Abstract
Declarative Title
Current research about tooth whitening shows that it is safe and effective when manufacturer’s protocol is followed, yet there are risks of which the profession and users should be aware.
This update provides a summary of current research and assessment of the safety and efficacy of tooth whitening regimens.
Background
Tooth whitening has become one of the most frequently requested dental procedures by the public. The public has come to demand whiter, more perfect smiles and in response many choices for tooth whitening have been made available. These include home-based products such as toothpastes, gels, and films, as well as in-office based systems where products containing highly concentrated bleaching agents are applied under professional supervision. The profession and public have been aware of certain risks related to tooth whitening such as increased tooth sensitivity and gingival irritation. New research has shown that there are other risks such as tooth surface roughening and softening, increased potential for demineralization, degradation of dental restorations, and unacceptable color change of dental restorations. The new research is also focused on optimizing whitening procedures to reduce tooth sensitivity and to increase the persistence of the whitening.
Methods
Current reports in the literature are reviewed that are related to the use of peroxide based whitening methods. These reports include in vitro studies for method optimization and mechanism as well as clinical studies on effects of various whitening regimens.
Conclusions
When manufacturer’s instructions are followed, hydrogen peroxide and carbamide peroxide based tooth whitening is safe and effective. Patients should be informed of the risks associated with tooth whitening and instructed on identification of adverse occurrences so that they may seek professional help asneeded.
Introduction
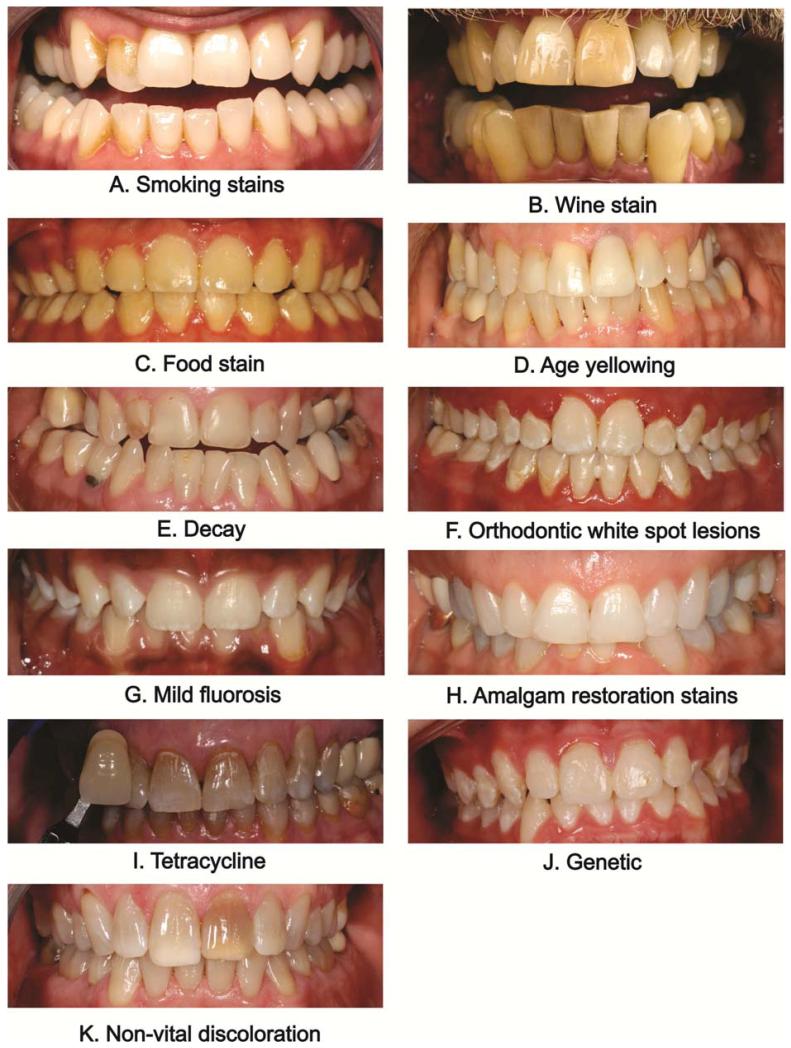
The public has been influenced by the portrayal of perfect white smiles in the media. . The color quality of television, movies, electronic and print media has raised self-awareness of discolored teeth. In the late 1980’s several companies introduced both home-based products and professionally applied tooth whitening products into the U.S. marketplace. These have gained popularity with the public who has come to demand whiter, more perfect smiles.1 There are several different methods for whitening teeth, each with their own mechanism of action. The efficacy of these different methods is dependent upon the particular tooth discoloration that is being treated. Causes of tooth discoloration can be categorized into