Abstract
This study involved evaluation of the shortterm impact of the RHANI Wives HIV intervention among wives at risk for HIV from husbands in Mumbai, India. A two-armed cluster RCT was conducted with 220 women surveyed on marital sex at baseline and 4–5 month followup. RHANI Wives was a multisession intervention focused on safer sex, marital communication, gender inequities and violence; control participants received basic HIV prevention education. Generalized linear mixed models were conducted to assess program impact, with cluster as a random effect and with time, treatment group, and the time by treatment interaction as fixed effects. A significant time by treatment effect on proportion of unprotected sex with husband (p = 0.01) was observed, and the rate of unprotected sex for intervention participants was lower than that of control participants at follow-up (RR = 0.83, 95 % CI = 0.75, 0.93). RHANI Wives is a promising model for women at risk for HIV from husbands.
Keywords: HIV intervention, Evaluation research, Women, India, Alcohol, Intimate partner violence
Introduction
Approximately 2.4 million people in India (0.3 % of the population) are infected with HIV; the vast majority of these (88 %) are infected via heterosexual sex [1, 2]. Commercial sex work drives the Indian epidemic, with transmission often occurring between female sex workers (FSWs) and male clients, and from male clients to their wives [1–3]. Recent national declines in the epidemic have been attributed to targeted intervention campaigns directed at FSWs and their male clients [1–3]. However, this approach neglects wives, and a lack of emphasis on wives at risk may explain the increase in proportion of HIV infected women in the country, from 25 % in 2001 to 39 % in 2009 [1, 4, 5]. The small proportion of women engaged in commercial sex work in the country suggests that this increase is not likely due to a rapid rise in HIV infections among FSWs [1, 6]. Marriage is now the primary risk factor for HIV among women in India, and almost 90 % of new HIV infections among women do not involve commercial sex and mostly occur in the context of marriage [1, 6–8]. Interventions focused on HIV prevention among wives at risk for contracting HIV from their husbands are needed in India, particularly in high epidemic areas of the country, such as Mumbai [1, 7].
Among married women, primary risk factors for HIV include geography and husband-related risks [1, 7]. More than one in six cases of HIV in India occurs in the state of Maharashtra, and most of these occur in the metropolitan area of Mumbai, the populous financial center of India [1, 7]. Antenatal care data from Mumbai indicate that women in this city are more than twice as likely to be infected with HIV, relative to women in India as a whole [1]. Mumbai has numerous commercial sex areas and large numbers of migrant males who visit FSWs, become infected with HIV and transmit their infection to their wives, as well as to other FSWs [7, 9, 10]. Women are often unaware of being exposed to this risk from their husbands. However, these wives are more commonly aware of their husbands’ risky alcohol use and spousal violence perpetration; factors that are associated with HIV among women and which appear to be markers for husbands’ involvement with FSWs [8– 12]. Such husband-related risk factors in the context of communities with high rates of HIV offer a means through which to identify wives at risk for HIV for intervention, since behavioral risk of wives appears to be uncommon in India and a less reliable means of identifying women at risk for HIV [8–12]. However, identification of women through such markers can impede options for couple intervention, as husbands may be defensive through this recruitment approach. Hence, women-focused interventions are needed in India for wives residing in HIV epidemic-affected locations such as Mumbai and reporting husbands’ risky alcohol use or spousal violence.
In the US and South Africa, women-focused interventions emphasizing HIV risk in relationships and related gender and sexual communication dynamics have resulted in significant impact on condom use in steady and marital relationships [13–15]. For example, the HIV Intensive Program (HIV-IP) intervention conducted with Latinas in the United States demonstrated increased safer sex communication and condom use with primary male partners via a multisession group intervention [14]. HIV-IP provided a safe and supportive environment for women to increase their knowledge and skills related to these health outcomes and increase their safer sex knowledge, skills and empowerment. Although HIV prevention among wives at risk from husbands in India is clearly needed, few models and little data exist on such interventions for this country [1].
This study evaluates the Raising HIV Awareness in Non-HIV-Infected Indian Wives (RHANI Wives) intervention, a multi-session HIV prevention intervention focused on sexual communication and empowerment with wives at risk for HIV in Mumbai, India. RHANI Wives was adapted from the HIV-IP intervention, described above, as HIV-IP study participants were comparable in risk profile to at risk Indian wives in terms of their vulnerability to HIV being from primary male partners engaging in risky substance use, partner violence perpetration, and concurrent sexual relationships [14]. The current evaluation study assessed both short-term impact of this intervention on unprotected sex, as well as its feasibility and acceptability as indicated by program participation and retention rates and participant response to program.
Methods
Between July 2010 and June 2011, 220 eligible women were enrolled into this study from slum areas in the Bhandup suburb of Mumbai, an area in which commercial sex work occurs and HIV/STI rates are higher than the city as a whole [16, 17]. Women were invited to participate in the two-armed cluster randomized controlled trial of RHANI Wives. [Treatment arms are outlined in detail in the next section.] Geographic clusters were created for randomization by the research team prior to study implementation via the mapping of the study area by geographic boundaries (e.g., a hill, street) and population density, such that each geographic cluster included approximately 300 households. This approach resulted in 22 clusters within our study area of focus, in three adjacent slum communities; 13 of these clusters were selected for study inclusion based on indications of a greater number of alcohol venues within them. One cluster was utilized for piloting but retained in the study, as no changes were made to the program; the remaining 12 clusters were randomized to the intervention or control conditions.
Eligibility Criteria
Based on surveillance data indicating greater risk for HIV among wives reporting husband’s heavy or frequent alcohol use[9–11] or lifetime spousal abuse perpetration against the participant [8], eligibility included the following criteria: (1) 18–40 years of age, (2) fluency in Hindi or Marathi, (3) residence with husband in the area of study for a period of 2 months or greater, (4) reports that husband engaged in either heavy drinking (past 30 day drunken behavior, or 3 drinking days in past 7 days) or lifetime physical or sexual spousal violence perpetration, and (5) no plans to relocate from the area in the next year.
Preparation of Study Site
Due to the sensitive topics of study as well as the vulnerable population we were reaching for inclusion, we prepared study clusters from both study arms via outreach to local leaders and street plays to build awareness of the research team and study, issues of alcohol and spousal violence in the community, and the planned outreach to wives. The street theatre highlighted how husbands’ heavy alcohol use can lead to financial strain, mistreatment and abuse of wives and children, and husbands’ extramarital sex, compromising the health of the family. These efforts were made prior to recruitment and baseline data collection for each cluster. While this preparation could affect participant responses on the survey, we would expect no difference between treatment groups based on this preparation effort, as these efforts were conducted equivalently for both treatment arms.
Recruitment and Screening
Within selected clusters, trained female research staff approached all households to determine if a married woman that met age criteria was available. Research staff members were female and all held Masters’ degrees in either psychology or social work. All staff members were trained on issues domestic violence and safety, HIV, and the research protocol and data collection procedures.
