, Boynuegri B, Ozpolat E, et al. Approach to mushroom intoxication and treatment: can we decrease mortality? Clin Res Hepatol Gastroenterol. 2012;36:139–145. doi: 10.1016/j.clinre.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 27.Wu BF, Wang MM. Molecular adsorbent recirculating system in dealing with maternal Amanita poisoning during the second pregnancy trimester: a case report. Hepatobil Pancreatol Dis Int. 2004;3(1):152–154. [PubMed] [Google Scholar]
- 28.Beuhler MC, Sasser HC, Watson WA. The outcome of North American pediatric unintentional mushroom ingestions with various decontamination treatments: an analysis of 14 years of TESS data. Toxicon. 2009;53:437–443. doi: 10.1016/j.toxicon.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 29.Berger KJ, Guss DA. Mycotoxins revistied: part I. J Emerg Med. 2005;28(1):53–62. doi: 10.1016/j.jemermed.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 30.Berger KJ, Guss DA. Mycotoxins revisited: part II. J Emerg Med. 2005;28(2):175–183. doi: 10.1016/j.jemermed.2004.08.019. [DOI] [PubMed] [Google Scholar]
- 31.Bergis D, Friedrich-Rust M, Zeuzem S, et al. Treatment of Amanita phalloides intoxication by fractionated plasma separation and adsorption (Prometheus) J Gastrointest Liver Dis. 2012;21(2):171–176. [PubMed] [Google Scholar]
- 32.Diaz JH. Syndromic diagnosis and management of confirmed mushroom poisonings. Crit Care Med. 2005;33(2):427–436. doi: 10.1097/01.ccm.0000153531.69448.49. [DOI] [PubMed] [Google Scholar]
- 33.Karlson-Stiber C, Persson H. Cytotoxic fungi—an overview. Toxicon. 2003;42(4):339–349. doi: 10.1016/s0041-0101(03)00238-1. [DOI] [PubMed] [Google Scholar]
- 34.Magdalan J, Piotrowska A, Gomulkiewicz A, Sozanski T, Szelag A, Dziegiel P. Influence of commonly used clinical antidotes on antioxidant systems in human hepatocyte culture intoxicated with alpha-amatoxin. Hum Exp Toxicol. 2010;30(1):38–43. doi: 10.1177/0960327110368418. [DOI] [PubMed] [Google Scholar]
- 35.Magdalan J, Ostrowska A, Piotrowska, et al. Alpha-amanitin induced apoptosis in primary cultured dog hepatocytes. Folia Histochem Cytobiol. 2010;48(1):58–62. doi: 10.2478/v10042-010-0010-6. [DOI] [PubMed] [Google Scholar]
- 36.Roberts DM, Hall MJ, Falkland MM, et al. Amanita phalloides poisoning and treatment with silibinin in the Australian Capital Territory and New South Wales. Med J Aust. 2013;198(1):43–47. doi: 10.5694/mja12.11180. [DOI] [PubMed] [Google Scholar]
- 37.Sorodoc L, Lionte C, Sorodoc V, Petris O, Jaba I. Is MARS system enough for A. phalloides-induced liver failure treatment? Hum Exp Toxicol. 2010;29(10):823–832. doi: 10.1177/0960327110363327. [DOI] [PubMed] [Google Scholar]
- 38.Trabulus S, Altiparmak MR. Clinical features and outcome of patients with amatoxin-containing mushroom poisoning. Clin Toxicol. 2011;49:303–310. doi: 10.3109/15563650.2011.565772. [DOI] [PubMed] [Google Scholar]
- 39.Lukasik-Glebocka M, Druzdz A, Naskret M. Clinical symptoms and circumstances of acute poisoning with fly agaric (Amanita muscaria) and panther cap (Amanita pantherina) Przegl Lek. 2011;68(8):449–452. [PubMed] [Google Scholar]
- 40.Pauli JL, Foot CL. Fatal muscarinic syndrome after eating wild mushrooms. Med J Aust. 2005;182:294–295. doi: 10.5694/j.1326-5377.2005.tb06705.x. [DOI] [PubMed] [Google Scholar]
- 41.Saviuc P, Harry P, Pulce C, et al. Can morels (Morcella sp.) induce a toxic neurological syndrome? Clin Toxicol. 2010;48(4):365–372. doi: 10.3109/15563651003698034. [DOI] [PubMed] [Google Scholar]