two main groups: intrinsic and extrinsic staining (see Fig. 1). Intrinsic staining, sometimes called internal staining, can be attributed to factors such as genetics, age (from enamel wear over time exposing yellower dentin), antibiotics, high levels of fluoride, and developmental disorders and can start before the tooth has erupted. After eruption of the tooth some dental restorations can cause tooth staining. Extrinsic staining, sometimes called external staining, is largely due to environmental factors including smoking,pigments in beverages and foods, antibiotics, and metals such as iron or copper. Colored compounds from these sources are adsorbed into acquired dental pellicle or directly onto the surface of the tooth causing a stain to appear. See Fig. 1 for examples of the staining from these sources.
Figure 1.
Examples of tooth staining. Extrinsic staining examples: A. Smoking; B. Wine stain; and C. Food stain. Intrinsic staining examples: D. Age yellowing; E. Decay; F. Orthodontic white spot lesion; G. Mild fluorosis; H. Amalgam restoration; I. Tetracycline stain; J. Genetic (amelogenesis imperfecta); K. and Non-vital coloring.
Whitening chemistry
Tooth whitening is any process that lightens the color of a tooth. Whitening may be accomplished by physical removal of the stain or a chemical reaction to lighten the tooth color. Bleaching is defined here as the chemical degradation of the chromogens. The active ingredient in most whitening products is hydrogen peroxide (H2O2) which is delivered as hydrogen peroxide or carbamide peroxide. Carbamide peroxide is a stable complex that breaks down in contact with water to release hydrogen peroxide. Because carbamide peroxide releases hydrogen peroxide the chemistry of most tooth whitening is that of hydrogen peroxide.
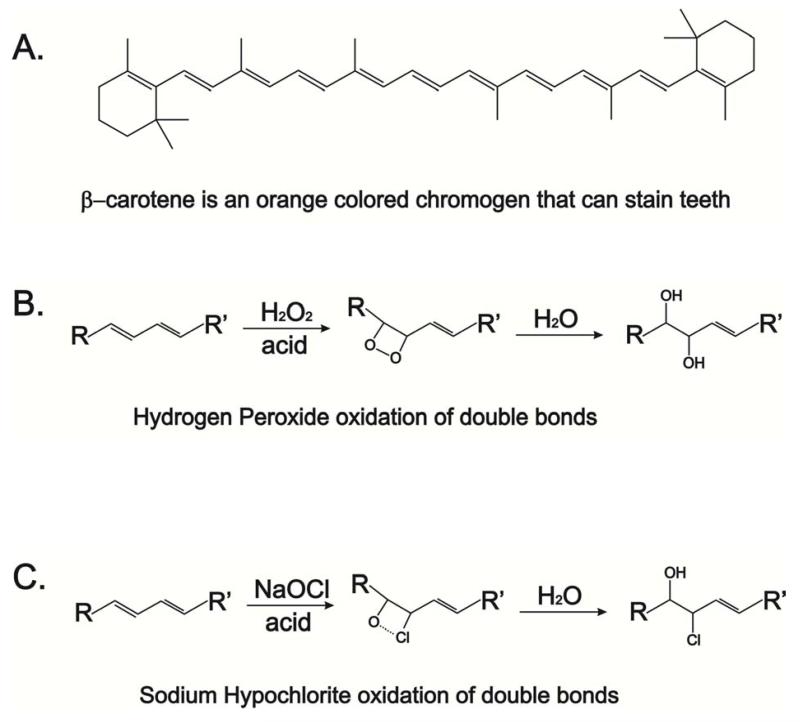
Tooth stains consist of compounds that have color or darker shades called chromogens that are accumulated in the tooth (intrinsic) or on the tooth (extrinsic). Chromogens fall into two categories: large organic compounds that have conjugated double bonds in their chemical structure as shown in Fig 2a; and metal containing compounds. Bleaching of the organic compounds by hydrogen peroxide involves reacting with the double bonds to oxidize the double bond as shown in Fig 2b. This causes the chromogen to become a lighter colored compound. Bleaching of the metallic compounds is much more difficult; better esthetic options may be veneers, bonding, or crowns. There are some professional products that contain sodium hypochlorite (NaOCl) which reacts with the double bonds of the chromogen in much the same way as peroxide as shown in Fig 2c.