If an age-eligible married woman was home, the research staff member explained that a women’s health focused research project for women in this community was being conducted and asked about her willingness to participate in a survey. If the woman indicated interest, a private space was identified within the house, or nearby, for the eligibility assessment and consent process. Due to the low literacy rates of our population of focus, and the sensitivity of the eligibility criteria, consent forms were read in full to all participants, and written informed consent was obtained prior to screening for eligibility. The consent form outlined that the purpose of the project was to evaluate an HIV intervention for women who are contending with husbands who engage in recent heavy alcohol use and/or have been physically or sexually abusive in the marital relationship. The consent form was clear that participants would either receive the multisession intervention or a brief one session intervention, and participants were informed after consent whether they were in the intervention or control condition. Thus, neither participants nor research staff members were blinded to treatment condition.
Subsequent to acquisition of written informed consent, the 20 min eligibility screener was conducted. The screener included a variety of questions on health care acquisition, fertility and parity, and family tobacco use, as well as eligibility items, to increase rapport with the interviewer prior to questions on husband’s alcohol use or abusive behaviors. If a woman was identified as eligible, research staff again clarified the study procedures and asked if she would like to participate in the broader study, which would involve surveys over a 5 month period, as well as an HIV intervention program for those women residing in intervention cluster areas.
Participation Rates
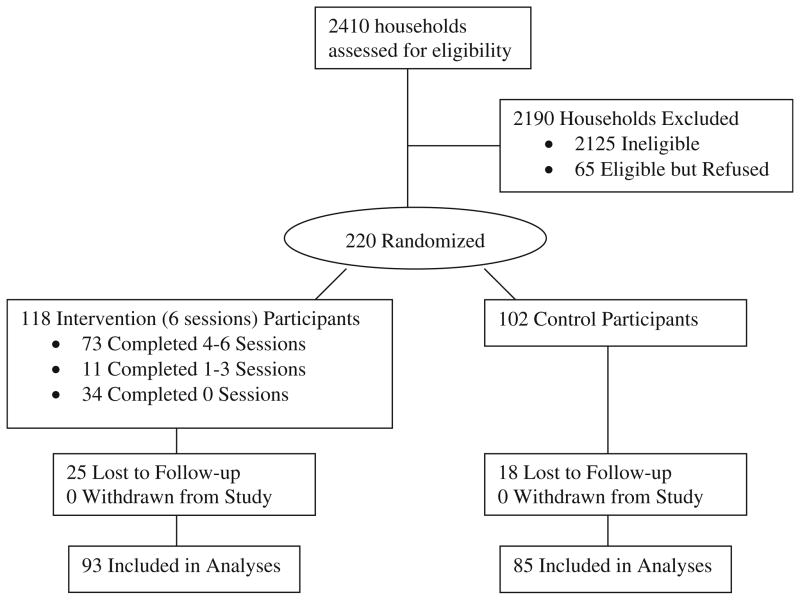
Over the 1 year recruitment period, research staff approached 2,410 households that included a married woman aged 18–40 years who agreed to screening. Of those screened, 285 women were eligible (12 % eligibility rate); 220 of these eligible women agreed to participate (77 % participation rate) and were enrolled into the study (see Fig. 1). Of those who were eligible but refused participation, time constraints and husband disapproval of participation were cited as primary reasons for refusals. Low eligibility rates in this study are believed to be a consequence of our informed consent outlining potentially stigmatizing eligibility criteria (e.g., spousal violence and husband drinking) prior to screening, a requirement of institutional review board (IRB) approval.
Fig. 1.
RHANI Wives randomized controlled trial recruitment and participation flow diagram
Study Procedure
Subsequent to written informed consent for study participation, screening, and confirmation of eligibility and willingness to participate in the study, a baseline survey was conducted with participants. Research staff administered the baseline survey via face-to-face interviews in the homes of study participants or at a nearby location, to help ensure privacy during research participation. The baseline survey assessed sociodemographics, sexual behaviors, marital violence, HIV knowledge, and attitudes toward marital condom use and condom negotiation.
Immediately following the baseline survey, women were also asked to provide a urine sample for sexually transmitted infection (STI) testing (Chlamydia trichomatis and Neisseria gonorrhea). Samples were labeled with the participant’s unique identifier number and stored in a portable storage unit. All samples were taken to the National Institute for Research in Reproductive Health at the end of each day for laboratory storage and subsequent diagnosis. Women enrolled from intervention clusters were then linked with RHANI Wives program staff for intervention receipt. At 4.5 months post-baseline, women were again assessed through a survey comparable to the baseline survey, but without demographics, and STI testing.
A number of efforts were made to support privacy for all study procedures. Research and intervention staff generally made visits during mid-day for both survey data collection and intervention sessions, as husbands were less likely to be home at that time and household chores were generally not being conducted. Morning and prior to husbands’ return from work were busy times for women and thus generally avoided. Staff requested privacy in the home, which was generally possible except in the cases where infants or children under five were present. In such cases, provided that women felt their responses would not be understood by their children, study and intervention procedures were conducted. If older or adult family members were present, staff asked those individuals if they could provide a private place, and this was generally supported as the project was identified as a health project and privacy for health exams was a norm in this setting. Staff made the request rather than asking participants to request this, to ensure participants were not held responsible for requesting the privacy. Staff members were trained to provide privacy for all efforts related to this project, and they were monitored in the field to ensure that privacy was prioritized. There were lapses in privacy identified in the course of this study, and in such cases, supervising staff intervened to establish privacy and reinforce training of frontline research and intervention staff. Where privacy was compromised, participant responses may have been affected. There should be no difference between treatment groups regarding this concern.
All data collection and intervention delivery were conducted in Hindi or Marathi by trained female research staff. No monetary or other incentive was provided for study or program participation, as required by Indian federal guidelines. All study procedures were reviewed and approved by the IRBs of Boston University Medical Campus, University of California at San Diego, the National Institute for Research in Reproductive Health, and the Indian Council of Medical Research.
Intervention Condition
As noted previously, the RHANI Wives intervention was adapted from the HIV-IP intervention conducted with US Latinas at risk for HIV from their primary male partner [14]. HIV-IP is a 12 session group intervention focused on HIV risk reduction, relationship dynamics and sexual communication, gender-based violence, poverty and financial stress, and substance use. Group discussion, counseling, and activities are used to educate and build skills among women, particularly regarding sexual communication and condom use, in a safe, supportive and women-focused environment. Formative research in the form of focus groups with at risk wives in Mumbai (7 groups), husbands reporting risky alcohol use or marital violence (2 groups) and health and social service providers working with at risk wives (3 groups) guided consideration on how the HIV-IP model should be adapted for this population. Groups were assessed on perceptions of HIV risks among wives, and then introduced to the HIV-IP model and assessed on their perceptions of it and how it might be adapted for Indian considerations. This formative research yielded the following important findings for adaptation:
The HIV-IP content and skill-building approach was consistent with needs and interests among this population in India. Emphasis on the issues of poverty and financial stress, as well as the role of husbands’ alcohol use contributing to these was viewed as an important topic. Women expressed interest in training on HIV and how to protect themselves, but greater interest was expressed for focus on the risk factors related to HIV, including husbands’ risky alcohol use, spousal violence, and potential or actual involvement with female sex workers, as well as the financial stressors that they identified as “reasons” for their husbands’ problem behaviors.