- 42.Michelot D, Toth B. Poisoning by Gyromitra esculenta—a review. J Appl Toxicol. 1991;11(4):235–243. doi: 10.1002/jat.2550110403. [DOI] [PubMed] [Google Scholar]
- 43.Flammer R, Gallen S. Hemolysis in mushroom poisoning; facts and hypotheses. Schweiz Med Wochenschr. 1983;113(42):1555–1561. [PubMed] [Google Scholar]
- 44.Leathem AM, Dorran TJ. Poisoning due to raw Gyromitra esculenta (false morels) west of the Rockies. CJEM. 2007;9(2):127–130. doi: 10.1017/s1481803500014937. [DOI] [PubMed] [Google Scholar]
- 45.Lheureux P, Penaloza A, Gris M. Pyridoxine in clinical toxicology: a review. Eur J Emerg Med. 2005;12(2):78–85. doi: 10.1097/00063110-200504000-00007. [DOI] [PubMed] [Google Scholar]
- 46.Gejyo F, Homma N, Higuchi N, et al. A novel type of encephalopathy associated with mushroom Sugihiratake ingestion in patients with chronic kidney diseases. Kidney Int. 2005;68(1):188–192. doi: 10.1111/j.1523-1755.2005.00393.x. [DOI] [PubMed] [Google Scholar]
- 47.Kuwabara T, Arai A, Honma N. Acute encephalopathy among patients with renal dysfunction after ingestion of “sugihiratake”, angel’s wing mushroom—study on the incipient cases in the northern area of Niigata Prefecture. Rinsho Shinkeigaku. 2005;45(3):239–245. [PubMed] [Google Scholar]
- 48.Kurokawa K, Sato H, Nakajima K, Kawanami T, Kato T. Clinical, neuroimaging and electroencephalographic findings of encephalopathy occurring after the ingestion of “sugihiratake” (Pleurocybella porrigens), an autumn mushroom: a report of two cases. Rinsho Shinkeigaku. 2005;45(2):111–116. [PubMed] [Google Scholar]
- 49.Saviuc P, Danel V. New syndromes in mushroom poisoning. Toxicol Rev. 2006;25(3):199–209. doi: 10.2165/00139709-200625030-00004. [DOI] [PubMed] [Google Scholar]
- 50.Obara K, Okawa S, Kobayashi M, et al. A case of encephalitis-type encephalopathy related to Pleurocybella porrigens (Sugihiratake) Rinsho Shinkeigaku. 2005;45(3):253–256. [PubMed] [Google Scholar]
- 51.Stribrny J, Sokol M, Merova B, et al. GC/MS determination of ibotenic acid and muscimol in the urine of patients intoxicated with Amanita pantherina. Int J Legal Med. 2012;126:519–524. doi: 10.1007/s00414-011-0599-9. [DOI] [PubMed] [Google Scholar]
- 52.Hiroshima Y, Nakae H, Gommon K. Amanita ibotengutake intoxication treated with plasma exchange. Ther Apher Dial. 2010;14(5):483–484. doi: 10.1111/j.1744-9987.2010.00862.x. [DOI] [PubMed] [Google Scholar]
- 53.Benjamin DR. Mushroom poisoning in infants and children: the Amanita pantherina/muscaria group. J Toxicol Clin Toxicol. 1992;30(1):13–22. doi: 10.3109/15563659208994442. [DOI] [PubMed] [Google Scholar]
- 54.Michelot D, Melendez-Howell LM. Amanita muscaria: chemistry, biology, toxicology, and ethnomycology. Mycol Res. 2003;107(Pt 2):131–146. doi: 10.1017/s0953756203007305. [DOI] [PubMed] [Google Scholar]
- 55.Satora L, Pach D, Butryn B, Hydzik P, Balicka-Slusarczyk B. Fly agaric (Amanita muscaria) poisoning, case report and review. Toxicon. 2005;45(7):941–943. doi: 10.1016/j.toxicon.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 56.Tupalska-Wilczynska K, Ignatowicz R, Poziemski A, Wojcik H, Wilczynski G. Poisoning with spotted and red mushrooms—pathogenesis, symptoms, treatment. Wiad Lek. 1996;49(1–6):66–71. [PubMed] [Google Scholar]
- 57.Beck O, Helander A, Karlson-Stiber SN. Presence of phenylethylamine in hallucinogenic Psilocybe mushroom: possible role in adverse reactions. J Anal Toxicol. 1998;22(1):45–49. doi: 10.1093/jat/22.1.45. [DOI] [PubMed] [Google Scholar]