Figure 2.
Chemistry of chromogen bleaching. A. β-carotene is an example of an organic chromogen with many conjugated double bonds; B. Chemical reaction of hydrogen peroxide with a chromogen double bond; and C. Chemical reaction of sodium hypochlorite with a chromogen double bond.
Different product types are marketed to address the particular stain to be removed. The broad categories include: cleansers such as smokers’ toothpastes which contain larger amounts of detergents and abrasives to aid in the removal of chromogens from the tooth surfaces; bleaches to react with the chromogens to lighten color; and products that have both increased cleansing and bleaching. More severe or complex stains are best lightened professionally, while over-the-counter products can be used for milder cases. The treatment time required for reaching the tooth whitening end point is dependent on the time of exposure and the concentration of bleaching compound. This end point is dependent on the type of whitening employed, usually 1 to 2 shades for cleansers and over-the-counter (OTC) gels, and more for professionally applied products.
Types of Teeth Whitening Systems
Whitening systems can be variously categorized. The following approach is in accordance with the American Academy of Cosmetic Dentistry.2
Whitening Toothpastes
Whitening toothpastes typically contain higher amounts of abrasives and detergents than standard toothpastes, to remove tougher stains. Whitening toothpastes do not contain bleach (sodium hypochlorite) but some contain low concentrations of carbamide peroxide or hydrogen peroxide that help lighten tooth color. Whitening toothpastes typically can lighten tooth color by about one or two shades.
OTC Whitening Strips and Gels
Whitening strips were introduced into the market in the late 1980’s. They deliver a thin layer of peroxide gel on plastic strips shaped to fit onto the buccal surfaces of the teeth. There are a variety of white strip products on the market with varying instructions. A typical set of instructions are to apply the strips twice daily for 30 minutes for 14 days. Tooth lightening can be seen in several days and this method can lighten the teeth by 1 or 2 shades. There are some newer whitening strip products that require only one 30-minute application per day that have the same whitening end point as the two-a-day products.
Whitening gels are peroxide-based gels applied with a small brush directly to the surface of the teeth. Manufacturer’s instructions are usually twice a day applications for 14 days. Like the whitening strips, the teeth can usually be lightened by 1 or 2 shades.
Whitening Rinses
Whitening rinses contain oxygen sources such as hydrogen peroxide to react with the chromogens. Manufacturer’s instructions are for twice a day rinsing for 60 seconds each. It takes up to 3 months to see a 1 or 2 shade improvement in tooth color.
Tray-Based Tooth Whiteners
Tray-based tooth whitening systems are available both professionally and OTC. This method involves use of a fitted tray containing carbamide peroxide-bleaching gel worn for 2 to 4 hours a day or overnight. Usually by following the manufacturer instructions tooth whitening is noticeable in a few days, lightening the teeth by 1 or 2 shades.