Individual (vs. group) sessions would be required for discussion of the marital relationship and sexual and relationship violence topics, due to cultural taboos against more public disclosure and discussion of these topics. Group sessions would help with social support. Couple sessions would be difficult due to women’s concerns regarding male willingness and availability to participate, as well as safety in disclosure issues.
Development of rapport via discussion of less sensitive but HIV-relevant topics such as financial stress and husband’s alcohol use should be the focus of initial discussions, so a relationship with the counselor can be built before marital sex and violence are discussed. Sexual “coercion” was highlighted more than sexual “violence” as a focus topic.
Reduction in number of sessions is needed to conduct the intervention, due to the amount of time taken to conduct individual household visits and due to women’s preferences for the program to be completed within a 2–3 month timeframe.
Building awareness among women regarding local programs and services available in the community, as well as skills to obtain informal support (i.e. from friends, family including in-laws, or local community members) against husbands’ alcohol use and partner violence perpetration were requested.
Based on the recommendations from the formative research, the RHANI Wives intervention was adapted to include four household-based individual sessions and two small group-based community sessions delivered over 6–9 weeks. Sessions began with private individual sessions focused on less sensitive topics and slowly moved to more sensitive topics in individual sessions and then group discussion on relevant topics, but without personal disclosure (see Table 1 for details). As with the HIV-IP [14], the intervention was based on Social Cognitive Theory (SCT) [18] and the Theory of Gender and Power (TGP) [19]. SCT application supported the focus on HIV/STI knowledge and condom skills building, as well as safer sex social norms and motivation. TGP guided the intervention focus on problem solving and skills building toward marital communication; embedded in this was gender empowerment counseling and support. The TGP approach promoted women taking a more active and assertive stance with husbands. Group sessions reinforced individual session knowledge and skills building and promoted local social support, both informal and from formal social service agencies (see Fig. 2 for overview of the intervention framework). All sessions were delivered by a RHANI Wives Counselor; all Counselors were female with Masters’ degrees in social work or psychology and trained in HIV prevention, spousal violence, substance use and the RHANI Wives intervention. NOTE: Condom provision was not included in the intervention, as free or low cost condom access was high in this community via a local urban health center with HIV/STI counseling and testing [16, 17].
Table 1.
Overview of RHANI Wives intervention
| Session | Timing | Content focus | Activities |
|---|---|---|---|
| Individual session 1 | Week 1 | Introductions and financial stresses and health | For individual sessions 1&2 repeat:
|
| Individual session 2 | Week 1–2 | Alcohol, IPV, financial stress, and poor health of family | |
| Group session 1 | Week 2–4 | Group support and education on HIV and marital communication |
|
| Individual session 3 | Week 3–6 | Alcohol, IPV and sexual violence, HIV and woman’s health, empowerment and safety |
|
| Group session 2 | Week 4–8 | Group support and education on linkage to local services for HIV/STI, IPV and alcohol |
|
| Individual session 4 | Week 5–9 | Alcohol, sexual violence, HIV & use of local support after program |
|
Fig. 2.
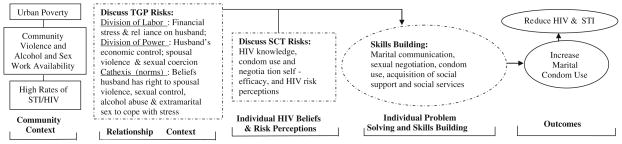
Application of Social Cognitive Theory (SCT) and Theory of Gender and Power (TGP) to the RHANI Wives intervention for wives at risk for HIV from husbands in India. Dashed line around box indicates factors targeted by RHANI Wives intervention via education, problem solving and or skills building
Control Condition
Control condition participants were provided referrals by research staff at recruitment. Referrals were for HIV/STI testing and treatment at a local urban health center, as well as local social services for alcoholics and victims of domestic violence. They were also informed through the consent process that women can be at risk for HIV from their husbands, and consistent condom use can help prevent transmission of HIV. Following completion of study participation, control condition subjects were provided with brief information on HIV prevention and local HIV/STI testing and treatment care availability.
Process Evaluation and Quality Assurance Component
A number of procedures were conducted to ensure high quality implementation of program and adherence to curriculum, and to track participant response to and engagement with the program. Attendance records with dates and length of sessions were maintained by the RHANI Wives Counselor. The RHANI Wives Counselor also maintained case notes detailing information about activities or strategies used in each session, as well as type and nature of social and health service referrals provided at each contact. Counselor notes and records were reviewed periodically and feedback was provided as necessary. Weekly meetings with the RHANI Wives Counselor were held to help problem-solve any difficulties with any clients. Finally, a brief participant satisfaction survey was conducted with participants at the 4.5 month follow-up, to obtain their feedback on the counselor and their perceptions of the utility of the program in terms of supporting the participant to be safe and healthy in their marriage.
Survey Measures
The baseline survey included information on demographics, marital sexual risk behaviors and communication, and substance use. Socio-demographics assessed were participant age, region of origin, duration of time in Mumbai, level of education (dichotomized as any vs. no formal education), number of children, relationship status and length, and age, education and employment of spouse. Sexual communication measures included whether the participant had discussed condom use with her husband in the past 3 months. The primary outcome measure for this study, the proportion of unprotected marital sex during the previous 30 days, was generated indirectly by using Poisson models with the number of marital unprotected vaginal sex acts reported in the past 30 days as the outcome variable and the total number of marital sex acts reported in the past 30 days as an offset variable. This rather than the number of unprotected marital sex acts was used to adjust for the varying number in total sex acts. Secondary outcomes were then chosen to clarify primary outcome findings by identifying whether time by treatment impact on the proportion of unprotected sex with husband was attributable to reduction of marital sex, increase in marital condom use or both. Thus, secondary outcomes included: (a) number of marital sex acts reported in the past 30 days, and among those reporting marital sex in the past 90 days, (b) any marital condom use in the past 90 days, and (c) marital condom use at last sex.
Data Analyses
Descriptive analyses were conducted to characterize the sample. Bivariate analyses were conducted to determine if participants were significantly different in demographic profile (age, education, income, marital length) and outcome characteristics for (a) intervention and control participants, (b) for those that did and did not complete the 4.5 month follow-up assessment (study attrition), and (c) for those that did and did not participate in intervention sessions among intervention participants (program attrition). Any factors significantly different between groups were considered as potential covariates in the outcome analyses.
