Abstract
Objective
Excess weight gain in American Indian/Alaskan native (AI/AN) children is a public health concern. This study tested 1) the feasibility of delivering community-wide interventions, alone or in combination with family-based interventions, to promote breastfeeding and reduce the consumption of sugar-sweetened beverages; and 2) whether these interventions decrease Body Mass Index (BMI)-Z scores in children 18–24 months of age.
Methods
Three AI/AN tribes were randomly assigned to two active interventions; a community-wide intervention alone (tribe A; n=63 families) or community-wide intervention containing a family component (tribes B and C; n=142 families). Tribal staff and the research team designed community-tailored interventions and trained community health workers to deliver the family intervention through home visits. Feasibility and acceptability of the intervention and BMI-Z scores at 18–24 months were compared between tribe A and tribes B&C combined using a separate sample pretest, posttest design.
Results
Eighty-six percent of enrolled families completed the study. Breastfeeding initiation and 6-month duration increased 14 and 15%, respectively, in all tribes compared to national rates for American Indians. Breastfeeding at 12 months was comparable to national data. Parents expressed confidence in their ability to curtail family consumption of sugar-sweetened beverages. Compared to a pretest sample of children of a similar age two years before the study begun, BMI-Z scores increased in all tribes. However, the increase was less in tribes B &C compared to tribe A (−0.75, p=0.016).
Conclusion
Family, plus community-wide interventions to increase breastfeeding and curtail sugar-sweetened beverages attenuate BMI rise in AI/AN toddlers more than community-wide interventions alone.
Keywords: Obesity prevention, infants, toddlers, breastfeeding, sugar-sweetened beverages
Introduction
The prevalence of overweight in children aged 2–5 years in the US has increased, with children from racial and ethnic minority populations showing the greatest increases.1,2 American Indian/Alaskan Native (AI/AN) children have a high risk of overweight, and potential for adult obesity. The prevalence of overweight (BMI≥85th percentile) among AI/AN children 5–17 years of age is approximately 47%, compared to 33.6% in similarly aged children of other races.3 The risk for overweight may begin at birth in AI/AN children. Pima Indian infants, for example, gain weight more rapidly in the first six months of life than reference children, and the most potent predictor of adolescent weight among the Pima is weight at 5 years of age.4, 5 Approximately 12.6% of AI/AN infants (0–11 months) and 24% of toddlers (12–23 months) are at risk for overweight, compared to 10.9% and 17%, respectively, for infants and toddlers from the general population.4 Among preschoolers, 40% of AI/AN children are overweight, compared to 31.2% in the general population of preschoolers aged 2–5 years.6
Obesity prevention efforts targeted at younger children in populations experiencing excess weight gain in early life are needed. Breastfeeding and curtailment of sugar-sweetened beverage consumption may prevent excess weight gain in children.7, 8 We describe results of a pilot intervention to prevent excess weight gain in AI/AN toddlers, by promoting breastfeeding and curtailment of sugar-sweetened beverage consumption..
Methods
The toddler overweight and tooth decay prevention study (TOTS) was an obesity prevention community-based study. We compared two active interventions to prevent obesity; 1) a community wide intervention and 2) a community wide intervention with an added family-based component, as methods for the promotion of breastfeeding and reducing consumption of sugar-sweetened beverages. Our goal was to assess the feasibility, acceptability and efficacy of these approaches in preventing toddler overweight.
Study population and setting
Expectant mothers and their families were recruited from three AI tribes who are members of the Northwest Portland Area Indian Health Board (NPAIHB). The NPAIHB is within the Portland Area Indian Health Service (IHS) cluster (Idaho, Oregon, and Washington). Tribes were divided into two groups: tribe A received community-wide interventions only; tribes B&C received community-wide interventions with family-based components. We did not recruit an active control group. Instead, we used a separate sample pretest-posttest design, also known as simulated before and after design.9 In this design, two equivalent groups are identified, one sample (the pre-test sample) is measured before the intervention and a different (but equivalent) sample (post-test sample) is measured after the intervention. In our case the “pre-test sample” was a cohort of AI/AN children born 2 years earlier in the same tribes, and whose data was collected as part of the Centers for Disease Control and Prevention’s Pediatric and Nutrition Surveillance System (PedNSS). This pre-test sample gave us the baseline prevailing levels of overweight in the participating tribes.
The Portland Area IHS Institutional Review Board approved the study. In addition to parental informed consent, each tribe gave permission for researchers to conduct the study and access the PedNSS longitudinal data. Anonymity of the participating tribes is retained as per their request.
Intervention design
Intervention Goals were to: 1) increase breastfeeding initiation and duration; 2) limit the introduction of sugar-sweetened beverages to infants and toddlers; and, 3) promote the consumption of water for thirst among toddlers. Interventions were informed by focus groups and interviews conducted at the beginning of the project.
Community-wide interventions were designed in six-month cycles, using five strategies: a) raising awareness b) providing health education c) facilitating individual behavior change, d) augmenting public health practice and e) modifying environments and/or policies related to breastfeeding, sugar-sweetened beverages and water consumption. A sample intervention plan targeting sugar-sweetened beverages is shown in appendix 1 (supplemental materials). Most interventions were media-based, taking the form of brochures, videos, newspaper articles, flyers, or other media.