In-Office Whitening
Quicker tooth lightening can be achieved through in-office whitening because the products deliver higher concentrations of peroxide than OTC. Consequently, gingival tissues are usually protected before the agent is applied. Some products claim to increase the oxidation of chromogens by exposure to heat or an intense blue light with a wave length between 480 nm and 520 nm to activate the product while on the tooth, causing the chemical reactions to proceed faster. Some professionals use laser systems to increase the rate of the chemical reactions. This use of lasers is considered to be an ‘off-label’ use of laser systems in dentistry by the US Food and Drug Administration. In a systematic review by Buchalla and Attin3 no added benefit from light-activated systems was found and thus the American Dental Association does not endorse such whitening systems. Tooth lightening results are seen after one 30- to 60-minute treatment. More dramatic results can be obtained with several applications.
Risks associated with Tooth Whitening
Risks commonly reported with tooth whitening include increased tooth sensitivity and mild gingival irritation. The degree of these side effects is directly related to the concentration of the peroxide bleach component, duration of the treatment, and the non-bleach composition of the product used. Tooth sensitivity usually occurs at the time of treatment and can last several days; gingival irritation begins within a day of the treatment and can also last several days. There are additional risks that have been reported from in vitro studies which include tooth erosion, tooth mineral degradation, increased susceptibility to demineralization, and pulpal damage.4 The ultimate endpoint for tooth whitening is dependent upon the tooth itself, with common wisdom telling us that all treatment regimens will eventually arrive at the same whitening endpoint. This is not exactly true as some very aggressive regimens can damage the tooth through dehydration and demineralization such that the tooth temporarily appears whiter.
What’s new in bleaching research?
New studies have shown that aggressive tooth bleaching can cause increased tooth sensitivity, changes in tooth microstructure, and restoration changes. Aggressive bleaching can chemically react with composite restorations, glass ionomer cements, sealants, and ceramic crowns, thus reducing their stability.
In one in vitro study seven tooth colored restoration substrates including a nanohybrid composite, a microhybrid composite, a flowable composite, and a packable composite resin, along with a compomer, a glass ionomer cement and a sintered ceramic used for CAD\/CAM restorations were exposed to 40 % hydrogen peroxide gel following manufacturer’s instructions at either 25 °C or 37 ° C and placed in artificial saliva between treatments.5 All of the materials were found to have surface softening with greater softening observed at 37 °C except for the sintered ceramic. No substance loss was observed for any material. However, the conditions of the experiments did not include subsequent abrasion (toothbrushing with dentifrice) as would occur in vivo and thus loss of restorative material from the softened surfaces is possible.
Another in vitro study looked at the effect of home bleaching on color change and translucency of resin composites. Five commercially available composites were treated for 14 days with either 10 % carbamide gel or 10 % hydrogen peroxide gel following manufacturer’s instructions. There was significant (and unacceptable) color change in all of the composites with either of the home-based treatments. They found no significant difference between the carbamide peroxide and hydrogen peroxide treatments in the color changes. Interestingly, there was no change in the resin composite translucency indicating that the color change was restricted to the surface of the resin composites.6
A randomized clinical trial showed that in-office bleaching of restored teeth using a 35 % hydrogen peroxide product caused tooth sensitivity in all cases. There was significantly greater intensity of tooth sensitivity pain for teeth that had restorations than for sound teeth. It was concluded that in-office bleaching with 35 % hydrogen peroxide was effective for patients with restored teeth, however that a higher degree of pain was found for these patients, especially associated with the upper lateral incisors.7
The risk of tooth structure damage has received attention by researchers who have evaluated the effects of aggressive tooth bleaching treatments on tooth structure and susceptibility to demineralization. Some of these studies have found that aggressive whitening treatments can change the surface integrity, microstructure of enamel crystals, and susceptibility to demineralization.