Outcome analyses assessed the impact of the RHANI Wives intervention on unprotected sex in the marital relationship. STI was not included as an outcome due to small numbers of participants testing positive for STI at baseline (n = 2). Apparent widespread use of antibiotics in this population during the study period [20, 21] likely affected our ability to obtain reliable STI indicator data. Outcomes were assessed via logistic and Poisson generalized linear mixed models (GLMM) with cluster as a random effect and with time, treatment group, and the time x treatment group interaction as fixed effects. Over-dispersion was assessed by the values of the generalized Chi Squared statistic divided by the degrees of freedom and a scale parameter was used as a random effect in order to correct for over-dispersion in the data. Age was included as a covariate in all the models. Since examining the interactions was an imperative step in correctly assessing the effect of the intervention on the outcome, we explored the interactions both graphically and analytically. Furthermore, since detecting an interaction usually requires much more power than detecting a simple main effect, we used a liberal alpha level of 0.15 for assessing an interaction, as suggested by Selvin [22] and commonly used by others [23, 24]. If an interaction effect was detected (p ≤ 0.15), in order to determine the significance and size of differences over time by group, we proceeded with evaluating the simple main effects from the model (i.e., the main effect of treatment on the outcome, at each level of time, and conversely, the main effect of time at each level of the treatment group) directly from the full model (i.e., the model that included the interaction effect) while accounting for the interaction term. Analyses included intent to treat design using the above approach. Additional analyses were conducted to assess differential impact on outcomes based on whether any intervention sessions were attended (session attendance analyses). The original variable consisted of the number of sessions attended by each participant and took on discrete values between zero and six. Since the control group participants did not attend any sessions they were all assigned a value of zero. Because this variable was highly unbalanced, with 62 % of participants having attended none of the sessions and 33 % having attended 4 or more sessions, we constructed a hybrid binary variable (any sessions attendance vs. no sessions attendance) and used this variable in the outcomes analyses. Control group participants were included in the no sessions group to provide sufficient power for analyses. All tests for the outcome analyses were two-sided and had an alpha level of 0.05 (with the exception of the tests for the interaction effects which had an alpha level of 0.15). All analyses were conducted using SAS (SAS Institute, Version 9.3, Cary, NC, USA).
Results
Sample Characteristics
Mean age of participants was 29.5 years (SD = 5.8), and mean marital length was 11.7 years (SD = 6.5) (see Table 2). Half of the women married prior to age 18 years. One in five women (21.4 %) had no formal education; 30.9 % reported any personal income generation. Most women (93.6 %) had children. One-third of participants (35.0 %) reported spousal violence in the past 90 days, and 58.6 % reported their husband was drunk in the past 30 days. One-fourth of the sample (24.5 %) had ever asked their husband to use a condom; 80.7 % of those who were sexually active in the past 90 days (n = 117/145) reported no condom use in this same timeframe.
Table 2.
Sample Characteristics of RHANI Wives study participants, total sample (N = 220) and by treatment group
| Total sample N = 220 n (%) |
Intervention group n = 118 n (%) |
Control group n = 102 n (%) |
|
|---|---|---|---|
| Demographics | |||
| Mean age (SD, range) | 29.5 years (5.8, 18–40) | 29.0 years (6.0, 18–40) | 30.1 years (5.5, 18–40) |
| Any formal education | 47 (21.4 %) | 27 (22.9 %) | 20 (19.6 %) |
| Any income generation | 68 (30.9 %) | 40 (33.9 %) | 28 (27.5 %) |
| Native to Mumbai | 81 (36.8 %) | 47 (39.8 %) | 34 (33.3 %) |
| Religion* | |||
| Hindu | 140 (63.3 %) | 77 (65.3 %) | 63 (61.8 %) |
| Muslim | 24 (10.9) | 3 (2.5 %) | 21 (20.6 %) |
| Buddhist | 48 (21.8 %) | 35 (29.7 %) | 13 (12.7 %) |
| Christian | 8 (3.6 %) | 3 (2.5 %) | 5 (4.9 %) |
| Mean length of marriage (SD, Range) | 11.7 years (6.5, 1–27) | 11.8 years (6.7, 2–27) | 11.7 years (6.4, 1–27) |
| Married prior to age 18 years | 110 (50.0 %) | 65 (55.1 %) | 45 (44.1 %) |
| Any children | 206 (93.6 %) | 113 (95.8 %) | 93 (91.2 %) |
| Mean number of children (SD, Range) | 2.4 (1.2, 0–7) | 2.3 (1.1, 0–5) | 2.4 (1.4, 0–7) |
| Risk profile | |||
| IPV (physical or sexual), past 90 days | 77 (35.0 %) | 45 (38.1 %) | 32 (31.4 %) |
| Husband drunk, past 90 days | 129 (58.6 %) | 74 (62.7 %) | 55 (53.9 %) |
| Asked husband to use a condom, past 90 days | 44 (20.0 %) | 23 (19.5 %) | 21 (20.6 %) |
| Frequency of condom use, past 90 daysa | |||
| Every time | 9 (6.2 %) | 6 (8.3 %) | 3 (4.1 %) |
| Almost every time | 9 (6.2 %) | 6 (8.3 %) | 3 (4.1 %) |
| Sometimes | 10 (6.9 %) | 8 (11.1 %) | 2 (2.7 %) |
| Never | 117 (80.7 %) | 52 (72.2 %) | 65 (89.0 %) |
| Condom use at last sex | 25 (11.4 %) | 17 (14.4 %) | 8 (7.8 %) |
Significant difference between intervention and control conditions observed for this variable (p <0.05)
Among subsample of participants reporting sexual activity in the past 90 days (Total N = 196; Intervention n = 103, Control n = 93)
Bivariate Associations to Assess Differences by Treatment Groups, Study Attrition/Retention and Intervention Attrition/Retention
Significant differences were observed between treatment groups at baseline for religion and condom negotiation (p<0.05). Hindus were the majority for both groups, but Buddhists were slightly more represented in the intervention group and Muslims in the control condition (see Table 2). Intervention participants were significantly more likely than control participants to have ever asked their partner to use a condom (p = 0.02). No significant differences were seen between those who did and did not participate in follow-up surveys; nor were any differences observed between those who did and did not participate in intervention sessions, among intervention participants.
Intent to Treat Outcome Analyses
Intent to treat analyses documented a significant time by treatment effect on the proportion of unprotected sex with husband (p = 0.01), but not on the number of marital sex acts or on the probability of using a condom with the husband (see Table 3). To clarify the observed time by treatment effect on the proportion of unprotected sex, simple main effects were evaluated from the full model taking into account the interaction term. The rate of unprotected sex for intervention participants was significantly lower than that of control participants at follow-up (RR = 0.83, 95 % CI = 0.75, 0.93; p = 0.001); this rate also significantly lessened over time for the intervention group (RR = 0.87; 95 % CI = 0.79, 0.95; p = 0.001) but not the control group.
Table 3.