Family Interventions were delivered in eight-visit clusters by community health workers (CHWs) using a home-visiting model. 10, 11 Each visit cluster could have up to 3 distinct contacts, and only one of these was required to be a face-to-face contact; the other two could be conducted by phone. This visit structure means that participants could receive 7–21 visits during the time they were on the study. The structure was necessary to introduce flexibility into the visits and to allow tailoring of the intervention to specific needs of participating families. As an example, a mother experiencing difficulties establishing lactation may need more than a single contact during the first week or two after the baby is born, while those establishing lactation easily would not need more than one contact in the early weeks of the baby’s life.
The first 2 visit clusters were intended to establish rapport, solidify contact guidelines between participants and their assigned CHWs, and collect baseline data. CHWs created a client-specific plan for initiating and maintaining breastfeeding along with water and sugar-sweetened beverage interventions in cluster 1–3. Clusters 4–7 consisted of intervention implementation and monitoring, while the final cluster covered closure activities.
Cluster 1 occurred before the baby’s birth, to facilitate counseling that would encourage early decisions to breastfeed. Clusters 2–4 occurred within 0–3 months of the baby’s birth, while the remaining visits were spread out over the rest of the project period. The interval between visit clusters, or contacts within a cluster, was timed to match the age of the baby, individual family’s needs and the workload of individual CHW. CHWs received training in the delivery of one-to-one counseling to reduce sugar-sweetened beverage consumption and promote water consumption, using principles of home visiting and outreach,10, 11 behavior change12 and motivational enhancement.13, 14
Measurements
Community-wide interventions were tracked monthly, with each tribe logging completed interventions and comparing them to planned Interventions. Plans judged to be complete, or those that were not very well received (as subjectively determined by project staff), were replaced with new plans at the 6-month point.
Family interventions were tracked and recorded separately within each cluster for each family. Visit forms used for this purpose contained information needed to facilitate counseling (visit date, content discussions, referrals, etc).
Breastfeeding status was defined as any form of breastfeeding including full, partial or complementary breastfeeding, as defined by the World Health Organization (WHO).15 Breastfeeding status was obtained from the Women, Infants, and Children (WIC) and from Maternal and Child Health (MCH) clinic charts, and confirmed through direct interviews at 6, 12, 18, and 24 months. PedNSS data was not used to determine breastfeeding for the PedNSS “pretest” sample, since this dataset did not contain information on timing of breastfeeding cessation.
Confidence to implement study goals was an aspect of acceptability of the intervention. It was assessed by asking parents/guardians to indicate their confidence and rate the usefulness of TOTS in helping them achieve these goals. Parents/guardians rated statements such as “I am sure I can serve water as the main beverage during meals” by using a 5-point scale anchored at the lower end (1) with “strongly disagree” and the upper end with “strongly agree” (5), with a score of 3 being neutral. We calculated the percentage of participants with a score of 4 or higher and those with a score of 2 or lower, to assess acceptance and implementation of the goals by participants.
Weight, height/length of lightly clothed children were collected as part of routine WIC or MCH clinic visits every six months by trained staff using calibrated scales and infantometers /toddler stadiometers. Measurement training for WIC and MCH staff at each site was provided by WIC trainers before the start of the study to ensure standardized measurements across all sites. Length/height measurements shifted from recumbent length to standing height at the first visit after the child’s second birthday.
Statistical methods
The analysis of anthropometric outcomes focused on changes in z-scores (for age) of BMI, weight, and height, from birth to 24 months. Due to the disparity of z-score distributions between tribes, an adjustment was made using the PedNSS data from the two-year period preceding the intervention study. Each study child was paired with a PedNSS child from the same community, matched by gender, calendar birth month (to correct for seasonal growth effects), and age at the 18–24-month measurement point. The purpose of this procedure was to construct a sample in which birth-to-24-month changes represented the community-specific growth patterns in the absence of any intervention. The use of z-scores partially adjusts for different ages in addition to the age-adjustment inherent in the process of matching to PedNSS data.
The analytic model was:
where ΔY represents a change from baseline in the outcome variable (such as weight-for-age z-score), T is an indicator of being the TOTS study group as opposed to being in the PedNSS sample (T=1 for TOTS, T=0 for PedNSS), B and C are indicators of communities B and C, and W is birth weight z-score. The “error” term is taken to be uncorrelated with the explanatory factors, as a matter of definition of the regression model. The interpretation of the parameters is as follows: β1 = effect of the TOTS study in the control (A) site; β2 = difference between site B and site A prior to the TOTS study; β3 = difference between site C and site A prior to the TOTS study; β4 = effect of the TOTS study on site B, relative to the effect of the TOTS study on site A; β5 = effect of the TOTS study on site C relative to the effect of the TOTS study on site A. All of these effects are adjusted for birth weight. For additional clarity, the meanings of the model effects are shown in tabular form in Table 1.
Table 1.