In an in vitro study performed in our lab we tested five different bleaching products for erosion of human enamel. The five products included strips at 6.5 % hydrogen peroxide, and gels at 10 % and 22 % carbamide peroxide, 35 % hydrogen peroxide, and a sodium hypochlorite containing gel system. We followed the manufacturer’s instructions and measured the loss of enamel surface by polarized light microscopy. We found that although some surfaces were softened, no enamel erosion was found.8
A new in vitro study conducted in Japan evaluated the susceptibility of a tooth to subsequent demineralization after a home based 10 % carbamide peroxide bleaching regimen compared to a more aggressive office-based 35 % hydrogen peroxide photoactivated regimen. Extracted teeth of color Vita shade A3 were bleached following manufacturer’s instructions until the shade was lightened to Vita shade A2 for all teeth. The teeth were then demineralized for two weeks and evaluated for mineral density loss. This study found that the surface integrity of the home-based treated teeth was altered such that significantly greater demineralization occurred in the home-based treated teeth than in the office-based treated teeth. The authors postulate that the peroxide in the office based gel penetrates deeper into the enamel before it was activated by photoirradiation.9
The effect of cold-light activated bleaching treatment on enamel surfaces in vitro was studied because there is concern that either heat (infrared) or ultraviolet light exposure of teeth and gingiva during office bleaching could cause pulp and/or gingival tissue damage.10 In this study the crystal and surface microstructure of dental enamel was evaluated after 35 % hydrogen peroxide bleaching with cold-light irradiation (group LP); 35 % hydrogen peroxide bleaching without cold-light irradiation (group P); a control group treated with what is identified as a silica dioxide catalyzing agent as a peroxide-free bleaching agent (control group NP); and a control group treated with the cold-light irradiation alone (control group L). The authors report that no color change or enamel crystal size change was observed in the two control groups, indicating that the cold-light treatment alone or the silica dioxide agent had no effect on the tooth structure. However, the groups that had 35 % hydrogen peroxide (with or without cold-light) did result in significant color change as well as significant decrease in crystal size and crystallinity. There was no significant difference in the degree of color change between the cold-light activated hydrogen peroxide and the hydrogen peroxide only groups. Additionally, surface roughness was observed to increase in all groups except the cold-light only control group. The authors conclude that the 35% hydrogen peroxide solution had a major demineralization effect on enamel surface and the cold-light had no significant increased or decreased effect on the demineralization or color change. The mechanism suggested for the surface demineralization is that during the bleaching procedure the pH of the whitening agent becomes more acidic and the hydrogen ions attack the enamel crystals, freeing calcium and phosphate ions from the enamel surface. Several important deductions can be made from this study: 1. Aggressive bleaching can lead to surface demineralization and reduction of enamel crystallinity; 2. Cold-light activation seems to have little effect on color change or tooth structure; and 3. Hydrogen peroxide reduces the pH on the tooth surface during treatment, leading to surface demineralization.
One of the common questions posited by patients is “How long will the treatment last?” It is difficult to predict the persistence of bleaching regimens because the patient may routinely expose their dentition to food or beverages which are known to stain teeth and would experience re-staining within a month. However, if the teeth are not exposed to chromogens such as coffee, red wine, cigarette smoke, then it would be reasonable to assume that whitened teeth could persist or up to a year. There are several in vitro and clinical studies on this topic.
An in vitro study that looked at the color change of enamel, dentine, and combined enamel and dentin of bleached tooth samples found that the color was not stable over time with regard to lightness. However, yellowness did not return to baseline within 1 year.11
Another in vitro study designed to evaluate the color stability of bleaching after light activation with either a halogen unit, laser, LED unit; or bleaching without light activation found that all the tested methods achieved good aesthetic results even 3 months after the end of the bleaching. Additionally, the authors found that light activation of the bleaching agent was not beneficial compared to bleaching alone and light activation made no difference in the color stability up to 3 months after bleaching.12
In a recent clinical trial it was found that by following a regimen consisting of in-office bleaching for two sessions with a 1-week interval, followed by home bleaching once a month for 3 months gave more persistence in color change over a 6-month period than in-office bleaching alone.13 This later study shows that this regimen for whitening maintenance can extend the effectiveness of the whitening treatment.