- 58.Satora L, Goszcz H, Ciszowski K. Poisonings resulting from the ingestion of magic mushrooms in Krakow. Przegl Lek. 2005;62(6):394–396. [PubMed] [Google Scholar]
- 59.McCawley EL, Brummett RE, Dana GW. Convulsions from Psilocybe mushroom poisoning. Proc West Pharmacol Soc. 1962;5:27–33. [PubMed] [Google Scholar]
- 60.Borowiak KS, Ciechanowski K, Waloszczyk P. Psilocybin mushroom (Psilocybe semilanceata) intoxication with myocardial infarction. J Toxicol Clin Toxicol. 1998;36(1–2):47–49. doi: 10.3109/15563659809162584. [DOI] [PubMed] [Google Scholar]
- 61.Pierrot M, Josse P, Raspiller MF, Goulmy M, Rambourg MO, Manel J, et al. Intoxications by hallucinogenic mushrooms. Ann Med Interne. 2000;151(Suppl B):B16–B19. [PubMed] [Google Scholar]
- 62.Saviuc P, Danel VC, Moreau PA. Erythromelalgia and mushroom poisoning. J Toxicol Clin Toxicol. 2001;39(4):403–407. doi: 10.1081/clt-100105162. [DOI] [PubMed] [Google Scholar]
- 63.Taguchi T, Tomotoshi K, Mizumura K. Excitatory actions of mushroom poison (acromelic acid) on unmyelinated muscular afferents in the rat. Neurosci Lett. 2009;456(2):69–73. doi: 10.1016/j.neulet.2009.03.102. [DOI] [PubMed] [Google Scholar]
- 64.Minami T, Matsumura S, Nishizawa M, et al. Acute and late effects of induction of allodynia by acromelic acid, a mushroom poison related structurally to kainic acid. Br J Pharmacol. 2004;142(4):679–688. doi: 10.1038/sj.bjp.0705834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shi G, He J, Shen T, et al. Hypoglycemia and death in mice following experimental exposure to an extract of Trogia venenata mushrooms. PLoS ONE. 2012;7(6):e38712. doi: 10.1371/journal.pone.0038712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Stone R. Heart-stopping revelation about how Chinese mushroom kills. Science. 2012;335:1293. doi: 10.1126/science.335.6074.1293. [DOI] [PubMed] [Google Scholar]
- 67.Zhang Y, Li Y, Wu G, et al. Evidence against barium in the mushroom Trogia venenata as a cause of sudden unexpected death in Yunnan, China. Appl Environ Microbiol. 2012;78(24):8834. doi: 10.1128/AEM.01798-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Shi GQ, Huang WL, Zhang J, et al. Clusters of sudden unexplained death associated with the mushroom, Trogia venenata, in rural Yunnan. PLoS ONE. 2012;7(5):e35894. doi: 10.1371/journal.pone.0035894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhang J, Shi GQ, Huang WL, et al. Clinical features of unexpected sudden death clustered in 7 families in Yunnan Province. Zhonghua Xin Xue Guan Bing Za Zhi. 2008;36(7):613–617. [PubMed] [Google Scholar]
- 70.Huang L, Liu XL, Cao CS, et al. Outbreak of fatal mushroom poisoning with Amanita franchetii and Ramaria rufescens. BMJ Case Rep. 2009 doi: 10.1136/bcr.06.2008.0327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Anand J, Chwaluk P. Acute intoxication with Tricholoma equestre. Przegl Lek. 2010;67(8):617–618. [PubMed] [Google Scholar]
- 72.Lee PT, Wu ML, Tsai WJ, et al. Rhabdomyolysis: an unusual feature with mushroom poisoning. Am J Kidney Dis. 2001;38(4):E17. doi: 10.1053/ajkd.2001.27725. [DOI] [PubMed] [Google Scholar]
- 73.Aygul N, Duzenli MA, Ozdemir K, Altnkeser BB. A case report of an unusual complication of Amanita phalloides poisoning: development of cardiogenic shock and its successful treatment with intra-aortic ballon counterpulsation. Toxicon. 2010;55:630–632. doi: 10.1016/j.toxicon.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 74.Besancon A, Schmitt C, Glaizal M et al. (2012) Occurrence of severe cardiac alterations in Amanita proxima poisoning: two original observations. Ann Fr Anesth Reanim Mar 30 (Epub ahead of print) [DOI] [PubMed]