Effect Variables (T, B, C, TB, TC) and Parameters (β‘s) in the Analytic Model
| A (Community intervention only) |
B (Community + family intervention) |
C (Community + family intervention) |
|
|---|---|---|---|
| Site-level Control (PedNSS) 2 years before TOTS |
β0 (reference) | B β0 + β2 |
C β0 + β3 |
| TOTS Project | T β0 + β1 |
T + B + TB β0 + β1 + β2 + β4 |
T + C + TC β0 + β1 + β3 + β5 |
β0 = effect present at all sites; β1 = secular effect on site A; β2 = difference of site B from site A, 2 years before TOTS; β3 = difference of site C from site A, 2 years before TOTS; β4 = TOTS effect on site B, relative to the secular effect at the control site A; β5 = TOTS effect on site C, relative to the secular effect at the control site A
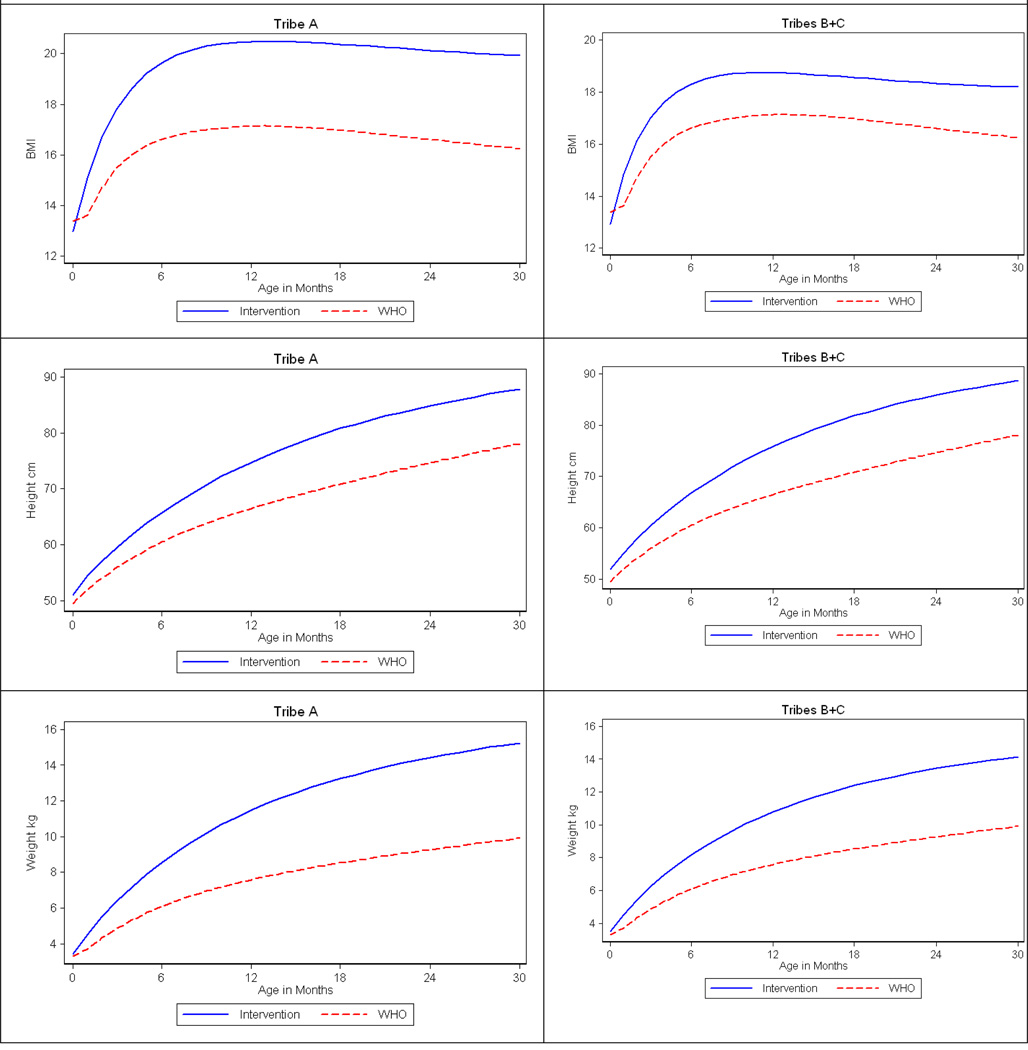
Growth curve of the form α + β (1-exp (-r*age)) was fitted to each study child, based on longitudinal measurements taken every six months, to assess growth trajectory. The fitted curves were used to provide values on a monthly grid, and these were then averaged every month. A comparison curve was generated from the WHO normative data, matched for gender. No inference was performed for these data, which were generated primarily to illuminate the primary analysis. All analyses were performed in STATA (Version 9 College Station TX).
Results
Baseline population characteristics
Table 2. shows characteristics of the study population and the PedNSS cohort.
Table 2.