A common topic for study is to evaluate the efficacy of the so-called light activation of peroxide-based bleaching. The three studies reviewed above on the persistence of whitening treatments found that light activation had no effect on the bleaching. The efficacy of light activation is controversial with numerous studies finding both improvement in short term and long term whitening as well as studies that find no effect on whitening at all. The controversy is largely due to study designs and methodology which are very divergent. The studies are heterogeneous and the results cannot be used in a meta-analysis. Meta-analysis is a powerful statistical evaluation method that combines the results from eligible RCTs of a treatment, in an effort to obtain a better understanding of how well the treatment works and to determine significance of that treatment. The recent studies below were selected because they are either randomized clinical trials that evaluated efficacy of light activation or an authoritative systematic literature review and meta-analysis of the best studies available.
In a randomized clinical trial involving 90 patients using a split mouth design, found that the degree of bleaching obtained with a home-bleaching technique using 10 % carbamide peroxide gel applied via a tray was similar to that obtained with the in-office technique that applied 35 % hydrogen peroxide, regardless of light irradiation or the combination of home/in-office techniques.14 The use of a light source for in-office bleaching did not influence the rate of bleaching, or the intensity of tooth sensitivity, or the durability of the bleaching effect; therefore, light irradiation is not recommended. The combination of in-office and home-bleaching techniques increased the rate of bleaching only in the first week. However, the same combination did not influence the results after the first week. Increase in the tooth sensitivity was observed with the in-office technique immediately after treatment, regardless of light irradiation.14 In view of these results – especially the higher degree of tooth sensitivity with the in-office techniques, the authors conclude that “Dentists must inform their patients about the expected outcomes of each procedure and provide an evidence-based choice.”
A systematic review and meta-analysis of the literature to evaluate the influence of light on bleaching efficacy and tooth sensitivity during in-office bleaching found that light increases the risk of tooth sensitivity during in-office bleaching.15 This review also found that light did not improve the bleaching effect when high concentrations of hydrogen peroxide (25–35%) were employed. The authors conclude that “dentists should use the light-activated system with great caution or avoid its use.” One disturbing aspect of this systematic review is that after nearly 30 years of tooth whitening there were only 11 randomized clinical trials of sufficient quality to be included in the meta-analysis out of the 301 studies regarding light-activated bleaching. Clearly there is a need for high quality clinical trials to help the profession understand the effects and risks associated with tooth whitening products and procedures.
What does this mean?
These new studies provide a body of evidence for the profession to use in the counseling, care and treatment of the dental patient. See Box 1 for conclusions drawn from the literature.
Box 1.
Conclusions Drawn from Whitening Literature
Light activation offers no benefits for amount of whitening achieved, persistence of the whitening treatment, or avoidance of tooth sensitivity from the whitening treatment.
Home-based bleaching (following manufacturer’s instructions) results in less tooth sensitivity than in-office bleaching.
The optimal regimen to obtain persistence of tooth whitening is to follow an in-office treatment with monthly home-based touch-up treatments using OTC products.
Aggressive bleaching with high concentrations of hydrogen peroxide office-based products causes enamel softening, surface roughness, and an increase in the susceptibility of the tooth to demineralization, based upon in vitro findings.
Dental restorations are susceptible to unacceptable color change even when using the home-based OTC systems.
In-office bleaching of restored teeth using a 35 % hydrogen peroxide product caused tooth sensitivity in all cases. Teeth with restorations have a significantly greater chance of becoming sensitive and result in a greater degree of pain when exposed to whitening regimens.
Summary.
When used following manufacturer’s instructions, hydrogen peroxide and carbamide peroxide based tooth whitening is safe and effective. However as with all dental therapies, there are risks, and practices should be tailored to the needs of each individual patient, based upon type and extent of staining, dietary habits, previous restorations and other intraoral conditions. Patients should be informed of the risks associated with tooth whitening and, if using agents a home, instructed for identification of adverse occurrences in order to seek professional help if needed. Supervision of the tooth whitening strategy by an oral healthcare professional will reduce the potential risks and optimize benefits of tooth bleaching.16
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Declaration:
None
References
- 1.Christensen GJ. Are snow-white teeth really so desirable? J Am Dent Assoc. 2005;136:933–935. doi: 10.14219/jada.archive.2005.0295. [DOI] [PubMed] [Google Scholar]
- 2.American Academy of Cosmetic Dentistry [assessed 01.06.14];Teeth Whitening. www.aacd.com/whitening.