- 75.Besancon A, Schmitt C, Glaizal M, et al. Survenue d’une cardiaque severe au cours du syndrome proximien: deux observations originales. Ann Fr Anest Reanim. 2012;31:466–468. doi: 10.1016/j.annfar.2012.01.021. [DOI] [PubMed] [Google Scholar]
- 76.Sun YJ, Yuan W, Liu LG, et al. An outbreak of gastroenteritis caused by poisonous Boletus mushroom in Sichuan, China, 2012. Zhonghua Liu Xing Bing Xue Za Zhi. 2012;33(12):1261–1264. [PubMed] [Google Scholar]
- 77.Stenklyft PH, Augenstein WL. Chlorophyllum molybdites—severe mushroom poisoning in a child. J Toxicol Clin Toxicol. 1990;28(2):159–168. doi: 10.3109/15563659008993488. [DOI] [PubMed] [Google Scholar]
- 78.Yokoyama K, Gonmori K. Increase of poisoning by tropical mushrooms in Japan in recent years. Chudoku Kenkyu. 2009;22(3):240–248. [PubMed] [Google Scholar]
- 79.Haberl B, Pfab R, Berndt S, et al. Case series: alcohol intolerance with Coprine-like syndrome after consumption of the mushroom Lepiota aspera (Pers.:Fr.) Quel., 1886 (Freckled Dapperling) Clin Toxicol. 2011;49(2):113–114. doi: 10.3109/15563650.2011.554840. [DOI] [PubMed] [Google Scholar]
- 80.Carisson A, Henning M, Linberg P, et al. On the disulfiram-like effect of coprine, the pharmacologically active principle of Coprinus atramentarius. Acta Pharmacol Toxicol. 1978;42(4):292–297. doi: 10.1111/j.1600-0773.1978.tb02204.x. [DOI] [PubMed] [Google Scholar]
- 81.Michelot D. Poisoning by Coprinus atramentarius. Nat Toxins. 1992;1(2):73–80. doi: 10.1002/nt.2620010203. [DOI] [PubMed] [Google Scholar]
- 82.Budmiger H, Kocher F. Boletus luridus and alcohol—case report. Schweiz Med Wochenschr. 1982;112(34):1179–1181. [PubMed] [Google Scholar]
- 83.Ferenc T, Lukasiewicz CJ, Kowalczyk E. Poisonings with Amanita phalloides. Med Pr. 2009;60(5):415–426. [PubMed] [Google Scholar]
- 84.Santi L, Maggioli C, Mastroroberto M, et al. Acute liver failure caused by Amanita phalloides poisoning. Int J Hepatol. 2012;2012:487480. doi: 10.1155/2012/487480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mengs U, Pohl RT, Mitchell T. Legalon SIL: the antidote of choice in patients with acute hepatotoxicity from amatoxin poisoning. Curr Pharm Biotechnol. 2012;13(10):1964–1970. doi: 10.2174/138920112802273353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Beuhler M, Lee DC, Gerkin R. The Meixner test in the detection of alpha-amanitin and false-positive reactions caused by psilocin and 5-substituted tryptamines. Ann Emerg Med. 2004;44(2):114–120. doi: 10.1016/j.annemergmed.2004.03.017. [DOI] [PubMed] [Google Scholar]
- 87.Hu J, Zhang P, Zeng J, et al. Determination of amatoxins in different tissues and development stages of Amanita exitialis. J Sci Food Agric. 2012;92(13):2664–2667. doi: 10.1002/jsfa.5685. [DOI] [PubMed] [Google Scholar]
- 88.Chen WC, Kassi M, Saeed U, et al. A rare case of amatoxin poisoning in the state of Texas. Case Rep Gastroenterol. 2012;6:350–357. doi: 10.1159/000339692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wittebole X, Hantson P. Use of the molecular adsorbent recirculating system (MARS) for the management of acute poisoning with or without liver failure. Clin Toxicol. 2011;49(9):782–793. doi: 10.3109/15563650.2011.624102. [DOI] [PubMed] [Google Scholar]