Baseline population characteristics
| tribe A | tribe B | tribe C | All tribes combined | |
|---|---|---|---|---|
| Study Cohort | ||||
| Number born during recruitment year | 90 | 67 | 115 | 272 |
| Number enrolled in the study | 63 | 62 | 80 | 205 |
| Number completing study | 53 | 56 | 69 | 178 |
| Maternal/Guardian age (range) | 25.0 (17–38) | 25.6 (17–41) | 24.8 (15–39) | 25.0±5.8 |
| Average Birth Weight (kg) | 3.30±0.68 | 3.41±0.58 | 3.28±0.4.8 | 3.28±0.57 |
| Average Birth Length (cm) | 50.8±3.4 | 52.8±2.9 | 50.7±2.5 | 51.4±3.1 |
| Average Birth BMI | 12.7±1.7 | 12.2±1.5 | 12.2±1.6 | 12.3±1.6 |
| Comparison Cohort (PedNSS 2 yrs earlier) | ||||
| Number matched to study cohort | 63 | 62 | 80 | 205 |
| Maternal/Guardian age | N/A | N/A | N/A | N/A |
| Average Birth Weight (kg) | 3.46±0.65 | 3.61±0.51 | 3.34±0.50 | 3.46±0.56 |
| Average Birth Length (cm) | 50.4±3.3 | 52.9±2.3 | 50.9±2.9 | 51.3±3.0 |
| Average Birth BMI | 13.6±2.0 | 12.9±1.2 | 12.9±1.4 | 13.1±1.6 |
PedNSS=Pediatric Nutrition Surveillance System4
This information was not available for the PedNSS population
We enrolled 75% of all children born during the recruitment year and collected final measurements on 86% (64.5% of complete annual cohort) of enrolled children. Reasons for dropping out included: moving (6% of families); loss of interest in project (6% of families); and change in child custody (2% of the children).
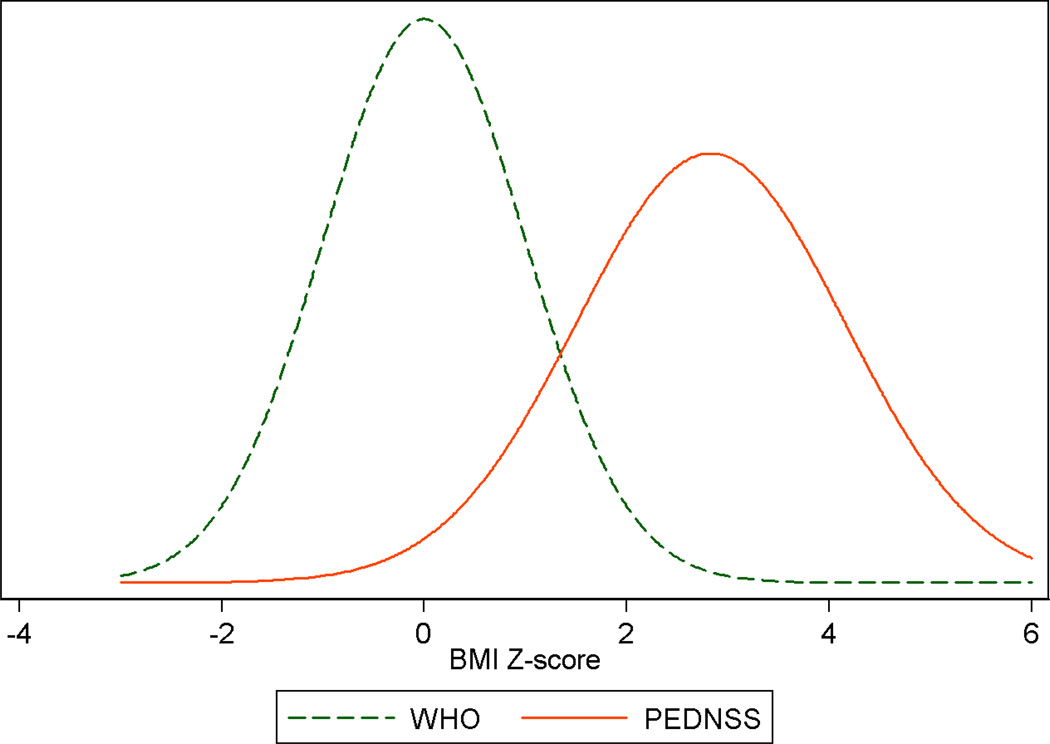
Figure 1 shows the distribution of BMI Z-scores among PedNSS children compared to WHO normative data, and is an indication of the prevailing levels of overweight in the communities studied prior to the TOTS intervention. The average BMI Z-score of the PedNSS group was 1.70. The majority (72%) of the PedNSS cohort had BMI Z-scores one standard deviation above the WHO distribution, and 39% had BMIs two standard deviations above the WHO children.
Figure 1.
PedNSSa BMI Z-Score distribution in 24-month old children a study initiation compared to WHOb standards
aPedNSS=Pediatric Nutrition Surveillance System4.
bWHO=World Health Organization
Community-intervention plan completion and home-visit completion rates
Community-wide interventions executed and home-visit completion rates are shown in Table 3. Breastfeeding interventions were comparable across all tribes. Completion of sugar-sweetened beverage and water interventions was lower in tribe A than in tribes B&C.
Table 3.
Community plans executed and home visits completed by tribe at the end of intervention
| tribe A | tribe B | tribe C | Total | |
|---|---|---|---|---|
| Community Interventions executed: | ||||
| Breastfeeding | 24 | 23 | 20 | 22.3 |
| Sugar-sweetened beverage | 10 | 18 | 14 | 14.0 |
| Water | 14 | 31 | 32 | 25.7 |
| Home visits: | ||||
| Average number of visits | N/A | 4.9 | 8.2 | 6.8 |
| % completing 7 clusters | N/A | 18% | 54% | 38% |
| % completing 4–6 clusters | N/A | 55% | 30% | 41% |
| % completing 3 clusters or less | N/A | 27% | 16% | 21% |
The majority of families (79%) in tribes B&C received at least 4 cluster visits. Significantly more families in tribe C received the full complement of visits compared to tribe B. Debriefing interviews with community coordinators and CHWs indicated that the additional visits in tribe C were to assist with breastfeeding.
