Abstract
Pigmented Villonodular Synovitis (PVNS) is a relatively rare, benign proliferation lesion of the synovium of large joints. The etiology is varied and unclear. We had report a 79-year-old woman had PVNS after 14 years right hip arthroplasty with metal prosthesis. Here we report another 4 patients had PVNS after arthroplasty. The second one had PVNS in the 2th year after hip arthroplasty with bone cement prosthesis. The specimen was brown and like usual PVNS in tissue. The third case had PVNS in the 8th after arthroplasty with human bone prosthesis because of the recurrence of PVNS. The proliferated synovium became black from brown. There was brown and many groups black pigment in the tissue. The fourth one had PVNS in the 4th year after knee arthroplasty with polyethylene prosthesis. The specimen was yellow. There was no pigment in the tissue but multinucleated giant cells with unstained foreign body. The fifth patient had PVNS in the 10th month after the left hip arthroplasty with metal prosthesis. The macroscopy was yellow. There were hemosiderin particles in the tissue but black metal particles. This indicates that arthroplasty with prosthesis could cause some new disease or PVNS had new etiology with different pathological show.
Keywords: Pigmented villonodular synovitis, arthroplasty, etiology
Introduction
Pigmented Villonodular Synovitis (PVNS) is a relatively rare, benign proliferation lesion of the synovium with villous or nodular changes in the large joints. The etiology is unclear. There were a few cases include our report have PVNS after arthroplasty with prosthesis in the literature [1-6]. The aim of our paper was to describe another 4 PVNS cases after arthroplasty with prosthesis.
Case reports
The case 1 we had reported [3] was a 79-year-old woman. 14 years ago, she had right hip arthroplasty with metal prosthesis because of femoral head necrosis. The patient had the second surgery because of prosthesis loosen. During the second operation, the surgeons found the synovium proliferated and filled with the hip articular cavity with black color which not presented in the first surgery. Histological, the surface of the specimen was black. There were black particles in the surface synoviocytes while without pigment under the surface tissue (Figure 1). The patient had no adjunctive therapy after the second surgery. She was followed up 42 months and did not recur.
Figure 1.
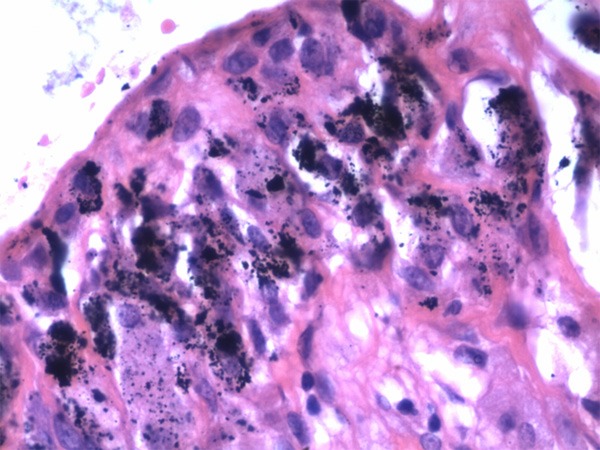
There was black pigmentation in the synoviocyte cytoplasm. Below the surface, there were foamy cells and multinucleated giant cells without black pigmentation or hemosiderin (hematoxylin and eosin; original magnification ×40).
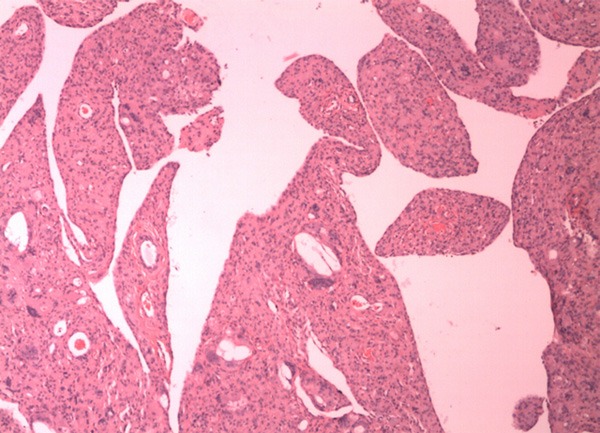
The case 2 was 72-year-old woman. She had total right hip arthroplasty with bone cement because of the femoral neck fracture. There was no complication after the operation. 2 years later, she presented the right hip joint pain without swelling which had no relationship with the action. She had no history of trauma. The physical examination of her right hip joint was normal. There was dark red fluid in the joint by arthrocentesis. The X-ray showed that the prosthesis was loose. The surgeon decided to have the second surgery. During the second operation, there was proliferated synovium filled with the knee articular cavity with brown color while there was no proliferated synovium during the first operation. The proliferated synovium was cut out. The specimen with was brown covered with nodules and both long and short papillae. There was brown pigment in the tissue in the cytoplasm of the surface and the undersurface (Figure 2) like the common PVNS cases. There was no bone cement in the tissue. The patient had no adjunctive therapy after the second surgery and been followed up 28 months and did not recur.