- 3.Buchalla W, Attin T. External bleaching therapy with activation by heat, light or laser--a systematic review. Dent Mater. 2007;23:586–596. doi: 10.1016/j.dental.2006.03.018. [DOI] [PubMed] [Google Scholar]
- 4.Goldberg M, Grootveld M, Lynch E. Undesirable and adverse effects of tooth-whitening products: a review. 2010;14:1–10. doi: 10.1007/s00784-009-0302-4. [DOI] [PubMed] [Google Scholar]
- 5.Yu H, Li Q, Wang Y, Cheng H. Effects of temperature and in-office bleaching agents on surface and subsurface properties of aesthetic restorative materials. J Dent. 2013;41:1290–1296. doi: 10.1016/j.jdent.2013.07.015. [DOI] [PubMed] [Google Scholar]
- 6.Kurtulmus-Yilmaz S, Cengiz E, Ulusoy N, Ozak ST, Yuksel E. The effect of home-bleaching application on the color and translucency of five resin composites. J Dent. 2013;41S:e70–e75. doi: 10.1016/j.jdent.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 7.Bonafe E, Bacovis CL, Iensen S, Loguercia AD, Reis A, Kossatz S. Tooth sensitivity and efficacy of in-office bleaching in restored teeth. J Dent. 2013;41:363–369. doi: 10.1016/j.jdent.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 8.Tompkins AM, Coleman SS, Carey CM. Erosive Capacity of Five Commercial Bleaching Products on Human Enamel. J Dent Res. 2014;93(Spec Iss A) ???? [Google Scholar]
- 9.Ogura K, Tanaka R, Shibata Y, Miyazaki T, Hisamitsu H. In vitro demineralization of tooth enamel subjected to two whitening regimens. J Am Dent Assoc. 2013;144:799–807. doi: 10.14219/jada.archive.2013.0190. [DOI] [PubMed] [Google Scholar]
- 10.Shi X-C, Ma H, Zhou J-L, Li W. The effect of cold-light-activated bleaching treatment on enamel surfaces in vitro. Internat J Oral Sci. 2012;4:208–213. doi: 10.1038/ijos.2012.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiegand A, Drebenstedt S, Roos M, Magalhaes AC, Attin T. 12-Month color stability of enamel, dentine, and enamel-dentine samples after bleaching. Clin Oral Invest. 2008;12:303–310. doi: 10.1007/s00784-008-0195-7. [DOI] [PubMed] [Google Scholar]
- 12.Hahn P, Schondelmaier N, Wolkewitz M, Altenburger MJ, Polydorou O. Efficacy of tooth bleaching with and without light activation and its effect on the pulp temperature: an in vitro study. Odontol. 2013;101:67–74. doi: 10.1007/s10266-012-0063-4. [DOI] [PubMed] [Google Scholar]
- 13.Al Quran FAM, Mansour Y, Al-Hyarl S, Al Wahadnl A, Mair L. Efficacy and persistence of tooth bleaching using a diode laser with three different treatment regimens. Eur J Esthet Dent. 2011;6:436–445. [PubMed] [Google Scholar]
- 14.Bernardon JK, Sartori N, Ballarin A, Perdigao J, Lopes G, Baratieri LN. Clinical performance of vital bleaching techniques. Oper Dent. 2010;35:3–10. doi: 10.2341/09-008CR. [DOI] [PubMed] [Google Scholar]
- 15.He LB, Shao MY, Tan K, Xu X, Li JY. The effects of light on bleaching and tooth sensitivity during in-office vital bleaching: a systematic review and meta-analysis. J Dent. 2012;40:644–653. doi: 10.1016/j.jdent.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 16.Li Y, Greenwall L. Safety issues of tooth whitening using peroxide-based materials. Brit Dent J. 2013;215:29–4. doi: 10.1038/sj.bdj.2013.629. [DOI] [PubMed] [Google Scholar]