Abstract
Atropine is the mainstay of therapy in organophosphate (OP) toxicity, though research and consensus on dosing is lacking. In 2004, as reported by Eddleston et al. (J Toxicol Clin Toxicol 42(6):865-75, 2004), they noted variation in recommended regimens. We assessed revisions of original references, additional citations, and electronic sources to determine the current variability in atropine dosing recommendations. Updated editions of references from Eddleston et al.’s work, texts of Internal and Emergency Medicine, and electronic resources were reviewed for atropine dosing recommendations. For comparison, recommendations were assessed using the same mean dose (23.4 mg) and the highest dose (75 mg) of atropine as used in the original paper. Recommendations were also compared with the dosing regimen from the World Health Organization (WHO). Thirteen of the original recommendations were updated and 15 additional references were added giving a convenience sample of 28. Sufficient information to calculate time to targeted dose was provided by 24 of these samples. Compared to 2004, current recommendations have greatly increased the speed of atropinization with 13/24 able to reach the mean and high atropine dose within 30 min compared to 1/36 in 2004. In 2004, there were 13 regimens where the maximum time to reach 75 mg was over 18 h, whereas now, there are 2. While only one recommendation called for doubling the dose for faster escalation in 2004, 15 of the 24 current works include dose doubling. In 2004, Eddleston et al. called for an evidence-based guideline for the treatment of OP poisoning that could be disseminated worldwide. Many current recommendations can adequately treat patients within 1 h. While the WHO recommendations remain slow to treat patients with OP poisoning, other authorities are close to a consensus on rapid atropinization.
Electronic supplementary material
The online version of this article (doi:10.1007/s13181-013-0324-9) contains supplementary material, which is available to authorized users.
Keywords: Atropine, Organophosphate Poisoning, Treatment Recommendations
Introduction
Organophosphate (OP) toxicity remains a major public health concern, primarily in the developing world, where widespread availability of agricultural pesticides may account for 200,000 deaths every year [1]. Although atropine is clearly the mainstay of initial therapy, strong consensus on the proper dosing regimen of atropine in OP-poisoned patients is lacking, likely due to the limited evidence on the optimal atropine dosing strategy. In 2004, Eddleston et al. assessed atropine dosing regimens from international authoritative texts [2]. The authors noted the mean atropine loading dose was 23.4 mg to treat cholinergic symptoms in a cohort of 22 Sri Lankan patients following intentional OP ingestions requiring intubation. They also noted the maximal initial dose, 75 mg, required by one patient. Referencing international authoritative texts, the authors found significant variation in recommended dosing regimens leading to huge variations in the time until the mean and maximal required atropine dose could be administered. In this analysis, the World Health Organization (WHO)’s recommendations resulted in the slowest rates of atropinization. The authors called on the medical community to evaluate the benefits of rapid atropine dosing and come to a consensus that could be easily followed by those treating OP-poisoned patients. Almost a decade after this important work was published, the sources that physicians are using have changed from large tomes to internet resources and medical applications accessed via smartphone. Our aim was to evaluate the current references with regard to initial atropine dosing recommendations to determine if the variability described by Eddleston et al. persists and to see how newer electronic resources compare to standard reference texts. Additionally, we aimed to compare these references to the WHO’s guidelines which may be the most accessible to those clinicians working in regions where OP poisoning is common.
Methods
Recommendations for atropine dosing in acute OP-poisoned patients were sought from updated and revised editions of the sources from Eddleston et al.’s original paper and additional resources that were not included in that study (see Supplementary Table for list of texts). Major texts of Internal and Emergency Medicine and Toxicology (Cecil [3], Tintinalli [4], Rosen [5], Goodman and Gilman [6], Casarett [7], Wexler [8]) were added to the source list as were medical study and pocket guides (Tarascon [9], Rivers [10], Wyatt [11], Stone [12]). Additionally, new electronic resources such as UpToDate [13], eMedicine [14], Lexicomp [15], Access Medicine [16], and Epocrates [17] were accessed for this analysis since these internet sources can be easily used at the bedside via physicians’ mobile devices or from a nearby desktop and have the potential to significantly impact medical care. Recommended dosing regimens for initial atropine administration in acute OP poisoning were recorded from each text.