- 90.Cress CM, Malliah A, Herrine SK. Fulminant hepatic failure due to Amanita phalloides toxicity. Clin Gastroenterol Hepatol. 2011;9(2):A26. doi: 10.1016/j.cgh.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 91.Antonyuk VO, Klyuchivska OY, Stoika RS. Cytotoxic proteins of Amanita virosa Secr. mushroom: purification, characteristics and action towards mammalian cells. Toxicon. 2010;55:1297–1305. doi: 10.1016/j.toxicon.2010.01.023. [DOI] [PubMed] [Google Scholar]
- 92.Vargas N, Bernal A, Sarria V, et al. Amatoxin and phallotoxin composition in species of the genus Amanita in Columbia: a taxonomic perspective. Toxicon. 2011;58:583–590. doi: 10.1016/j.toxicon.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 93.Stasyk T, Lutsik-Kordovshy M, Wernstedt C, et al. A newly highly toxic protein isolated from the death cap Amanita phalloides is an L-amino acid oxidase. FEBS J. 2010;277(5):1260–1269. doi: 10.1111/j.1742-4658.2010.07557.x. [DOI] [PubMed] [Google Scholar]
- 94.Shi Y, He J, Chen S, Zhang L, Yang X, Wang Z. MARS: optimistic therapy method in fulminant hepatic failure secondary to cytotoxic mushroom poisoning—a case report. Liver. 2002;22(Suppl 2):78–80. doi: 10.1034/j.1600-0676.2002.00017.x. [DOI] [PubMed] [Google Scholar]
- 95.Mrzljak A, Knotek M, Gustin D, et al. End-stage kidney disease after mushroom poisoning and ABO-incompatible liver transplantation. Nephrology. 2010;15(6):660–661. doi: 10.1111/j.1440-1797.2010.01277.x. [DOI] [PubMed] [Google Scholar]
- 96.Das RN, Parajuli S, Jayakumar J. Last supper with mushroom soup: a case report of amatoxin poisoning. Mcgill J Med. 2007;10(2):93–95. [PMC free article] [PubMed] [Google Scholar]
- 97.Giannini L, Vannacci A, Missanelli A, et al. Amatoxin poisoning: a 15 year retrospective analysis and follow up evaluation of 105 patients. Clin Toxicol. 2007;45(5):539–542. doi: 10.1080/15563650701365834. [DOI] [PubMed] [Google Scholar]
- 98.Lionte C, Sorodoc L, Simionescu V. Successful treatment of an adult with Amanita phalloides-induced fulminant liver failure with molecular adsorbent recirculating system (MARS) Rom J Gastroenterol. 2005;14(3):267–271. [PubMed] [Google Scholar]
- 99.Jander S, Bischoff J, Woodcock BG. Plasmapheresis in the treatment of Amanita phalloides poisoning: II. A review and recommendations. Ther Apher. 2000;4(4):308–312. doi: 10.1046/j.1526-0968.2000.004004308.x. [DOI] [PubMed] [Google Scholar]
- 100.Ferreira R, Romaozinha JM, Amaro P, Ferreira M, Sofia C. Assessment of emergency liver transplantation criteria in acute liver failure due to Amanita phalloides. Eur J Gastroenterol Hepatol. 2011;23(12):1226–1232. doi: 10.1097/MEG.0b013e32834c7b8f. [DOI] [PubMed] [Google Scholar]
- 101.Centers for Disease Control and Prevention (CDC) Amanita phalloides mushroom poisoning—North California. MMWR Morb Mortal Wkly Rep. 1997;46(22):489–492. [PubMed] [Google Scholar]
- 102.Fantozzi R, Ledda F, Caramelli L, et al. Clinical findings and follow-up evaluation of an outbreak of mushroom poisoning—survey of Amanita phalloides poisoning. Klin Wochenschr. 1986;54(1):38–43. doi: 10.1007/BF01721579. [DOI] [PubMed] [Google Scholar]
- 103.Harper KA, Smart CD, Davis RM. Development of a DNA-based macroarray for the detection and identification of Amanita species. J Forensic Sci. 2011;56(4):1003–1009. doi: 10.1111/j.1556-4029.2011.01739.x. [DOI] [PubMed] [Google Scholar]
- 104.Jansson D, Fredriksson SA, Herrmann A, et al. A concept study on identification and attribution profiling of chemical threat agents using liquid chromatography-mass spectrometry applied to Amanita toxins in food. Forensic Sci Int. 2012;221:44–49. doi: 10.1016/j.forsciint.2012.03.023. [DOI] [PubMed] [Google Scholar]