Breastfeeding
Tribal PedNSS records did not contain the time of breastfeeding termination, making it difficult to estimate breastfeeding duration. So we compared the TOTS breastfeeding rates to the national PedNSS data for American Indian mothers. Compared to the national PedNSS sample of AI/AN , breastfeeding initiation and 6-month rates were 14 and 15 percentage points higher, respectively, at the conclusion of TOTS (Table 4).
Table 4.
Breastfeeding initiation and duration of participating tribes during the intervention, compared to national AI breastfeeding rates
| Breastfeeding | tribe A | tribe B | tribe C | Total | National AI rates* |
|---|---|---|---|---|---|
| Initiation | 72% | 86% | 63% | 74% | 60% |
| 6-months | 49% | 48% | 18% | 38% | 23% |
| 12-months | 19% | 23% | 9% | 17% | 17% |
| 18-months | 10% | 5% | 5% | 7% | N/A |
| 24 months | 6% | 3% | 2% | 4% | N/A |
Average of rates reported by CDC (PedNSS) for years 2003–2005
Sugar-sweetened beverage consumption
Sugar-sweetened beverage and water consumption were assessed retrospectively, by asking parents to indicate their confidence in implementing the study recommendations for their children and families, and to indicate the usefulness of the project in helping them change targeted behaviors. Parents expressed high confidence (a score of 4 or above on a 5-point scale) in their abilities to implement the recommendations of the study (Table 4). All interventions except breastfeeding were given a score of 4 or higher by 60% of the participants, indicating confidence in the usefulness of TOTS in implementing target behaviors.
Environmental, public health practice, and policy changes
Breastfeeding policy changes included: 1) hospitals becoming more “baby friendly” 14 (allowing co-rooming, increasing access to lactation counseling, eliminating free formula sample packs); and 2) tribal employers allowing longer breaks for mothers returning to work to pump breast milk. Beverage-related policy included 1) placing water vending machines next to soda vending machines 2) passing tribal resolutions to not purchase sugar-sweetened beverages with tribal government dollars; 3) replacing sugar-sweetened beverages with water at events where children are present; and 4) subsidizing cost of providing water in tribal health facilities.
Anthropometric measures
Mean and standard deviations of the 24-month anthropometric measures, including PedNSS values, are shown in Table 6a. BMI Z-score decreased by 0.75 in tribes B and C (p=0.016) combined and ; there was not an appreciable difference in BMI Z scores between these two tribes. Height and weight were not statistically different between the three tribes (Table 6b.).
Table 6.
| a. 24-montha BMI, weight and height-for-age Z-scores | ||||
|---|---|---|---|---|
| tribe A N pairs=53 |
tribe B N pairs=56 |
tribe C N pairs=68 |
Total B+C N pairs=124 |
|
| BMI for age Z-scores | ||||
| Study populations | 2.69 (1.06) | 1.41 (1.57) | 2.00 (1.44) | 1.73 (1.52) |
| PedNSS (comparisons) | 1.96 (1.47) | 1.35 (1.26) | 1.74 (1.18) | 1.56 (1.23) |
| Weight for age Z-score | ||||
| Study populations | 1.74 (0.83) | 1.15 (1.28) | 1.22 (1.25) | 1.19 (1.26) |
| PedNSS (comparisons) | 1.38 (0.90) | 1.09 (1.18) | 1.06 (1.16) | 1.07 (1.17) |
| Height for age Z-score | ||||
| Study populations | −0.34 (1.45) | 0.21 (1.40) | −0.38 (1.12) | 0.12 (128) |
| PedNSS (comparisons) | −0.08 (1.42) | 0.20 (1.10) | −0.28 (1.27) | −0.07 (1.22) |
| b. Intervention effects on changes in anthropometric measures from birth to 24 months | ||||
|---|---|---|---|---|
| tribe A N pairs=53 |
tribe B N pairs=56 |
tribe C N pairs=68 |
Total B+C N pairs=124 |
|
| BMI for age Z-score | ||||
| Change from 0–24 mos—Study populations | 2.92 (1.82) | 1.86 (1.72) | 2.44 (1.84) | 2.18 (1.80) |
| Change from 0–24 mos—PedNSS (comparison) | 2.03 (2.22) | 1.74 (1.46) | 2.23 (1.52) | 2.01 (1.50) |
| Intervention Effecta | -0.81, p=0.025 | -0.70, p=.036 | -0.75, p=.016 | |
| Weight for age Z-score | ||||
| Change from 0–24 mos—Study populations | 1.57 (1.64) | 0.52 (1.35) | 1.20 (1.50) | 0.89 (1.46) |
| Change from 0–24 mos—PedNSS (comparison) | 1.22 (1.75) | 0.41 (1.23) | 1.01 (1.19) | 0.75 (1.24) |
| Intervention Effect | -0.29, p=.167 | -0.20, p=.242 | -0.24, p=.173 | |
| Height for age Z-score | ||||
| Change from 0–24 mos—Study populations | −0.90 (1.81) | −1.59 (1.67) | −0.97 (1.52) | −1.25 (1.61) |
| Change from 0–24 mos—PedNSS (comparison) | −0.43 (2.37) | −1.62 (1.42) | −1.01 (1.42) | −1.27 (1.45) |
| Intervention Effect | 0.28, p=.798 | 0.17, p= .700 | 0.23, p=.781 | |
All p-values are one-sided, to detect a decrease in BMI in tribes receiving the community+family intervention relative to the tribe receiving only the community intervention.