Statistical Analysis
Dosing recommendations were applied to two hypothetical patients using the mean required loading dose, 23.4 mg, used for the Sri Lankan patients in Eddleston et al.’s original paper and to the highest utilized loading dose, 75 mg in their cohort. The time until adequate dosing for these two scenarios was then calculated for each text’s recommendation and these times were compared.
Results
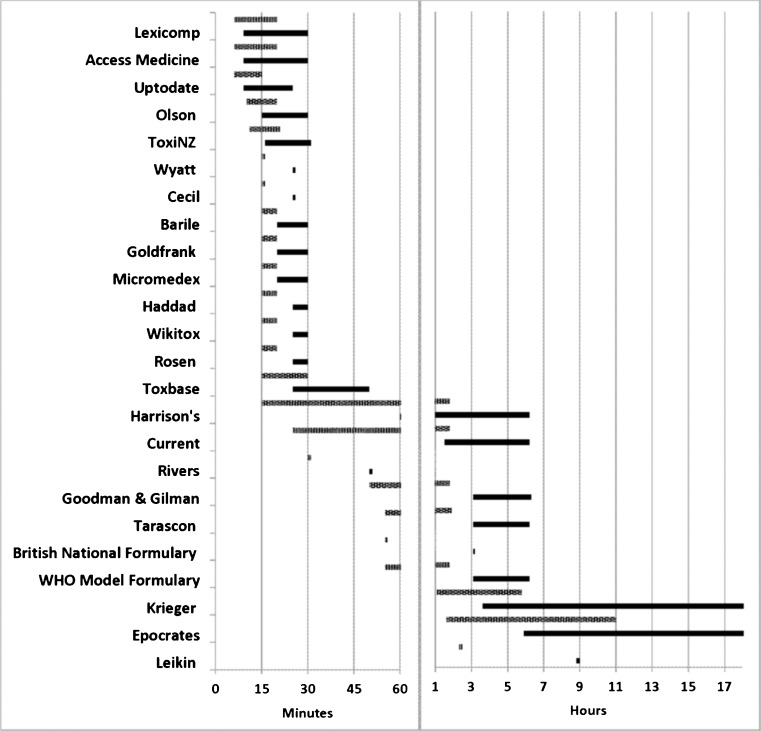
We were unable to locate six sources from Eddleston et al.’s article and 24 of the original sources had not been updated since 2004 (see Supplementary Table). Thirteen of the sources from Eddleston et al.’s publication had updated recommendations and 15 additional sources were added giving a convenience sample of 28 recommendations [3–30]. Of the reviewed references, Tintinalli [4], Casarett [7], and Wexler [8] were too vague to allow calculation of time until adequate atropine dose and eMedicine [14] gave a recommendation for dosing that would never reach the mean or maximum atropine doses for patients with severe OP poisoning. The remaining 24 sources provided enough information to make comparisons between times until administration of our targeted loading doses. Five recommendations (Cecil [3], Rivers [10], Wyatt [11], the British National Formulary [25], and Leikin [28]) provided an exact dosing regimen whereas all others provided a range. Figure 1 presents the range of time to administer the mean and highest doses of atropine based on each reference’s recommendation.
Fig. 1.
Time range for the administration of mean (23.5 mg; gray bars) and high (75 mg; black bars) atropine requirements for patients with severe OP poisoning based on dosing recommendations from each text. Requirements were based on 22 Sri Lankan patients presented in Eddleston et al.’s report. Times were curtailed after 18 h. Representation adapted from Eddleston, et al. [2]
In relation to the 2004 recommendations, current recommendations have greatly increased the speed of atropine dose escalation. In fact, if followed, 13/24 current recommendations attain the mean and high atropine requirement within 30 min even if the slowest dose escalation is employed, as compared with only 1/36 in 2004. Using the slowest dosing option in each current regimen, there are 12 that reach the mean atropine requirement of 23.4 mg in 1 h, while there were just three in 2004. In 2004, there were 13 regimens that took 18 h or more until the atropine dose was adequate to treat patients with a higher requirement of 75 mg, whereas now, there are only two. Of the recommendations in Eddleston et al.’s paper that were revised since 2004, 8 of 13 now include doubling the last dose for faster escalation. Dose doubling was recommended in 15/24 total current sources. This recommendation was present in only one source in 2004, notably, the only one that could provide an adequate dose for the mean and high doses within 1 hour.