- 105.Fantozzi R, Ledda F, Caramelli L, et al. Clinical findings and follow-up evaluation of an outbreak of mushroom poisoning survey of Amanita phalloides poisoning. Klin Wochenschr. 1986;64:38–43. doi: 10.1007/BF01721579. [DOI] [PubMed] [Google Scholar]
- 106.Jan MA, Siddiqui TS, Ahmed N, et al. Mushroom poisoning in children: clinical presentation and outcome. J Ayub Med Coll Abbottabad. 2008;20(2):99–101. [PubMed] [Google Scholar]
- 107.Raschke RA, Curry SC, Rempe S, et al. Results of a protocol for the management of patients with fulminant liver failure. Crit Care Med. 2008;36(8):2244–2448. doi: 10.1097/CCM.0b013e31818029a3. [DOI] [PubMed] [Google Scholar]
- 108.D’Agostino D, Diaz S, Sanchez MC, Boldrini G. Management and prognosis of acute liver failure in children. Curr Gastroenterol Rep. 2012;14(3):262–269. doi: 10.1007/s11894-012-0260-x. [DOI] [PubMed] [Google Scholar]
- 109.Devictor D, Tissieres P, Durand P, Chevret L, Debray D. Acute liver failure in neonates, infants and children. Expert Rev Gastroenterol Hepatol. 2011;5(6):717–729. doi: 10.1586/egh.11.57. [DOI] [PubMed] [Google Scholar]
- 110.Ganzert M, Felgenhauer N, Schuster T, et al. Amanita poisoning—comparison of silibinin with a combination of silibinin and penicillin. Dtsch Med Wochenschr. 2008;133(44):2261–2267. doi: 10.1055/s-0028-1091268. [DOI] [PubMed] [Google Scholar]
- 111.Poucheret P, Fons F, Dore JC, Michelot D, Rapior S. Amatoxin poisoning treatment decision-making; pharmaco-therapeutic clinical strategy assessment using multidimensional multivariate statistic analysis. Toxicon. 2010;55(7):1338–1345. doi: 10.1016/j.toxicon.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 112.Magdalan J, Ostrowska A, Piotrowska A, et al. Comparative antidotal efficacy of benzylpenicillin, ceftazidime and rifamycin in cultured human hepatocytes intoxicated with alpha-amanitin. Arch Toxicol. 2009;83:1091–1096. doi: 10.1007/s00204-009-0466-3. [DOI] [PubMed] [Google Scholar]
- 113.Magdalan J, Ostrowska A, Piotrowska A, et al. Failure of benzylpenicillin, N-acetylcysteine and silibinin to reduce alpha-amanitin hepatotoxicity. Vivo. 2009;23(3):393–399. [PubMed] [Google Scholar]
- 114.Tong TC, Hernandez M, Richardson WH, 3rd, et al. Comparative treatment of alpha-amanitin poisoning with N-acetylcysteine, benzylpenicillin, cimetidine, thioctic acid, and silybin in a murine model. Ann Emerg Med. 2007;50(3):282–288. doi: 10.1016/j.annemergmed.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 115.Enjalbert F, Rapior S, Nouguier-Soule J, Guillon S, Amouroux N, Cabot C. Treatment of amatoxin poisoning: 20-year retrospective analysis. J Toxicol Clin Toxicol. 2002;40(6):715–717. doi: 10.1081/clt-120014646. [DOI] [PubMed] [Google Scholar]
- 116.Garcia de la Fuente I, McLin VA, Rimensberger PC, et al. Amanita poisoning and liver transplantation: do we have the right decision criteria? J Pediatr Gastroenterol Nutr. 2011;53(4):459–462. doi: 10.1097/MPG.0b013e318216f2c7. [DOI] [PubMed] [Google Scholar]
- 117.Mullins ME, Horowitz BZ. The futility of hemoperfusion and hemodialysis in Amanita phalloides poisoning. Vet Hum Toxicol. 2000;42:90–91. [PubMed] [Google Scholar]
- 118.Kacic M, Dujsin M, Puretic Z, Slavicek J. Mycetismus in children—report of an epidemic poisoning. Lijec Vjesn. 1990;112(11–12):369–373. [PubMed] [Google Scholar]