Poisson and logistic GLMM to assess the RHANI Wives intervention effects on marital safer sex practices (n = 220)
| Outcome | Analysis type | Effect | Regression coefficient | Standard error | Rate ratioa | Lower 95 % CI | Upper 95 % CI | Test statisticb | p value |
|---|---|---|---|---|---|---|---|---|---|
| Proportion of unprotected vaginal sex with husband, past 30 days | Full model | Visit (follow-up vs. baseline) | 0.006 | 0.036 | 1.01 | 0.94 | 1.08 | 5.68 | 0.018 |
| Intervention group (intervention vs. control) | −0.032 | 0.042 | 0.97 | 0.89 | 1.05 | 7.26 | 0.007 | ||
| Age | 0.005 | 0.003 | 1.01 | 1.00 | 1.01 | 2.85 | 0.092 | ||
| Visit × intervention group | −0.150 | 0.058 | 0.86 | 0.77 | 0.96 | 6.77 | 0.010 | ||
| Simple main effects | Baseline: intervention vs. control | −0.032 | 0.042 | 0.97 | 0.89 | 1.05 | −0.77 | 0.440 | |
| Follow-up: intervention vs. control | −0.182 | 0.055 | 0.83 | 0.75 | 0.93 | −3.29 | 0.001 | ||
| Control group: follow- up vs. baseline | 0.006 | 0.036 | 1.01 | 0.94 | 1.08 | 0.17 | 0.863 | ||
| Intervention group: follow-up vs. baseline | −0.143 | 0.045 | 0.87 | 0.79 | 0.95 | −3.20 | 0.001 | ||
| Total number of vaginal sex acts with husband, past 30 days | Full model | Visit (follow-up vs. baseline) | −0.212 | 0.115 | 0.81 | 0.64 | 1.02 | 11.94 | 0.001 |
| Intervention group (intervention vs. control) | −0.348 | 0.168 | 0.71 | 0.49 | 1.02 | 7.05 | 0.029 | ||
| Age | −0.055 | 0.010 | 0.95 | 0.93 | 0.97 | 31.84 | 0.000 | ||
| Visit × intervention group | −0.126 | 0.159 | 0.88 | 0.64 | 1.21 | 0.63 | 0.429 | ||
| Simple main effects (NA) | Baseline: intervention vs. control | −0.348 | 0.168 | 0.71 | 0.49 | 1.02 | −2.07 | 0.061 | |
| Follow-up: intervention vs. control | −0.474 | 0.180 | 0.62 | 0.42 | 0.91 | −2.64 | 0.019 | ||
| Control group: follow- up vs. baseline | −0.212 | 0.115 | 0.81 | 0.64 | 1.02 | −1.84 | 0.068 | ||
| Intervention group: follow-up vs. baseline | −0.338 | 0.110 | 0.71 | 0.57 | 0.89 | −3.07 | 0.003 | ||
| Any marital condom use in the past 90 daysc | Full model | Visit (follow-up vs. baseline) | −0.152 | 0.395 | 0.86 | 0.39 | 1.87 | 0.30 | 0.583 |
| Intervention group (intervention vs. control) | 0.439 | 0.388 | 1.55 | 0.72 | 3.33 | 4.70 | 0.031 | ||
| Age | −0.072 | 0.031 | 0.93 | 0.88 | 0.99 | 5.47 | 0.020 | ||
| Visit × intervention group | 0.576 | 0.496 | 1.78 | 0.67 | 4.72 | 1.35 | 0.246 | ||
| Simple main effects | Baseline: intervention vs. control | 0.424 | 0.300 | 1.53 | 0.85 | 2.76 | 1.42 | 0.158 | |
| Follow-up: intervention vs. control | −0.152 | 0.395 | 0.86 | 0.39 | 1.87 | −0.38 | 0.701 | ||
| Control group: follow- up vs. baseline | 1.015 | 0.444 | 2.76 | 1.15 | 6.60 | 2.29 | 0.023 | ||
| Intervention group: follow-up vs. baseline | 0.439 | 0.388 | 1.55 | 0.72 | 3.33 | 1.13 | 0.259 | ||
| Marital condom use at last sexc | Full model | Visit (follow-up vs. baseline) | 0.103 | 0.424 | 1.11 | 0.48 | 2.55 | 3.71 | 0.055 |
| Intervention group (intervention vs. control) | 0.037 | 0.480 | 1.04 | 0.40 | 2.67 | 1.39 | 0.239 | ||
| Age | −0.092 | 0.036 | 0.91 | 0.85 | 0.98 | 6.58 | 0.011 | ||
| Visit × intervention group | 0.849 | 0.547 | 2.34 | 0.80 | 6.86 | 2.40 | 0.122 | ||
| Simple main effects | Baseline: intervention vs. control | 0.952 | 0.347 | 2.59 | 1.31 | 5.13 | 2.74 | 0.006 | |
| Follow-up: intervention vs. control | 0.103 | 0.424 | 1.11 | 0.48 | 2.55 | 0.24 | 0.808 | ||
| Control group: follow- up vs. baseline | 0.885 | 0.474 | 2.42 | 1.002 | 5.76 | 1.97 | 0.049 | ||
| Intervention group: follow-up vs. baseline | 0.037 | 0.480 | 1.04 | 0.40 | 2.67 | 0.08 | 0.939 |
Analyses were adjusted for age
Intent to treat analyses
For the binary outcomes (i.e., any marital condom use and condom use at last sex) the corresponding estimates represent odds ratios
The effects in the full model were tested by type III F tests for fixed effects whereas the simple main effects were tested for the differences in least squares means by using t tests
For subsample of participants reporting marital sex in the past 90 days (n = 196)
For the any condom use outcome, the interaction between time and treatment group was not significant (p = 0.246) and for condom use at last sex, the corresponding interaction was significant (p = 0.122). However, in both cases, graphical display of the interactions indicated a possible differential time effect on the outcome based on the intervention groups. As a result, to explore the differences in the effect over time by treatment for these outcomes, simple main effects were estimated from the full models and their significance was assessed.
Any condom use was significantly more likely for intervention relative to control group at follow-up (OR = 2.76, 95 % CI = 1.15, 6.60, p = 0.023), but no significant differences were observed in change over time for intervention or control groups. Condom use at last sex was significantly more likely for intervention relative to control group at follow-up (OR = 2.42, 95 % CI = 1.002, 5.70; p = 0.049); the corresponding odds also significantly increased over time for the intervention group (RR = 2.59; 95 % CI = 1.31, 5.13; p = 0.006) but not for the control group.
Session Attendance Analyses
Significant time by any session attendance impact was seen on the proportion of unprotected sex with husband (p = 0.002), condom use at last sex with husband (p = 0.015), and any marital condom use (p = 0.077); no effect was seen on total number of sex acts with husband (see Table 4). Simple main effects analyses revealed that, at follow-up, the rate of marital unprotected sex for those who attended any sessions was significantly lower than for those who attended no sessions (RR = 0.81, 95 % CI = 0.72, 0.91; p<0.001); this rate also decreased over time for those who attended any sessions (RR = 0.84; 95 % CI = 0.76, 0.92; p<0.001) but not for those attending no sessions.
Table 4.