Figure 2.
There was hemosiderin in the synoviocyte cytoplasm of the surface and below the surface (hematoxylin and eosin; original magnification ×4).
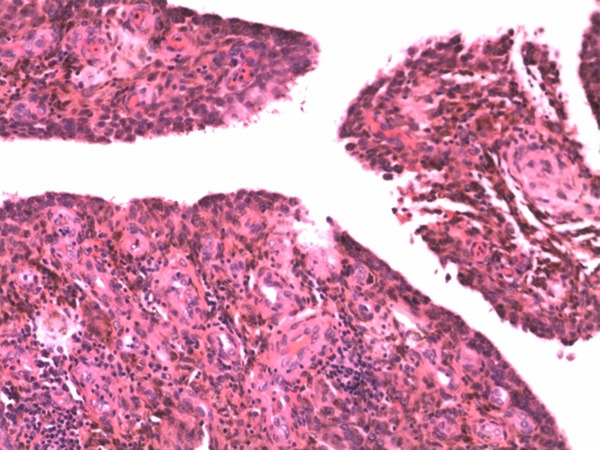
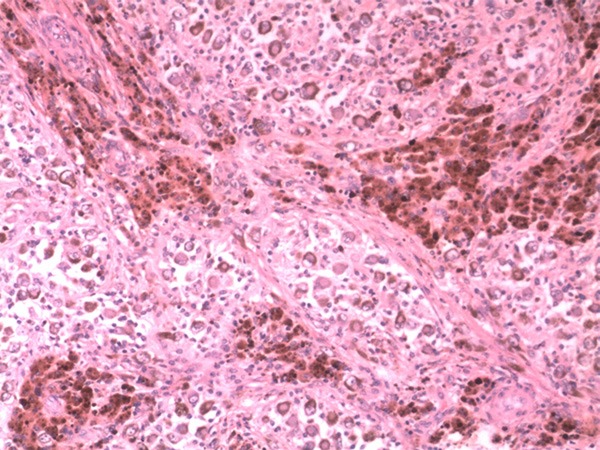
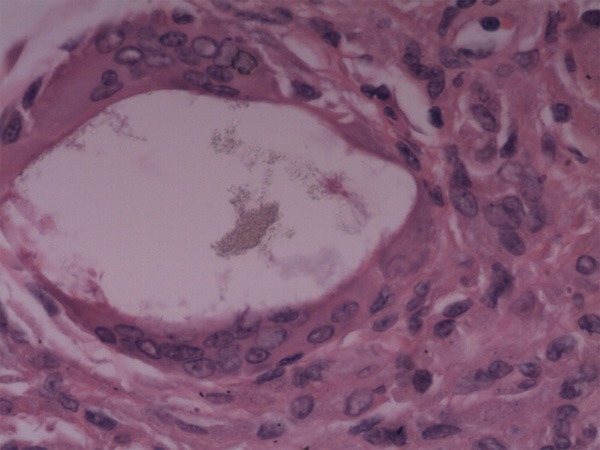
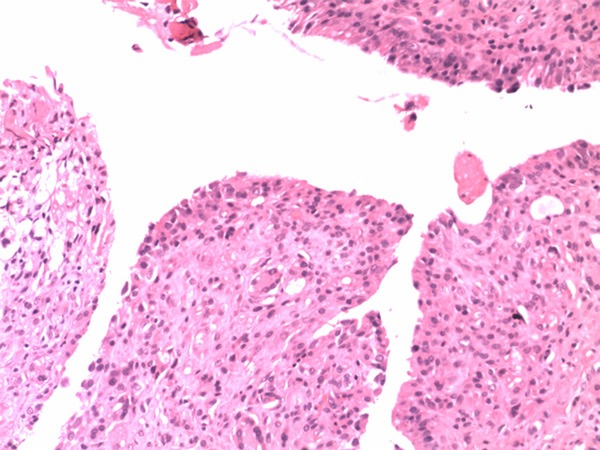
The case 3 was 22-year-old woman. She had the right hip joint pain without inducement for 4 years. The MRI diagnosis was the synovium proliferation. She had the first surgery and the pathological diagnosis was PVNS. There was no complication after the operation. The right hip joint pain was disappeared. In the 8th year after the first surgery, the right hip joint pain appeared again. The MRI diagnosis was the PVNS recurred. She had the second surgery when she was 30-year-old. The hyperplastic synovium was resected, and at the same time, she had the total right hip arthroplasty with human bone prosthesis. The specimen of the secondary like the first one was as the usual PVNS. In the 8th year after the second surgery, she presented that the right hip joint pain again. The X-ray showed that the synovium proliferation around the prosthesis. She had the third surgery that the proliferated synovium was resected. The specimen of third one was black and brown while brown of the first and the second before arthroplasty. Microscopically, it was the same as the usual PVNS except the brown and many groups black pigment in the tissue (Figures 3 and 4). The patient had radiotherapy after the third surgery and did not recur with the 49 months following-up.