In several sources, the maximum time that would be required to administer the mean atropine dose based on current recommendations and those reported in 2004 have changed significantly. ToxiNZ [20] has the largest improvement with a decrease of 11.2 h. WHO [26] and Haddad [22] had decreases of over 5 h. Wikitox [23] and Olson [19] suggest regimens that result in improvements of at least 3.5 h compared to 2004. The minimal time until administration of 23.4 mg is unchanged from prior in the current British National Formulary [25] regimen, but the maximal time to reach that same goal decreased by 55 min as the recommended dosing interval was changed from every 5–10 min, to simply every 5 min in the current iteration. Krieger [27] and Leikin [28] updated their recommendations to regimens that achieve the 23.4-mg goal dose more slowly, by 25 and 115 min, respectively. Notably, the WHO [26] recommendation, which was among the slowest in 2004, remains in the slowest 20 % in the current analysis.
Discussion
In areas where OP toxicity is a major health concern, delay to atropinization can be fatal due to central nervous system effects, bradycardia, circulatory collapse, and respiratory failure from bronchorrhea and bronchospasm. The aggressive treatment of patients with increasing doses of atropine at frequent intervals has the potential to significantly reduce the morbidity from OP poisoning. Eddleston et al.’s work in 2004 shed light on the significant differences in atropine dosing recommendations. Although there is little evidence proving that rapid atropinization is beneficial, animal data suggests early death after OP toxicity is, at least in part, centrally mediated. Mortality in mice is mitigated by pretreatment with anticholinergics that cross the blood brain barrier [31]. Additionally, there is observational evidence suggesting that rapid atropinization with dose doubling every 3 to 5 min is protective against mental status changes and decreases the case fatality rate of severe OP ingestions. Interestingly, in the cohort of patients that received titrated atropine rather than ad hoc administration, the patients were more critically ill and lower cumulative doses of atropine were given, causing fewer cases of atropine toxicity [32]. While the ideal randomized controlled trial evaluating the benefits of rapid atropinization in severely OP-poisoned patients has not been performed, atropine is able to prevent central symptoms and lessen bronchorrhea and bronchoconstriction characteristic of OP toxicity. It is reasonable to conclude that allowing these symptoms to continue for hours longer than necessary could pose significant risks for patient harm.
A consensus on the correct atropine dosing regimen does not exist. However there has been a shift in just a few years towards achieving atropinization much faster as many authoritative texts and new online sources suggest doubling the last dose when a patient requires further atropine treatment. Regimens that include dose doubling result in significant dose escalation and even allow a patient with a higher atropine requirement to be treated in less than 1 h. This is a significant improvement over the previously recommended regimens. Interestingly, Lexicomp [15], Access Medicine [16], and UpToDate [13], all online resources, suggest dosing schemes that allow for the fastest titration of atropine. While it is unreasonable to think that every hospital can easily access these sites, there is an undeniable trend toward greater reliance on internet resources for medical information and these sources can be utilized by a very broad audience. Like the other updated guidelines, the WHO [26] recommendation is an improvement on prior iterations, but still lags significantly behind many other sources. This is unfortunate as the WHO recommendation may be the most widely accessed throughout the regions of the world where OP toxicity remains an important concern.
Limitations: This review is a convenience sample of sources that the authors were able to access and included some of the most widely used texts and references. Limitations based on institutional subscriptions and availability prevented this analysis from being a complete review of published guidelines. It is also important to realize that while there is an assumption that rapid atropinization improves outcome, this has not been substantiated. The only “outcome” evaluated here is the time to atropinization rather than a clinical benefit.