- 119.Covic A, Goldsmith DJ, Gusbeth-Tatomir P, Volovat C, Dimitriu AG, Cristogel F, et al. Successful use of molecular absorbent regenerating system (MARS) dialysis for the treatment of fulminant hepatic failure in children accidentally poisoned by toxic mushroom ingestion. Liver Int. 2003;23(Suppl 3):21–27. doi: 10.1034/j.1478-3231.23.s.3.9.x. [DOI] [PubMed] [Google Scholar]
- 120.Kantola T, Kantola T, Koivusalo AM, Hockerstedt K, Isoniemi H. Early molecular adsorbents recirculating system treatment of Amanita mushroom poisoning. Ther Apher Dial. 2009;13(5):399–403. doi: 10.1111/j.1744-9987.2009.00758.x. [DOI] [PubMed] [Google Scholar]
- 121.Vardar R, Gunsar F, Akarca U, Karasu Z. Efficacy of fractionated plasma separation and adsorption system (Prometheus) for treatment of liver failure due to mushroom poisoning. Hepato-Gastroenterology. 2010;57(99–100):573–577. [PubMed] [Google Scholar]
- 122.Faybik P, Hetz H, Baker A, et al. Extracorporeal albumin dialysis in patients with Amantia phalloides poisoning. Liver Int. 2003;23(Suppl 3):28–33. doi: 10.1034/j.1478-3231.23.s.3.8.x. [DOI] [PubMed] [Google Scholar]
- 123.Garrouste C, Hemery M, Boudat AM, Kamar N. Amanita phalloides poisoning-induced end-stage renal failure. Clin Nephrol. 2009;71(5):571–574. doi: 10.5414/cnp71571. [DOI] [PubMed] [Google Scholar]
- 124.Rosenthal P. Auxiliary liver transplant for Amanita phalloides poisoning. J Pediatr Gastroenterol Nutr. 2012;54(3):438. doi: 10.1097/MPG.0b013e318241ceaa. [DOI] [PubMed] [Google Scholar]
- 125.Araz C, Karaaslan P, Esen A, et al. Successful treatment of a child with fulminant liver failure and coma due to Amanita phalloides poisoning using urgent liver transplantation. Transplant Proc. 2006;38(2):596–597. doi: 10.1016/j.transproceed.2005.12.089. [DOI] [PubMed] [Google Scholar]
- 126.Yildiz BD, Abbasoglu O, Saglam A, et al. Urgent liver transplantation for Amanita phalloides poisoning. Pediatr Transplant. 2008;12(1):105–108. doi: 10.1111/j.1399-3046.2007.00838.x. [DOI] [PubMed] [Google Scholar]
- 127.Ganzert M, Felgenhauer N, Zilker T. Rassessment of predictors of fatal outcome in amatoxin poisoning: some critical comments. J Hepatol. 2007;47(3):424–425. doi: 10.1016/j.jhep.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 128.Durand F, Francoz C, Escudie L. Reply to “reassessment of predictors of fatal outcome in amatoxin poisoning: some critical comments. J Hepatol. 2007;47:424–427. doi: 10.1016/j.jhep.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 129.Judge BS, Ammirati JF, Lincoff GH, et al. Ingestion of a newly described North American mushroom species from Michigan resulting in chronic renal failure: Cortinarius orellanosus. Clin Toxicol. 2010;48:545–549. doi: 10.3109/15563650.2010.495346. [DOI] [PubMed] [Google Scholar]
- 130.Herrmann A, Hedman H, Rosen J, et al. Analysis of the mushroom nephrotoxin orellanine and its glucosides. J Nat Prod. 2012;75:1690–1696. doi: 10.1021/np300135k. [DOI] [PubMed] [Google Scholar]
- 131.Talmud D, Wynckel A, Grossenbacher F, et al. Four family cases of acute renal failure. Pediatr Nephrol. 2011;26:385–389. doi: 10.1007/s00467-010-1545-7. [DOI] [PubMed] [Google Scholar]
- 132.Alvarez TS, Gonzalez LA, Nava RA, et al. Mushroom poisoning: Orellanus syndrome. Nefrologia. 2011;31(4):495–496. doi: 10.3265/Nefrologia.pre2011.Apr.10824. [DOI] [PubMed] [Google Scholar]
- 133.Wessely M, Schonermarck U, Raziorrouh B, Jung MC, Samtleben W. Orellanus syndrome: a rare cause of acute renal failure. Dtsch Med Wochenschr. 2007;132(37):1880–1882. doi: 10.1055/s-2007-984979. [DOI] [PubMed] [Google Scholar]