Figure 3.
There was brown and many groups black pigmentation in some cells while few brown pigmentation in other cells (hematoxylin and eosin; original magnification ×4).
Figure 4.
There was some round black beside brown pigmentation in the mononuclear cell and multinuclear cell cytoplasm (hematoxylin and eosin; original magnification ×40).
The case 4 was 51-year-old woman. She had pain of the bilateral keen joints for more than 10 years. Walking made the pain more seriously. The X-ray and MRI diagnosis was osteoarthritis of the both keen joints. She had been injected steroid hormones in the both knee joints many times and had little effect. There was dark red fluid in the both joints. She had had bilateral keens arthroplasty with polyethylene prosthesis. There was no complication after the operation. 4 years later, the patient sprained the left knee uncarefully. In the following time, she felled that the action of the left knee was limited. The X-ray showed that the left prosthesis loosen. So she had the second surgery of the left knee. The surgeon found that the proliferated synovium with yellow color (Figure 5) filled with the left knee joint cave. Microscopically, there was no pigment in the tissue (Figure 6) but multinucleated giant cells with unstained foreign body (Figure 7). The pathological diagnosis was PVNS. The patient had no adjunctive therapy after the second surgery and been followed up 37 months and did not recur.
Figure 5.

The proliferated synovium was papillary and nodular, with a yellow color.
Figure 6.
There was no pigment in the tissue but multinucleated giant cells with unstained foreign body (hematoxylin and eosin; original magnification ×4).
Figure 7.
There were small particles as foreign body in the empty spaces in the multinucleated giant cells (hematoxylin and eosin; original magnification ×40).
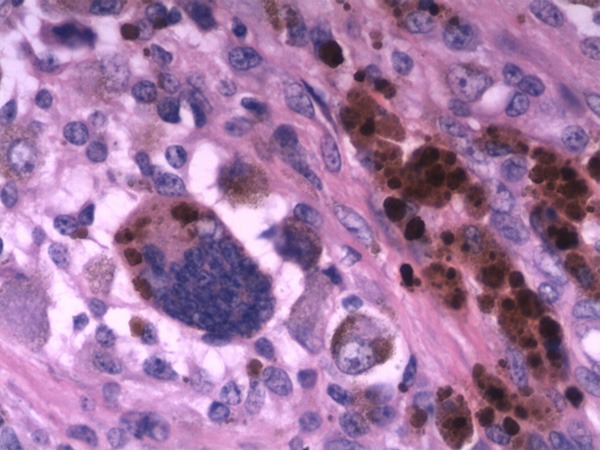
The case 5 was 64-year-old woman. She had total left hip arthroplasty with metal prosthesis because of the femoral neck fracture caused felled down uncarefully. There was no complication after the operation. 10 months later, she presented the left hip joint was uncomfortable especially walking. The X-ray showed that there was soft tissue around the metal prosthesis. So she had the second surgery. The surgeon found some localized proliferated synovium with yellow color in the joint cave. Microscopically, there were hemosiderin particles in the tissue but black metal particles. The pathological diagnosis was PVNS (Figure 8). The patient had radiotherapy after the second surgery and been followed up 5 months and did not recur.
Figure 8.