Change from birth to 24m, compared to tribe A, adjusted for PedNSS data as described in the text, and adjusted for baseline values
Figure 2 shows patterns of growth from birth to 18–24 months for tribe A alone, and for tribes B and C combined, and compares these patterns to a WHO reference population for BMI, height/length, and weight. AI children appear to grow faster than the WHO reference children, gaining more weight, height, and BMI over the first 6–9 months of life. After this initial difference in growth rates, trajectories appear to be similar, with tribes B&C resembling the WHO trajectories more closely than tribe A. These growth curves show no interruption of linear growth as a consequence of the intervention. The higher BMIs in AI children appear to be the result of very rapid weight gain in the first 6–9 months of life.
Figure 2.
Growth patterns comparing TOTS children to WHO standards for A and B+C tribes
Discussion
Child overweight and obesity will likely decrease the quality of life and raise national health-care costs as these children enter adulthood.15 Growth within the first year, and possibly the first months, of life may predict adolescent and adult obesity. 16 Interventions that limit early increases in adiposity, and establish healthful behavior patterns that persist in later childhood, may prevent the likelihood of adult obesity and its attendant consequences.
The purpose of this study was to test the feasibility of an intervention to prevent obesity, and to obtain preliminary efficacy data of such an intervention in preventing child overweight beginning at birth. Growth data collected in AI/AN children prior to the initiation of this project suggested birth as a logical time to institute prevention efforts, since obesity was established early and did not reverse itself in late toddlerhood and pre-school years.
Our results show that the community-based intervention targeting breastfeeding and sugar-sweetened beverage consumption to prevent toddler overweight, is feasible. We recruited 75% of children born in participating tribes during the year-long recruitment period. Retention and participation rates were high, with 86% of families recruited providing anthropometric data for their children at the end of the study. We attribute the high participation rates to a strong collaboration during the formative phase, where we consulted with tribes in honing the intervention, data collection, and implementation logistics. The resulting design integrated the study into existing MCH clinic visits, and created a peer-counseling model that tailored the intervention to family needs and availability. Our results also show that a home- visiting program is a feasible intervention approach in tribal communities, as the majority of participants received more than half the planned home visits.
Process measures show that tribes created effective community plans, as well as policy and environmental changes, to increase breastfeeding and curtail consumption of sugar-sweetened beverages by infants and toddlers. This study began before the national attention to sugar-sweetened beverage consumption that has occurred in recent years.17 It is therefore unlikely that the changes we report here are due to secular trends in sugar-sweetened beverage consumption. Nevertheless, it is difficult to fully assess the impact of these community initiatives on behaviors and practices that affect child BMI. As an example, our study did not have a pure control tribe (a tribe that received no community or family intervention). Such a design would have allowed us to assess the effect of the community-wide intervention alone, as well as assess whether the observed changes were due to secular changes. Similarly, a design that included a tribe receiving the family intervention alone would have allowed us to assess the separate impact of the family intervention. Despite these limitations, this study demonstrates that these community-based initiatives are feasible and acceptable to AI tribes.
Our results show that a combination of two relatively simple interventions (increasing breastfeeding and curtailing consumption of sugar-sweetened beverages in favor of water) results in an attenuated community-level increase in child BMIs at 18–24 months in tribes receiving both a community-wide and an individualized family intervention. The lower BMIs were achieved without a detectable effect on linear growth, as the increase in height/length was similar in all tribes.
We are aware of only one other study that has explored prevention of overweight in children beginning at birth. Costom and Shore18 provided individualized feeding counseling that tailored the advice to the growth patterns of 182 infants. The authors concluded that individualized counseling is more effective that a one-size-fits-all counseling program in preventing excess adiposity.18 Our study differs from that of Costom and Shore in focusing on specific approaches to preventing overweight (breastfeeding and curtailment of sugar-sweetened beverages), but is similar in its customization of the intervention to the needs of the communities and families.
BMI ‘s were lower in tribes receiving community plus family interventions, but still higher than those of children in the PedNSS sample two years earlier. This outcome may be due to a number of factors. Toddler overweight has many contributing factors. It is possible that a more comprehensive intervention incorporating other aspects of feeding (delay of complementary foods, introducing healthier food choices, etc) and/or physical activity (reducing sedentary activities, facilitating natural play, etc.) would have slowed BMI escalation more profoundly.
There were fewer than the expected number of community interventions completed in the tribe receiving the community intervention only, and the average number of home visits differed between the two tribes that received home visits. This “dilution” of the intervention may explain the less-than-expected moderation of BMI increase. It is more likely, however, that the BMI increase is a reflection of a secular trend towards increased BMIs during the study period. Although we did not have a pure control tribe in which to track secular trends, national trends show that the percent of AI/AN children 2 years or younger defined as overweight (weight for length ≥95th percentile) rose from 17.2% to 18.4% during the time TOTS was underway.
