Abstract
Autologous skull flaps were frequently used in craniotomy, and after craniotomy, autologous skull flaps need to be replanted in situ at most of the time, and complications such as infection and resorption may occur. Ultimately, resorption may result in dislocation of the autologous skull flaps. Here we describe a case of completely resorption of autologous skull flap shortly after orthotopic transplantation which required an extra cranioplasty and potential causes were discussed. Improper processing procedure such as peeling periosteum excessively before replantation, and postoperative subdural effusion and the use of bone wax were considered to be responsible for the rapid complete resorption of the skull flap.
Keywords: Craniotomy, neurosurgery
Introduction
In clinical practice, autologous skull flaps were frequently used in craniotomy when the situation permitted and the skull would recover at most of the time except those with complications such as infection and dislocation of the skull flaps. Resorption of autologous skull flaps that was orthotopically transplanted by two-stage operation was widely reported no matter how it was preserved before replantation. However, completely resorption of autologous skull flaps after first operation has not been reported before. Here, we reported a case of completely resorption of autologous skull flaps shortly after orthotopic transplantation, which required an extra cranioplasty.
Case present
A 38-year-old man visited the Department of neurosurgery with the chief complaint of headache for about 4 hours. The medical history and family history of the patient were unremarkable, and he denied any history of neither high blood pressure nor diabetes mellitus. Head CT showed intracerebral hematoma in the left temporal lobe of about 49.7×26.7×30.0 mm in size (Figure 1A). Cere-bral angiography indicated aneurysm in the left anterior cerebral artery. Craniotomy with bone flap was implemented to remove the hematoma and the aneurysm was clipped with clamp. Bone wax was applied to the edge of the bone window to stop bleeding and the bone flap was re-implanted in situ right after surgery with skull locks (Figure 1B). Seven days after operation subscalp effusion within the operation area was found and puncture were performed twice to extract the effusion the next three days, and after each puncture his head was wrapped with pressure. After one week he was discharged and two months later he complained of headache again. Head CT scan showed that the bone flap shrank. No treatment was taken except some neurotrophic drugs, and he was advised to follow-up the next year. Then two month later, his head CT showed that most of the bone flap was absorbed with only several pieces of small flaps left just like little islands. In addition, the skull locks were drifting (Figure 1C). Cranioplasty was implemented with titanium mesh and the skull locks were removed. He did not complain any discomfort and his head CT did not show any resorption of the skull or dislocation of the titanium mesh in one year follow-up (Figure 1D).
Figure 1.
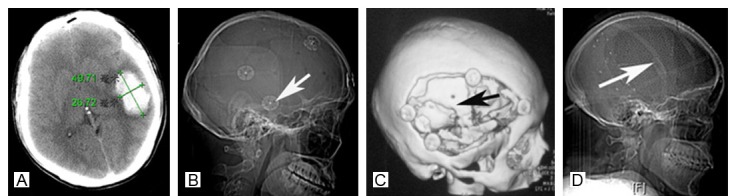
Head CT showed intracerebral hematoma in the left temporal lobe (A) and the bone flap was re-implanted in situ with skull locks (white arrow) (B). The bone flap was absorbed with only several pieces of small flaps left (C) five months after the first operation and cranioplasty was implemented with titanium mesh (white arrow) (D).
Discussion
Every craniotomy requires immediate replacement of a fresh autograft of skull or in the presence of cerebral swelling, delayed reimplantation of preserved autogenous skull or other substitutes in order to protect the brain and restore skull conformity. In clinical practice, autologous skull flap is frequently used in craniotomy [1,2], and the flap is orthotopically transplanted if the situation is permitted. Compli-cations such as infection and resorption may occur especially in those two-stage operations [3]. No matter how the autologous skull flap was preserved before replantation, the flap died when the periosteum was peeling from it. Resorption of the autologous skull flap that was orthotopic transplantation by two-stage operation is widely reported [4,5]. To the best of our knowledge, resorption of autologous skull flap shortly after orthotopic transplantation, requiring an extra cranioplasty was less reported [6,7]. In this case, the bone flap was nearly absorbed within only five months. The craniotomy lasted four hours and the bone flap was wrapped with wet saline gauze during the operation and no other handling was made before reimplantation.
Because of less report of such cases little is known on the pathophysiology of this phenomenon. A possible explanation could be Gorham syndrome which characterized by progressive osteolysis. As there is no evidence of osteolysis in any other part of the body before or after the operation, and the skull did not show any resorption after cranioplasty, we can rule out this diagnosis.
Other explanations could be the use of bone wax during the operation and the subscalp effusion after operation. As we know once the bone flap was taken out from the skull and periosteum was peeled from it the bone is dead actually. It’s recovery needs blood supply that comes from surrounding periosteum and endocranium. Bone wax is applied to the edge of bone window to stop bleeding; this also separates the bone flap from the skull. If subscalp effusion occurs in the early stage of the recovery, the bone flap is steeping in water (cerebrospinal fluid at most of the time) and cannot gain blood supply, it might be absorbed gradually.
Although it is not yet possible to give a final explanation of the phenomenon, this complication has always be considered as a possible event in this kind of cranial vault implant and the patient should therefore be informed about such an eventuality, and doctors should keep it in mind that subscalp effusion must be avoid after operation in those patients.
Disclosure of conflict of interest
None.
References
- 1.Hunter PD, Pelofsky S. Classification of autogenous skull grafts in cranial reconstruction. J Craniomaxillofac Trauma. 1995;4:8–15. [PubMed] [Google Scholar]
- 2.Movassaghi K, Ver-Halen J, Ganchi P, Amin-Hanjani S, Mesa J, Yaremchuk MJ. Cranioplasty with subcutaneously preserved autologous bone grafts. Plast Reconstr Surg. 2006;117:202–206. doi: 10.1097/01.prs.0000187152.48402.17. [DOI] [PubMed] [Google Scholar]
- 3.Gooch MR, Gin GE, Kenning TJ, German JW. Complications of cranioplasty following decompressive craniectomy: analysis of 62 cases. Neurosurg Focus. 2009;26:E9. doi: 10.3171/2009.3.FOCUS0962. [DOI] [PubMed] [Google Scholar]
- 4.Chang V, Hartzfeld P, Langlois M, Mahmood A, Seyfried D. Outcomes of cranial repair after craniectomy. J Neurosurg. 2010;5:1120–1124. doi: 10.3171/2009.6.JNS09133. [DOI] [PubMed] [Google Scholar]
- 5.Shoakazemi A, Flannery T, McConnell RS. Long-term outcome of subcutaneously preserved autologous cranioplasty. Neurosurgery. 2009;65:505–510. doi: 10.1227/01.NEU.0000350870.69891.86. [DOI] [PubMed] [Google Scholar]
- 6.Schneider T. [Subtotal bone resorption following reimplantation of a bone flap. 2 case examples] . Neurochirurgia. 1987;30:19–20. doi: 10.1055/s-2008-1053649. [DOI] [PubMed] [Google Scholar]
- 7.Prolo DJ, Burres KP, McLaughlin WT, Christensen AH. Autogenous skull cranioplasty: fresh and preserved (frozen), with consideration of the cellular response. Neurosurgery. 1979;4:18–29. doi: 10.1227/00006123-197901000-00005. [DOI] [PubMed] [Google Scholar]