There was no pigment or hemosiderin in the synoviocyte cytoplasm of the surface or the foamy cells and multinucleated giant cells below the surface (hematoxylin and eosin; original magnification ×4).
Discussion
Pigmented villonodular synovitis was first reported in 1941. It is known to be a benign proliferative disorder of the synovium. Histologically, PVNS is characterized by the presence of hemosiderin deposition, lipid-laden macrophages. Till now, there was no a consensus about the etiology of PVNS. The debate was that PVNS is inflammatory or neoplasm in origin. Trauma and other associated reason caused hemorrhage maybe was one of the etiologies [7]. In our study, there was no one had a clearly history of trauma before the diagnosis of PVNS but arthroplasty. There were 2 cases had dark red fluid in the arthroplastied joints. These maybe could cause synovium proliferation in the involved joints directly or indirectly.
There were some non-PVNS disease has been described after arthroplasty which been thought to be a response to the component of the prosthesis [8,9]. There were reports that PVNS recurred after arthroplasty surgery [10,11] like the case 3. Our case 3 had specimen change in color after arthroplasty. Histologically, there were some black pigment particles in the cytoplasm after arthroplasty. Moreover, there were few sporadic PVNS reports after arthroplasty in the patients who had no this disease at primary surgery [1-6].
To review the literature (Table 1), the arthroplasty-PVNS cases were all the aged. The anatomic sites were all the knees while the hip joints in our cases. The form of arthroplasty-PVNS was diffuse mostly except two localized cases include our case [2]. In the literature, the prosthesis most was cement except the one not mentioned. In our cases, there were cement, metal, human bone and polyethylene. The time occur PVNS after arthroplasty was between 10 months to 168 months. The shortest time and the longest time were all our cases who all had metal prosthesis but with different color and microscopy show.
Table 1.
Clinical Characteristics of 10 patients of PVNS after arthroplasty
| No | Gender | age | Anatomic site | Form | PVNS | Materials | Time occur PVNS (m) | Color | Follow-up (m) | Recur |
|---|---|---|---|---|---|---|---|---|---|---|
| Ballard WT [1] | F | 67 | RK | D | N | not mentioned | 113 | brownish-yellow | 6 | N |
| Bunting D [2] | F | 71 | RK | L | N | cement | 22 | heavy pigmentation | N | ? |
| Mohanlal P [4] | M | 69 | ?K | D | N | not mentioned | 48 | hemosiderin colored | N | ? |
| Oni JK [5] | M | 73 | LK | D | N | cement | 18 | hemosiderin colored | 6 | N |
| Onodera T [6] | F | 61 | RK | D | N | cement | 36 | hemosiderin colored | 12 | N |
| Case 1 [3] | F | 79 | RH | D | N | metal | 168 | black | 37 | N |
| Case 2 | F | 74 | RH | D | N | cement | 23 | brown | 21 | N |
| Case 3 | F | 42 | RH | D | Y | human bone | 34 | black | 39 | N |
| Case 4 | F | 54 | LK | D | N | polyethylene | 47 | yellow | 13 | N |
| Case 5 | F | 64 | LH | L | N | metal | 10 | yellow | 6 | N |
PVNS means the patient had PVNS before arthroplasty. Time occur PVNS means the time occur PVNS after arthroplasty. RH means right hip. RK means right knee. LK means left knee. LH means hip. D means diffuse. L means Localized. Y means yes. N means no.
In practice, there was a series biological reaction after arthroplasty. The appearances of various in the tissues viewed by conventional light microscopy have been described by Revell [12]. Although we couldn’t detect the black pigment and the foreign-body and the particles, we believed that it was the component of the prosthesis such as polyethylene (PE), metal or cement wear. Perhaps all of these prosthesis components served as inflammatory factors causing the proliferation of synoviocytes into PVNS between the time after arthroplasty and before PVNS [1].
However, trauma from the prosthesis or the surgery but the material of the prosthesis maybe was the etiology. The fifth one had PVNS after arthroplasty in the 10 months. There were no particles of the prosthesis in the tissue. Maybe the synovial tissue in the joint proliferation spontaneously after the surgery but the prostheses cause during the short 10 months. It indicated that the implantation of prostheses may be the etiopathogenesis of disease or may cause new disease, just as Bunting et al suspected [2].