Poisson and logistic GLMM to assess time by receipt of RHANI Wives intervention sessions (any sessions received) on marital safer sex practices (n = 220)
| Outcome | Analysis type | Effect | Regression coefficient | Standard error | Rate ratioa | Lower 95 % CI | Upper 95 % CI | Test statisticb | p value |
|---|---|---|---|---|---|---|---|---|---|
| Proportion of unprotected vaginal sex with husband, past 30 days | Full model | Visit (follow-up vs. baseline) | 0.014 | 0.035 | 1.01 | 0.95 | 1.09 | 7.13 | 0.008 |
| Group (any vs. no intervention sessions) | −0.024 | 0.041 | 0.98 | 0.90 | 1.06 | 8.36 | 0.004 | ||
| Age | 0.005 | 0.003 | 1.01 | 1.00 | 1.01 | 2.54 | 0.111 | ||
| Visit × group | −0.190 | 0.061 | 0.83 | 0.73 | 0.93 | 9.75 | 0.002 | ||
| Simple main Effects | Baseline: any vs. no sessions | −0.024 | 0.041 | 0.98 | 0.90 | 1.06 | −0.58 | 0.561 | |
| Follow-up: any vs. no sessions | −0.214 | 0.050 | 0.81 | 0.72 | 0.91 | −3.60 | 0.000 | ||
| No sessions: follow- up vs. baseline | 0.014 | 0.035 | 1.01 | 0.95 | 1.09 | 0.39 | 0.693 | ||
| Any vs. no sessions: follow-up vs. baseline | −0.176 | 0.050 | 0.84 | 0.76 | 0.92 | −3.53 | 0.000 | ||
| Total number of vaginal sex acts with husband, past 30 days | Full model | Visit (follow-up vs. baseline) | −0.218 | 0.601 | 0.80 | 0.24 | 2.64 | 0.43 | 0.511 |
| Any sessions group (any vs. no sessions) | −0.178 | 0.670 | 0.84 | 0.22 | 3.24 | 0.25 | 0.621 | ||
| Age | −0.058 | 0.041 | 0.94 | 0.87 | 1.03 | 2.02 | 0.166 | ||
| Visit × group | −0.181 | 0.934 | 0.83 | 0.13 | 5.28 | 0.04 | 0.847 | ||
| Simple main effects (NA) | Baseline: any vs. no sessions | −0.178 | 0.670 | 0.84 | 0.22 | 3.24 | −0.26 | 0.792 | |
| Follow-up: any vs. no sessions | −0.358 | 0.744 | 0.70 | 0.16 | 3.14 | −0.48 | 0.633 | ||
| No sessions: follow- up vs. baseline | −0.218 | 0.602 | 0.80 | 0.24 | 2.64 | −0.36 | 0.718 | ||
| Any sessions: follow- up vs. baseline | −0.398 | 0.715 | 0.67 | 0.16 | 2.75 | −0.56 | 0.578 | ||
| Any marital condom use in the past 90 daysc | Full model | Visit (follow-up vs. baseline) | −0.287 | 0.355 | 0.75 | 0.37 | 1.51 | 0.34 | 0.561 |
| Any sessions group (any vs. no sessions) | 0.254 | 0.394 | 1.29 | 0.59 | 2.80 | 3.94 | 0.048 | ||
| Age | −0.073 | 0.031 | 0.93 | 0.87 | 0.99 | 5.63 | 0.018 | ||
| Visit × group | 0.853 | 0.481 | 2.35 | 0.91 | 6.05 | 3.14 | 0.077 | ||
| Simple main effects | Baseline: any vs. no sessions | 0.566 | 0.324 | 1.76 | 0.93 | 3.33 | 1.75 | 0.082 | |
| Follow-up: any vs. no sessions | −0.287 | 0.355 | 0.75 | 0.37 | 1.51 | −0.81 | 0.421 | ||
| No sessions: follow- up vs. baseline | 1.107 | 0.442 | 3.03 | 1.27 | 7.22 | 2.50 | 0.013 | ||
| Any sessions: follow- up vs. baseline | 0.254 | 0.394 | 1.29 | 0.59 | 2.80 | 0.65 | 0.519 | ||
| Marital condom use at last sexc | Full model | Visit (follow-up vs. baseline) | −0.056 | 0.378 | 0.95 | 0.45 | 1.99 | 5.07 | 0.025 |
| Any sessions group (any vs. no sessions) | −0.400 | 0.492 | 0.67 | 0.25 | 1.76 | 0.58 | 0.445 | ||
| Age | −0.090 | 0.035 | 0.91 | 0.85 | 0.98 | 6.51 | 0.011 | ||
| Visit × group | 1.370 | 0.559 | 3.94 | 1.31 | 11.83 | 6.00 | 0.015 | ||
| Simple main effects | Baseline: any vs. no sessions | 1.315 | 0.413 | 3.72 | 1.65 | 8.38 | 3.19 | 0.002 | |
| Follow-up: any vs. no sessions | −0.056 | 0.378 | 0.95 | 0.45 | 1.99 | −0.15 | 0.883 | ||
| No sessions: follow- up vs. baseline | 0.971 | 0.440 | 2.64 | 1.11 | 6.27 | 2.21 | 0.028 | ||
| Any sessions: follow- up vs. baseline | −0.400 | 0.492 | 0.67 | 0.25 | 1.76 | −0.81 | 0.417 |
Analyses were adjusted for age
Session attendance analyses
For the binary outcomes (i.e., any marital condom use and condom use at last sex) the corresponding estimates represent odds ratios
The effects in the full model were tested by type III F tests for fixed effects whereas the simple main effects were tested for the differences in least squares means by using t tests
For subsample of participants reporting marital sex in the past 90 days (n = 196)
Simple main effects analyses also indicated that, at follow-up, the odds of condom use at last sex with husband were significantly higher for those who attended any sessions relative to those who did not attend any sessions (OR = 2.64, 95 % CI = 1.11, 6.27; p = 0.028); the corresponding odds also significantly increased over time for those who attended sessions (OR = 3.72; 95 % CI = 1.65, 8.38; p = 0.002) but not for those who did not attend any sessions. The odds of any condom use with husband were significantly higher, at follow-up, for those who attended any versus no sessions (OR = 3.03, 95 % CI = 1.29, 7.22; p = 0.013), and the corresponding odds increased marginally over time for those who attended any sessions (OR = 1.76, 95 % CI = 0.93, 3.33; p = 0.082) but not for those who did not attend any sessions.
Intervention Participants’ Reports of Program Topics Covered and Response to Program
Most (>75 %) of the 80 intervention participants who provided participant response data reported discussions with their RHANI Wives Counselor on the topics of health, alcohol, the marital relationship and communication, HIV prevention, and STI knowledge (see Table 5). A small percentage (15.0 %) reported discussion of condom use with the counselor. In terms of participants’ perceived impact of the intervention, most women reported improved STI knowledge (85.0 %) and marital communication (81.0 %); slightly less than half reported increasing their sexual negotiation (45.0 %) and condom discussion (43.8 %) with husbands. Approximately a quarter reported improved condom use with husband (26.3 %) and husband care for her sexual concerns (27.5 %).
Table 5.