We have assumed that the change in BMI at 18–24 months was mediated by changes in breastfeeding and sugar-sweetened beverage consumption. It is possible, however, that parents made other changes that we did not track, since we did not collect quantitative measures of sugar-sweetened beverage consumption, nor did we directly observe changes in these intervention components. As an example, reliable baseline breastfeeding initiation and duration data were not available. Our estimation of change is based on comparing post-study data to national data. Thus it is not possible to gauge whether the higher breastfeeding initiation and duration rates, compared to a national sample, were causally related to the outcomes However, policy shifts were documented (e.g increased support of breastfeeding mothers at worksites), making it plausible that some improvement may have been due to the project-related activities to promote breastfeeding. Similarly, parents indicated that their confidence in implementing recommended changes had increased at the time of the exit interview. Stronger measures of change in mediating variables may be needed in future to better understand which factors have the greatest impact on children’s BMIs.
Conclusion
This pilot study demonstrates that interventions to prevent excess adiposity in infants and toddlers are both feasible and acceptable to the AI/AN tribes. Our results suggest that simple interventions may slow down trends in escalating overweight and obesity in children. Comprehensive studies in diverse populations, and more rigorous assessments, are needed to further understand and hone approaches to prevent BMI escalation in children.
Table 5.
Percent of participants expressing confidence* and usefulness* of the TOTS study in assisting with target behavior change
| tribe A | tribe B | tribe C | Total | |
|---|---|---|---|---|
| A. Confidence in implementing recommendations | ||||
| Breastfeeding | 64 | 54 | 56 | 57 |
| Limiting Sugar-sweetened beverages for the family | 93 | 92 | 71 | 82 |
| Serving water as the primary beverage at meal times | 89 | 80 | 73 | 79 |
| Serving water when family members are thirsty | 73 | 48 | 63 | 62 |
| B. Usefulness of the TOTS study in helping change targeted behaviors | ||||
| Breastfeeding | 40 | 65 | 43 | 49 |
| Help family drink more water | 96 | 92 | 81 | 90 |
| Help family drink fewer sugar-sweetened beverages | 88 | 89 | 80 | 86 |
A score of 4.0 or higher on a 5-point scale
Acknowledgements
This work was supported by: NIH Grants # 1S056M64122, 1S066M074086 and U01 HL081624.
Abbreviations
- BMI
Body Mass Index
- PedNSS
Pediatric Nutrition Surveillance System
- WHO
World Health Organization
- IHS
Indian Health Service
Appendix
Appendix table 1.
Sample community intervention plan targeting reduction of sugar-sweetened beverages and breastfeeding:
| Item: Sugar-sweetened- beverage |
||||
|---|---|---|---|---|
| Approach | Action # | Action | Collaborators | Issues to be Addressed |
|
Level of Intervention |
What is to be done | People Involved |
(Choose the one that fits your intervention) |
|
| Awareness | 1 | Provide American Indian specific media messages that highlight health risks associated with drinking sugar-sweetened-beverage. Encourage drinking water as a cultural value (media delivery through newspaper articles, public access TV, posters & brochures). |
Site Coordinator |
|
| Project Director | ||||
| Local newspaper editor | ||||
| Awareness | 2 | Draft video interview/script about the merits of drinking water and not pop to use for public service announcement. |
Site Coordinator | |
| Project Director | ||||
| Environment | 3 | Propose policy to Tribal Business Council that prohibits the use of tribal purchase orders or dollars to purchase sugar-sweetened-beverages for community events |
Site Coordinator | |
| Health Director | ||||
| Tribal business council | ||||
| Behavior Change |
4 | Replace sugar-sweetened beverages with water coolers or dispensers (or milk and 100% juice) at youth and community events. |
Site Coordinator | |
| Cook | ||||
| Behavior Change |
5 | Make sure water is provided as a selection in all soda vending machine sites throughout the community |
Site Coordinator | |
| Facility managers | ||||
| Health Education |
6 | Provide TOTS bibs to TOTS mothers and give information about withholding sugar-sweetened beverages from babies and encourage appropriate 100% juice, milk and water. |
Site Coordinator | |
| Project Director | ||||
| WIC | ||||
| Environment | 7 | Research strategies (policy, resolution, revenue replacement) to remove pop machines from community center and neighborhood facilities and replace them with water or non-sugar-sweetened beverages. |
Site Coordinator | |
| Health Director | ||||
| Awareness | 1 | Provide American Indian specific media messages that promote breast-feeding. Encourage breastfeeding as a cultural value (media delivery through newspaper articles, public access TV, posters & brochures). |
Site Coordinator |
|
| Local newspaper editor | ||||
| Health Education |
2 | Construct and Distribute a laminated magnet that provides phone number of resources for assistance with breastfeeding continuation. |
Site coordinator | |
| Behavior Change |
3 | Display “Breastfeeding Accomplishment “ board of moms who have breastfed |
Site Coordinator | |
| MCH clinics | ||||
| Health Education |
4 | Distribute key chains that provide basic information on breastfeeding |
Site Coordinator | |
| MCH clinics | ||||
| Health Education |
5 | Work with administration to provide a breastfeeding room for moms who are visiting or working at the tribal health offices. |
Site Coordinator | |
| Administration | ||||
| Public Health Nurse | ||||
| Behavior Change |
6 | Connect expectant moms with other moms who have been successful at breastfeeding and moms who have breastfed and gone back to work (during third trimester). |
Site Coordinator | |
| CHW | ||||
Footnotes
We are grateful to the tribal governments of the following communities for supporting this work: the Shoshone Bannock Tribes, the Nez Perce Tribe and the Lummi Nation. The following staff assisted the study team and provided advice on ways to implement the study in their communities: Shoshone Bannock Tribes: Not-So Gah-Nee Health Center: Angela Mendez, Tribal Health Director, Tamara Hollinger, Site Supervisor, Theresa Bache, TOTS Site Coordinator, Julie Kutch, CHW. Nez Perce Tribe: Nimiipuu Tribal Health Center: Karen Carter, Health Director, Julie Keller, Site Supervisor, Lara Munden, TOTS Site Coordinator, Andy Albert, CHW. Lummi Nation: Lummi Tribal Health Center: Barbara Finkbonner, Health Director& Site Supervisor, Ardith Tom, TOTS Site Coordinator.