While MRI was useful for the diagnosis of PVNS, it was not useful sometime for the patients who had arthroplasty because of the prosthesis. So the PVNS primary diagnosis was made during the operation and the final diagnosis was made by pathology for these arthroplasty patients usually. That is to say it is difficult in macroscopy to distinguish PVNS with rheumatoid arthritis, degenerative osteoarthropathy, synovial hemangioma et al. It needs pathology to diagnose accurately.
Macroscopically, the specimen was pieces. The surface was brown or black which concerned with the material of the prosthesis covered with nodules and both long and short papillae. Histologically, the surface of the tissue was composed of synoviocytes with black or hemosiderin particles in the cytoplasm or multinucleated giant cells with foreign body in the different prosthesis which was different with the usual PVNS.
Surgery is usually considered the mainstay of therapy, although no standard therapy has been defined to date for PVNS. Moreover, radiotherapy is recommended as an adjunct to total synovectomy for preventing recurrences in the presence of residual or as second-stage treatment in recurrent cases. This may be useful for the treatment of PVNS after arthroplasty too.
In conclusion, the etiology of PVNS was variety. Arthroplasty maybe was one of the etiologies that had not been mentioned till recently. The prosthesis components or the trauma from the prosthesis or the surgery maybe were all the etiologies. The PVNS after arthroplasty had special figures. Macroscopically, it was the same as the usual PVNS beside the color. Microscopically, there were black or hemosiderin particles in the synoviocytes cytoplasm, or multinucleated giant cells with foreign body below the surface which concerned with the material of the prosthesis. Complete surgical removal the proliferated synovectomy may be the effective treatment.
Disclosure of conflict of interest
None.
References
- 1.Ballard WT, Clark CR, Callaghan JJ. Recurrent spontaneous hemarthrosis nine years after a total knee arthroplasty. A presentation with pigmented villonodular synovitis. J Bone Joint Surg Am. 1993;75:764–7. doi: 10.2106/00004623-199305000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Bunting D, Kampa R, Pattison R. An unusual case of pigmented villonodular synovitis after total knee arthroplasty. J Arthroplasty. 2007;22:1229–31. doi: 10.1016/j.arth.2006.11.022. [DOI] [PubMed] [Google Scholar]
- 3.Ma X, Xia C, Wang L, Zhao L, Liu H, He J. An unusual case of pigmented villonodular synovitis 14 years after total hip arthroplasty. J Arthroplasty. 2011;26:339, e56. doi: 10.1016/j.arth.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 4.Mohanlal P, Pillai D, Jain S. A rare case of pigmented villonodular synovitis after unicompartmental knee replacement: a case report. Cases J. 2009;2:9076. doi: 10.1186/1757-1626-2-9076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oni JK, Cavallo RJ. A Rare Case of Diffuse Pigmented Villonodular Synovitis After Total Knee Arthroplasty. J Arthroplasty. 2011;26:978, e9978. doi: 10.1016/j.arth.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 6.Onodera T, Tanji H, Majima T, Kamishima T, Minami A. An unusual case of pigmented villonodular synovitis after unicompartmental knee arthroplasty. IJCRI. 2012;3:9–12. [Google Scholar]
- 7.Tyler WK, Vidal AF, Williams RJ, Healey JH. Pigmented villonodular synovitis. J Am Acad Orthop Surg. 2006;14:376. doi: 10.5435/00124635-200606000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Karl LA, Sundstrom WR. Prosthesis-induced synovitis simulating villonodular synovitis. Wis Med J. 1991;90:165. [PubMed] [Google Scholar]
- 9.Kaufman RL, Tong I, Beardmore TD. Prosthetic synovitis: clinical and histologic characteristics. J Rheumatol. 1985;12:1066–74. [PubMed] [Google Scholar]
- 10.Lawrence T, Moskal JT, Diduch DR. Analysis of routine histological evaluation of tissues removed during primary hip and knee arthroplasty. J Bone Joint Surg Am. 1999;81:926. doi: 10.2106/00004623-199907000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Hamlin BR, Duffy GP, Trousdale RT, Morrey BF. Total knee arthroplasty in patients who have pigmented villonodular synovitis. J Bone Joint Surg Am. 1998;80:76. doi: 10.2106/00004623-199801000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Revell PA. Tissue reactions to joint prostheses and the products of wear and corrosion. Curr Top Pathol. 1982;71:73–101. doi: 10.1007/978-3-642-68382-4_3. [DOI] [PubMed] [Google Scholar]