Intervention participants’ response to program (n = 80 intervention participants)
| n (%) | |
|---|---|
| Topics covered in RHANI Wives individual counseling sessions | |
| General health | 68 (85.0) |
| Husband’s alcohol use | 72 (90.0) |
| Microfinance and poverty management opportunities | 49 (61.3) |
| Poverty | 39 (48.8) |
| Violence within relationship | 53 (66.3) |
| Your relationship with husband | 66 (82.5) |
| Your communication with husband | 64 (80.0) |
| Your relationship with other men | 43 (53.8) |
| Your knowledge about transmission of HIV | 58 (72.5) |
| Your knowledge about prevention of HIV | 62 (77.5) |
| Your knowledge about STI | 68 (85.0) |
| Causes of STI | 60 (75.0) |
| Use of condoms | 36 (15.0) |
| Beliefs regarding perceived effects of individual counseling sessions | |
| Counseling resulted in my better marital communication | 65 (81.3) |
| Counseling resulted in my improved sex negotiation | 36 (45.0) |
| Counseling resulted in my more effectively dealing with tension (life stresses) | 45 (56.3) |
| Counseling resulted in my better knowledge about STI | 68 (85.0) |
| Counseling resulted in my husband and I discussing condom use | 35 (43.8) |
| Counseling resulted in my husband communicating with me better | 58 (72.5) |
| Counseling resulted in my husband being more caring about my sexual concerns | 22 (27.5) |
| Counseling resulted in my husband respecting my views in decision making | 36 (45.0) |
| Counseling resulted in my husband contributing to reduction in my tension | 37 (46.3) |
| Counseling resulted in my husband participating in more household chores | 25 (31.3) |
| Counseling resulted in my husband reducing his intake in alcohol | 27 (33.8) |
| Counseling resulted in my husband having better health | 16 (20.0) |
| Counseling resulted in my husband having better knowledge about STI | 45 (56.3) |
| Counseling resulted in my husband agreeing to use condoms | 21 (26.3) |
Discussion
Findings from this study indicate that the RHANI Wives intervention is effective in reducing unprotected marital sex among women contending with husbands who engage in risky alcohol use and/or spousal violence, factors associated with HIV among men and their wives in a high epidemic slum community in Mumbai, India [8–11]. These findings reinforce studies from Asia, Africa and the US, documenting the utility of sexual risk reduction programs for women at risk for HIV from their steady male partner. [13–15, 25–27] Consistent with prior effective HIV interventions for women [25–27], RHANI Wives included gender and risk tailoring, use of behavioral change theory, focus on self-management and self-efficacy skill-building, and provision of social support at the community level.
Of note, further analysis indicates that intervention impact on unprotected sex is attributable to improved marital condom use, rather than reduction in marital sex. Such findings may have been affected by intervention participants being more likely than control participants to report ever requesting their husbands to use condoms at baseline. However, exploratory analyses did not indicate this to be the case. Nonetheless, despite significant improvements in any marital condom use for intervention relative to control participants, such use was still reported by the minority (25 %) of intervention participants at follow- up. Greater emphasis on condom use in the intervention may have been needed, as the minority of participants reported discussion of condom use. The intervention did include condom demonstrations and statements promoting condom use for HIV prevention, but such an approach does not require condom discussion. Further, provision of the condom demonstration and opportunity for HIV risk discussion was not a focus until Session 3, potentially minimizing its recognition among participants that did not receive these sessions. Strong and significant effects of intervention participation on this variable support this point, suggesting that the intervention’s impact on condom use is significant but requires program participation. However, further analysis is needed and likely requires a larger sample size, as the original study was not powered to focus on consistent marital condom use, but only on proportion of unprotected sex.
Though the intervention model was effective, participant identification and intervention participation was a concern. Few women screened were eligible (12 %), suggesting household recruitment was an inefficient means of reaching this population. Another recent study involving household recruitment for an HIV intervention with Indian wives of heavy drinkers similarly found this to be an inefficient means of reaching this population [28]. Such limited numbers of eligible participants likely indicates selection bias, inhibiting generalizability of study findings. Selection bias may be a concern, as participants were required to disclose stigmatizing behaviors of their husbands, limiting generalizability of study findings. Additionally, among those agreeing to participate in the study, 29 % of intervention participants received no sessions, limiting our understanding of response to program. Nonetheless, among those participating in any sessions, 87 % participated in all four individual sessions, though only 28 % received group sessions (see Fig. 1). These findings suggest that individual sessions are the crux of RHANI Wives and are highly acceptable to women once they initiate program participation. Focus on more efficient recruitment of participants who are ready to initiate the intervention would be needed for future implementation. Indicators of such willingness and readiness need to be determined.
Other study limitations included reliance on self-report outcomes, aside from STI. Assessment of solely bacterial STIs at a time of very high antibiotic use in Mumbai impeded our ability to assess biological impact of the intervention [20, 21]. Lack of an attention comparison condition prohibits assumptions that observed program effects are attributable to the intervention rather than counselor contact. Also, small sample size limits our ability to determine if the observed intervention impact occurred via the theory-generated risk factors addressed in the intervention, as outlined in Fig. 2. Fertility desire was not measured, limiting our ability to consider the role of such desire on the intervention’s impact on condom use. Short term follow-up and use of only one follow-up assessment are also weaknesses of this study. Future larger scale evaluation of RHANI Wives is needed and should be inclusive of an attention comparison group, analysis of potential mediators, longer term follow-up, as well as viral STI outcomes.
Conclusion
The RHANI Wives intervention is effective in reducing unprotected sex via increased marital condom use among wives at risk for HIV from husbands based on a randomized cluster controlled trial and short-term follow-up. These findings, notable for achieving significant impact on reducing unprotected marital sex, suggest that RHANI Wives is a promising model of HIV prevention. Nonetheless, longer-term evaluation inclusive of STI outcomes is needed, as is determination of the model’s adaptability in clinic or facility based settings where wives at risk for HIV may be more easily reached.
Acknowledgments
This work was presented at a Poster Exhibition at the XIX International AIDS Conference (AIDS 2012), held in Washington, DC, 22–27 July 2012.
We would like to thank the women who participated in this study for providing their time and input for this study as well as the RHANI Wives research and intervention counseling teams for their integral role in the implementation of study. We would also like to thank the non-governmental organizations Cehat, Alcoholics Anonymous, and Swadhaar for their consultation and input in the areas of domestic violence, alcohol use, and financial stressors and solutions, respectively. This input was significant both for intervention development and referrals for RHANI Wives study participants. Additionally, would like to thank Dr. Jayanti of NIRRH for her important contributions to STI diagnosis for this study and Dr. Stephen Schensul for his consultations on the intervention. The RHANI Wives study could not have been conducted without the support of all of these individuals and groups. This study was funded via grants from the Indian Council for Medical Research (Indo-US/38/2007- ECD-II; PI: D. Balaiah) and the United States National Institutes of Health (R21MH85614; PI: A. Raj).
Footnotes
Conflict of interest: Authors have no conflicts of interest to report.
This study is registered at ClinicalTrials.gov, ID# NCT01592994.
Contributor Information
Anita Raj, Email: anitaraj@ucsd.edu, Division of Global Public Health, Department of Medicine, University of California, San Diego School of Medicine, San Diego, CA, USA. Center on Gender Equity and Health, University of California, San Diego, CA, USA. Clinical Addiction Research and Education, Section of General Internal Medicine, Department of Medicine, Boston University School of Medicine/Boston Medical Center, Boston, MA, USA. University of California San Diego School of Medicine, 9500 Gilman Drive, MC 0507, La Jolla, CA 92093-0507, USA.
Niranjan Saggurti, Population Council, New Delhi, India.
Madhusudana Battala, Population Council, New Delhi, India.
Saritha Nair, National Institute for Research in Reproductive Health, Mumbai, India.
Anindita Dasgupta, Division of Global Public Health, Department of Medicine, University of California, San Diego School of Medicine, San Diego, CA, USA.Center on Gender Equity and Health, University of California, San Diego, CA, USA. Joint Doctoral Program in Public Health (Global Health), San Diego State University/University of California, San Diego, San Diego, CA, USA.
D. D. Naik, National Institute for Research in Reproductive Health, Mumbai, India
Daniela Abramovitz, Division of Global Public Health, Department of Medicine, University of California, San Diego School of Medicine, San Diego, CA, USA.