- 134.Kilner RG, D’Souza RJ, Oliveria DB, et al. Acute renal failure from intoxication by Cortinarius orellanus: recovery using anti-oxidant therapy and steroids. Nephrol Dial Transplant. 1999;14(11):2779–2780. doi: 10.1093/ndt/14.11.2779-a. [DOI] [PubMed] [Google Scholar]
- 135.Apperley S, Kroeger P, Kirchmair M, et al. Laboratory confirmation of Amanita smithiana mushroom poisoning. Clin Toxicol. 2013;51:249–251. doi: 10.3109/15563650.2013.778995. [DOI] [PubMed] [Google Scholar]
- 136.Courtin P, Gallardo M, Berrouba A, et al. Renal failure after ingestion of Amanita proxima. Clin Toxicol. 2009;47(9):906–908. doi: 10.3109/15563650903289485. [DOI] [PubMed] [Google Scholar]
- 137.Iwafuchi Y, Morita T, Kobayashi H, et al. Delayed onset acute renal failure associated with Amanita pseudoporphyria Hongo ingestion. Intern Med. 2003;42(1):78–81. doi: 10.2169/internalmedicine.42.78. [DOI] [PubMed] [Google Scholar]
- 138.West PL, Lindgren J, Horowitz BZ. Amanita smithiana mushroom ingestion: a case of delayed renal failure and literature review. J Med Toxicol. 2009;5(1):32–38. doi: 10.1007/BF03160979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Yarze JC, Tulloss RE. Acute liver injury and renal failure due to poisonous mushroom (Amanita bisporigera) ingestion. Am J Gastroenterol. 2012;107:790–791. doi: 10.1038/ajg.2012.29. [DOI] [PubMed] [Google Scholar]
- 140.de Haro L, Jouglard J, Arditti J, David JM. Acute renal insufficiency caused by Amanita proxima poisoning: experience of the Poison Center of Marseille. Nephrologie. 1998;19:21–24. [PubMed] [Google Scholar]
- 141.Anand J, Chwaluk P, Sut M. Acute poisoning with Tricholoma equestre. Przegl Lek. 2009;66(6):339–340. [PubMed] [Google Scholar]
- 142.Bedry R, Baudrimont I, Deffieux G, et al. Wild-mushroom intoxication as a cause of rhabdomyolysis. N Engl J Med. 2001;345(11):798–802. doi: 10.1056/NEJMoa010581. [DOI] [PubMed] [Google Scholar]
- 143.Matsuura M, Saikawa Y, Inui K, et al. Identification of the toxic trigger in mushroom poisoning. Nat Chem Biol. 2009;5(7):465–467. doi: 10.1038/nchembio.179. [DOI] [PubMed] [Google Scholar]
- 144.Nishiyama K, Ohta Y, Matsuda N, et al. Back pain after wild mushroom consumption. Emerg Med J. 2010;27:61. doi: 10.1136/emj.2008.066803. [DOI] [PubMed] [Google Scholar]
- 145.Musselius SG, Ryk AA, Lebedev AG, et al. Toxicity of mushrooms Paxillus involutus and Paxillus atrotomentosus mushrooms. Anesteziol Reanimatol. 2002;2:30–35. [PubMed] [Google Scholar]
- 146.Winkelmann M, Stangel W, Schedel I, Grabensee B. Severe hemolysis caused by antibodies against the mushroom Paxillus involutus and its therapy by plasma exchange. Klin Wochenschr. 1986;64(19):935–938. doi: 10.1007/BF01728620. [DOI] [PubMed] [Google Scholar]
- 147.Ahn JY, Seok SJ, Song JE, et al. Two cases of mushroom poisoning by Podostroma Cornu-Damae. Yonsei Med J. 2013;54(1):265–268. doi: 10.3349/ymj.2013.54.1.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Gonmori K, Yokoyama K. Acute encephalopathy caused by cyanogenic fungi in 2004 and magic mushroom regulation in Japan. Chudoku Kenkyu. 2009;22(1):61–69. [PubMed] [Google Scholar]
- 149.Obara K, Wada C, Yoshioka T, et al. Acute encephalopathy associated with ingestion of a mushroom, Pleurocybella porrigens (Angel’s Wing), in a patient with chronic renal failure. Neuropathology. 2008;28(2):151–156. doi: 10.1111/j.1440-1789.2007.00819.x. [DOI] [PubMed] [Google Scholar]