Literature cited
- 1.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288:1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 2.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM, et al. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 3.Zephier E, Himes JH, Story M. Prevalence of overweight and obesity in American Indian school children and adolescents in the Aberdeen area: a population study. Int J Obes Relat Metab Disord. 1999;23(Suppl 2):S28–S30. doi: 10.1038/sj.ijo.0800856. [DOI] [PubMed] [Google Scholar]
- 4.Lindsay RS, Cook V, Hanson RL, Salbe AD, Tataranni A, Knowler WC, et al. Early excess weight gain of children in the Pima Indian population. Pediatrics. 2002;109:E33. doi: 10.1542/peds.109.2.e33. [DOI] [PubMed] [Google Scholar]
- 5.Touger L, Looker HC, Krakoff J, Lindsay RS, Cook V, Knowler WC. Early growth in offspring of diabetic mothers. Diabetes Care. 2005;28:585–589. doi: 10.2337/diacare.28.3.585. [DOI] [PubMed] [Google Scholar]
- 6.Polhamus B, Dalenius K, Borland E, Smith B, Grummer-Strawn L. Pediatric Nutrition Surveillance 2006 Report. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. [Google Scholar]
- 7.Owen CG, Martin RM, Whincup PH, Davey-Smith G, Gillman MW, Cook DG. The effect of breastfeeding on mean body mass index throughout life: a quantitative review of published and unpublished observational evidence. Am J Clin Nutr. 2005;82:1298–1307. doi: 10.1093/ajcn/82.6.1298. [DOI] [PubMed] [Google Scholar]
- 8.Nelson JA, Carpenter K, Chiasson MA. Diet, activity, and overweight among preschool-age children enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Prev Chronic Dis. 2006;3:A49. Epub. [PMC free article] [PubMed] [Google Scholar]
- 9.Campbell DT, Stanley JC. Experimental and Quasi-Experimental Designs for Research. Chicago: Rand McNally College Publishing Company; 1963. [Google Scholar]
- 10.Wasik BH, Bryant DM. Home visiting: Procedures for helping families. Thousand Oaks, CA: Sage publications; 2001. [Google Scholar]
- 11.Crane B, Dean C. Empowerment skills for family workers: The comprehensive curriculum of the New York State family development credential, trainer’s manual. Ithaca, NY: Cornell Empowering Families Project; 1999. [Google Scholar]
- 12.Miltenberger RG. Behavior modification: Principles and procedures. 4th Ed. Pacific Grove, CA: Thomson/Wadsworth publishing; 2008. [Google Scholar]
- 13.Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd ed. New York, NY: Guilford Press; 2002. [Google Scholar]
- 14.DiClemente CC, Velasquez MW. Motivational Interviewing and the Stages of Change. In: Miller WR, Rollnick S, editors. Motivational interviewing: Preparing people for change. 2nd ed. New York, NY: Guilford Press; 2002. pp. 217–250. [Google Scholar]
- 15.World Health Organization. Conclusions of a consensus meeting held 6–8 November 2007. Washington, DC, USA: Indicators for Assessing Infant and Young Child Feeding Practices. Part 1, Definitions. [Google Scholar]
- 16.Perez-Escamilla R, Segura-Milla S, Pollitt E, Dewey KG. Effect of the maternity ward system on the lactation success of low-income urban Mexican women. Early Hum Dev. 1992;31:25–40. doi: 10.1016/0378-3782(92)90012-6. [DOI] [PubMed] [Google Scholar]
- 17.Ludwig DS. Childhood obesity--the shape of things to come. N Engl J Med. 2007;357:2325–2327. doi: 10.1056/NEJMp0706538. [DOI] [PubMed] [Google Scholar]
- 18.Stettler N, Zemel BS, Kumanyika S, Stallings VA. Infant weight gain and childhood overweight status in a multicenter, cohort study. Pediatrics. 109:194–199. doi: 10.1542/peds.109.2.194. [DOI] [PubMed] [Google Scholar]
- 19.Suarez-Balcazar Y, Redmond L, Kouba J, Hellwig M, Davis R, Martinez LI, Jones L. Introducing systems change in the schools: the case of school luncheons and vending machines. Am J Community Psychol. 2007;39:335–345. doi: 10.1007/s10464-007-9102-7. [DOI] [PubMed] [Google Scholar]
- 20.Costom BH, Shore D. Effect of a comprehensive nutritional program on the growth and ponderosity of infants. Clin Pediatr (Phila) 1983;22:105–111. doi: 10.1177/000992288302200204. [DOI] [PubMed] [Google Scholar]