Jay G. Silverman, Division of Global Public Health, Department of Medicine, University of California, San Diego School of Medicine, San Diego, CA, USA. Center on Gender Equity and Health, University of California, San Diego, CA, USA. University of California San Diego School of Medicine, 9500 Gilman Drive, MC 0507, La Jolla, CA 92093-0507, USA. Department of Society, Human Development and Health, Harvard School of Public Health, Harvard University, Boston, MA, USA
Donta Balaiah, National Institute for Research in Reproductive Health, Mumbai, India.
References
- 1.National AIDS Control Organization (NACO) [Accessed 3 Aug 2013];NACO Annual Report 2010–2011. http://aidsdatahub.org/dmdocuments/NACO_Annual_Report_2011_12.pdf.
- 2.The World Bank. [Accessed 2 July 2012];HIV/AIDS in India. 2012 http://www.worldbank.org/en/news/feature/2012/07/10/hiv-aids-india.
- 3.Pandey A, Sahu D, Bakkali T, et al. Estimate of HIV prevalence and number of people living with HIV in India 2008–2009. BMJ Open. 2012;2:e000926. doi: 10.1136/bmjopen-2012-000926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ganju D, Mahapatra B, Saggurti N. Male migrants’ non-spousal sexual partnerships in the place of origin: an in-depth investigation in two rural settings of India. Cult Health Sex. 2013;15(3):341–57. doi: 10.1080/13691058.2012.756932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saggurti N, Mahapatra B, Sabarwal S, et al. Male out-migration: a Factor for the spread of HIV among married men and women in rural India. PLoS One. 2012;7(9):e43222. doi: 10.1371/journal.pone.0043222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National family health survey (NFHS-3), 2005–06: India. Mumbai: International Institute for Population Sciences (IIPS) and Macro International; 2007. [Google Scholar]
- 7.Population Council. HIV Transmission among Married Men and Women in Districts with High Out-migration in India. [Accessed 3 Aug 2013];Study Brief. http://www.popcouncil.org/pdfs/2011HIV_IndiaHIVandMigrationStudyBrief.pdf.
- 8.Silverman JG, Decker MR, Saggurti N, et al. Intimate partner violence and HIV infection among married Indian women. JAMA. 2008;300(6):703–10. doi: 10.1001/jama.300.6.703. [DOI] [PubMed] [Google Scholar]
- 9.Saggurti N, Schensul SL, Verma RK. Migration, mobility and sexual risk behavior in Mumbai, India: mobile men with nonresidential wife show increased risk. AIDS Behav. 2009;13(5):921–7. doi: 10.1007/s10461-009-9564-8. [DOI] [PubMed] [Google Scholar]
- 10.Saggurti N, Schensul SL, Singh R. Alcohol use, sexual risk behavior and STIs among married men in Mumbai, India. AIDS Behav. 2010;14(Suppl 1):S40–7. doi: 10.1007/s10461-010-9728-6. [DOI] [PubMed] [Google Scholar]
- 11.Schensul JJ, Singh SK, Gupta K, et al. Alcohol and HIV in India: a review of current research and intervention. AIDS Behav. 2010;14:S1–7. doi: 10.1007/s10461-010-9740-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Decker MR, Miller E, Raj A, et al. Indian men’s use of commercial sex workers: prevalence, condom use, and related gender attitudes. J Acquir Immune Defic Syndr. 2010;53(2):240–6. doi: 10.1097/QAI.0b013e3181c2fb2e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pronyk PM, Hargreaves JR, Kim JC, et al. Effect of a structural intervention for the prevention of intimate partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet. 2006;368(9551):1973–83. doi: 10.1016/S0140-6736(06)69744-4. [DOI] [PubMed] [Google Scholar]
- 14.Raj A, Amaro H, Cranston K, et al. Is a general women’s health promotion program as effective as an HIV-intensive prevention program in reducing HIV risk among Hispanic women? Public Health Rep. 2001;116(6):599–607. doi: 10.1093/phr/116.6.599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wechsberg WM, Browne FA, Ellerson RM, et al. Adapting the evidence-based Women’s CoOp intervention to prevention human immunodeficiency virus infection in North Carolina and international settings. N C Med J. 2010;71(5):477–81. [PMC free article] [PubMed] [Google Scholar]
- 16.Vahini Shakti. [Accessed 3 Aug 2013];Trafficking in India Report. 2004 http://www.scribd.com/doc/75417881/Trafficking-in-India-Report-2004-Shakti-Vahini.
- 17.Pathak H. MDACS (Mumbai District AIDS Control) data shared with Dr. Anita Raj during personal meeting with Dr Harish Pathak, Additional Project Director, MDACS, Mumbai; February 2012; Mumbai, India. [Google Scholar]
- 18.Bandura A. Social cognitive theory and exercise of control over HIV infection. In: DiClemente R, Peterson J, editors. Preventing AIDS: theories and methods of behavioral interventions. New York: Plenum; 1994. pp. 25–59. [Google Scholar]
- 19.Connell RW. Gender and power: society, the person and sexual politics. Stanford, CA: Stanford University Press; 1987. [Google Scholar]
- 20.Abdul Ghafur K. An obituary—on the death of antibiotics. JAPI. 2010;58:143–4. [PubMed] [Google Scholar]
- 21.Parikh F. Status of antibiotic use in India. JAPI. 2010;58:7. [PubMed] [Google Scholar]
- 22.Selvin S. Statistical analysis of epidemiologic data. New York: Oxford University Press; 1996. pp. 213–4. [Google Scholar]
- 23.Kwan ML, Block G, Selvin S, et al. Food consumption by children and the risk of childhood acute leukemia. Am J Epidemiol. 2004;160:1098–107. doi: 10.1093/aje/kwh317. [DOI] [PubMed] [Google Scholar]
- 24.Sansbury LB, Millikan RC, Schroeder JC, et al. Use of nonsteroidal antiinflammatory drugs and risk of colon cancer in a population-based, case-control study of African Americans and Whites. Am J Epidemiol. 2005;162:548–58. doi: 10.1093/aje/kwi248. [DOI] [PubMed] [Google Scholar]
- 25.Rotheram-Borus MJ, Swendeman D, Flannery D, et al. Common factors in effective HIV prevention programs. AIDS Behav. 2009;13(3):399–408. doi: 10.1007/s10461-008-9464-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tan JY, Huedo-Medina TB, Warren MR, et al. A Meta-Analysis of efficacy of HIV/AIDS prevention interventions in Asia, 1995–2009. Soc Sci Med. 2012;75(4):676–87. doi: 10.1016/j.socscimed.2011.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wechsberg WM, Luseno WK. The need for culturally appropriate, gender-specific global HIV prevention efforts with vulnerable women. J Prev Interv Community. 2010;38(2):85–8. doi: 10.1080/10852351003640559. [DOI] [PubMed] [Google Scholar]
- 28.Cottler LB, Satyanarayana VA, O’Leary CC, et al. Feasibility and effectiveness of HIV prevention among wives of heavy drinkers in Bangalore. AIDS Behav. 2010;14(Suppl 1):S168–76. doi: 10.1007/s10461-010-9729-5. [DOI] [PMC free article] [PubMed] [Google Scholar]