Conclusion
In 2004, there was a call for clinical toxicology associations to work with the WHO to produce a simple and evidence-based guideline for the treatment of severe OP poisoning that could be disseminated worldwide. While the WHO recommendation lags in terms of the time to appropriate dosing for an average patient with severe OP poisoning and even more significantly, for those in the reference cohort with the highest atropine requirements, other authors have come closer to a consensus and their recommendations can treat severely poisoned patients within 1 h. We urge both further patient-centered research and efforts at consensus building pending the results of clinical trials.
Electronic supplementary material
A: The sources used in this analysis updated since 2004, B: those in Eddleston et al.’s paper that were not updated, C: those that were not located, and D: new sources accessed for atropine dosing recommendations (DOCX 25 kb).
Acknowledgments
Conflicts of Interest
This study received no funding. The authors report no conflicts of interest.
References
- 1.Eddleston M, Buckley NA, Eyer P, et al. Management of acute organophosphorus pesticide poisoning. Lancet. 2008;371(9612):597–607. doi: 10.1016/S0140-6736(07)61202-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eddleston M, Buckley NA, Checketts H, et al. Speed of initial atropinisation in significant organophosphorus pesticide poisoning—a systematic comparison of recommended regimens. J Toxicol Clin Toxicol. 2004;42(6):865–875. doi: 10.1081/CLT-200035223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ford MD. Acute poisoning. In: Goldman L, Schafer AI, editors. Goldman’s Cecil medicine. Philadelphia: Elsevier/Saunders; 2012. pp. 670–684. [Google Scholar]
- 4.Robey WC, III, Meggs WJ. Pesticides. In: Tintinalli JE, Stapczynski JS, editors. Tintinalli’s emergency medicine: a comprehensive study guide. New York: McGraw-Hill; 2011. [Google Scholar]
- 5.Aaron CK, Rhee JW, Dolcourt BA, et al. Pesticides. In: Marx JA, Hockberger RS, Walls RM, et al., editors. Rosen’s emergency medicine: concepts and clinical practice. Philadelphia: Mosby Elsevier; 2010. pp. 2052–2060. [Google Scholar]
- 6.Taylor P. Anticholinesterase Agents. In: Brunton LL, Blumenthal DK, Murri N, Hilal-Dandan R, Knollman BC, editors. Goodman & Gilman’s The pharmacological basis of therapeutics, online edition. New York: McGraw-Hill Medical; 2011. [Google Scholar]
- 7.Costa LG. Toxic Effects of Pesticides. In: Klaassen CD, editor. Casarett & Doull’s toxicology: the basic science of poisons. New York: McGraw-Hill Medical; 2013. [Google Scholar]
- 8.Ehrich M. Organophosphates. In: Wexler P, editor. Encyclopedia of toxicology. Oxford: Elsevier; 2005. [Google Scholar]
- 9.Rothrock SG. Tarascon’s adult emergency pocketbook. Sudbury, Massachusetts: Jones & Bartlett Learning; 2012. p. 176. [Google Scholar]
- 10.Rivers CS, Howell J, Barkin R. Preparing for the written board exam in emergency medicine. Milford: Emergency Medicine Educational Enterprises; 2006. Toxicologic emergencies; pp. 733–800. [Google Scholar]
- 11.Wyatt JP, Illingworth RN, Graham CA, Hogg K. Oxford handbook of emergency medicine. Oxford: Oxford University Press; 2012. Toxicology. [Google Scholar]
- 12.Stone CK, Humphries R. Current diagnosis and treatment emergency medicine. 7. New York: McGraw Hill; 2011. [Google Scholar]
- 13.Bird, S. Organophosphate and carbamate poisoning. In: Basow D, editor. UpToDate. Waltham, Massachusetts: UpToDate.com; 2012. Accessed August 2012
- 14.Katz KD. Organophosphate toxicity treatment and management. In: Pinsky MR, editor. eMedicine emergency medicine : an on-line medical reference. Medscape Reference; 2012. Accessed August 2012.
- 15.Lexicomp. Lexi-Drugs: Atropine. Lexicomp American Pharmacists Association Hudson, Ohio; 2012. Accessed August 2012.
- 16.Drug monographs: Atropine. Access Emergency Medicine; 2012. Available from: www.accessemergencymedicine.com. Accessed August 2012.
- 17.Epocrates. Atropine. Epocrates online. Available from: https://online.epocrates.com. Accessed August 2012.
- 18.Barile FA. Clinical toxicology: principles and mechanisms. 2. London: Informa HealthCare; 2010. [Google Scholar]
- 19.Vohra R. Organophosphorous and carbamate insecticides. In: Olson K, editor. Poisoning and drug overdose. USA: McGraw-Hill Companies; 2012. [Google Scholar]
- 20.Organophosphorus poisoning. In: ToxiNZ; 2012. Available from: toxinz.co.nz. Accessed August 2012.
- 21.Howland MA. Antidotes in depth: atropine. In: Nelson LS, Lewin NA, Howland MA, Hoffman RS, Goldfrank LR, Flomenbaum NE, editors. Goldfrank’s toxicologic emergencies. New York: McGraw-Hill; 2011. pp. 1473–1476. [Google Scholar]
- 22.Aaron CK. Organophosphates and carbamates. In: Shannon MW, Borron SW, Burns MJ, editors. Haddad and Winchester’s clinical management of poisoning and drug overdose. Philadelphia: Saunders/Elsevier; 2007. pp. 1171–1184. [Google Scholar]
- 23.Wiki Tox. 2.2.7.4.5 organophosphates. Wiki Tox: open source clinical toxicology curriculum; 2012. Available from http://curriculum.toxicology.wikispaces.net/2.2.7.4.5+Organophosphates Accessed August 2012.
- 24.Hurst CG, Newmark J, Romano JA. Chemical terrorism. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson L, Loscalzo J, editors. Harrison’s Online. Access Medicine; 2012
- 25.Joint Formulary Committee (2011) British National Formulary. 62nd ed. London: British Medical Association and Royal Pharmaceutical Society of Great Britain
- 26.Stuart MC, Kouimtzi M, Hill SR, (eds) (2008) Antidotes and other substances used in poisonings. In: WHO model formulary 2008. World Health Organization, Geneva, p. 55–66
- 27.Lotti M. Clinical toxicology of anticholinesterase agents in humans. In: Krieger RI, editor. Hayes’ handbook of pesticide toxicology. London: Elsevier; 2010. pp. 1543–1589. [Google Scholar]
- 28.Leikin JB, Paloucek FP (eds) (2008) Antidotes and drugs used in toxicology. In: Poisoning and toxicology handbook. Informa Healthcare, New York, pp. 965–1013
- 29.Poisindex System. Organophosphorous poisoning. Thomson Reuters (Healthcare) Inc. Greenwood Village, Colorado. Accessed June 2013.
- 30.National Poisons Information Service UK. Organophosphorus insecticides. TOXBASE. Accessed June 2013.
- 31.Bird SB, Gaspari RJ, Dickson EW. Early death due to severe organophosphate poisoning is a centrally mediated process. Acad Emerg Med. 2003;10:295–298. doi: 10.1111/j.1553-2712.2003.tb01338.x. [DOI] [PubMed] [Google Scholar]
- 32.Perera PM, Shahmy S, Gawarammana I, Dawson AH. Comparison of two commonly practiced atropinization regimens in acute organophosphorus and carbamate poisoning, doubling doses vs. ad hoc: a prospective observational study. Hum Exp Toxicol. 2008;27:513–518. doi: 10.1177/0960327108091861. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A: The sources used in this analysis updated since 2004, B: those in Eddleston et al.’s paper that were not updated, C: those that were not located, and D: new sources accessed for atropine dosing recommendations (DOCX 25 kb).